Toward Evaluation of the Subjective Experience of a General Class of User-Controlled, Robot-Mediated Rehabilitation Technologies for Children with Neuromotor Disability
Abstract
:1. Introduction
1.1. Objective
1.2. Research Question (RQ1)
- Existing theories of pediatric home exercise program adherence;
- Published criteria for gauging acceptance of game-mediated therapy in children; and
- A valid and reliable instrument for measuring subjective assessment of specifically robotic assistive and/or rehabilitative technologies (A/RT)
2. Materials and Methods
2.1. Procedure
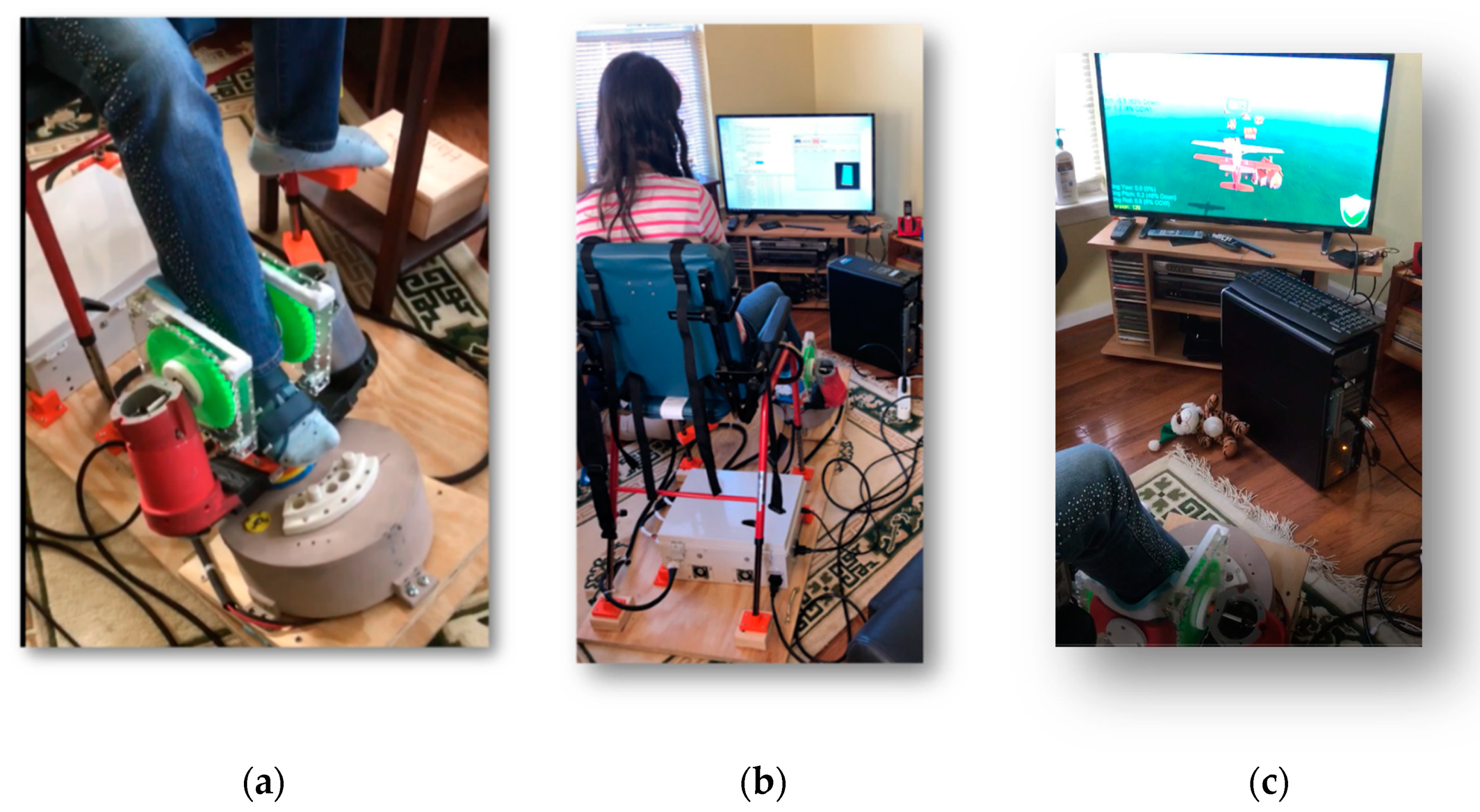
2.2. Participants and Setting
3. Results
3.1. Alignment of PedBotHome User Experience with HEP Adherence Theory in CP (RQ1a)
3.1.1. Fit of Exercise Program in the Home Environment
Exercise Equipment
What the Exercise Is
Perceived Effectiveness of Exercise
Comfort during Exercise
Perceived Complexity of Doing Exercise
Family Support or Disruption
Fun Doing Exercise
Time Exercises Take to Complete
Exercise Logbook
3.1.2. Therapist Support
Demonstrating Exercises
Coaching
Perceived Regular Monitoring
Giving Reminders
Identifying Changes in Child’s Performance
Providing Goal-Based Incentives
Providing Peace of Mind
Clinical, Regulatory, Engineering, and Commercial Product Domain Expert Advice on Role of Clinicians in Extending Therapy Provision Models
3.1.3. Personal Factors
Autonomy
Effort
Health
Motivation
Time Management
3.2. Alignment of PedBotHome Experience with Exergame Engagement Factors (RQ1b)
3.2.1. Enjoyment Overall
Overall Degree of Game Enjoyment/Fun
Difficulty/Ease of Playing
3.2.2. Physical Interface
Range of Motion and Hold Time Diminish Fun
Repetitions Do Not Diminish Fun
Game Controls Are Most Difficult to Get Positively Appraised
Being Comfortable While Playing
3.2.3. Game Scenario and Graphics
Visual Esthetic
Immersion in Game
Realism of Look and Feel of Game
Enjoyment of Game Scenario
3.2.4. Overall Competence and Control
Sense of Competence Playing Game
Sense of Control of Game
Challenge of Game
3.2.5. Incentive from Therapeutic Awareness
Perceived Therapeutic Function
Help Game Provides Correctly Doing Therapeutic Movements
Game Increased Motivation to Do Exercise
Game Spurred Child’s Initiative to Exercise
3.3. Alignment of PedBotHome Experience with Acceptance Factors Measured by the PYTHEIA (RQ1c)
3.3.1. Adaptability
3.3.2. Improvement to Everyday Life
3.3.3. Ease of Learning All Individual Functions (Item 3)
3.3.4. Ease of Learning All Basic Functions
3.3.5. Ease of Use (Complexity, Required Effort)
3.3.6. Security
3.3.7. Dimensions (Height, Width, Length)
3.3.8. Weight
3.3.9. Sufficiency of Functionality
3.3.10. Feeling Protected, Secure, Confident
3.3.11. Feeling More Autonomous
3.3.12. Needing Help from Another Person to Use
3.3.13. Comfort Using in the Community
3.3.14. Comfort Using around Colleagues (Working Environment)
3.3.15. Comfort Using around Friends and Family
3.3.16. Individual Functionalities, Item IF1, Ease of Use
3.3.17. Individual Functionalities, Item IF2, Help Provided in Everyday Life
3.3.18. Individual Functionalities, Item IF3, Safety, Security
3.3.19. Item IF4, Reliability
3.3.20. Item IF5, Feeling of Safety
4. Discussion
4.1. HEP Adherence Theory, the Experience of PedBotHome, and PYTHEIA Scale Alignment
4.1.1. Domain: Fit of Exercise in the Home Environment
4.1.2. Domain: Therapist Support
4.1.3. Domain: Personal Factors
4.2. Exergame Engagement Theory, the Experience of PedBotHome, and PYTHEIA Scale Alignment
4.2.1. Domain: Overall Enjoyment
4.2.2. Domain: Physical Interface
4.2.3. Game and Scenario Graphics
4.2.4. Overall Competence and Control
4.2.5. Incentive from Therapeutic Awareness
4.3. The PYTHEIA Scale: What Works for A/R Gamebot Assessment and What Might Be Improved
4.3.1. The Individual Functionalities (IF) Subscale and Evaluation of Functionality in General
- Item IF1 queries ease of use. This item is clear, whether the target functionality involves hardware or software.
- IF2 queries the help the specified functionality provides “in your everyday life”. Here an interpretation is needed. Two possible interpretations relative to the footplate are (1) how well is supports functional improvement by delivering appropriate exercise or (2) how well it works in controlling the game. These two “helps” may or may not align. Similarly, with respect to the airplane game, two possible ways it could be helpful in everyday life are (1) how generally entertaining the game is or (2) how much it helps engage the child in his/her HEP. These two options likely converge, but not necessarily. The question “Help what?” needs to be explicit to be sure all users are evaluating the same phenomenon.
- IF3 deals with safety and security. As noted, these factors are ambiguous in the context of a device such as an A/R gamebot. We know the hardware caused discomfort for some children in the PedBotHome pilot and this problem may map to IF5, the feeling of safety. It may also map to IF4, reliability: insecurity secondary to unreliable functioning. The item does not resonate when applied in the realm of software, i.e., The Airplane Game. The response in this latter case would be N/A.
- IF4, reliability, applies equally well to our selected hardware and software functionalities.
- IF5, finally, may make sense in the case of hardware strapped onto a child’s ankle but it does not in the case of software.
4.3.2. Personal Factors
4.3.3. Short-Term versus Longer-Term “Life Improvement”
4.3.4. Assistive Technology (AT) Operating at Two Conceptual Levels
4.3.5. Referents in the PYTHEIA That Do Not Align with Assistive Technology for Rehabilitation Conceptually
4.3.6. PYTHEIA Items to Carry Forward
4.3.7. Potentially Important Use Factors the PYTHEIA Does Not Measure
5. Limitations
6. Conclusions
7. Patents
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Oskoui, M.; Coutinho, F.; Dykeman, J.; Jetté, N.; Pringsheim, T. An update on the prevalence of cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2013, 55, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.R.; Neelakantan, M.; Pandher, K.; Merrick, J. Cerebral palsy in children: A clinical overview. Transl. Pediatr. 2020, 9, S125–S135. [Google Scholar] [CrossRef] [PubMed]
- Hutton, J.L.; Colver, A.F.; Mackie, P.C. Effect of severity of disability on survival in north east England cerebral palsy cohort. Arch. Dis. Child. 2000, 83, 468–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeffries, L.M.; LaForme Fiss, A.; Westcott McCoy, S.; Bartlett, D.; Avery, L.; Hanna, S. Developmental Trajectories and Reference Percentiles for Range of Motion, Endurance, and Muscle Strength of Children with Cerebral Palsy. Phys. Ther. 2019, 99, 329–338. [Google Scholar] [CrossRef]
- Gannotti, M.E. Coupling Timing of Interventions with Dose to Optimize Plasticity and Participation in Pediatric Neurologic Populations. Pediatr. Phys. Ther. 2017, 29, S37–S47. [Google Scholar] [CrossRef]
- Wiart, L.; Darrah, J.; Kembhavi, G. Stretching with children with cerebral palsy: What do we know and where are we going? Pediatr. Phys. Ther. 2008, 20, 173–178. [Google Scholar] [CrossRef]
- Pin, T.; Dyke, P.; Chan, M. The effectiveness of passive stretching in children with cerebral palsy. Dev. Med. Child Neurol. 2006, 48, 855–862. [Google Scholar] [CrossRef]
- O’Neil, M.E.; Fragala-Pinkham, M.A.; Westcott, S.L.; Martin, K.; Chiarello, L.A.; Valvano, J.; Rose, U.R. Physical therapy clinical management recommendations for children with cerebral palsy—Spastic diplegia: Achieving functional mobility outcomes. Pediatr. Phys. Ther. 2006, 18, 49–72. [Google Scholar] [CrossRef]
- Dodd, K.J.; Taylor, N.F.; Damiano, D.L. A systematic review of the effectiveness of strength-training programs for people with cerebral palsy. Arch. Phys. Med. Rehabil. 2002, 83, 1157–1164. [Google Scholar] [CrossRef] [Green Version]
- Aboutorabi, A.; Arazpour, M.; Ahmadi Bani, M.; Saeedi, H.; Head, J.S. Efficacy of ankle foot orthoses types on walking in children with cerebral palsy: A systematic review. Ann. Phys. Rehabil. Med. 2017, 60, 393–402. [Google Scholar] [CrossRef]
- Trabacca, A.; Vespino, T.; Di Liddo, A.; Russo, L. Multidisciplinary rehabilitation for patients with cerebral palsy: Improving long-term care. J. Multidiscip. Healthc. 2016, 9, 455–462. [Google Scholar] [CrossRef] [Green Version]
- Castelli, E.; Fazzi, E. Recommendations for the rehabilitation of children with cerebral palsy. Eur. J. Phys. Rehabil. Med. 2016, 52, 691–703. [Google Scholar] [PubMed]
- Taylor, N.F.; Dodd, K.J.; McBurney, H.; Gram, H.K. Factors influencing adherence to a home-based strength-training programme for young people with cerebral palsy. J. Physiother. 2004, 90, 57–63. [Google Scholar] [CrossRef]
- Lillo-Navarro, C.; Medina-Mirapeix, F.; Escolar-Reina, P.; Montilla-Herrador, J.; Gomez-Arnaldos, F.; Olivera-Sousa, S.L. Parents of children with physical disabilities perceive that characteristics of home exercise programs and physiotherapists’ teaching styles influence adherence: A qualitative study. J. Physiother. 2015, 61, 81–86. [Google Scholar] [CrossRef] [Green Version]
- Burdea, G.C.; Cioi, D.; Kale, A.; Janes, W.E.; Ross, S.A.; Engsberg, J.R. Robotics and Gaming to Improve Ankle Strength, Motor Control, and Function in Children With Cerebral Palsy—A Case Study Series. IEEE Trans. Neural Syst. Rehabil. Eng. 2013, 21, 165–173. [Google Scholar] [CrossRef] [Green Version]
- Monfaredi, R.; Fooladi, H.; Tabrizi, P.R.; Kovelman, S.; Salvador, T.; Coley, C.; Alyamani, S.; Pergami, P.; Cleary, K.; Evans, S. PedBot: Robotically assisted ankle robot and video game for children with neuromuscular disorders. In Proceedings of the SPIE Medical Imaging Conference 2018, Huston, TX, USA, 12–15 February 2018. [Google Scholar]
- Sukal-Moulton, T.; Clancy, T.; Zhang, L.-Q.; Gaebler-Spira, D. Clinical application of a robotic ankle training program for cerebral palsy compared to the research laboratory application: Does it translate to practice? Arch. Phys. Med. Rehabil. 2014, 95, 1433–1440. [Google Scholar] [CrossRef] [Green Version]
- Coley, C.; Belschner, J.; Kovelman, S.; Monfaredi, R.; Salvador, T.; Fooladi, H.; Monfaredi, R.; Salvador, T.; Schladen, M.; Alyamani, S. Use of a robot (PedBotHome) to increase compliance with home exercise program in children with static neurologic injury. In Proceedings of the ISPRM World Congress and AAP Annual Meeting, Orlando, FL, USA, 4–9 March 2020. [Google Scholar]
- Cleary, K.; Monfaredi, R.; Salvador, T.; Talari, H.; Coley, C.; Kovelman, S.; Belschner, J.; Alyamani, S.; Schladen, M.; Evans, S.H. PedBotHome: Robotically-assisted ankle rehabilitation system for children with cerebral palsy. In Proceedings of the IEEE International Conference on Rehabilitation Robotics, Toronto, ON, Canada, 24–28 June 2019. [Google Scholar]
- Chen, K.; Wu, Y.-N.; Ren, Y.; Liu, L.; Gaebler-Spira, D.; Tankard, K.; Lee, J.; Song, W.; Wang, M.; Zhang, L.-Q. Home-Based Versus Laboratory-Based Robotic Ankle Training for Children with Cerebral Palsy: A Pilot Randomized Comparative Trial. Arch. Phys. Med. Rehabil. 2016, 97, 1237–1243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopes, S.; Magalhães, P.; Pereira, A.; Martins, J.; Magalhães, C.; Chaleta, E.; Rosário, P. Games Used with Serious Purposes: A Systematic Review of Interventions in Patients with Cerebral Palsy. Front. Psychol. 2018, 9, 1712. [Google Scholar] [CrossRef] [Green Version]
- Falzarano, V.; Marini, F.; Morasso, P.; Zenzeri, J. Devices and Protocols for Upper Limb Robot-Assisted Rehabilitation of Children with Neuromotor Disorders. Appl. Sci. 2019, 9, 2689. [Google Scholar] [CrossRef] [Green Version]
- Peiris, V.; (U.S. Food and Drug Administration Center, Washington, DC, USA). Personal Communication, 2020.
- Cleary, K.; Evans, S.H.; Salvador, T.; Schladen, M.M.; Coley, C.; Kovelman, S.; Belschner, J.; Vinopol, C. PedBot: A Rehabilitative Ankle Robot [Presentation]; Children’s National Medical Center: Washington, DC, USA, 2020. [Google Scholar]
- Shelburne, N.; Oduye, A.; Williams, K.; Lou, E.; Litherland, C. Design Engineering Handbook; InVision: New York, NY, USA, 2020. [Google Scholar]
- Koumpouros, Y. A systematic review on existing measures for the subjective assessment of rehabilitation and assistive Robot Devices. J. Healthc. Eng. 2016. [Google Scholar] [CrossRef] [Green Version]
- What Is AT? Chicago, IL: Assistive Technology Industry Association (ATIA). Available online: https://www.atia.org/home/at-resources/what-is-at/ (accessed on 1 September 2020).
- Fasoli, S.E. Rehabilitation Technologies to Promote Upper Limb Recovery after Stroke. In Stroke Rehabilitation, 4th ed.; Gillen, G., Ed.; Mosby: Maryland Heights, MO, USA, 2016; pp. 486–510. [Google Scholar]
- Scherer, M.; Jutai, J.; Fuhrer, M.; Demers, L.; Deruyter, F. A framework for modelling the selection of assistive technology devices (ATDs). Disabil. Rehabil. Assist. Technol. 2007, 2, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Demers, L.; Monette, M.; Lapierre, Y.; Arnold, D.L.; Wolfson, C. Reliability, validity, and applicability of the Quebec User Evaluation of Satisfaction with assistive Technology (QUEST 2.0) for adults with multiple sclerosis. Disabil. Rehabil. 2002, 24, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Koumpouros, Y.; Papageorgiou, E.; Karavasili, A.; Koureta, F. PYTHEIA: A scale for assessing rehabilitation and assistive robotics. Int. J. Med. Health Biomed. Bioeng. Pharm. Eng. 2016, 10, 456–460. [Google Scholar]
- Schladen, M.M.; Koumpouros, Y.; Sandison, M.; Casas, R.; Lum, P. Conceptualization of Hand-TaPS to measure the subjective experience of dynamic hand orthoses in promoting functional recovery at home after stroke. Technol. Disabil. 2020. preprint. [Google Scholar] [CrossRef]
- Brancato, G.; Macchia, S.; Murgia, M.; Signore, M.; Simeoni, G.; Blanke, K.; Körner, T.; Nimmergut, A.; Lima, P.; Paulino, R.; et al. Handbook of Recommended Practices for Questionnaire Development and Testing in the European Statistical System; European Commission: Brussels, Belgium, 2006. [Google Scholar]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Anaysis: The Use of Factor Analysis for Instrument Development in Health Care Research; SAGE Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Sandlund, M.; Waterworth, E.L.; Hager, C.K. Using motion interactive games to promote physical activity and enhance motor performance in chldren with cerebral palsy. Dev. Neurorehabilit. 2011, 14, 15–21. [Google Scholar] [CrossRef] [Green Version]
- Whittinghill, D.M.; Brown, J.S. Gamification of physical therapy for treatment of pediatric cerebral palsy: A pilot study examining player preferences. In Proceedings of the 121st ASEE Annual Conference & Exposition, Indianapolis, IN, USA, 15–18 June 2014. [Google Scholar]
- Radtka, S.; Hone, R.; Brown, C.; Mastick, J.; Melnick, M.E.; Dowling, G.A. Feasibility of computer-based videogame therapy for children with cerebral palsy. Games Health J. 2013, 2, 222–228. [Google Scholar] [CrossRef] [Green Version]
- Freitas, D.Q.; Da Gama, A.E.F.; Figueiredo, L.; Chaves, T.M.; Marques-Olivera, D.; Teichrieb, V.; Cristiano, A. Development and evaluation of a kinect based motor rehabilitation game. In Proceedings of the XI SBGames, Brasilia, Brazil, 2–4 November 2012; pp. 144–153. [Google Scholar]
- Bryanton, C.; Bosse, J.; Brien, M.; McLean, J.; McCormick, A.; Sviestrup, H. Feasibility, motivation, and selective motor control: Virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol. Behav. 2006, 9, 123–128. [Google Scholar] [CrossRef] [Green Version]
- Rosenbaum, P.L.; Palisano, R.J.; Bartlett, D.J.; Galuppi, B.E.; Russell, D.J. Development of the Gross Motor Function Classification System for cerebral palsy. Dev. Med. Child Neurol. 2008, 50, 249–253. [Google Scholar] [CrossRef]
- Ose Askvik, E.; van der Weel, F.R.R.; van der Meer, A.L.H. The Importance of Cursive Handwriting over Typewriting for Learning in the Classroom: A High-Density EEG Study of 12-Year-Old Children and Young Adults. Front. Psychol. 2020, 11, 1810. [Google Scholar] [CrossRef]
- Abuhamdeh, S. Investigating the “Flow” Experience: Key Conceptual and Operational Issues. Front. Psychol. 2020, 11, 158. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Towards a Common Language for Functioning, Disability, and Health; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Cowan, R.E.; Fregly, B.J.; Boninger, M.L.; Chan, L.; Rodgers, M.M.; Reinkensmeyer, D.J. Recent trends in assistive technology for mobility. J. Neuroeng. Rehabil. 2012, 9, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Djulbegovic, B.; Hozo, I.; Ioannidis, J. Modern health care as a game theory problem. Eur. J. Clin. Investig. 2015, 45, 1–12. [Google Scholar] [CrossRef] [PubMed]



| Logic Model: A/R Gamebot Subjective Evaluation Instrument Conceptualization | ||
|---|---|---|
| Activity | Inputs to Instrument Conceptualization | Outputs Identified for Initial Item Generation |
| Literature Review | Home Exercise Program Adherence Theory |
|
| Games Used Seriously—Theories of Use and Effect | ||
| A/RT Instrument Review | PYTHEIA—Validated Scale for Measuring Explicitly Robotic Assistive and Rehabilitative Technologies | |
| Family User Interviews | Eight families (9 children, eight parents) participating in 28-day home pilot of PedBotHome A/R Gamebot prototype | |
| Clinical, Engineering, Regulatory Expert Consultations | In conjunction with grantor-sponsored program to explore mechanisms of technology transfer | |
| Participant | GMFCS Level | Age | Sex | Facilitating Parent | Number of Days Played (Out of 28) |
|---|---|---|---|---|---|
| 1 | 2 | 15 | female | mother | 27 |
| 2 | 1 | 13 | female | mother | 19 |
| 3 | 2 | 16 | male | father | 28 |
| 4 | 2 | 16 | female | father | 24 |
| 5 | 2 | 10 | female | mother | 5 * |
| 6 | 1 | 9 | female | mother | 21 |
| 7 | 1 | 11 | female | mother | 17 |
| 8 | 2 | 13 | female | father | 7 + |
| THEORY 1 [12] | THEORY 2 [13] | Adherence Factors (Synthesis) | Alignment with PedBotHome Experience | Alignment with PYTHEIA Scale Items |
|---|---|---|---|---|
| Fit of Exercise Program in the Home Environment | ||||
| x | Exercise Equipment | Aligned | Aligned. Similarly, the technology itself is focal. | |
| x | What the Exercise Is | Aligned | Aligned. Responsive to Individual Functionalities flexibility. | |
| x | Perceived Effectiveness of Exercise | Aligned | Aligned. Contribution to improvement to one’s everyday life (item 2). | |
| x | Comfort During Exercise | Aligned | Not clearly aligned. Potentially implicit in items 2 and 10. Items 12–15 deal with specifically social comfort. | |
| x | Perceived Complexity of Doing Exercise | Aligned | Aligned. Item 5, ease of use (complexity, required effort) | |
| x | x | Family Support or Disruption | Aligned | Aligned. Item 11, autonomy and Item 12, needing help from another. |
| x | Fun Doing Exercise | Aligned | Not clearly aligned. Results from ambiguity of interpretation of item 2, improvement to everyday life. Need to distinguish short-term improvement (in-game fun) from longer-term, therapeutic outcome improvement. | |
| x | x | Time Exercises Take to Complete | Aligned | Not aligned. No explicit time component in the PYTHEIA. |
| x | Exercise Logbook | Ambiguous | Further exploration needed. PedBotHome system log not presently accessible to the user. Conceivably, a logbook function could be an Individual Functionality. | |
| Therapist Support | ||||
| x | x | Demonstrating Exercises | Not aligned | Aligned. Item 12, needing help from another; implicitly, the ease of learning items, 3 and 4. |
| x | x | Coaching | Not aligned | Aligned. Item 12, needing help from another; implicitly, the ease of learning items, 3 and 4. |
| x | Perceived Regular Monitoring | Not aligned | Not aligned. No items measure monitoring. | |
| x | Giving Reminders | Not aligned | Aligned. Item 1, adaptability. Items 11 and 12, autonomy and needing help respectively. | |
| x | Identifying Changes in Child’s Exercise Performance | Not aligned | Ambiguous. Item 2 pertains but improvements identified NOT through therapist but through change in game performance (score) and/or subjective experience in physical activity. | |
| x | Providing Goal-based incentives | Not aligned | Ambiguous. As immediately above. | |
| x | Providing Peace of mind | Not aligned | Not aligned | |
| Personal Factors | ||||
| x | Autonomy | Aligned | Not Aligned. Item 11, autonomy, has opposite directionality. | |
| x | Effort | Aligned | Not aligned. Item 5, ease of use (complexity, required effort) pertains to interaction with the device, not to personal satisfaction in putting forth effort. | |
| x | Health | Aligned | Not aligned. Health factors not addressed by PYTHEIA scale. | |
| x | Motivation | Aligned | Not aligned. Personal factors not addressed by PYTHEIA scale. | |
| x | Time Management | Aligned | Not aligned. No explicit time component in the PYTHEIA. | |
| Item | Dimension | Acceptance Factors | R, Item/Total Score Correlation | Alignment with PedBotHome Experience |
|---|---|---|---|---|
| 1 | Fit to Use | Adaptability to the spaces where one spends one’s everyday life (home, work) | 0.724 | Aligned |
| 2 | Fit to Use | Contribution to the improvement to one’s everyday life | 0.695 | Aligned (dual interpretation) |
| 3 | Ease of Use | Ease of learning all individual functions | 0.354 | Aligned (ambiguity noted) |
| 4 | Ease of Use | Ease of learning the basic functions (the functions that concern the individual more) | 0.518 | Aligned (ambiguity noted) |
| 5 | Ease of Use | Ease of use (complexity, required effort) | 0.485 | Aligned |
| 6 | Fit to Use | Security | 0.681 | Ambiguous |
| 7 | Fit to Use | Dimensions (height, width, length) | 0.633 | Aligned |
| 8 | Fit to Use | Weight | 0.614 | Aligned |
| 9 | Fit to Use | Sufficiency of functionality | 0.465 | Aligned |
| 10 | Fit to Use | Feeling protected, secure, confident | 0.600 | Ambiguous |
| 11 | Ease of Use | Feeling more autonomous | 0.628 | Aligned |
| 12 | Ease of Use | Needing help from another person to use | 0.612 | Aligned |
| 13 | Fit to Use | I will feel comfortable to use the assistive device around the community. | 0.655 | Not aligned |
| 14 | Ease of Use | Feeling comfortable using around colleagues (working environment) | 0.732 | Not aligned |
| 15 | Fit to Use | Feeling comfortable using around friends and family | 0.719 | Aligned |
| IF1 | Individual Functionalities | Ease of use | 0.946 | Aligned |
| IF2 | Individual Functionalities | Help provided in everyday life | 0.991 | Aligned (dual interpretation) |
| IF3 | Individual Functionalities | Safety, security | 0.993 | Ambiguous |
| IF4 | Individual Functionalities | Reliability | 0.991 | Aligned |
| IF5 | Individual Functionalities | Feeling of safety | 0.996 | Ambiguous |
| Exergame Engagement Factors | Studies Reporting | Alignment with PedBotHome Experience | Alignment (Tentative) with PYTHEIA Scale Items |
|---|---|---|---|
| Overall Enjoyment | |||
| Overall degree of game enjoyment/fun | Whittinghill and Brown, 2014; Radtka et al., 2013; Freitas et al., 2013 | Aligned | Aligned. Item 2 |
| Difficulty/ease of playing | Radtka et al., 2013; Freitas et al., 2013 | Aligned | Aligned. Item 2 |
| Physical Interface | |||
| Range of motion and hold time diminish fun | Bryanton et al., 2006 | Aligned | Aligned. IF1-5 |
| Repetitions do not diminish fun | Bryanton et al., 2006 | Ambiguous | Aligned. Item 2 |
| Game controls are most difficult to get positively appraised | Whittinghill and Brown, 2014 | Aligned | Aligned. Items IF1-5 |
| Being comfortable while playing | Radtka et al., 2013 | Aligned | Ambiguous. Potential partial alignment with Items 10 and 2. |
| Game and Scenario Graphics | |||
| Visual aesthetic | Whittinghill and Brown, 2014 | Aligned | Ambiguous. Potential alignment with items 2/ IF2. |
| Immersion in game | Radtka et al., 2013 | Aligned | Ambiguous. Potential alignment with items 2/ IF-2. |
| Realism of look and feel of game | Radtka et al., 2013 | Aligned | Not aligned |
| Enjoyment of game scenario | Freitas et al., 2013 | Aligned | Ambiguous. Potential alignment with items 2/IF-2. |
| Overall Competence and Control | |||
| Sense of competence playing game | Radtka et al., 2013 | Aligned | Ambiguous. Potential partial alignment with items 3, 4, and 11. |
| Sense of control of game | Radtka et al., 2013; Freitas et al., 2012 | Aligned | Ambiguous. Possible alignment with item 12. |
| Challenge of the game | Freitas et al., 2013 | Aligned | Not aligned |
| Incentive From Therapeutic Awareness | |||
| Perceived therapeutic function | Freitas et al., 2013 | Aligned | Not aligned |
| Help game provided correctly doing therapeutic movements | Freitas et al., 2013 | Not aligned | Not aligned |
| Game increased motivation to perform exercises | Freitas et al., 2013; Sandlund et al., 2011 | Aligned | Not aligned |
| Spurred child’s initiative to exercise | Sandlund et al., 2011 | Not aligned | Ambiguous. Potential partial alignment with item 11. |
| Item | Individual Functionality Rating Criteria with Respect to the Specified Functionality | Selected Functionality | |
|---|---|---|---|
| Robotic Footplate Interface for Game Control (Hardware) | The Airplane Game (Software) | ||
| IF1 | Rate your satisfaction in relation to its ease of use | Aligned | Aligned |
| IF2 | Rate your satisfaction in relation to the help it provides in your everyday life. | Dual (Multiple) Alignments “Everyday Life” Interpretations (1) As supports functional improvement, i.e., exercises your ankle as it should (2) As works well for gameplay | Dual (Multiple) Alignments “Everyday Life” Interpretations (1) As is generally entertaining (2) As helps engagement in HEP |
| IF3 | Rate your satisfaction in relation to how safe/secure it is. | Ambiguous—need to distinguish this risk from that of injury on the system (IF5) and unreliability of function (IF4). | Not aligned |
| IF4 | Rate your satisfaction in relation to its reliability | Aligned Hardware reliability | Aligned Software reliability |
| IF5 | Rate your satisfaction in relation to the feeling of safety it provides | Aligned Freedom from non-injurious malfunction | Not Aligned |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schladen, M.M.; Cleary, K.; Koumpouros, Y.; Monfaredi, R.; Salvador, T.; Talari, H.F.; Slagle, J.; Coley, C.; Kovelman, S.; Belschner, J.; et al. Toward Evaluation of the Subjective Experience of a General Class of User-Controlled, Robot-Mediated Rehabilitation Technologies for Children with Neuromotor Disability. Informatics 2020, 7, 45. https://0-doi-org.brum.beds.ac.uk/10.3390/informatics7040045
Schladen MM, Cleary K, Koumpouros Y, Monfaredi R, Salvador T, Talari HF, Slagle J, Coley C, Kovelman S, Belschner J, et al. Toward Evaluation of the Subjective Experience of a General Class of User-Controlled, Robot-Mediated Rehabilitation Technologies for Children with Neuromotor Disability. Informatics. 2020; 7(4):45. https://0-doi-org.brum.beds.ac.uk/10.3390/informatics7040045
Chicago/Turabian StyleSchladen, Manon Maitland, Kevin Cleary, Yiannis Koumpouros, Reza Monfaredi, Tyler Salvador, Hadi Fooladi Talari, Jacob Slagle, Catherine Coley, Staci Kovelman, Justine Belschner, and et al. 2020. "Toward Evaluation of the Subjective Experience of a General Class of User-Controlled, Robot-Mediated Rehabilitation Technologies for Children with Neuromotor Disability" Informatics 7, no. 4: 45. https://0-doi-org.brum.beds.ac.uk/10.3390/informatics7040045






