Non-Pharmacological Pain Management in Labor: A Systematic Review
Abstract
:1. Introduction
2. Understanding Pain in Labor
3. Materials and Methods
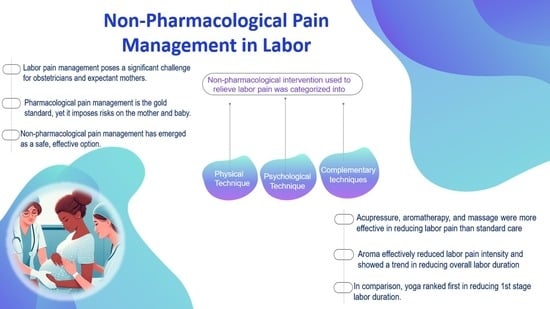
4. Categorization of Non-Pharmacological Methods for Pain Relief in Labor
4.1. Physical Modalities
| Methods | Methods Sub-Types | Proposed Mechanism of Action | Perceived Benefit | Authors’ Name; Publication Year |
|---|---|---|---|---|
| Massage |
|
|
| Pawale et al. [30]; 2020 Silva Gallo et al. [31]: 2013 Eskandari F et al. [32]; 2022 |
| Pressure on precise anatomical locations |
|
|
| Smith et al. [33]; 2020 Schlaeger et al. [34]; 2017 Eshraghi et al. [35]; 2021 |
| Transcutaneous Electrical Nerve Stimulation (TENS) |
|
|
| Thuvarakan et al. [36]; 2020 Gibson et al. [37]; 2019 Daniel et al. [38]; 2021 |
| Water immersion |
|
|
| Cluett et al. [39]; 2018 Carlsson et al. [40]; 2020 Cooper et al. [41]; 2022 |
| Heat therapy |
|
|
| Goswami et al. [42]; 2022 Akbarzadeh et al. [43]; 2018 Akbarzadeh et al. [44]; 2016 Dastjerd et al. [45]; 2023 |
| Cold therapy |
|
|
| Shirvani et al. [46]; 2014 Emine et al. [47]; 2022 Serap et al. [48]; 2022 |
| Breathing techniques |
|
|
| Baljon et al. [49]; 2022 Issac et al. [50]; 2023 Yuksel H et al. [51]; 2017 Boaviagem et al. [52]; 2017 |
| Positioning and Movement |
|
|
| Huang et al. [53]; 2019 Ondeck et al. [54]; 2019 Borges et al. [55]; 2021 Ali SA et al. [56]; 2018 |
4.2. Psychological Techniques
- Relaxation techniques;
- Virtual reality (VR);
- Music;
- Distraction technique.
| Methods | Methods Sub-Types | Proposed Mechanism of Action | Perceived Benefit | Authors’ Name; Publication Year |
|---|---|---|---|---|
| Relaxation technique |
| Progressive muscle relaxation, guided imagery, and visualization have been found to be effective in mitigating anxiety and fostering tranquility throughout labor. |
| Smith et al. [15]; 2018 Zhang et al. [60] Jahdi et al. [61]; 2017 |
| Virtual reality (VR) |
|
|
| Massov et al. [62]; 2021 Musters et al. [63]; 2023 Baradwan et al. [64]; 2022Xu et al. [65]; 2022 |
| Music | -- |
|
| Timmerman et al. [66]; 2023 Estrella-Juarez et al. [67]; 2023 Chehreh et al. [68]; 2023 García González et al. [69]; 2018 |
| Distraction |
|
|
| Ireland et al. [70]; 2016 Amiri et al. [71]; 2019 Melillo et al. [72]; 2022 |
4.3. Complementary and Alternative Approaches
5. Discussion
5.1. The Efficiency of Non-Pharmacological Pain Management Techniques in Reducing Labor Pain
5.2. Benefits of Non-Pharmacological Pain Management
5.3. Challenges of Non-Pharmacological Pain Management
5.4. Side Effects of Non-Pharmacological Methods
| Method | Category of Action | Authors Name; Year |
|---|---|---|
| Physical Non-Pharmacological Techniques | ||
| Massage |
| Pawale et al. [30]; 2020 Sindle et al. [119]; 2021 |
| Acupressure | If too much pressure is used
| Tan et al. [120]; 2015 Torkiyan et al. [121]; 2021 |
| Transcutaneous electrical nerve stimulation (TENS) |
| Johnson et al. [122]; 2007 Mokhtari et al. [123]; 2020 Njogu et al. [124]; 2021 |
| Water immersion |
| Cluett et al. [39]; 2018 Cooper et al. [125]; 2018 Maude et al. [126]; 2020 |
| Heat and cold therapy |
| Türkmen et al. [127]; 2021 Didevar et al. [128]; 2022 |
| Breathing techniques |
| Yuksel et al. [51]; 2017 Issac et al. [50]; 2023 |
| Psychological Non-Pharmacological Technique | ||
| Relaxation techniques |
| Kaple et al. [129]; 2023 Smith et al. [15]; 2018 |
| Virtual Reality (VR) |
| Kirca et al. [130]; 2023 Carus et al. [131]; 2022 Kılıç et al. [132]; 2023 |
| Music |
| Santiváñez et al. [133]; 2020 Chehreh et al. [134]; 2023 Surucu et al. [135]; 2018 |
| Distraction |
| Yurtsev et al. [136]; 2021 Amiri et al. [71]; 2019 |
| Complementary and Alternative Approaches | ||
| Hypnosis |
| Beevi et al. [137]; 2019 Babbar et al. [138]; 2021 Azizmohammadi et al. [139]; 2019 |
| Aromatherapy |
| Kendall et al. [140]; 2018 Tanvisut et al. [86]; 2018 |
| Dancing |
| Akin et al. [141]; 2022 Akin et al. [84]; 2020 |
| Photomodulation |
| Traverzim et al. [89]; 2018 Badger et al. [142]; 2017 |
5.5. Further Research and Future Perspective
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jones, L. Pain Management for Women in Labour: An Overview of Systematic Reviews. J. Evid. Based Med. 2012, 5, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.L.; Jackson, A.D. The Historical Development of Obstetric Anesthesia and Its Contributions to Perinatology. Am. J. Perinatol. 2017, 34, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Skowronski, G.A. Pain Relief in Childbirth: Changing Historical and Feminist Perspectives. Anaesth. Intensiv. Care 2015, 43, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.A. Advances in Labor Analgesia. Int. J. Women’s Health 2009, 1, 139–154. [Google Scholar] [CrossRef]
- Boselli, E.; Hopkins, P.; Lamperti, M.; Estèbe, J.P.; Fuzier, R.; Biasucci, D.G.; Disma, N.; Pittiruti, M.; Traškaitė, V.; Macas, A.; et al. European Society of Anaesthesiology and Intensive Care Guidelines on Peri-Operative Use of Ultrasound for Regional Anaesthesia (PERSEUS Regional Anesthesia): Peripheral Nerves Blocks and Neuraxial Anaesthesia. Eur. J. Anaesthesiol. 2021, 38, 219–250. [Google Scholar] [CrossRef]
- Smith, L.A.; Burns, E.; Cuthbert, A. Parenteral Opioids for Maternal Pain Management in Labour. Cochrane Database Syst. Rev. 2018, 2018, CD007396. [Google Scholar] [CrossRef]
- Callahan, E.C.; Lee, W.; Aleshi, P.; George, R.B. Modern Labor Epidural Analgesia: Implications for Labor Outcomes and Maternal-Fetal Health. Am. J. Obstet. Gynecol. 2023, 228, S1260–S1269. [Google Scholar] [CrossRef]
- Marcum, Z.A.; Griend, J.P.; Linnebur, S.A. FDA Drug Safety Communications: A Narrative Review and Clinical Considerations for Older Adults. Am. J. Geriatr. Pharmacother. 2012, 10, 264–271. [Google Scholar] [CrossRef]
- Zipursky, J.S.; Gomes, T.; Everett, K.; Calzavara, A.; Paterson, J.M.; Austin, P.C.; Mamdani, M.M.; Ray, J.G.; Juurlink, D.N. Maternal Opioid Treatment after Delivery and Risk of Adverse Infant Outcomes: Population Based Cohort Study. BMJ 2023, 380, e074005. [Google Scholar] [CrossRef]
- Halliday, L.; Nelson, S.M.; Kearns, R.J. Epidural Analgesia in Labor: A Narrative Review. Int. J. Gynecol. Obstet. 2022, 159, 356–364. [Google Scholar] [CrossRef]
- Zuarez-Easton, S.; Erez, O.; Zafran, N.; Carmeli, J.; Garmi, G.; Salim, R. Pharmacologic and Nonpharmacologic Options for Pain Relief during Labor: An Expert Review. Am. J. Obstet. Gynecol. 2023, 228, S1246–S1259. [Google Scholar] [CrossRef] [PubMed]
- Siyoum, M.; Mekonnen, S. Labor Pain Control and Associated Factors among Women Who Gave Birth at Leku Primary Hospital, Southern Ethiopia. BMC Res. Notes 2019, 12, 619. [Google Scholar] [CrossRef]
- Beigi, S.; Valiani, M.; Alavi, M.; Mohamadirizi, S. The Relationship between Attitude toward Labor Pain and Length of the First, Second, and Third Stages in Primigravida Women. J. Educ. Health Promot. 2019, 8, 130. [Google Scholar] [CrossRef]
- Komariah, N.; Wahyuni, S. The Relation Between Labor Pain with Maternal Anxiety. In Proceedings of the First International Conference on Health, Social Sciences and Technology (ICoHSST 2020), Palembang, Indonesia, 20–21 October 2020; Volume 521. [Google Scholar] [CrossRef]
- Smith, C.A.; Levett, K.M.; Collins, C.T.; Armour, M.; Dahlen, H.G.; Suganuma, M. Relaxation Techniques for Pain Management in Labour. Cochrane Database Syst. Rev. 2018, 2018, CD009514. [Google Scholar] [CrossRef]
- Cook, K.; Loomis, C. The Impact of Choice and Control on Women’s Childbirth Experiences. J. Perinat. Educ. 2012, 21, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Lunda, P.; Minnie, C.S.; Benadé, P. Women’s Experiences of Continuous Support during Childbirth: A Meta-Synthesis. BMC Pregnancy Childbirth 2018, 18, 167. [Google Scholar] [CrossRef]
- Stjernholm, Y.V.; Charvalho, P.d.S.; Bergdahl, O.; Vladic, T.; Petersson, M. Continuous Support Promotes Obstetric Labor Progress and Vaginal Delivery in Primiparous Women—A Randomized Controlled Study. Front. Psychol. 2021, 12, 582823. [Google Scholar] [CrossRef]
- Makvandi, S.; Mirzaiinajmabadi, K.; Tehranian, N.; Esmily, H.; Mirteimoori, M. The Effect of Normal Physiologic Childbirth on Labor Pain Relief: An Interventional Study in Mother-Friendly Hospitals. Maedica 2018, 13, 286. [Google Scholar]
- Hoffmann, L.; Hilger, N.; Banse, R. The Mindset of Birth Predicts Birth Outcomes: Evidence from a Prospective Longitudinal Study. Eur. J. Soc. Psychol. 2023, 53, 857–871. [Google Scholar] [CrossRef]
- Whitburn, L.Y.; Jones, L.E.; Davey, M.A.; McDonald, S. The Nature of Labour Pain: An Updated Review of the Literature. Women Birth 2018, 32, 28–38. [Google Scholar] [CrossRef]
- Navarro-Prado, S.; Sánchez-Ojeda, M.; Marmolejo-Martín, J.; Kapravelou, G.; Fernández-Gómez, E.; Martín-Salvador, A. Cultural Influence on the Expression of Labour-Associated Pain. BMC Pregnancy Childbirth 2022, 22, 836. [Google Scholar] [CrossRef]
- Yaya Bocoum, F.; Kabore, C.P.; Barro, S.; Zerbo, R.; Tiendrebeogo, S.; Hanson, C.; Dumont, A.; Betran, A.P.; Bohren, M.A. Women’s and Health Providers’ Perceptions of Companionship during Labor and Childbirth: A Formative Study for the Implementation of WHO Companionship Model in Burkina Faso. Reprod. Health 2023, 20, 46. [Google Scholar] [CrossRef] [PubMed]
- WHO. Companion of Choice during Labour and Childbirth for Improved Quality of Care; No. 4; Publications of the World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L. The PRISMA 2020 state-ment: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimized digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Leonardo, R. PICO: Model for clinical questions. Evid. Based Med. Pract. 2018, 3, 2. [Google Scholar]
- Klein, B.E.; Gouveia, H.G. USE Of NON-PHARMACOLOGICAL PAIN RELIEF METHODS In LABOR. Cogitare Enferm. 2022, 27, 481–496. [Google Scholar] [CrossRef]
- Madden, K.L.; Turnbull, D.; Cyna, A.M.; Adelson, P.; Wilkinson, C. Pain Relief for Childbirth: The Preferences of Pregnant Women, Midwives and Obstetricians. Women Birth 2013, 26, 33–40. [Google Scholar] [CrossRef]
- Pawale, M.; Salunkhe, J. Effectiveness of Back Massage on Pain Relief during First Stage of Labor in Primi Mothers Admitted at a Tertiary Care Center. J. Fam. Med. Prim. Care 2020, 9, 5933. [Google Scholar] [CrossRef]
- Silva Gallo, R.B.; Santana, L.S.; Jorge Ferreira, C.H.; Marcolin, A.C.; PoliNeto, O.B.; Duarte, G.; Quintana, S.M. Massage Reduced Severity of Pain during Labour: A Randomised Trial. J. Physiother. 2013, 59, 5933–5938. [Google Scholar] [CrossRef] [PubMed]
- Eskandari, F.; Mousavi, P.; Valiani, M.; Ghanbari, S.; Iravani, M. A Comparison of the Effect of Swedish Massage with and without Chamomile Oil on Labor Outcomes and Maternal Satisfaction of the Childbirth Process: A Randomized Controlled Trial. Eur. J. Med. Res. 2022, 27, 266. [Google Scholar] [CrossRef]
- Smith, C.A.; Collins, C.T.; Levett, K.M.; Armour, M.; Dahlen, H.G.; Tan, A.L.; Mesgarpour, B. Acupuncture or Acupressure for Pain Management during Labour. Cochrane Database Syst. Rev. 2020, 2, CD009232. [Google Scholar] [CrossRef]
- Schlaeger, J.M.; Gabzdyl, E.M.; Bussell, J.L.; Takakura, N.; Yajima, H.; Takayama, M.; Wilkie, D.J. Acupuncture and Acupressure in Labor. J. Midwifery Womens Health 2017, 62, 12–28. [Google Scholar] [CrossRef] [PubMed]
- Ashtarkan, M.J.; Akbari, S.A.A.; Nasiri, M.; Heshmat, R.; Eshraghi, N. Comparison of the Effect of Acupressure at SP6 and SP8 Points on Pain Intensity and Duration of the First Stage of Labor. Evid. Based Care J. 2021, 11, 25–34. [Google Scholar] [CrossRef]
- Thuvarakan, K.; Zimmermann, H.; Mikkelsen, M.K.; Gazerani, P. Transcutaneous Electrical Nerve Stimulation As A Pain-Relieving Approach in Labor Pain: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Neuromodulation 2020, 23, 732–746. [Google Scholar] [CrossRef]
- Gibson, W.; Wand, B.M.; Meads, C.; Catley, M.J.; O’Connell, N.E. Transcutaneous Electrical Nerve Stimulation (TENS) for Chronic Pain—An Overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2019, 4, CD011890. [Google Scholar] [CrossRef] [PubMed]
- Daniel, L.; Benson, J.; Hoover, S. Transcutaneous Electrical Nerve Stimulation for Pain Management for Women in Labor. MCN Am. J. Matern. Child Nurs. 2021, 46, 76–81. [Google Scholar] [CrossRef]
- Cluett, E.R.; Burns, E.; Cuthbert, A. Immersion in Water during Labour and Birth. Cochrane Database Syst. Rev. 2018, 2018, CD000111. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, T.; Ulfsdottir, H. Waterbirth in Low-Risk Pregnancy: An Exploration of Women’s Experiences. J. Adv. Nurs. 2020, 76, 1221–1231. [Google Scholar] [CrossRef]
- Cooper, M.; Warland, J. The Views and Perceptions of Water Immersion for Labor and Birth from Women Who Had Birthed in Australia but Had Not Used the Option. Eur. J. Midwifery 2022, 6, 54. [Google Scholar] [CrossRef]
- Goswami, S.; Jelly, P.; Sharma, S.K.; Negi, R.; Sharma, R. The Effect of Heat Therapy on Pain Intensity, Duration of Labor during First Stage among Primiparous Women and Apgar Scores: A Systematic Review and Meta-Analysis. Eur. J. Midwifery 2022, 6, 66. [Google Scholar] [CrossRef] [PubMed]
- Akbarzadeh, M.; Nematollahi, A.; Farahmand, M.; Amooee, S. The Effect of Two-Staged Warm Compress on the Pain Duration of First and Second Labor Stages and Apgar Score in Prim Gravida Women: A Randomized Clinical Trial. J. Caring Sci. 2018, 7, 21–26. [Google Scholar] [CrossRef]
- Akbarzadeh, M.; Vaziri, F.; Farahmand, M.; Masoudi, Z.; Amooee, S.; Zare, N. The Effect of Warm Compress Bistage Intervention on the Rate of Episiotomy, Perineal Trauma, and Post-partum Pain Intensity in Primiparous Women with Delayed Valsalva Maneuver Referring to the Selected Hospitals of Shiraz University of Medical Sciences in 2012–2013. Adv. Ski. Wound Care 2016, 29, 79–84. [Google Scholar] [CrossRef]
- Dastjerd, F.; Erfanian Arghavanian, F.; Sazegarnia, A.; Akhlaghi, F.; Esmaily, H.; Kordi, M. Effect of Infrared Belt and Hot Water Bag on Labor Pain Intensity among Primiparous: A Randomized Controlled Trial. BMC Pregnancy Childbirth 2023, 23, 405. [Google Scholar] [CrossRef]
- Shirvani, M.A.; Ganji, Z. The Influence of Cold Pack on Labour Pain Relief and Birth Outcomes: A Randomised Controlled Trial. J. Clin. Nurs. 2014, 23, 2473–2480. [Google Scholar] [CrossRef]
- Yildirim, E.; Inal, S. The Effect of Cold Application to the Sacral Area on Labor Pain and Labor Process: A Randomized Controlled Trial. Health Sci. J. Adıyaman Univ. 2022, 8, 96–105. [Google Scholar] [CrossRef]
- Altınayak, S.Ö.; Özkan, H. The Effects of Conventional, Warm and Cold Acupressure on the Pain Perceptions and Beta-Endorphin Plasma Levels of Primiparous Women in Labor: A Randomized Controlled Trial. Explore 2022, 18, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Baljon, K.; Romli, M.H.; Ismail, A.H.; Khuan, L.; Chew, B.H. Effectiveness of Breathing Exercises, Foot Reflexology and Massage (BRM) on Maternal and Newborn Outcomes Among Primigravidae in Saudi Arabia: A Randomized Controlled Trial. Int. J. Womens Health 2022, 14, 279–295. [Google Scholar] [CrossRef]
- Issac, A.; Nayak, S.G.; Priyadarshini, T.; Balakrishnan, D.; Halemani, K.; Mishra, P.; Indumathi, P.; Vijay, V.R.; Jacob, J.; Stephen, S. Effectiveness of Breathing Exercise on the Duration of Labour: A Systematic Review and Meta-Analysis. J. Glob. Health 2023, 13, 04023. [Google Scholar] [CrossRef] [PubMed]
- Yuksel, H.; Cayir, Y.; Kosan, Z.; Tastan, K. Effectiveness of Breathing Exercises during the Second Stage of Labor on Labor Pain and Duration: A Randomized Controlled Trial. J. Integr. Med. 2017, 15, 456–461. [Google Scholar] [CrossRef]
- Boaviagem, A.; Melo Junior, E.; Lubambo, L.; Sousa, P.; Aragão, C.; Albuquerque, S.; Lemos, A. The Effectiveness of Breathing Patterns to Control Maternal Anxiety during the First Period of Labor: A Randomized Controlled Clinical Trial. Complement. Ther. Clin. Pract. 2016, 26, 30–35. [Google Scholar] [CrossRef]
- Huang, J.; Zang, Y.; Ren, L.H.; Li, F.J.; Lu, H. A Review and Comparison of Common Maternal Positions during the Second-Stage of Labor. Int. J. Nurs. Sci. 2019, 6, 460–467. [Google Scholar] [CrossRef]
- Ondeck, M. Healthy Birth Practice #2: Walk, Move Around, and Change Positions Throughout Labor. J. Perinat. Educ. 2019, 28, 81–87. [Google Scholar] [CrossRef]
- Borges, M.; Moura, R.; Oliveira, D.; Parente, M.; Mascarenhas, T.; Natal, R. Effect of the Birthing Position on Its Evolution from a Biomechanical Point of View. Comput. Methods Programs Biomed. 2021, 200, 105921. [Google Scholar] [CrossRef]
- Abdul-Sattar Khudhur Ali, S.; Mirkhan Ahmed, H. Effect of Change in Position and Back Massage on Pain Perception during First Stage of Labor. Pain Manag. Nurs. 2018, 19, 288–294. [Google Scholar] [CrossRef]
- Gür, E.Y.; Apay, S.E. The Effect of Cognitive Behavioral Techniques Using Virtual Reality on Birth Pain: A Randomized Controlled Trial. Midwifery 2020, 91, 102856. [Google Scholar] [CrossRef] [PubMed]
- Khojasteh, F.; Afrashte, M.; Khayat, S.; Navidian, A. Effect of Cognitive–Behavioral Training on Fear of Childbirth and Sleep Quality of Pregnant Adolescent Slum Dwellers. J. Educ. Health Promot. 2022, 11, 311. [Google Scholar] [CrossRef]
- Ehde, D.M.; Dillworth, T.M.; Turner, J.A. Cognitive-Behavioral Therapy for Individuals with Chronic Pain Efficacy, Innovations, and Directions for Research. Am. Psychol. 2014, 69, 153–166. [Google Scholar] [CrossRef] [PubMed]
- The Efficacy of Prenatal Yoga on Labor Pain: A Systematic Review and Meta-analysis—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/37023315/ (accessed on 23 July 2023).
- Jahdi, F.; Sheikhan, F.; Haghani, H.; Sharifi, B.; Ghaseminejad, A.; Khodarahmian, M.; Rouhana, N. Yoga during Pregnancy: The Effects on Labor Pain and Delivery Outcomes (A Randomized Controlled Trial). Complement Ther. Clin. Pract. 2017, 27, 1–4. [Google Scholar] [CrossRef]
- Massov, L. Giving Birth on a Beach Women’s Experiences of Using Virtual Reality in Labour A Pragmatic Mixed Methods Approach. Ph.D. Thesis, Open Access Te Herenga Waka-Victoria University of Wellington, Wellington, New Zealand, 2021. [Google Scholar] [CrossRef]
- Musters, A.; Vandevenne, A.S.; Franx, A.; Wassen, M.M.L.H. Virtual Reality Experience during Labour (VIREL); a Qualitative Study. BMC Pregnancy Childbirth 2023, 23, 283. [Google Scholar] [CrossRef] [PubMed]
- Baradwan, S.; Khadawardi, K.; Badghish, E.; Alkhamis, W.H.; Dahi, A.A.; Abdallah, K.M.; Kamel, M.; Sayd, Z.S.; Mohamed, M.A.; Ali, H.M.; et al. The Impact of Virtual Reality on Pain Management during Normal Labor: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sex. Reprod. Healthc. 2022, 32, 100720. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Chen, S.; Liu, Y.; Jing, Y.; Gu, P. The Effects of Virtual Reality in Maternal Delivery: Systematic Review and Meta-Analysis. JMIR Serious Games 2022, 10, e36695. [Google Scholar] [CrossRef] [PubMed]
- Timmerman, H.; van Boekel, R.L.M.; van de Linde, L.S.; Bronkhorst, E.M.; Vissers, K.C.P.; van der Wal, S.E.I.; Steegers, M.A.H. The Effect of Preferred Music versus Disliked Music on Pain Thresholds in Healthy Volunteers. An Observational Study. PLoS ONE 2023, 18, e0280036. [Google Scholar] [CrossRef]
- Estrella-Juarez, F.; Requena-Mullor, M.; Garcia-Gonzalez, J.; Lopez-Villen, A.; Alarcon-Rodriguez, R. Effect of Virtual Reality and Music Therapy on the Physiologic Parameters of Pregnant Women and Fetuses and on Anxiety Levels: A Randomized Controlled Trial. J. Midwifery Womens Health 2023, 68, 35–43. [Google Scholar] [CrossRef]
- Chehreh, R.; Tavan, H.; Karamelahi, Z. The Effect of Music Therapy on Labor Pain: Systematic Review and Meta-Analysis. Douleurs Évaluation Diagn. Trait. 2023, 24, 110–117. [Google Scholar] [CrossRef]
- García González, J.; Ventura Miranda, M.I.; Requena Mullor, M.; Parron Carreño, T.; Alarcón Rodriguez, R. Effects of Prenatal Music Stimulation on State/Trait Anxiety in Full-Term Pregnancy and Its Influence on Childbirth: A Randomized Controlled Trial. J. Matern. Fetal Neonatal Med. 2018, 31, 1058–1065. [Google Scholar] [CrossRef] [PubMed]
- Ireland, L.D.; Allen, R.H. Pain Management for Gynecologic Procedures in the Office. Obstet. Gynecol. Surv. 2016, 71, 89–98. [Google Scholar] [CrossRef]
- Amiri, P.; Mirghafourvand, M.; Esmaeilpour, K.; Kamalifard, M.; Ivanbagha, R. The Effect of Distraction Techniques on Pain and Stress during Labor: A Randomized Controlled Clinical Trial. BMC Pregnancy Childbirth 2019, 19, 534. [Google Scholar] [CrossRef]
- Melillo, A.; Maiorano, P.; Rachedi, S.; Caggianese, G.; Gragnano, E.; Gallo, L.; De Pietro, G.; Guida, M.; Giordano, A.; Chirico, A. Labor Analgesia: A Systematic Review and Meta-Analysis of Non-Pharmacological Complementary and Alternative Approaches to Pain during First Stage of Labor. Crit. Rev. Eukaryot. Gene Expr. 2022, 32, 61–89. [Google Scholar] [CrossRef]
- Smith, C.A.; Shewamene, Z.; Galbally, M.; Schmied, V.; Dahlen, H. The Effect of Complementary Medicines and Therapies on Maternal Anxiety and Depression in Pregnancy: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2019, 245, 428–439. [Google Scholar] [CrossRef]
- Hosseni, S.F.; Pilevarzadeh, M.; Vazirinasab, H. Non-Pharmacological Strategies on Pain Relief During Labor. Biosci. Biotechnol. Res. Asia 2016, 13, 701–706. [Google Scholar] [CrossRef]
- Frawley, J.; Adams, J.; Sibbritt, D.; Steel, A.; Broom, A.; Gallois, C. Prevalence and Determinants of Complementary and Alternative Medicine Use during Pregnancy: Results from a Nationally Representative Sample of Australian Pregnant Women. Aust. N. Z. J. Obstet. Gynaecol. 2013, 53, 347–352. [Google Scholar] [CrossRef]
- Fjær, E.L.; Landet, E.R.; McNamara, C.L.; Eikemo, T.A. The Use of Complementary and Alternative Medicine (CAM) in Europe. BMC Complement Med. Ther. 2020, 20, 108. [Google Scholar] [CrossRef]
- Madden, K.; Middleton, P.; Cyna, A.M.; Matthewson, M.; Jones, L. Hypnosis for Pain Management during Labour and Childbirth. Cochrane Database Syst. Rev. 2016, 2016, CD009356. [Google Scholar] [CrossRef] [PubMed]
- Cyna, A.M.; Crowther, C.A.; Robinson, J.S.; Andrew, M.I.; Antoniou, G.; Baghurst, P. Hypnosis Antenatal Training for Childbirth: A Randomised Controlled Trial. BJOG 2013, 120, 1248–1259. [Google Scholar] [CrossRef] [PubMed]
- Downe, S.; Finlayson, K.; Melvin, C.; Spiby, H.; Ali, S.; Diggle, P.; Gyte, G.; Hinder, S.; Miller, V.; Slade, P.; et al. Self-Hypnosis for Intrapartum Pain Management in Pregnant Nulliparous Women: A Randomised Controlled Trial of Clinical Effectiveness. BJOG 2015, 122, 1226–1234. [Google Scholar] [CrossRef]
- McLaren, H.; Patmisari, E.; Hamiduzzaman, M.; Jones, M.; Taylor, R. Respect for Religiosity: Review of Faith Integration in Health and Wellbeing Interventions with Muslim Minorities. Religions 2021, 12, 692. [Google Scholar] [CrossRef]
- Desmawati, D.; Kongsuwan, W.; Chatchawet, W. Effect of Nursing Intervention Integrating an Islamic Praying Program on Labor Pain and Pain Behaviors in Primiparous Muslim Women. Iran. J. Nurs. Midwifery Res. 2019, 24, 220–226. [Google Scholar] [CrossRef]
- Kocak, M.Y.; Göçen, N.N.; Akin, B. The Effect of Listening to the Recitation of the Surah Al-Inshirah on Labor Pain, Anxiety and Comfort in Muslim Women: A Randomized Controlled Study. J. Relig. Health 2022, 61, 2945–2959. [Google Scholar] [CrossRef]
- Abdolahian, S.; Ghavi, F.; Abdollahifard, S.; Sheikhan, F. Effect of Dance Labor on the Management of Active Phase Labor Pain & Clients’’Satisfaction: A Randomized Controlled Trial Study. Glob. J. Health Sci. 2014, 6, 219–226. [Google Scholar] [CrossRef]
- Akin, B.; Saydam, B.K. The Effect of Labor Dance on Perceived Labor Pain, Birth Satisfaction, and Neonatal Outcomes. Explore 2020, 16, 310–317. [Google Scholar] [CrossRef]
- Tabatabaeichehr, M.; Mortazavi, H. The Effectiveness of Aromatherapy in the Management of Labor Pain and Anxiety: A Systematic Review. Ethiop. J. Health Sci. 2020, 30, 449–458. [Google Scholar] [CrossRef]
- Tanvisut, R.; Traisrisilp, K.; Tongsong, T. Efficacy of Aromatherapy for Reducing Pain during Labor: A Randomized Controlled Trial. Arch. Gynecol. Obstet. 2018, 297, 1145–1150. [Google Scholar] [CrossRef]
- Hamdamian, S.; Nazarpour, S.; Simbar, M.; Hajian, S.; Mojab, F.; Talebi, A. Effects of Aromatherapy with Rosa Damascena on Nulliparous Women’’ ‘Pain and Anxiety of Labor during First Stage of Labor. J. Integr. Med. 2018, 16, 120–125. [Google Scholar] [CrossRef]
- Traverzim, M.A.; Sobral, A.P.T.; Fernandes, K.P.S.; De Fátima Teixeira Silva, D.; Pavani, C.; Mesquita-Ferrari, R.A.; Horliana, A.C.R.T.; Gomes, A.O.; Bussadori, S.K.; Motta, L.J. The Effect of Photobiomodulation on Analgesia during Childbirth: A Controlled and Randomized Clinical Trial. Photobiomodul Photomed Laser Surg. 2021, 39, 265–271. [Google Scholar] [CrossRef]
- Traverzim, M.A.D.S.; Makabe, S.; Silva, D.F.T.; Pavani, C.; Bussadori, S.K.; Fernandes, K.S.P.; Motta, L.J. Effect of Led Photobiomodulation on Analgesia during Labor: Study Protocol for a Randomized Clinical Trial. Medicine 2018, 97, e11120. [Google Scholar] [CrossRef]
- Akbaş, P.; Özkan Şat, S.; Yaman Sözbir, Ş. The Effect of Holistic Birth Support Strategies on Coping With Labor Pain, Birth Satisfaction, and Fear of Childbirth: A Randomized, Triple-Blind, Controlled Trial. Clin. Nurs. Res. 2022, 31, 1352–1361. [Google Scholar] [CrossRef] [PubMed]
- Bohren, M.A.; Hofmeyr, G.J.; Sakala, C.; Fukuzawa, R.K.; Cuthbert, A. Continuous Support for Women during Childbirth. Cochrane Database Syst. Rev. 2017, 2017, CD003766. [Google Scholar] [CrossRef] [PubMed]
- Ip, W.Y.; Tang, C.S.K.; Goggins, W.B. An Educational Intervention to Improve Women’s Ability to Cope with Childbirth. J. Clin. Nurs. 2009, 18, 2125–2135. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, I.; Pradhan, N.; Sharma, J. Factors Influencing Perception of Labor Pain among Parturient Women at Tribhuvan University Teaching Hospital. Nepal J. Obstet. Gynaecol. 2013, 8, 26–30. [Google Scholar] [CrossRef]
- Parthasarathy, S.; Ravishankar, M.; Hemanthkumar, V.R. Reported Pain during Labour—A Qualitative Study of Influencing Factors among Parturient during Confinement in Private or Government Hospital. J. Clin. Diagn. Res. 2016, 10, UC01–UC03. [Google Scholar] [CrossRef]
- Smith, C.A.; Levett, K.M.; Collins, C.T.; Dahlen, H.G.; Ee, C.C.; Suganuma, M. Massage, Reflexology and Other Manual Methods for Pain Management in Labour. Cochrane Database Syst. Rev. 2018, 2018, CD009290. [Google Scholar] [CrossRef]
- Hu, Y.; Lu, H.; Huang, J.; Zang, Y. Efficacy and Safety of Non-Pharmacological Interventions for Labour Pain Management: A Systematic Review and Bayesian Network Meta-Analysis. J. Clin. Nurs. 2021, 30, 3398–3414. [Google Scholar] [CrossRef] [PubMed]
- Doering, K.; Patterson, J.; Griffiths, C.R. Japanese Women’’ ‘Experiences of Pharmacological Pain Relief in New Zealand. Women Birth 2014, 27, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Beyable, A.A.; Bayable, S.D.; Ashebir, Y.G. Pharmacologic and Non-Pharmacologic Labor Pain Management Techniques in a Resource-Limited Setting: A Systematic Review. Ann. Med. Surg. 2022, 74, 103312. [Google Scholar] [CrossRef]
- Thomson, G.; Feeley, C.; Moran, V.H.; Downe, S.; Oladapo, O.T. Women’s Experiences of Pharmacological and Non-Pharmacological Pain Relief Methods for Labour and Childbirth: A Qualitative Systematic Review. Reprod. Health 2019, 16, 71. [Google Scholar] [CrossRef] [PubMed]
- Nanji, J.A.; Carvalho, B. Pain Management during Labor and Vaginal Birth. Best Pract. Res. Clin. Obstet. Gynaecol. 2020, 67, 100–112. [Google Scholar] [CrossRef]
- Sng, B.L.; Sia, A.T.H. Maintenance of Epidural Labour Analgesia: The Old, the New and the Future. Best Pract. Res. Clin. Anaesthesiol. 2017, 31, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Gourounti, K.; Sarantaki, A.; Dafnou, M.E.; Hadjigeorgiou, E.; Lykeridou, A.; Middleton, N. A Qualitative Study of Assessing Learning Needs and Digital Health Literacy in Pregnancy: Baby Buddy Forward Greek Findings. Eur. J. Midwifery 2022, 6, 55. [Google Scholar] [CrossRef]
- Freeman, M.; Ayers, C.; Peterson, C.; Kansagara, D. Aromatherapy and Essential Oils: A Map of The Evidence. Evid. Synth. Program 2019. Available online: https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/books/NBK551017/ (accessed on 25 October 2023).
- Lira, L.C.S.; Amorim, M.M.; Delgado, A.; de Oliveira Menezes, M.; Takemoto, M.L.S. Concerning the Article Aromatherapy Intervention on Anxiety and Pain during First Stage Labour in Nulliparous Women: A Systematic Review and Meta-Analysis. J. Obstet. Gynaecol. 2021, 41, 1180. [Google Scholar] [CrossRef]
- Chen, S.F.; Wang, C.H.; Chan, P.T.; Chiang, H.W.; Hu, T.M.; Tam, K.W.; Loh, E.W. Labour Pain Control by Aromatherapy: A Meta-Analysis of Randomised Controlled Trials. Women Birth 2019, 32, 327–335. [Google Scholar] [CrossRef]
- Biana, C.B.; Cecagno, D.; Porto, A.R.; Cecagno, S.; Marques, V.D.A.; Soares, M.C. Non-Pharmacological Therapies Applied in Pregnancy and Labor: An Integrative Review. Rev. Esc. Enferm. 2021, 55, e03681. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.Y.; Gau, M.L.; Huang, C.J.; Cheng, H.M. Effects of Non-Pharmacological Coping Strategies for Reducing Labor Pain: A Systematic Review and Network Meta-Analysis. PLoS ONE 2022, 17, e0261493. [Google Scholar] [CrossRef]
- Leutenegger, V.; Grylka-Baeschlin, S.; Wieber, F.; Daly, D.; Pehlke-Milde, J. The Effectiveness of Skilled Breathing and Relaxation Techniques during Antenatal Education on Maternal and Neonatal Outcomes: A Systematic Review. BMC Pregnancy Childbirth 2022, 22, 856. [Google Scholar] [CrossRef] [PubMed]
- Hassan, W.N.M.; Shallal, F.; Roomi, A.B. Prediction of Successful Induction of Labor Using Ultrasonic Fetal Parameters. Curr. Women Health Rev. 2021, 18, 134–139. [Google Scholar] [CrossRef]
- Carter, H.H.; Spence, A.L.; Pugh, C.J.A.; Ainslie, P.; Naylor, L.H.; Green, D.J. Cardiovascular Responses to Water Immersion in Humans: Impact on Cerebral Perfusion. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2014, 306, R636–R640. [Google Scholar] [CrossRef]
- Ugwu, E.O.; Iferikigwe, E.S.; Obi, S.N.; Eleje, G.U.; Ozumba, B.C. Effectiveness of Antenatal Perineal Massage in Reducing Perineal Trauma and Post-Partum Morbidities: A Randomized Controlled Trial. J. Obstet. Gynaecol. Res. 2018, 44, 1252–1258. [Google Scholar] [CrossRef]
- Heim, M.; Makuch, M. Pregnant Women’s Knowledge of Non-Pharmacological Techniques for Pain Relief during Childbirth. Eur. J. Midwifery 2022, 6, 5. [Google Scholar] [CrossRef]
- Shang, J.; Dolikun, N.; Tao, X.; Zhang, P.; Woodward, M.; Hackett, M.L.; Henry, A. The Effectiveness of Postpartum Interventions Aimed at Improving Women’s Mental Health after Medical Complications of Pregnancy: A Systematic Review and Meta-Analysis. BMC Pregnancy Childbirth 2022, 22, 809. [Google Scholar] [CrossRef] [PubMed]
- Boateng, E.A.; Kumi, L.O.; Diji, A.K.A. Nurses and Midwives’ Experiences of Using Non-Pharmacological Interventions for Labour Pain Management: A Qualitative Study in Ghana. BMC Pregnancy Childbirth 2019, 19, 168. [Google Scholar] [CrossRef]
- Pietrzak, J.; M˛ Edrzycka-D ˛ Abrowska, W.; Wróbel, A.; Grzybowska, M.E. Women’s Knowledge about Pharmacological and Non-Pharmacological Methods of Pain Relief in Labor. Healthcare 2023, 11, 1882. [Google Scholar] [CrossRef]
- Maillefer, F.; de Labrusse, C.; Cardia-Vonèche, L.; Hohlfeld, P.; Stoll, B. Women and Healthcare Providers’ Perceptions of a Midwife-Led Unit in a Swiss University Hospital: A Qualitative Study. BMC Pregnancy Childbirth 2015, 15, 56. [Google Scholar] [CrossRef] [PubMed]
- McCauley, M.; Actis Danna, V.; Mrema, D.; Van Den Broek, N. “we Know It’s Labour Pain, so We Don’t Do Anything”: Healthcare Provider’s Knowledge and Attitudes Regarding the Provision of Pain Relief during Labour and after Childbirth. BMC Pregnancy Childbirth 2018, 18, 444. [Google Scholar] [CrossRef]
- Lally, J.E.; Thomson, R.G.; MacPhail, S.; Exley, C. Pain Relief in Labour: A Qualitative Study to Determine How to Support Women to Make Decisions about Pain Relief in Labour. BMC Pregnancy Childbirth 2014, 14, 6. [Google Scholar] [CrossRef]
- Sindle, A.; Martin, K. Art of Prevention: Essential Oils—Natural Products Not Necessarily Safe. Int. J. Women’s Dermatol. 2020, 7, 304–308. [Google Scholar] [CrossRef]
- Tan, J.Y.; Suen, L.K.P.; Wang, T.; Molassiotis, A. Sham Acupressure Controls Used in Randomized Controlled Trials: A Systematic Review and Critique. PLoS ONE 2015, 10, e0132989. [Google Scholar] [CrossRef]
- Torkiyan, H.; Sedigh Mobarakabadi, S.; Heshmat, R.; Khajavi, A.; Ozgoli, G. The Effect of GB21 Acupressure on Pain Intensity in the First Stage of Labor in Primiparous Women: A Randomized Controlled Trial. Complement Ther. Med. 2021, 58, 102683. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M. Transcutaneous Electrical Nerve Stimulation: Mechanisms, Clinical Application and Evidence. Rev. Pain 2007, 1, 7–11. [Google Scholar] [CrossRef]
- Mokhtari, T.; Ren, Q.; Li, N.; Wang, F.; Bi, Y.; Hu, L. Transcutaneous Electrical Nerve Stimulation in Relieving Neuropathic Pain: Basic Mechanisms and Clinical Applications. Curr. Pain Headache Rep. 2020, 24, 14. [Google Scholar] [CrossRef]
- Njogu, A.; Qin, S.; Chen, Y.; Hu, L.; Luo, Y. The Effects of Transcutaneous Electrical Nerve Stimulation during the First Stage of Labor: A Randomized Controlled Trial. BMC Pregnancy Childbirth 2021, 21, 164. [Google Scholar] [CrossRef]
- Cooper, M.; Warland, J.; McCutcheon, H. Australian Midwives Views and Experiences of Practice and Politics Related to Water Immersion for Labour and Birth: A Web Based Survey. Women Birth 2018, 31, 184–193. [Google Scholar] [CrossRef]
- Maude, R.M.; Kim, M. Getting into the Water: A Prospective Observational Study of Water Immersion for Labour and Birth at a New Zealand District Health Board. BMC Pregnancy Childbirth 2020, 20, 312. [Google Scholar] [CrossRef]
- Türkmen, H.; Oran, N.T. Massage and Heat Application on Labor Pain and Comfort: A Quasi-Randomized Controlled Experimental Study. Explore 2021, 17, 438–445. [Google Scholar] [CrossRef]
- Didevar, M.; Navvabi-Rigi, S.D.; Dadkhah, S. The Effectiveness of Heat Therapy and Cold Therapy in Labor Pain Intensity in Primiparous Women: A Randomized Controlled Trial. Nurs. Midwifery Stud. 2022, 11, 171–176. [Google Scholar] [CrossRef]
- Kaple, G.S.; Patil, S. Effectiveness of Jacobson Relaxation and Lamaze Breathing Techniques in the Management of Pain and Stress During Labor: An Experimental Study. Cureus 2023, 15, e33212. [Google Scholar] [CrossRef]
- Şolt Kırca, A.; Güdücü, N.; İkiz, B. The Effect of Virtual Glasses Application on Pain and Anxiety During Episiotomy Repair: Randomized Controlled Trial. Pain Manag. Nurs. 2023, 24, e123–e130. [Google Scholar] [CrossRef] [PubMed]
- Carus, E.G.; Albayrak, N.; Bildirici, H.M.; Ozmen, S.G. Immersive Virtual Reality on Childbirth Experience for Women: A Randomized Controlled Trial. BMC Pregnancy Childbirth 2022, 22, 354. [Google Scholar] [CrossRef]
- Kılıç, S.; Dereli Yılmaz, S. Virtual Reality Headset Simulating a Nature Environment to Improve Health Outcomes in Pregnant Women: A Randomized-Controlled Trial. Clin. Nurs. Res. 2023, 32, 1104–1114. [Google Scholar] [CrossRef]
- Santiváñez-Acosta, R.; Tapia-López, E.; de las, N.; Santero, M. Music Therapy in Pain and Anxiety Management during Labor: A Systematic Review and Meta-Analysis. Medicina 2020, 56, 526. [Google Scholar] [CrossRef] [PubMed]
- An, S.Y.; Park, E.J.; Moon, Y.R.; Lee, B.Y.; Lee, E.; Kim, D.Y.; Jeong, S.H.; Kim, J.K. The effects of music therapy on labor pain, childbirth experience, and self-esteem during epidural labor analgesia in primiparas: A non-randomized experimental study. Korean J. Women Health Nurs. 2023, 29, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Gokyildiz Surucu, S.; Ozturk, M.; Avcibay Vurgec, B.; Alan, S.; Akbas, M. The Effect of Music on Pain and Anxiety of Women during Labour on First Time Pregnancy: A Study from Turkey. Complement Ther. Clin. Pract. 2018, 30, 96–102. [Google Scholar] [CrossRef]
- Yurtsev, E.; Sahin, N. Distraction and Focusing on the Management of Labour Pain: Stereograms. J. Educ. Res. Nurs. 2021, 18, 196–202. [Google Scholar] [CrossRef]
- Beevi, Z.; Low, W.Y.; Hassan, J. The Effectiveness of Hypnosis Intervention in Alleviating Post-partum Psychological Symptoms. Am. J. Clin. Hypn. 2019, 61, 409–425. [Google Scholar] [CrossRef]
- Babbar, S.; Oyarzabal, A.J. The Application of Hypnosis in Obstetrics. Clin. Obstet. Gynecol. 2021, 64, 635–647. [Google Scholar] [CrossRef]
- Azizmohammadi, S.; Azizmohammadi, S. Hypnotherapy in Management of Delivery Pain: A Review. Eur. J. Transl. Myol. 2019, 29, 210–217. [Google Scholar] [CrossRef]
- Kendall, M.C. Efficacy of Aromatherapy to Reduce Labor Pain. Arch. Gynecol. Obstet. 2018, 298, 453. [Google Scholar] [CrossRef] [PubMed]
- Akin, B.; Yurteri Türkmen, H.; Yalnız Dilcen, H.; Sert, E. The Effect of Labor Dance on Traumatic Childbirth Perception and Comfort: A Randomized Controlled Study. Clin. Nurs. Res. 2022, 31, 909–917. [Google Scholar] [CrossRef]
- Badger, J.; Taylor, P.; Swain, I. The Safety of Electrical Stimulation in Patients with Pacemakers and Implantable Cardioverter Defibrillators: A Systematic Review. J. Rehabil. Assist. Technol. Eng. 2017, 4, 2055668317745498. [Google Scholar] [CrossRef]
- Shieh, P.L.; Cheng, L.Y.; Hsu, W.S.; Li, R.H. Mother-Infant Group Intervention on Maternal Depression and Bonding: A Quasi-Experimental Study. Matern. Child Health J. 2023, 27, 1114–1125. [Google Scholar] [CrossRef] [PubMed]
- Butcher, C.J.; Hussain, W. Digital Healthcare: The Future. Future Healthc. J. 2022, 9, 113–117. [Google Scholar] [CrossRef]
- Kassim, M.A.K.; Pantazi, A.C.; Tuta, L.A.; Balasa, A.L.; Mihai, C.M.; Mihai, L.; Frecus, C.E.; Lupu, V.V.; Lupu, A.; Andrusca, A. Non-Pharmacological Interventions for Pain Management in Hemodialysis: A Narrative Review. J. Clin. Med. 2023, 12, 5390. [Google Scholar] [CrossRef]
- Ingram, M.A.; Brady, S.; Peacock, A.S. The Barriers to Offering Non-Pharmacological Pain Management as an Initial Option for Laboring Women: A Review of the Literature. Eur. J. Midwifery 2022, 6, 37. [Google Scholar] [CrossRef] [PubMed]




| Methods | Methods Sub-Types | Proposed Mechanism of Action | Perceived Benefit | Authors’ Name; Publication Year |
|---|---|---|---|---|
| Hypnosis |
|
|
| Madden et al. [77]; 2016 Cyna et al. [78]; 2013 Downe et al. [79]; 2015 |
| Integration of religion/health and well-being |
|
|
| McLaren H et al. [80]; 2021 Desmawati et al. [81]; 2019 Kocak et al. [82]; 2022 |
| Dancing | -- |
|
| Abdolahian et al. [83]; 2014 Akin et al. [84]; 2020 |
| Aromatherapy |
Essential oils may be given as:
|
|
| Tabatabaeichehr et al. [85]; 2020 Sirkeci et al. [86]; 2023 Hamdamian et al. [87]; 2018 |
| Photomodulation | -- |
Irradiation induces.
|
| Traverzim et al. [88]: 2021 Traverzim et al. [89]; 2018 |
| Support therapy |
|
|
| Akbas et al. [90]; 2022 Bohren et al. [91]; 2017 Ip et al. [92]; 2009 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nori, W.; Kassim, M.A.K.; Helmi, Z.R.; Pantazi, A.C.; Brezeanu, D.; Brezeanu, A.M.; Penciu, R.C.; Serbanescu, L. Non-Pharmacological Pain Management in Labor: A Systematic Review. J. Clin. Med. 2023, 12, 7203. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12237203
Nori W, Kassim MAK, Helmi ZR, Pantazi AC, Brezeanu D, Brezeanu AM, Penciu RC, Serbanescu L. Non-Pharmacological Pain Management in Labor: A Systematic Review. Journal of Clinical Medicine. 2023; 12(23):7203. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12237203
Chicago/Turabian StyleNori, Wassan, Mustafa Ali Kassim Kassim, Zeena Raad Helmi, Alexandru Cosmin Pantazi, Dragos Brezeanu, Ana Maria Brezeanu, Roxana Cleopatra Penciu, and Lucian Serbanescu. 2023. "Non-Pharmacological Pain Management in Labor: A Systematic Review" Journal of Clinical Medicine 12, no. 23: 7203. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12237203