The Effect of an Active Break Intervention on Nonspecific Low Back Pain and Musculoskeletal Discomfort during Prolonged Sitting among Young People—Protocol for a Randomized Controlled Trial
Abstract
:1. Background
2. Methods
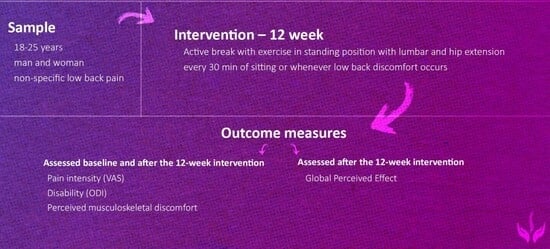
2.1. Study Population
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
2.2. Assessment
2.3. Pre-Intervention Questionnaire
- -
- gender,
- -
- age,
- -
- current physical activity (sports discipline, number of training days and hours per week),
- -
- illnesses, injuries, surgical history due to spinal problems, treatment related to LBP, diagnosed defects in body posture,
- -
- experience of LBP within the last three months. Individuals who respond positively (“yes”) to the question “Have you experienced low back pain for the last three months?” will then answer the question in the frequency of experiencing LBP (rarely, few times per week, often, or constantly) and the types of situations in which LBP occurred or increased.
2.4. Outcome Measures
2.5. Primary Outcome Measures
2.5.1. Pain Intensity
2.5.2. Disability Index
2.5.3. Perceived Musculoskeletal Discomfort during Prolonged Sitting
2.5.4. The Global Perceived Effect
2.6. Secondary Outcome Measures
Post-Intervention Questionnaire
2.7. Intervention Protocol
2.8. Active Break Program
2.9. Control Group
2.10. Procedure
2.11. Study Procedures
2.11.1. Sample Size
2.11.2. Randomization
2.11.3. Blinding
3. Study Participants Protocol Adherence
3.1. Statistical Analysis
3.2. Missing Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary lifestyle: Overview of updated evidence of potential health risks. Korean J. Fam. Med. 2020, 41, 365. [Google Scholar] [CrossRef]
- Paterson, D.C.; Ramage, K.; Moore, S.A.; Riazi, N.; Tremblay, M.S.; Faulkner, G. Exploring the impact of COVID-19 on the movement behaviors of children and youth: A scoping review of evidence after the first year. J. Sport Health Sci. 2021, 10, 675–689. [Google Scholar] [CrossRef] [PubMed]
- Rossi, L.; Behme, N.; Breuer, C. Physical activity of children and adolescents during the COVID-19 pandemic—A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 11440. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Huang, W.Y.; Sheridan, S.; Sit, C.H.-P.; Chen, X.-K.; Wong, S.H.-S. COVID-19 pandemic brings a sedentary lifestyle in young adults: A cross-sectional and longitudinal study. Int. J. Environ. Res. Public Health 2020, 17, 6035. [Google Scholar] [CrossRef] [PubMed]
- Knapp, E.A.; Dong, Y.; Dunlop, A.L.; Aschner, J.L.; Stanford, J.B.; Hartert, T.; Teitelbaum, S.L.; Hudak, M.L.; Carroll, K.; O’Connor, T.G.; et al. Changes in BMI during the COVID-19 pandemic. Pediatrics 2022, 150, e2022056552. [Google Scholar] [CrossRef]
- Yaseen, Q.B.; Salah, H. The impact of e-learning during COVID-19 pandemic on students’ body aches in Palestine. Sci. Rep. 2021, 11, 1–9. [Google Scholar] [CrossRef]
- Papalia, G.F.; Petrucci, G.; Russo, F.; Ambrosio, L.; Vadalà, G.; Iavicoli, S.; Papalia, R.; Denaro, V. COVID-19 Pandemic Increases the Impact of Low Back Pain: A Systematic Review and Metanalysis. Int. J. Environ. Res. Public Health 2022, 19, 4599. [Google Scholar] [CrossRef]
- GBD 2021 Low Back Pain Collaborators. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e316–e329. [Google Scholar] [CrossRef]
- Kędra, A.; Kolwicz-Gańko, A.; Sitarski, D.; Kędra, P.; Czaprowski, D. Prevalence of back pain and the knowledge of preventive measures in a cohort of 11619 Polish school-age children and youth—An epidemiological study. Medicine 2019, 98, e15729. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Noll, M.; Candotti, C.T.; Rosa, B.N.d.; Vieira, A.; Loss, J.F. Back pain and its risk factors in Brazilian adolescents: A longitudinal study. Br. J. Pain 2021, 15, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Fang, K.; Mu, M.; Liu, K.; He, Y. Screen time and childhood overweight/obesity: A systematic review and meta—Analysis. Child Care Health Dev. 2019, 45, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef] [PubMed]
- Hoogendoorn, W.E.; Van Poppel, M.N.M.; Bongers, P.M.; Koes, B.W.; Bouter, L.M. Physical load during work and leisure time as risk factors for back pain. Scand. J. Work. Environ. Health 1999, 25, 387–403. [Google Scholar] [CrossRef]
- Heneweer, H.; Vanhees, L.; Picavet, H.S.J. Physical activity and low back pain: A U-shaped relation? Pain 2009, 143, 21–25. [Google Scholar] [CrossRef]
- McGill, S.M.; Hughson, R.L.; Parks, K. Changes in lumbar lordosis modify the role of the extensor muscles. Clin. Biomech. 2000, 15, 777–780. [Google Scholar] [CrossRef]
- Bontrup, C.; Taylor, W.R.; Fliesser, M.; Visscher, R.; Green, T.; Wippert, P.-M.; Zemp, R. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl. Ergon. 2019, 81, 102894. [Google Scholar] [CrossRef]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Is ‘ideal’sitting posture real?: Measurement of spinal curves in four sitting postures. Man. Ther. 2009, 14, 404–408. [Google Scholar] [CrossRef]
- Akkarakittichoke, N.; Janwantanakul, P. Seat pressure distribution characteristics during 1 h sitting in office workers with and without chronic low back pain. Saf. Health Work. 2017, 8, 212–219. [Google Scholar] [CrossRef]
- Zadoń, H.; Nowakowska-Lipiec, K.; Michnik, R. A sitting or standing position-which one exerts more loads on the musculoskeletal system of the lumbar spine? Comparative tests based on the methods of mathematical modelling. Acta Bioeng. Biomech. 2021, 23, 113–120. [Google Scholar] [CrossRef]
- Callaghan, J.P.; McGill, S.M. Low back joint loading and kinematics during standing and unsupported sitting. Ergonomics 2001, 44, 280–294. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.F.; Farrell, G.T.; Jefford, E.; Naylor, C.S.; O’Sullivan, K.J. Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population. Spine 2006, 31, E707–E712. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.M.; Hawley, J.A.; McKenzie, R.A.; van Wijmen, P.M. A comparison of the effects of two sitting postures on back and referred pain. Spine 1991, 16, 1185–1191. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, K.; O’Sullivan, P.; O’Sullivan, L.; Dankaerts, W. What do physiotherapists consider to be the best sitting spinal posture? Man. Ther. 2012, 17, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Korakakis, V.; O’Sullivan, K.; O’Sullivan, P.B.; Evagelinou, V.; Sotiralis, Y.; Sideris, A.; Sakellariou, K.; Karanasios, S.; Giakas, G. Physiotherapist perceptions of optimal sitting and standing posture. Musculoskelet. Sci. Pract. 2019, 39, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.Y.; Park, S.Y.; Park, J.H.; Kim, T.K.; Jung, T.W.; Lee, H.M. The effect of standing and different sitting positions on lumbar lordosis: Radiographic study of 30 healthy volunteers. Asian Spine J. 2015, 9, 762. [Google Scholar] [CrossRef]
- Lee, T.P.; Woon, C.K.; Ching, L.Y.; Boon, O.P. Sitting Behaviour in Home Working Environment and its Association with Back Pain during Pandemic in Malaysia. J. Clin. Health Sci. 2022, 7, 10–24. [Google Scholar] [CrossRef]
- Emerson, S.; Emerson, K.; Fedorczyk, J. Computer workstation ergonomics: Current evidence for evaluation, corrections, and recommendations for remote evaluation. J. Hand. Ther. 2021, 34, 166–178. [Google Scholar] [CrossRef]
- Waongenngarm, P.; Areerak, K.; Janwantanakul, P. The effects of breaks on low back pain, discomfort, and work productivity in office workers: A systematic review of randomized and non-randomized controlled trials. Appl. Ergon. 2018, 68, 230–239. [Google Scholar] [CrossRef]
- Waongenngarm, P.; van der Beek, A.J.; Akkarakittichoke, N.; Janwantanakul, P. Effects of an active break and postural shift inter-vention on preventing neck and low-back pain among high-risk office workers: A 3-arm cluster-randomized controlled trial. Scand J. Work Environ. Health 2021, 47, 306–317. [Google Scholar] [CrossRef]
- Gore, M.; Tai, K.S.; Sadosky, A.; Leslie, D.; Stacey, B.R. Use and costs of prescription medications and alternative treatments in patients with osteoarthritis and chronic low back pain in community—Based settings. Pain Pract. 2012, 12, 550–560. [Google Scholar] [CrossRef] [PubMed]
- Olafsson, G.; Jonsson, E.; Fritzell, P.; Hägg, O.; Borgström, F. A health economic lifetime treatment pathway model for low back pain in Sweden. J. Med. Econ. 2017, 20, 1281–1289. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.-W.; Tetzlaff, J.M.; Altman, D.G.; Laupacis, A.; Gøtzsche, P.C.; Krleža-Jerić, K.; Hróbjartsson, A.; Mann, H.; Dickersin, K.; Berlin, J.A. SPIRIT 2013 statement: Defining standard protocol items for clinical trials. Ann. Intern. Med. 2013, 158, 200–207. [Google Scholar] [CrossRef]
- Butcher, N.J.; Monsour, A.; Mew, E.J.; Chan, A.W.; Moher, D.; Mayo-Wilson, E.; Terwee, C.B.; Chee-A-Tow, A.; Baba, A.; Gavin, F.; et al. Guidelines for Reporting Outcomes in Trial Reports: The CONSORT-Outcomes 2022 Extension. JAMA 2022, 328, 2252–2264. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. JAMA J. Am. Med. Assoc. 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. J. Am. Acad. Orthop. Surgeons. Glob. Res. Rev. 2018, 2, e088. [Google Scholar] [CrossRef]
- McCaffery, M.; Beebe, A. Pain. Clinical Manual for Nursing Practice; CV Mosby Co.: St. Louis, MI, USA, 1989; p. 2012. [Google Scholar]
- Lamba, D.; Upadhyay, R.K. Comparison between modified oswestry low back pain disability questionnaire and aberdeen low back pain scale taking low back-specific version of the sf-36 physical functioning scale as a gold standard in patients with low back pain. Asian J. Pharm. Clin. Res. 2018, 11, 97–99. [Google Scholar] [CrossRef]
- Fairbank, J. Revised Oswestry disability questionnaire. Spine 2000, 25, 2552. [Google Scholar] [CrossRef]
- Borg, G. Escalamiento psicofísico con aplicaciones en el trabajo físico y la percepción del esfuerzo. Scand J. Work Environ. Health 1990, 16, 55–58. [Google Scholar] [CrossRef]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Ostelo, R.W.; de Vet, H.C.; Vlaeyen, J.W.; Kerckhoffs, M.R.; Berfelo, W.M.; Wolters, P.M.; van den Brandt, P.A. Behavioral graded activity following first-time lumbar disc surgery: 1-year results of a randomized clinical trial. Spine 2003, 28, 1757–1765. [Google Scholar] [CrossRef] [PubMed]
- Meisingset, I.; Stensdotter, A.K.; Woodhouse, A.; Vasseljen, O. Predictors for global perceived effect after physiotherapy in patients with neck pain: An observational study. Physiotherapy 2018, 104, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Bileviciute-Ljungar, I.; Norrefalk, J.-R.; Borg, K. Pain burden in post-COVID-19 syndrome following mild COVID-19 infection. J. Clin. Med. 2022, 11, 771. [Google Scholar] [CrossRef]
- Waongenngarm, P.; Rajaratnam, B.S.; Janwantanakul, P. Perceived body discomfort and trunk muscle activity in three prolonged sitting postures. J. Phys. Ther. Sci. 2015, 27, 2183–2187. [Google Scholar] [CrossRef]
- Jia, B.; Nussbaum, M.A. Influences of continuous sitting and psychosocial stress on low back kinematics, kinetics, discomfort, and localized muscle fatigue during unsupported sitting activities. Ergonomics 2018, 61, 1671–1684. [Google Scholar] [CrossRef]
- Juraida, A. Effects of Netbook and Tablet Usage Postures on the Development of Fatigue, Discomfort and Pain. J. Eng. Technol. Sci. 2016, 48, 243–253. [Google Scholar]
- Roffey, D.M.; Wai, E.K.; Bishop, P.; Kwon, B.K.; Dagenais, S. Causal assessment of occupational standing or walking and low back pain: Results of a systematic review. Spine J. 2010, 10, 262–272. [Google Scholar] [CrossRef]
- Lis, A.M.; Black, K.M.; Korn, H.; Nordin, M. Association between sitting and occupational LBP. Eur. Spine J. 2007, 16, 283–298. [Google Scholar] [CrossRef]
- Gupta, N.; Christiansen, C.S.; Hallman, D.M.; Korshøj, M.; Carneiro, I.G.; Holtermann, A. Is objectively measured sitting time associated with low back pain? A cross-sectional investigation in the NOMAD study. PLoS ONE 2015, 10, e0121159. [Google Scholar] [CrossRef] [PubMed]
- Kourtis, D.; Magnusson, M.L.; Smith, F.; Hadjipavlou, A.; Pope, M.H. Spine height and disc height changes as the effect of hyperextension using stadiometry and MRI. Iowa Orthop. J. 2004, 24, 65. [Google Scholar] [PubMed]
- Sheahan, P.J.; Diesbourg, T.L.; Fischer, S.L. The effect of rest break schedule on acute low back pain development in pain and non-pain developers during seated work. Appl. Ergon. 2016, 53, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Waongenngarm, P.; van der Beek, A.J.; Akkarakittichoke, N.; Janwantanakul, P. Perceived musculoskeletal discomfort and its association with postural shifts during 4-h prolonged sitting in office workers. Appl. Ergon. 2020, 89, 103225. [Google Scholar] [CrossRef]
| Enrollment | Before Intervention | Randomization | Intervention | |
|---|---|---|---|---|
| Timepoint | 1st month | 2nd month | 2nd month | 3rd, 4th, and 5th months (12 weeks) |
| Enrollment | ||||
| Eligibility pre-screening | + | |||
| Informed consent | + | |||
| Allocation | + | |||
| Interventions | ||||
| Active break group and control group | + | |||
| Assessments | ||||
| Pain intensity | + | + | ||
| Disability index | + | + | ||
| Perceived musculoskeletal discomfort | + | + | ||
| The Global Perceived Effect | + | |||
| Post-Intervention Questionnaire | + |
| Exercises | Duration | ||
|---|---|---|---|
| Phase 1—1st month |
| 30 s |  |
|  | ||
|  | ||
| Phase 2—2nd month |
| 45 s |  |
|  | ||
|  | ||
|  | ||
| Phase 3—3rd month |
| 60 s |  |
|  | ||
|  | ||
|  | ||
|  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plandowska, M.; Labecka, M.K.; Truszczyńska-Baszak, A.; Płaszewski, M.; Rajabi, R.; Makaruk, B.; Różańska, D. The Effect of an Active Break Intervention on Nonspecific Low Back Pain and Musculoskeletal Discomfort during Prolonged Sitting among Young People—Protocol for a Randomized Controlled Trial. J. Clin. Med. 2024, 13, 612. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm13020612
Plandowska M, Labecka MK, Truszczyńska-Baszak A, Płaszewski M, Rajabi R, Makaruk B, Różańska D. The Effect of an Active Break Intervention on Nonspecific Low Back Pain and Musculoskeletal Discomfort during Prolonged Sitting among Young People—Protocol for a Randomized Controlled Trial. Journal of Clinical Medicine. 2024; 13(2):612. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm13020612
Chicago/Turabian StylePlandowska, Magdalena, Marta Kinga Labecka, Aleksandra Truszczyńska-Baszak, Maciej Płaszewski, Reza Rajabi, Beata Makaruk, and Dorota Różańska. 2024. "The Effect of an Active Break Intervention on Nonspecific Low Back Pain and Musculoskeletal Discomfort during Prolonged Sitting among Young People—Protocol for a Randomized Controlled Trial" Journal of Clinical Medicine 13, no. 2: 612. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm13020612