What Is the Most Effective Frictionless Method for Retracting Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection and Data Extraction
2.4. Assessment of Risk of Bias in Individual Studies
3. Results
3.1. Literature Search Flow and the Retrieved Studies
3.2. Characteristics of the Included Studies
3.3. Risk of Bias of Included Studies
3.4. Effects of Intervention
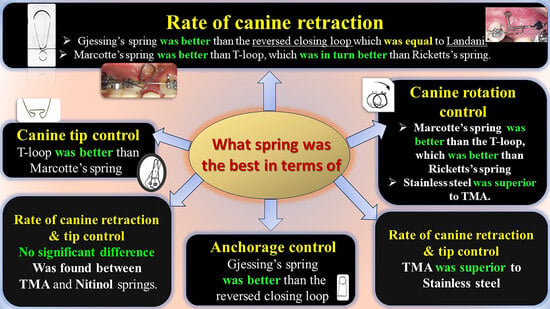
3.4.1. Rate of Canine Retraction
According to the Details of the Wires
According to the Spring Designs
3.4.2. Canine Tipping and Rotation following Canine Retraction
3.4.3. Anchorage Loss following Canine Retraction
4. Discussion
4.1. Rate of Canine Retraction
4.2. Canine Tipping and Rotation following Canine Retraction
4.3. Anchorage Loss following Canine Retraction
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| PubMed | #1 (Class II relationship OR extraction of the first premolars OR severe crowding OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR permanent occlusion OR anterior open bite) #2 (Upper anterior teeth retraction OR lower anterior teeth retraction OR space closure OR incisors retraction OR canine retraction OR En-masse retraction OR moving anterior teeth backward) #3 (Anchorage loss OR rotation OR inclination OR torque OR angulation OR tipping OR root resorption OR Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration) #4 (Frictionless Mechanics OR Sectional Technique OR Segmental technique OR springs for retracting T-loop OR L-loop OR Ricketts's spring OR Marcotte spring OR Ladanyi spring OR Gjessing retraction spring OR Reverse Closing Loop) #5 #1 AND #2 AND #3 AND #4 |
| CENTRAL (The Cochrane Library) | #1 (Class II relationship OR extraction of the first premolars OR severe crowding OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR permanent occlusion OR anterior open bite) #2 (Upper anterior teeth retraction OR lower anterior teeth retraction OR space closure OR incisors retraction OR canine retraction OR En-masse retraction OR moving anterior teeth backward) #3 (Anchorage loss OR rotation OR inclination OR torque OR angulation OR tipping OR root resorption OR Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration) #4 (Frictionless Mechanics OR Sectional Technique OR Segmental technique OR springs for retracting T-loop OR L-loop OR Ricketts's spring OR Marcotte spring OR Ladanyi spring OR Gjessing retraction spring OR Reverse Closing Loop) #5 #1 AND #2 AND #3 AND #4 |
| Web of Science | #1TS = (Class II relationship OR extraction of the first premolars OR severe crowding OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR permanent occlusion OR anterior open bite) #2TS = (Upper anterior teeth retraction OR lower anterior teeth retraction OR space closure OR incisors retraction OR canine retraction OR En-masse retraction OR moving anterior teeth backward) #3TS = (Anchorage loss OR rotation OR inclination OR torque OR angulation OR tipping OR root resorption OR Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration) #4TS = (Frictionless Mechanics OR Sectional Technique OR Segmental technique OR springs for retracting T-loop OR L-loop OR Ricketts's spring OR Marcotte spring OR Ladanyi spring OR Gjessing retraction spring OR Reverse Closing Loop) #5 #1 AND #2 AND #3 AND #4 |
| Scopus | #1 TITLE ABS (Class II relationship OR extraction of the first premolars OR severe crowding OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR permanent occlusion OR anterior open bite) #2 TITLE ABS-KEY (Upper anterior teeth retraction OR lower anterior teeth retraction OR space closure OR incisors retraction OR canine retraction OR En-masse retraction OR moving anterior teeth backward) #3 TITLE ABS-KEY (Anchorage loss OR rotation OR inclination OR torque OR angulation OR tipping OR root resorption OR Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration) #4 TITLE ABS-KEY (Frictionless Mechanics OR Sectional Technique OR Segmental technique OR springs for retracting T-loop OR L-loop OR Ricketts's spring OR Marcotte spring OR Ladanyi spring OR Gjessing retraction spring OR Reverse Closing Loop) #5 #1 AND #2 AND #3 AND #4 |
| EMBASE | #1 (Class II relationship OR extraction of the first premolars OR severe crowding OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR permanent occlusion OR anterior open bite) #2 (Upper anterior teeth retraction OR lower anterior teeth retraction OR space closure OR incisors retraction OR canine retraction OR En-masse retraction OR moving anterior teeth backward) #3 (Anchorage loss OR rotation OR inclination OR torque OR angulation OR tipping OR root resorption OR Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration) #4 (Frictionless Mechanics OR Sectional Technique OR Segmental technique OR springs for retracting T-loop OR L-loop OR Ricketts's spring OR Marcotte spring OR Ladanyi spring OR Gjessing retraction spring OR Reverse Closing Loop) #5 #1 AND #2 AND #3 AND #4 |
| Google scholar | (Class II relationship OR extraction of the first premolars OR severe crowding OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR permanent occlusion OR anterior open bite) AND (Upper anterior teeth retraction OR lower anterior teeth retraction OR space closure OR incisors retraction OR canine retraction OR En-masse retraction OR moving anterior teeth backward) AND (Anchorage loss OR rotation OR inclination OR torque OR angulation OR tipping OR root resorption OR Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration) AND (Frictionless Mechanics OR Sectional Technique OR Segmental technique OR springs for retracting T-loop OR L-loop OR Ricketts's spring OR Marcotte spring OR Ladanyi spring OR Gjessing retraction spring OR Reverse Closing Loop) |
| Trip | (Class II relationship OR extraction of the first premolars OR severe crowding OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR permanent occlusion OR anterior open bite) AND (Upper anterior teeth retraction OR lower anterior teeth retraction OR space closure OR incisors retraction OR canine retraction OR En-masse retraction OR moving anterior teeth backward) AND (Anchorage loss OR rotation OR inclination OR torque OR angulation OR tipping OR root resorption OR Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration) AND (Frictionless Mechanics OR Sectional Technique OR Segmental technique OR springs for retracting T-loop OR L-loop OR Ricketts's spring OR Marcotte spring OR Ladanyi spring OR Gjessing retraction spring OR Reverse Closing Loop) |
References
- Bishara, S.E. Textbook of Orthodontics; WB Saunders Company: Philadelphia, PA, USA, 2001. [Google Scholar]
- Al-Sibaie, S.; Hajeer, M.Y. Assessment of changes following en-masse retraction with mini-implants anchorage compared to two-step retraction with conventional anchorage in patients with class II division 1 malocclusion: A randomized controlled trial. Eur. J. Orthod. 2014, 36, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Khlef, H.N.; Hajeer, M.Y.; Ajaj, M.A.; Heshmeh, O. En-masse Retraction of Upper Anterior Teeth in Adult Patients with Maxillary or Bimaxillary Dentoalveolar Protrusion: A Systematic Review and Meta-analysis. J. Contemp. Dent. Pract. 2019, 20, 113–127. [Google Scholar] [PubMed]
- Leonardi, R.; Annunziata, A.; Licciardello, V.; Barbato, E. Soft tissue changes following the extraction of premolars in nongrowing patients with bimaxillary protrusion. A systematic review. Angle Orthod. 2010, 80, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Masaes, M.M.; Burhan, A.S.; Youssef, M.; Nawaya, F.R. T-loop spring vs. Ricketts maxillary canine retractor in canine retraction efficacy and anchorage loss control: A CBCT study. AJO-DO Clin. Companion 2022, 2, 26–40. [Google Scholar] [CrossRef]
- Sarikaya, S.; Haydar, B.; Ciger, S.; Ariyurek, M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Felemban, N.H.; Al-Sulaimani, F.F.; Murshid, Z.A.; Hassan, A.H. En masse retraction versus two-step retraction of anterior teeth in extraction treatment of bimaxillary protrusion. J. Orthod. Sci. 2013, 2, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Alhadlaq, A.; Alkhadra, T.; El-Bialy, T. Anchorage condition during canine retraction using transpalatal arch with continuous and segmented arch mechanics. Angle Orthod. 2016, 86, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, P.; Ingervall, B. A clinical study of maxillary canine retraction with a retraction spring and with sliding mechanics. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Burstone, C.J.; Choy, K. The Biomechanical Foundation of Clinical Orthodontics; Quintessence Publishing Company, Inc.: Batavia, IL, USA, 2015. [Google Scholar]
- Kuhlberg, A.J.; Priebe, D. Testing force systems and biomechanics--measured tooth movements from differential moment closing loops. Angle Orthod. 2003, 73, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.; Sundareswaran, S.; James, J. Comparative evaluation of the efficiency of canine retraction using modified Marcotte and T-loop retraction springs—A split-mouth, randomized clinical trial. J. Orthod. Sci. 2019, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Keng, F.Y.; Quick, A.N.; Swain, M.V.; Herbison, P. A comparison of space closure rates between preactivated nickel-titanium and titanium-molybdenum alloy T-loops: A randomized controlled clinical trial. Eur. J. Orthod. 2012, 34, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Ozkan, S.; Bayram, M. Comparison of direct and indirect skeletal anchorage systems combined with 2 canine retraction techniques. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Dincer, M.; Iscan, H.N. The effects of different sectional arches in canine retraction. Eur. J. Orthod. 1994, 16, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Mehta, K.R.; Sable, R.B. Comparison of the amount of maxillary canine retraction, with T-Loops, using TMA and Stainless steel Wires: A clinical study. J. Indian Orthod. Soc. 2013, 47, 178–183. [Google Scholar] [CrossRef]
- Hayashi, K.; Uechi, J.; Murata, M.; Mizoguchi, I. Comparison of maxillary canine retraction with sliding mechanics and a retraction spring: A three-dimensional analysis based on a midpalatal orthodontic implant. Eur. J. Orthod. 2004, 26, 585–589. [Google Scholar] [CrossRef] [PubMed]

| Orthodontics | Class II relationship, extraction of the first premolars, severe crowding, maxillary dentoalveolar protrusion, bimaxillary protrusion, permanent occlusion, and anterior open bite. |
| Treatment plan | Upper anterior teeth retraction, lower anterior teeth retraction, space closure, incisors retraction, canine retraction, en masse retraction, moving anterior teeth backward. |
| Outcomes | Anchorage loss, rotation, inclination, torque, angulation, tipping, and root resorption are among the factors that affect orthodontic tooth movement rate, amount, speed, velocity, and duration. |
| Intervention | Frictionless mechanics, sectional technique, segmental technique, springs for retracting T-loop, L-loop, Ricketts spring, Marcotte spring, Ladanyi spring, Gjessing retraction spring, and Reverse Closing Loop. |
| Authors | Patient Count, Average Age, and Study Design | The Application Mechanism and Force Intensity | Outcomes | Follow-Up Period | Extraction Time/Anchorage | Evaluation Instrument |
|---|---|---|---|---|---|---|
| Dincer and Iscan, 1994 [17] | Upper Jaw: 12 Range: 11 y, 9 m to 19 y, 9 m; mean age: 15 y. Lower Jaw: 8 Range: 11 y, 5 m to 16 y, 10 m Mean age: 13 y, 7 m. Split-mouth | Group 1: S.S 0.016 × 0.022-inch Reverse Closing Loop Group 2: S.S 0.016 × 0.022-inch Gjessing’s retraction spring Force: 150 g Bracket: 0.018 in/without angulation or torque. | Canine retraction rate, treatment time, tipping, and anchorage loss in both jaws | Until completion of the retraction of the canine | Immediately before retraction | CRs before and at the end of canine retraction Eight linear and two angular measurements were made on the cephalometric tracings for each upper and lower treatment group |
| Keng et al., 2012 [15] | 12 (6 male, 6 female) Age: 13 y, 3 m to 20 y, 1 m. Median: 14 y, 4 m both parallel and split-mouth | Group 1: TMA 0.017 × 0.025 TLS Group 2: NITI 0.018 × 0.025 TLS Force: 150 g Bracket: 0.018 in/the Wick Alexander prescription. | Rate of space closure per month and changes in upper canine tipping | Until completion of the canine retraction or achieving class I relationships. | Class II elastics, Nance and TADs according to the requirements of anchorage for each case | Upper dental impressions at the start and at each visit to assess space closure. A digital image of each cast was taken |
| Mehta and Sable, 2013 [18] | 15 Split-mouth | Group 1: TMA 0.017 × 0.025 TLS Group 2: S.S 0.016 × 0.022 TLS Force: 200 g Bracket: 0.018 in/MBT. | Amount of maxillary canine retraction, tipping, and rotation control | 4-month period | At the beginning of treatment. Nance holding arch | The rotation of the canines during retraction was evaluated by making occlusal photographs of the study models at the study’s start (T0) and end (T4). CRs at (T0) and (T4) for angulation. Linear measurement with a digital caliper |
| Ozkan and Bayram, 2016 [16] | 36 (17 male, 19 female) Mean age 16.8 ± 2.4 y Split-mouth | Group 1: Remaloy wires 0.016 × 0.022 Reverse Closing Loop Group 2: Remaloy wires 0.016 × 0.022 Ladanyi spring to the other canine randomly Force: 120 to 150 g Bracket: 0.018 in/MBT. | Canine distalization rates, anchorage loss, and rotation | Prior to acquiring a class I canine relationship | At the beginning of treatment. Indirect skeletal anchorage system: mini-implant-supported Nance appliance. Direct skeletal anchorage system: mini-implant | Casts before and after retraction for rotation study. The mesial and distal contact points of the canines were marked on the dental casts and transferred to the computer via a scanner CRs before the retraction and when the canines reached the class 1 relationship |
| Davis et al., 2019 [14] | 24 13–20 y Split-mouth | Group 1: 0.017 × 0.025 modified Marcotte spring Group 2: TLS Force: 150 g Bracket: 0.022-in/MBT. | Amount of retraction, rate of retraction, anchorage loss, tipping, and rotation | To completion of 18 weeks | At the beginning of treatment. TPA and banding of second molars | Study models at the beginning and after 18 weeks. The casts were then scanned CRS uses radiopaque TMA wire markers to differentiate the right and left sides for tipping |
| Masaes et al., 2022 [5] | 2 group (31) 14–23 y Group 1: n: 14 by T-loop spring (2 male, 12 female) Group 2: n: 17, Ricketts retractor. Retrospective study (4 ma, 13 fe) | Group 1: TMA 0.017 × 0.025 TLS. brackets: 0.022 in/edgewise Force: 344 g (at 6 mm activation) Group 2: blue Elgiloy 0.016 × 0.016 Ricketts maxillary canine retractor Brackets: 0.018 in/Ricketts prescription Force: 150 g. | Canine retraction efficacy (amount of canine retraction, tipping, rotation, torque, and root resorption) Anchorage loss control. | Until both canines reach a class I relationship | At the beginning of treatment. TPA | CBCT before retraction and after ending retraction of both left and right canines. |
| Authors | Rate of Canine Retraction | Tipping * | Rotation | Anchorage Loss & Root Resorption |
|---|---|---|---|---|
| Dincer and Iscan, 1994 [17] | Goup1: Right side (Reverse Closing Loop) Maxilla: 0.59 ± 0.35 mm/month. Mandible: 0.39 ± 0.15 mm/month Group2: Left side (Gjessing’s retraction spring) Maxilla: 0.85 ± 0.41 mm/month Mandible: 1.03 ± 0.85 mm/month | G1: 5.41 ± 5.18/7.75 months. G2: 3.33 ± 6.89/6.25 months. Nonsignificant | Anchorage loss: G1: 2.46 mm. G2: 1.63 mm. | |
| Keng et al., 2012 [15] | T-loop (TMA): 0.87 ± 0.34 mm/month. T-loop (NITI): 0.91 ± 0.46 mm/month Nonsignificant | NITI: 0.71 ± 2.34°/month. TMA: 1.15 ± 2.86°/month. Nonsignificant | ||
| Mehta and Sable, 2013 [18] | 0.017 × 0.025 TMA T-loop: 5.46 mm/4 months 0.016 × 0.022 S.S. T-loop: 4.20 mm/4 months | TMA: 7.83°/4 months. S.S: 10°/4 months. Indicating that the TMA had better control. | S.S. T-loop offered better rotational control (39.44%) over the TMA T-loop (50.82%). | |
| Ozkan and Bayram, 2016 [16] | Direct anchorage: RCL: 1.57 ± 0.53 mm/4 weeks. LS: 1.80 ± 0.67 mm/4 weeks. Nonsignificant Indirect anchorage: RCL: 1.45 ± 0.69 mm/4 weeks. LS: 1.42 ± 0.63 mm/4 weeks Nonsignificant | Direct anchorage: RCL: 16.82 ± 9.19°/7.62 mm. LS: 16.24 ± 4.97°/7.62 mm. Nonsignificant Indirect anchorage: RCL: 15.66 ± 6.34°/7.25 mm. LS: 15.90 ± 5.12°/6.94 mm. Nonsignificant | Direct anchorage: RCL: 33.55°/7.62 mm LS: 33.71°/7.62 mm. Nonsignificant Indirect anchorage: RCL: 27.65°/7.25 mm LS: 28.19°/6.94 mm. Nonsignificant | Anchorage loss: Direct anchorage: RCL: 1.21 ± 2.48 mm LS: 0.02 ± 2.28 mm Nonsignificant Indirect anchorage: RCL: 1.01 ± 2.83 mm. LS: 0.91 ± 2.25 mm Nonsignificant |
| Davis et al., 2019 [14] | MS: 1.187 ± 0.232 mm/month. TLS: 0.708 ± 0.157 mm/month. | MS: 6.645 ± 2.744°/3 months. T-loop: 1.229 ± 5.124°/3 months. | MS: 2.416 ± 1.868°/3 months. T-loop: 5.645 ± 2.849°/3 months. | Anchorage loss: MS: 0.791 ± 0.142. T-loop: 0.250 ± 0.466. |
| Masaes et al., 2022 [5] | TLS: 1.85 ± 0.64 mm/5.92 ± 1.75 months. RMCR: 1.10 ± 0.63 mm/5.26 ± 1.10 months. | TLS: 8.06 ± 3.66°/5.92 ± 1.75 months. RMCR: 10.19 ± 3.99°/5.26 ± 1.10 months. Nonsignificant. | TLS: 5.71 ± 6.95 °/5.92 ± 1.75 months. RMCR: 14.99 ± 9.24 °/5.26 ± 1.10 months. | Anchorage loss: TLS: 1.40 ± 0.89 mm/5.92 ± 1.75 months. RMCR: 1.20 ± 0.65 mm/5.26 ± 1.10 months. Nonsignificant Root resorption: TLS: 0.51 ± 0.5 mm. RMCR: 0.62 ± 0.59 mm. Nonsignificant |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kheshfeh, M.N.; Hajeer, M.Y.; Al Hinnawi, M.F.; Awawdeh, M.A.; Albalawi, F.; Alotaib, G.S.; Alam, M.K.; Zakaria, A.S. What Is the Most Effective Frictionless Method for Retracting Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review. J. Clin. Med. 2024, 13, 231. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm13010231
Kheshfeh MN, Hajeer MY, Al Hinnawi MF, Awawdeh MA, Albalawi F, Alotaib GS, Alam MK, Zakaria AS. What Is the Most Effective Frictionless Method for Retracting Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review. Journal of Clinical Medicine. 2024; 13(1):231. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm13010231
Chicago/Turabian StyleKheshfeh, Mohammad Naem, Mohammad Younis Hajeer, Mhd. Firas Al Hinnawi, Mohammed Adel Awawdeh, Farraj Albalawi, Ghada Serhan Alotaib, Mohammad Khursheed Alam, and Ahmad Salim Zakaria. 2024. "What Is the Most Effective Frictionless Method for Retracting Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review" Journal of Clinical Medicine 13, no. 1: 231. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm13010231