Allopurinol-Induced Oral Lichenoid Drug Reaction with Complete Regression after Drug Withdrawal
Abstract
:1. Introduction
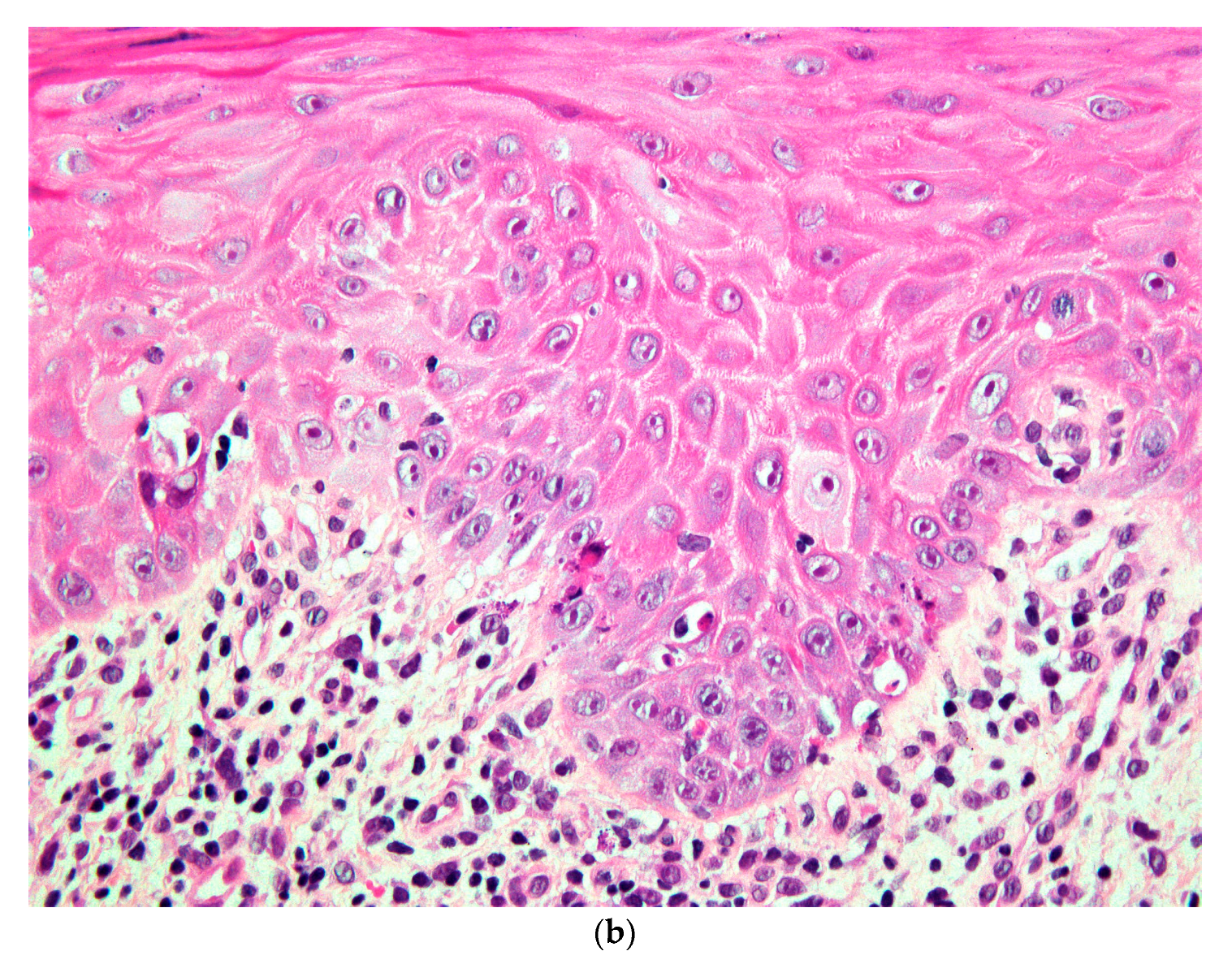
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Saurat, J.-H.; Lipsker, D.; Thomas, L.; Borradori, L.; Lachapelle, J.-M. Dermatologie Et Infections Sexuellement Transmissibles, 6th ed.; Elsevier-Masson: Paris, France, 2017. [Google Scholar]
- Lombardi, T.; Küffer, R. Concept actuel du lichen plan oral. Le diagnostic facile au début, peut devenir très difficile dans les lichens anciens. La Presse Médicale 2016, 45, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.-S.L.; Gould, A.; Kurago, Z.; Fantasia, J.; Muller, S. Diagnosis of oral lichen pla-nus: A position paper of the American Academy of Oral and Maxillofacial Pathology. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 332–354. [Google Scholar] [CrossRef] [PubMed]
- Seth, R.; Kydd, A.S.; Buchbinder, R.; Bombardier, C.; Edwards, C.J. Allopurinol for chronic gout. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.U.R.; Díaz-Torné, C.; Perez-Ruiz, F.; March, L.M. Epidemiology of gout: An up-date. Best Pract. Res. Clin. Rheumatol. 2010, 24, 811–827. [Google Scholar] [CrossRef] [PubMed]
- Atzori, L.; Pinna, A.L.; Mantovani, L.; Ferreli, C.; Pau, M.; Mulargia, M.; Aste, N. Cutaneous adverse drug reactions to allopurinol: 10 year observational survey of the dermatology de-partment—Cagliari University (Italy). J. Eur. Acad. Dermatol. Venereol. 2011, 26, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Chau, N.Y.; Reade, P.C.; Rich, A.M.; Hay, K.D. Allopurinol-amplified lichenoid reactions of the oral mucosa. Oral Surg. Oral Med. Oral Pathol. 1984, 58, 397–400. [Google Scholar] [CrossRef]
- Nair, R.G.; Newsome, P.R.H.; Itthagarun, A.; Samaranayake, L.P. Severe oral erosive lichen planus due to methyldopa and allopurinol: A case report. Hong Kong Dent. J. 2005, 2, 122–125. [Google Scholar]
- Arimone, Y.; Bidault, I.; Dutertre, J.-P.; Gérardin, M.; Guy, C.; Haramburu, F.; Hillaire-Buys, D.; Meglio, C.; Penfornis, C. Réactualisation de la méthode française d’imputabilité des effets indésirables des médicaments. Therapie 2011, 66, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Halevy, S.; Shai, A. Lichenoid drug eruptions. J. Am. Acad. Dermatol. 1993, 29, 249–255. [Google Scholar] [CrossRef]
- Giuliani, M.; Troiano, G.; Cordaro, M.; Corsalini, M.; Gioco, G.; Muzio, L.L.; Pignatelli, P.; Lajolo, C. Rate of malignant transformation of oral lichen planus: A systematic review. Oral Dis. 2019, 25, 693–709. [Google Scholar] [CrossRef] [PubMed]
- Van der Meij, E.H.; Mast, H.; van der Waal, I. The possible premalignant character of oral lichen planus and oral lichenoid lesions: A prospective five-year follow-up study of 192 patients. Oral Oncol. 2007, 43, 742–748. [Google Scholar] [CrossRef] [PubMed]





| Clinical Features | Allopurinol Indication | Histopathological Features | Outcomes | ||
|---|---|---|---|---|---|
| Chau et al. 1984 [7] | M, Caucasian, 53 y | Ulcerations Keratotic striae and plaques | Gout | No biopsy | Healing of ulcers Persistence of the keratosis |
| M, Caucasian, 56 y | Ulcerations on the lip, buccal mucosa and tongue | Gout | No biopsy | Healing of ulcers Persistence of the keratosis | |
| M, Caucasian, 60 y | Ulcerations Keratotic striae on the lip, buccal mucosa and tongue | Gout | LP versus lichenoid reaction | Persistence of minor ulcerations | |
| Nair et al. 2005 [8] | F, Chinese, 75 y | Erosions and ulcerations Keratotic striae and plaques on the buccal mucosa and tongue | Gout | No biopsy | Resolution of erosions Persistence of faint keratosis |
| Present case | M, Caucasian, 59 y | Buccal ulceration Keratotic striae on the lip, buccal mucosa and tongue | Gout | LP versus lichenoid reaction | Complete healing |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perez, A.; Lazzarotto, B.; Carrel, J.-P.; Lombardi, T. Allopurinol-Induced Oral Lichenoid Drug Reaction with Complete Regression after Drug Withdrawal. Dermatopathology 2020, 7, 18-25. https://0-doi-org.brum.beds.ac.uk/10.3390/dermatopathology7020004
Perez A, Lazzarotto B, Carrel J-P, Lombardi T. Allopurinol-Induced Oral Lichenoid Drug Reaction with Complete Regression after Drug Withdrawal. Dermatopathology. 2020; 7(2):18-25. https://0-doi-org.brum.beds.ac.uk/10.3390/dermatopathology7020004
Chicago/Turabian StylePerez, Alexandre, Benjamin Lazzarotto, Jean-Pierre Carrel, and Tommaso Lombardi. 2020. "Allopurinol-Induced Oral Lichenoid Drug Reaction with Complete Regression after Drug Withdrawal" Dermatopathology 7, no. 2: 18-25. https://0-doi-org.brum.beds.ac.uk/10.3390/dermatopathology7020004





