Transitioning of Helicobacter pylori Therapy from Trial and Error to Antimicrobial Stewardship
Abstract
:1. Introduction
2. Antimicrobial Stewardship in Traditional Infectious Disease Therapy
3. Original Development of H. pylori Antimicrobial Therapies
4. Development of H. pylori Therapies with Different Antibiotics
5. The Effect of Gastroenterology Rather Than Infectious Disease Being Responsible for Development of H. pylori Therapies
6. Meta-Analysis and H. pylori Therapy
7. The Role of Pharmaceutical Companies in Developing H. pylori Therapy
8. The Role of the U.S. Food and Drug Administration
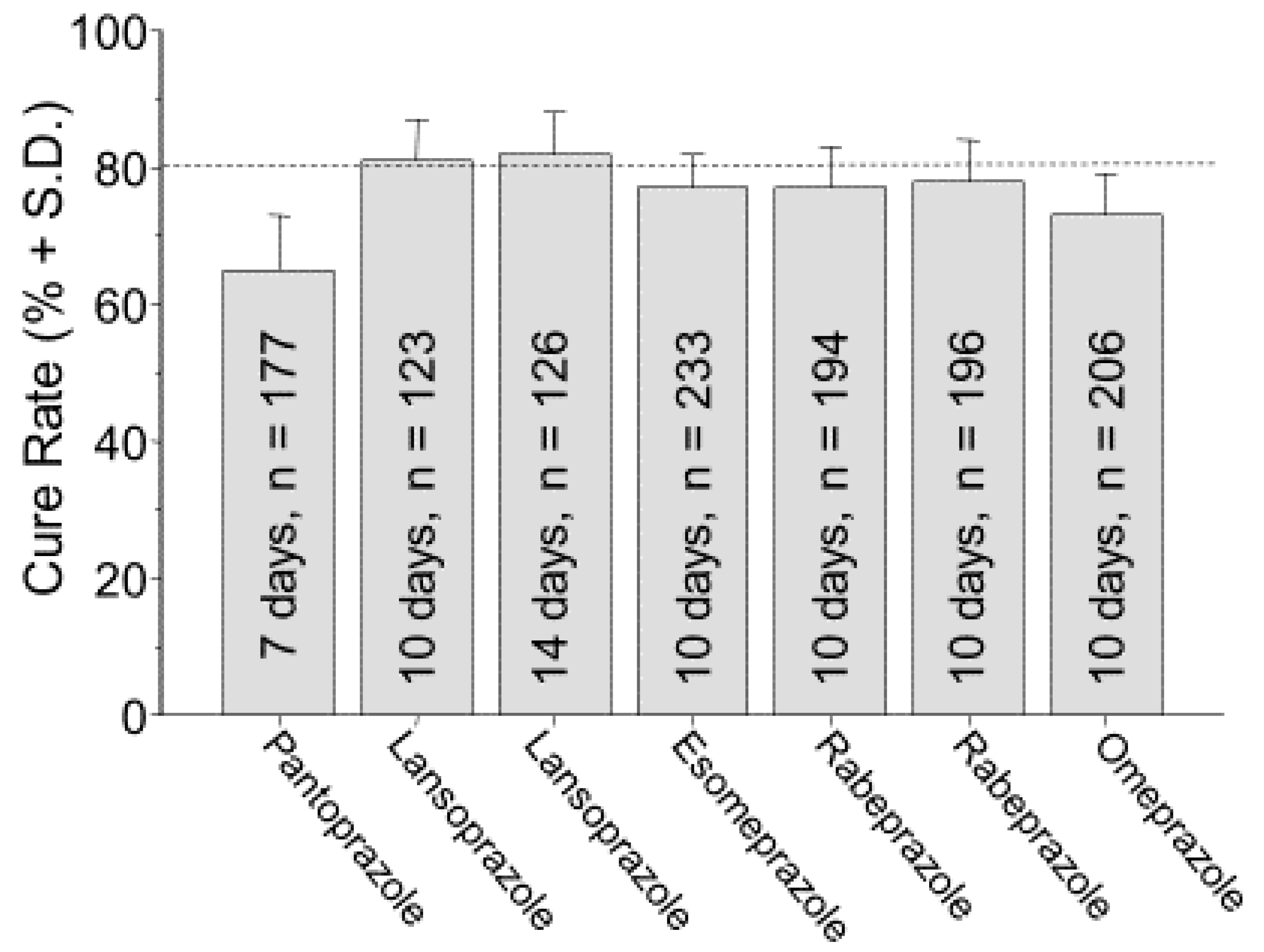
9. Basis for the General Recommendation for a Treatment Duration of 14 Days
10. Optimization: Duration of Therapy
11. Poly-Antimicrobial Therapies
12. Requirements and Impediments for Transition of H. pylori Therapy to the Principles of Antimicrobial Stewardship
13. Adoption of the Principles of Antimicrobial Stewardship
14. Proposal Regarding How to Improve Empiric Therapies While Introducing Antimicrobial Stewardship
Funding
Conflicts of Interest
Support
References
- Hulscher, M.E.J.L.; Prins, J.M. Antibiotic stewardship: Does it work in hospital practice? A review of the evidence base. Clin. Microbiol. Infect. 2017, 23, 799–805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charani, E.; Holmes, A. Antibiotic Stewardship-Twenty Years in the Making. Antibiotics 2019, 8, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugano, K.; Tack, J.; Kuipers, E.J.; Graham, D.Y.; El-Omar, E.M.; Miura, S.; Haruma, K.; Asaka, M.; Uemura, N.; Malfertheiner, P. Kyoto global consensus report on Helicobacter pylori gastritis. Gut 2015, 64, 1353–1367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, D.Y.; Dore, M.P. Helicobacter pylori therapy: A paradigm shift. Expert. Rev. Anti Infect. Ther. 2016, 14, 577–585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geisler, W.M.; Uniyal, A.; Lee, J.Y.; Lensing, S.Y.; Johnson, S.; Perry, R.C.; Kadrnka, C.M.; Kerndt, P.R. Azithromycin versus Doxycycline for Urogenital Chlamydia trachomatis Infection. N. Engl. J. Med. 2015, 373, 2512–2521. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, K.G.; Erbelding, E.J.; Cheng, W.W.; Rompalo, A.M. Doxycycline compared with benzathine penicillin for the treatment of early syphilis. Clin. Infect. Dis. 2006, 42, e45–e49. [Google Scholar] [CrossRef] [Green Version]
- Riedner, G.; Rusizoka, M.; Todd, J.; Maboko, L.; Hoelscher, M.; Mmbando, D.; Samky, E.; Lyamuya, E.; Mabey, D.; Grosskurth, H.; et al. Single-dose azithromycin versus penicillin G benzathine for the treatment of early syphilis. N. Engl. J. Med. 2005, 353, 1236–1244. [Google Scholar] [CrossRef] [Green Version]
- Olga, P.; Nyssen, O.P.; Bordin, D.; Tepes, B.; Pérez-Aisa, A.; Vaira, D. European Registry on Helicobacter pylori management (Hp-EuReg): Patterns and trends in first-line empirical eradication prescription and outcomes of 5 years and 21,533 patients. Gut 2020, in press. [Google Scholar]
- McNulty, C.A.; Dent, J.; Wise, R. Susceptibility of clinical isolates of Campylobacter pyloridis to 11 antimicrobial agents. Antimicrob. Agents Chemother. 1985, 28, 837–838. [Google Scholar] [CrossRef] [Green Version]
- Borsch, G.M.; Graham, D.Y. Helicobacter pylori. In Pharmacology of Peptic Ulcer Disease, Handbook of Experimental Pharmacology Volume 99; Collen, M.J., Benjamin, S.B., Eds.; Springer: Berlin, Germany, 1991; pp. 107–148. [Google Scholar]
- George, L.L.; Borody, T.J.; Andrews, P.; Devine, M.; Moore Jones, D.; Walton, M.; Brandl, S. Cure of duodenal ulcer after eradication of Helicobacter pylori. Med. J. Aust. 1990, 153, 145–149. [Google Scholar] [CrossRef]
- Graham, D.Y.; Lew, G.M.; Klein, P.D.; Evans, D.G.; Evans, D.J., Jr.; Saeed, Z.A.; Malaty, H.M. Effect of treatment of Helicobacter pylori infection on the long- term recurrence of gastric or duodenal ulcer. A randomized, controlled study. Ann. Intern. Med. 1992, 116, 705–708. [Google Scholar] [CrossRef]
- Graham, D.Y.; Lee, S.Y. How to effectively use bismuth quadruple therapy: The good, the bad, and the ugly. Gastroenterol. Clin. N. Am. 2015, 44, 537–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNulty, C.A.; Gearty, J.C.; Crump, B.; Davis, M.; Donovan, I.A.; Melikian, V.; Lister, D.M.; Wise, R. Campylobacter pyloridis and associated gastritis: Investigator blind, placebo controlled trial of bismuth salicylate and erythromycin ethylsuccinate. Br. Med. J. (Clin. Res. Ed.) 1986, 293, 645–649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peterson, W.L.; Graham, D.Y.; Marshall, B.; Blaser, M.J.; Genta, R.M.; Klein, P.D.; Stratton, C.W.; Drnec, J.; Prokocimer, P.; Siepman, N. Clarithromycin as monotherapy for eradication of Helicobacter pylori: A randomized, double-blind trial. Am. J. Gastroenterol. 1993, 88, 1860–1864. [Google Scholar] [PubMed]
- Al-Assi, M.T.; Genta, R.M.; Karttunen, T.J.; Graham, D.Y. Clarithromycin-amoxycillin therapy for Helicobacter pylori infection. Aliment. Pharmacol. Ther. 1994, 8, 453–456. [Google Scholar] [CrossRef]
- Prevacid (Lansoprazole) Lable, FDA Full Prescribing Information [Online]. 2012. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020406s078-021428s025lbl.pdf (accessed on 16 September 2020).
- Graham, D.Y.; Dore, M.P.; Lu, H. Understanding treatment guidelines with bismuth and non-bismuth quadruple Helicobacter pylori eradication therapies. Expert Rev. Anti Infect. Ther. 2018, 16, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Dore, M.P.; Lu, H.; Graham, D.Y. Role of bismuth in improving Helicobacter pylori eradication with triple therapy. Gut 2016, 65, 870–878. [Google Scholar] [CrossRef]
- Unge, P.; Gad, A.; Gnarpe, H.; Olsson, J. Does omeprazole improve antimicrobial therapy directed towards gastric Campylobacter pylori in patients with antral gastritis? A pilot study. Scand. J. Gastroenterol. Suppl. 1989, 167, 49–54. [Google Scholar] [CrossRef]
- Yang, J.C.; Lin, C.J.; Wang, H.L.; Chen, J.D.; Kao, J.Y.; Shun, C.T.; Lu, C.W.; Lin, B.R.; Shieh, M.J.; Chang, M.C.; et al. High-dose dual therapy is superior to standard first-line or rescue therapy for Helicobacter pylori infection. Clin. Gastroenterol. Hepatol. 2015, 13, 895–905. [Google Scholar] [CrossRef] [Green Version]
- Furuta, T.; Yamade, M.; Kagami, T.; Uotani, T.; Suzuki, T.; Higuchi, T.; Tani, S.; Hamaya, Y.; Iwaizumi, M.; Miyajima, H.; et al. Dual Therapy with Vonoprazan and Amoxicillin Is as Effective as Triple Therapy with Vonoprazan, Amoxicillin and Clarithromycin for Eradication of Helicobacter pylori. Digestion 2019, 1–9. [Google Scholar] [CrossRef]
- Graham, D.Y.; Dore, M.P. Update on the use of vonoprazan: A competitive acid blocker. Gastroenterology 2018, 154, 462–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, D.Y. Efficient identification and evaluation of effective Helicobacter pylori therapies. Clin. Gastroenterol. Hepatol. 2009, 7, 145–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, D.Y. Helicobacter pylori eradication therapy research: Ethical issues and description of results. Clin. Gastroenterol. Hepatol. 2010, 8, 1032–1036. [Google Scholar] [CrossRef]
- Laheij, R.J.; Rossum, L.G.; Jansen, J.B.; Straatman, H.; Verbeek, A.L. Evaluation of treatment regimens to cure Helicobacter pylori infection- a meta-analysis. Aliment. Pharmacol. Ther. 1999, 13, 857–864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janssen, M.J.; Van Oijen, A.H.; Verbeek, A.L.; Jansen, J.B.; de Boer, W.A. A systematic comparison of triple therapies for treatment of Helicobacter pylori infection with proton pump inhibitor/ranitidine bismuth citrate plus clarithromycin and either amoxicillin or a nitroimidazole. Aliment. Pharmacol. Ther. 2001, 15, 613–624. [Google Scholar] [CrossRef]
- Zullo, A.; De, F.V.; Hassan, C.; Morini, S.; Vaira, D. The sequential therapy regimen for Helicobacter pylori eradication: A pooled-data analysis. Gut 2007, 56, 1353–1357. [Google Scholar] [CrossRef] [Green Version]
- Gatta, L.; Vakil, N.; Vaira, D.; Scarpignato, C. Global eradication rates for Helicobacter pylori infection: Systematic review and meta-analysis of sequential therapy. BMJ 2013, 347, f4587. [Google Scholar] [CrossRef] [Green Version]
- Graham, D.Y. Illusions regarding Helicobacter pylori clinical trials and treatment guidelines. Gut 2017, 66, 2043–2046. [Google Scholar] [CrossRef]
- Graham, D.Y.; Tansel, A. Interchangeable use of proton pump inhibitors based on relative potency. Clin. Gastroenterol. Hepatol. 2018, 6, 800–808. [Google Scholar] [CrossRef]
- Infectious Diseases Society of America (IDSA). White paper: Recommendations on the conduct of superiority and organism-specific clinical trials of antibacterial agents for the treatment of infections caused by drug-resistant bacterial pathogens. Clin. Infect. Dis. 2012, 55, 1031–1046. [Google Scholar] [CrossRef] [Green Version]
- Chey, W.D.; Leontiadis, G.I.; Howden, C.W.; Moss, S.F. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am. J. Gastroenterol. 2017, 112, 212–239. [Google Scholar] [CrossRef] [PubMed]
- Graham, D.Y.; El-Serag, H.B. The European registry on Helicobacter pylori management shows that Gastroenterology has largely failed in its efforts to guide practitioners. Gut 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- European Helicobacter Pylori Study Group. Current European concepts in the management of Helicobacter pylori infection. The Maastricht Consensus Report. Gut 1997, 41, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Lam, S.K.; Talley, N.J. Report of the 1997 Asia Pacific Consensus Conference on the management of Helicobacter pylori infection. J. Gastroenterol. Hepatol. 1998, 13, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bochenek, W.J.; Peters, S.; Fraga, P.D.; Wang, W.; Mack, M.E.; Osato, M.S.; El Zimaity, H.M.; Davis, K.D.; Graham, D.Y. Eradication of Helicobacter pylori by 7-Day Triple-Therapy Regimens Combining Pantoprazole with Clarithromycin, Metronidazole, or Amoxicillin in Patients with Peptic Ulcer Disease: Results of Two Double-Blind, Randomized Studies. Helicobacter 2003, 8, 626–642. [Google Scholar] [CrossRef]
- Fennerty, M.B.; Kovacs, T.O.; Krause, R.; Haber, M.; Weissfeld, A.; Siepman, N.; Rose, P. A comparison of 10 and 14 days of lansoprazole triple therapy for eradication of Helicobacter pylori. Arch. Intern. Med. 1998, 158, 1651–1656. [Google Scholar] [CrossRef] [Green Version]
- Vakil, N.; Lanza, F.; Schwartz, H.; Barth, J. Seven-day therapy for Helicobacter pylori in the United States. Aliment. Pharmacol. Ther. 2004, 20, 99–107. [Google Scholar] [CrossRef]
- Laine, L.; Frantz, J.E.; Baker, A.; Neil, G.A. A United States multicentre trial of dual and proton pump inhibitor-based triple therapies for Helicobacter pylori. Aliment. Pharmacol. Ther. 1997, 11, 913–917. [Google Scholar] [CrossRef]
- Prilosec (Omeprazole) Label, FDA Full Prescribing Information [Online]. 1909. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/019810s096lbl.pdf (accessed on 16 September 2020).
- Aciphex (Rabeprazole Sodium) Label, FDA Full Prescribing Information [Online]. 2014. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/020973s035204736s005lbl.pdf (accessed on 16 September 2020).
- Nexium (Esomprazole Magnesium) Label, FDA Full Prescribing Information [Online]. 2014. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/022101s014021957s017021153s050lbl.pdf (accessed on 16 September 2020).
- Helicac. FDA Full Prescribing Information 2008. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/050719s013lbl.pdf (accessed on 16 September 2020).
- Pylera. FDA Full Prescribing Information 2017. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/050786s016lbl.pdf (accessed on 16 September 2020).
- Graham, D.Y.; Shiotani, A. New concepts of resistance in the treatment of Helicobacter pylori infections. Nat. Clin. Pract. Gastroenterol. Hepatol. 2008, 5, 321–331. [Google Scholar] [CrossRef]
- Keren, I.; Kaldalu, N.; Spoering, A.; Wang, Y.; Lewis, K. Persister cells and tolerance to antimicrobials. FEMS Microbiol. Lett. 2004, 230, 13–18. [Google Scholar] [CrossRef] [Green Version]
- Lewis, K. Persister cells, dormancy and infectious disease. Nat. Rev. Microbiol. 2007, 5, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.; Weeks, D.; Melchers, K.; Sachs, G. The life and death of Helicobacter pylori. Gut 1998, 43 (Suppl. S1), S56–S60. [Google Scholar] [CrossRef] [PubMed]
- Sachs, G.; Weeks, D.L.; Melchers, K.; Scott, D.R. The gastric Biology of Helicobactor pylori. Annu. Rev. Physiol. 2003, 65, 349–369. [Google Scholar] [CrossRef] [PubMed]
- Graham, D.Y.; Lee, Y.C.; Wu, M.S. Rational Helicobacter pylori therapy: Evidence-based medicine rather than medicine-based evidence. Clin. Gastroenterol. Hepatol. 2014, 12, 177–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liou, J.M.; Chen, C.C.; Chen, M.J.; Chen, C.C.; Chang, C.Y.; Fang, Y.J.; Lee, J.Y.; Hsu, S.J.; Luo, J.C.; Chang, W.H.; et al. Sequential versus triple therapy for the first-line treatment of Helicobacter pylori: A multicentre, open-label, randomised trial. Lancet 2013, 381, 205–213. [Google Scholar] [CrossRef]
- Saad, R.J.; Schoenfeld, P.; Kim, H.M.; Chey, W.D. Levofloxacin-based triple therapy versus bismuth-based quadruple therapy for persistent Helicobacter pylori infection: A meta-analysis. Am. J. Gastroenterol. 2006, 101, 488–496. [Google Scholar] [CrossRef]
- Miehlke, S.; Krasz, S.; Schneider-Brachert, W.; Kuhlisch, E.; Berning, M.; Madisch, A.; Laass, M.W.; Neumeyer, M.; Jebens, C.; Zekorn, C.; et al. Randomized trial on 14 versus 7 days of esomeprazole, moxifloxacin, and amoxicillin for second-line or rescue treatment of Helicobacter pylori Iinfection. Helicobacter 2011, 16, 420–426. [Google Scholar] [CrossRef]
- Graham, D.Y. Hp-normogram (normo-graham) for assessing the outcome of H. pylori therapy: Effect of resistance, duration, and CYP2C19 genotype. Helicobacter 2015, 21, 85–90. [Google Scholar] [CrossRef]
- de Boer, W.A.; Driessen, W.M.; Potters, V.P.; Tytgat, G.N. Randomized study comparing 1 with 2 weeks of quadruple therapy for eradicating Helicobacter pylori. Am. J. Gastroenterol. 1994, 89, 1993–1997. [Google Scholar]
- de Boer, W.A.; Driessen, W.M.; Tytgat, G.N. Only four days of quadruple therapy can effectively cure Helicobacter pylori infection. Aliment. Pharmacol. Ther. 1995, 9, 633–638. [Google Scholar] [CrossRef]
- de Boer, W.A.; van Etten, R.J.; Schade, R.W.; Ouwehand, M.E.; Schneeberger, P.M.; Tytgat, G.N. 4-day lansoprazole quadruple therapy: A highly effective cure for Helicobacter pylori infection. Am. J. Gastroenterol. 1996, 91, 1778–1782. [Google Scholar] [PubMed]
- de Boer, W.A.; van Etten, R.J.; Lai, J.Y.; Schneeberger, P.M.; van de Wouw, B.A.; Driessen, W.M. Effectiveness of quadruple therapy using lansoprazole, instead of omeprazole, in curing Helicobacter pylori infection. Helicobacter 1996, 1, 145–150. [Google Scholar] [CrossRef] [PubMed]
- El-Serag, H.B.; Kao, J.Y.; Kanwal, F.; Gilger, M.; LoVecchio, F.; Moss, S.F.; Crowe, S.; Elfant, A.; Haas, T.; Hapke, R.J.; et al. Houston Consensus Conference on testing for Helicobacter pylori infection in the United States. Clin. Gastroenterol. Hepatol. 2018, 16, 992–1002. [Google Scholar] [CrossRef] [Green Version]
- Malfertheiner, P.; Megraud, F.; O’Morain, C.A.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.T.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut 2017, 66, 6–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fallone, C.A.; Chiba, N.; van Zanten, S.V.; Fischbach, L.; Gisbert, J.P.; Hunt, R.H.; Jones, N.L.; Render, C.; Leontiadis, G.I.; Moayyedi, P.; et al. The Toronto Consensus for the Treatment of Helicobacter pylori Infection in Adults. Gastroenterology 2016, 151, 51–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howden, C.W.; Hunt, R.H. Guidelines for the management of Helicobacter pylori infection. Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology. Am. J. Gastroenterol. 1998, 93, 2330–2338. [Google Scholar] [CrossRef] [PubMed]
- Osato, M.S.; Graham, D.Y. Etest for metronidazole susceptibility in H. pylori: Use of the wrong standard may have led to the wrong conclusion. Am. J. Gastroenterol. 2004, 99, 769. [Google Scholar] [CrossRef] [PubMed]
- Osato, M.S.; Reddy, R.; Reddy, S.G.; Penland, R.L.; Graham, D.Y. Comparison of the Etest and the NCCLS-approved agar dilution method to detect metronidazole and clarithromycin resistant Helicobacter pylori. Int. J. Antimicrob. Agents 2001, 17, 39–44. [Google Scholar] [CrossRef]
- Nyssen, O.P.; McNicholl, A.G.; Gisbert, J.P. Meta-analysis of three-in-one single capsule bismuth-containing quadruple therapy for the eradication of Helicobacter pylori. Helicobacter 2019, 24, e12570. [Google Scholar] [CrossRef] [PubMed]
- Nyssen, O.P.; Perez-Aisa, A.; Rodrigo, L.; Castro, M.; Mata, R.P.; Ortuno, J.; Barrio, J.; Huguet, J.M.; Modollel, I.; Alcaide, N.; et al. Bismuth quadruple regimen with tetracycline or doxycycline versus three-in-one single capsule as third-line rescue therapy for Helicobacter pylori infection: Spanish data of the European Helicobacter pylori Registry (Hp-EuReg). Helicobacter 2020, e12722. [Google Scholar] [CrossRef]
- Shiotani, A.; Lu, H.; Dore, M.P.; Graham, D.Y. Treating Helicobacter pylori effectively while minimizing misuse of antibiotics. Cleve. Clin. J. Med. 2017, 84, 310–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dang, B.N.; Graham, D.Y. Helicobacter pylori infection and antibiotic resistance: A WHO high priority? Nat. Rev. Gastroenterol. Hepatol. 2017, 7, 383–384. [Google Scholar] [CrossRef] [PubMed]
- Riahizadeh, S.; Malekzadeh, R.; Agah, S.; Zendehdel, N.; Sotoudehmanesh, R.; Ebrahimi-Dariani, N.; Pourshams, A.; Vahedi, H.; Mikaeli, J.; Khatibian, M.; et al. Sequential metronidazole-furazolidone or clarithromycin-furazolidone compared to clarithromycin-based quadruple regimens for the eradication of Helicobacter pylori in peptic ulcer disease: A double-blind randomized controlled trial. Helicobacter 2010, 15, 497–504. [Google Scholar] [CrossRef] [PubMed]
- A Rule by the Centers for Medicare & Medicaid Services Federal Register [Online]. 2019. Available online: https://federalregister.gov/d/2019-20736 (accessed on 15 July 2020).
- Core Elements of Antibiotic Stewardship. Centers for Disease Control and Prevention [Online] 2019. Available online: https://www.cdc.gov/antibiotic-use/core-elements/resource-limited.html (accessed on 15 July 2020).
- Malfertheiner, P.; Megraud, F.; O’Morain, C.; Bazzoli, F.; El-Omar, E.; Graham, D.; Hunt, R.; Rokkas, T.; Vakil, N.; Kuipers, E.J. Current concepts in the management of Helicobacter pylori infection: The Maastricht III Consensus Report. Gut 2007, 56, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Malfertheiner, P.; Megraud, F.; O’Morain, C.A.; Atherton, J.; Axon, A.T.; Bazzoli, F.; Gensini, G.F.; Gisbert, J.P.; Graham, D.Y.; Rokkas, T.; et al. Management of Helicobacter pylori infection--the Maastricht IV/ Florence Consensus Report. Gut 2012, 61, 646–664. [Google Scholar] [CrossRef] [Green Version]
- Savoldi, A.; Carrara, E.; Graham, D.Y.; Conti, M.; Tacconelli, E. Prevalence of Antibiotic Resistance in Helicobacter pylori: A Systematic Review and Meta-analysis in World Health Organization Regions. Gastroenterology 2018, 155, 1372–1382. [Google Scholar] [CrossRef] [Green Version]
- Graham, D.Y.; Lu, H.; Shiotani, A. Vonoprazan-containing H, pylori triple therapy contributes to increasing global antimicrobial resistance. J. Gastroenterol. Hepatol. 2020, in press. [Google Scholar]

| Term | Definition |
|---|---|
| Successful | Excellent or good results |
| Excellent results | Reliably achieve 95% or greater cure rates in adherent patients with susceptible infections |
| Good results | Reliably achieve 90% or greater cure rates in adherent patients with susceptible infections |
| Optimum duration | Days of therapy required to reliably achieve good to excellent results |
| Doses and frequency of administration | Those that will reliably achieve good to excellent results |
|
|
|
|
|
|
| Sensitivity Pattern of H. pylori to Clarithromycin and Metronidazole | Prevalence of Pattern | Successful Treatment of H. pylori | Number of Ineffective Drugs Used | Number of Unnecessary Drugs Used | |
|---|---|---|---|---|---|
| Clarithromyin: Susceptible 80%; Resistant 20% | Metronidazole: Susceptible 60%; Resistant 40% | ||||
| Susceptible | Susceptible | 48% | Yes | 0 | 1 |
| Susceptible | Resistant | 32% | Yes | 1 | 1 |
| Resistant | Susceptible | 12% | Yes | 1 | 1 |
| Resistant | Resistant | 8% | No | 2 | 2 |
|
|
|
| Principle 1 Only regimens proven to reliably achieve high cure rates. |
| Principle 2 Routinely monitor and report outcomes using test-of-cure result to provide real-time information about whether the goals are being met. |
| Principle 3 Abandon or modify the therapies that fail to reliably achieve the desired high cure rates. |
|
|
|
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graham, D.Y. Transitioning of Helicobacter pylori Therapy from Trial and Error to Antimicrobial Stewardship. Antibiotics 2020, 9, 671. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9100671
Graham DY. Transitioning of Helicobacter pylori Therapy from Trial and Error to Antimicrobial Stewardship. Antibiotics. 2020; 9(10):671. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9100671
Chicago/Turabian StyleGraham, David Y. 2020. "Transitioning of Helicobacter pylori Therapy from Trial and Error to Antimicrobial Stewardship" Antibiotics 9, no. 10: 671. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9100671




