The Influence of Sagittal Pin Angulation on the Stiffness and Pull-Out Strength of a Monolateral Fixator Construct
Abstract
:1. Introduction
2. Materials and Methods
2.1. Fracture Model
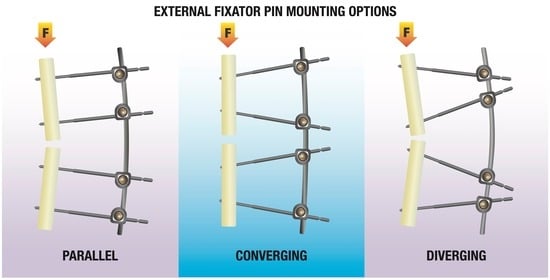
2.2. Frame Assembly
2.3. Mechanical Testing
2.4. Data Analysis
2.5. Statistics
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fragomen, A.T.; Rozbruch, S.R. The Mechanics of External Fixation. HSS J. 2006, 3, 13–29. [Google Scholar] [CrossRef]
- Behrens, F. General theory and principles of external fixation. Clin. Orthop. Relat. Res. 1989, 241, 15–23. [Google Scholar] [CrossRef]
- Narayan, B.; Giotakis, N. Stability with unilateral external fixation in the tibia. Strat. Trauma Limb Reconstr. 2007, 2, 13–20. [Google Scholar] [CrossRef]
- Lenarz, C.; Bledsoe, G.; Watson, T.J. Circular External Fixation Frames with Divergent Half Pins: A Pilot Biomechanical Study. Clin. Orthop. Relat. Res. 2008, 466, 2933–2939. [Google Scholar] [CrossRef]
- Bottlang, M.; Doornink, J.; Lujan, T.J.; Fitzpatrick, D.C.; Marsh, J.L.; Augat, P.; von Rechenberg, B.; Lesser, M.; Madey, S.M. Effects of construct stiffness on healing of fractures stabilized with locking plates. J. Bone Jt. Surg. Am. 2010, 92 (Suppl. S2), 12–22. [Google Scholar] [CrossRef]
- Claes, L.E.; Heigele, C.A.; Neidlinger-Wilke, C.; Kaspar, D.; Seidl, W.; Margevicius, K.J.; Augat, P. Effects of mechanical factors on the fracture healing process. Clin. Orthop. Relat. Res. 1998, 355, S132–S147. [Google Scholar] [CrossRef]
- Augat, P.; Burger, J.; Schorlemmer, S.; Henke, T.; Peraus, M.; Claes, L. Shear movement at the fracture site delays healing in a diaphyseal fracture model. J. Orthop. Res. 2003, 21, 1011–1017. [Google Scholar] [CrossRef]
- Hente, R.; Füchtmeier, B.; Schlegel, U.; Ernstberger, A.; Perren, S.M. The influence of cyclic compression and distraction on the healing of experimental tibial fractures. J. Orthop. Res. 2004, 22, 709–715. [Google Scholar] [CrossRef]
- Kenwright, J.; Goodship, A.E. Controlled mechanical stimulation in the treatment of tibial fractures. Clin. Orthop. Relat. Res. 1989, 241, 36–47. [Google Scholar] [CrossRef]
- Jagodzinski, M.; Krettek, C. Effect of mechanical stability on fracture healing—An update. Injury 2007, 38, S3–S10. [Google Scholar] [CrossRef]
- Behrens, F.; Johnson, W.D.; Koch, T.W.; Kovacevic, N. Bending stiffness of unilateral and bilateral fixator frames. Clin. Orthop. Relat. Res. 1983, 178, 103–110. [Google Scholar] [CrossRef]
- Kempson, G.; Campbell, D. The comparative stiffness of external fixation frames. Injury 1981, 12, 297–304. [Google Scholar] [CrossRef]
- Weeth, R.E.; Madsen, T.; Schrøder, H.A. Experimental analysis of hoffmann external fixation in various mountings. Arch. Orthop. Trauma Surg. 1985, 104, 197–200. [Google Scholar] [CrossRef]
- Willie, B.; Adkins, K.; Zheng, X.; Simon, U.; Claes, L. Mechanical characterization of external fixator stiffness for a rat femoral fracture model. J. Orthop. Res. 2008, 27, 687–693. [Google Scholar] [CrossRef]
- Oni, O.O.; Capper, M.; Soutis, C. External fixation of upper limb fractures: The effect of pin offset on fixator stability. Biomaterials 1995, 16, 263–264. [Google Scholar] [CrossRef] [PubMed]
- Egan, J.M.; Shearer, J.R. Behavior of an external fixation frame incorporating an angular separation of the fixator pins. A finite element approach. Clin. Orthop. Relat. Res. 1987, 223, 265–274. [Google Scholar] [CrossRef]
- Fernando, P.; Abeygunawardane, A.; Wijesinghe, P.; Dharmaratne, P.; Silva, P. An engineering review of external fixators. Med. Eng. Phys. 2021, 98, 91–103. [Google Scholar] [CrossRef]
- Pettine, K.A.; Chao, E.Y.S.; Kelly, P.J. Analysis of the External Fixator Pin-Bone Interface. Clin. Orthop. Relat. Res. 1993, 293, 18–27. [Google Scholar] [CrossRef]
- Schell, H.; Reuther, T.; Duda, G.N.; Lienau, J. The Pin-Bone Interface in External Fixator: A Standardized Analysis in a Sheep Osteotomy Model. J. Orthop. Trauma 2011, 25, 438–445. [Google Scholar] [CrossRef]
- Dernell, W.S.; Harari, J.; Blackketter, D.M. A Comparison of Acute Pull-Out Strength Between Two-Way and One-Way Transfixation Pin Insertion for External Skeletal Fixation in Canine Bone. Vet. Surg. 1993, 22, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.; Spencer, M.; Wang, Q.; White, S.; Cunningham, J. Design and testing of external fixator bone screws. J. Biomed. Eng. 1990, 12, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Seitz, W.H.; Froimson, A.I.; Brooks, D.B.; Postak, P.; Polando, G.; Greenwald, A.S.; Phil, D. External fixator pin insertion techniques: Biomechanical analysis and clinical relevance. J. Hand Surg. 1991, 16, 560–563. [Google Scholar] [CrossRef] [PubMed]
- Gathen, M.; Ploeger, M.M.; Jaenisch, M.; Koob, S.; Cucchi, D.; Kasapovic, A.; Randau, T.; Placzek, R. Outcome evaluation of new calcium titanate schanz-screws for external fixators. First clinical results and cadaver studies. J. Mater. Sci. Mater. Med. 2019, 30, 124. [Google Scholar] [CrossRef]
- Moroni, A.; Vannini, F.; Mosca, M.; Giannini, S. State of the Art Review: Techniques to Avoid Pin Loosening and Infection in External Fixation. J. Orthop. Trauma 2002, 16, 189–195. [Google Scholar] [CrossRef]
- Klein, P.; Schell, H.; Streitparth, F.; Heller, M.; Kassi, J.-P.; Kandziora, F.; Bragulla, H.; Haas, N.P.; Duda, G.N. The initial phase of fracture healing is specifically sensitive to mechanical conditions. J. Orthop. Res. 2003, 21, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Augat, P.; Merk, J.; Ignatius, A.; Margevicius, K.; Bauer, G.; Rosenbaum, D.; Claes, L. Early, full weightbearing with flexible fixation delays fracture healing. Clin. Orthop. Relat. Res. 1996, 328, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Sellei, R.M.; Kobbe, P.; Dienstknecht, T.; Lichte, P.; Pfeifer, R.; Behrens, M.; Brianza, S.; Pape, H.-C. Biomechanical properties of different external fixator frame configurations. Eur. J. Trauma Emerg. Surg. 2014, 41, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Sellei, R.M.; Kobbe, P.; Dadgar, A.; Pfeifer, R.; Behrens, M.; von Oldenburg, G.; Pape, H.-C. External fixation design evolution enhances biomechanical frame performance. Injury 2015, 46, S23–S26. [Google Scholar] [CrossRef]
- Shi, D.; Liu, K.; Zhang, H.; Wang, X.; Li, G.; Zheng, L. Investigating the biomechanical function of the plate-type external fixator in the treatment of tibial fractures: A biomechanical study. BMC Musculoskelet. Disord. 2020, 21, 128. [Google Scholar] [CrossRef]
- Ang, B.F.H.; Chen, J.Y.; Yew, A.K.S.; Chua, S.K.; Chou, S.M.; Chia, S.L.; Koh, J.S.B.; Howe, T.S. Externalised locking compression plate as an alternative to the unilateral external fixator: A biomechanical comparative study of axial and torsional stiffness. Bone Jt. Res. 2017, 6, 216–223. [Google Scholar] [CrossRef]
- Pavic, A.; Kodvanj, J.; Sabalic, S.; Cukelj, F.; Bakota, B. Novel external fixation fracture method with circular locking mechanism compared with the application of dynamic axial external fixator on experimental tibial model ensures better stability in bending and favourable performance in dynamic loads. Injury 2013, 44, S52–S55. [Google Scholar] [CrossRef] [PubMed]
- Kouassi, K.J.-E.; Cartiaux, O.; Fonkoué, L.; Detrembleur, C.; Cornu, O. Biomechanical study of a low-cost external fixator for diaphyseal fractures of long bones. J. Orthop. Surg. Res. 2020, 15, 247. [Google Scholar] [CrossRef]
- Liu, W.; Yang, L.; Kong, X.; An, L.; Hong, G.; Guo, Z.; Zang, L. Stiffness of the locking compression plate as an external fixator for treating distal tibial fractures: A biomechanics study. BMC Musculoskelet. Disord. 2017, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Roseiro, L.M.; Neto, M.A.; Amaro, A.; Leal, R.P.; Samarra, M.C. External fixator configurations in tibia fractures: 1D optimization and 3D analysis comparison. Comput. Methods Programs Biomed. 2014, 113, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Chao, E.; Kasman, R.; An, K. Rigidity and stress analyses of external fracture fixation devices—A theoretical approach. J. Biomech. 1982, 15, 971–983. [Google Scholar] [CrossRef]
- Behrens, F.; Searls, K. External fixation of the tibia. Basic concepts and prospective evaluation. J. Bone Jt. Surg. Br. 1986, 68, 246–254. [Google Scholar] [CrossRef]
- Aro, H.T.; Markel, M.D.; Chao, E.Y. Cortical bone reactions at the interface of external fixation half-pins under different loading conditions. J. Trauma 1993, 35, 776–785. [Google Scholar] [CrossRef] [PubMed]
- Huiskes, R.; Chao, E.Y.S. Guidelines for external fixation frame rigidity and stresses. J. Orthop. Res. 1986, 4, 68–75. [Google Scholar] [CrossRef]
- Stoffel, K.; Dieter, U.; Stachowiak, G.; Gachter, A.; Kuster, M.S. Biomechanical testing of the LCP—How can stability in locked internal fixators be controlled? Injury 2003, 34 (Suppl. S2), B11–B19. [Google Scholar] [CrossRef]
- Roberts, C.S.; Dodds, J.C.; Perry, K.; Beck, D.; Seligson, D.; Voor, M.J. Hybrid External Fixation of the Proximal Tibia: Strategies to Improve Frame Stability. J. Orthop. Trauma 2003, 17, 415–420. [Google Scholar] [CrossRef]








| Pin Configuration | Sample | Stiffness (N/mm) | Mean Stiffness ± SD (N/mm) |
|---|---|---|---|
| Parallel | 1 | 20.29 | 20.24 ± 0.24 |
| 2 | 20.46 | ||
| 3 | 19.98 | ||
| Converging | 4 | 27.71 | 27.13 ± 0.67 |
| 5 | 26.41 | ||
| 6 | 27.27 | ||
| Diverging | 7 | 17.82 | 17.71 ± 0.19 |
| 8 | 17.49 | ||
| 9 | 17.81 |
| Pin Configuration | Sample | F Max (kN) | Mean F Max ± SD (kN) |
|---|---|---|---|
| Parallel | 1a | 3.45 | 3.16 ± 0.24 |
| 1b | 2.84 | ||
| 2a | 3.16 | ||
| 2b | 3.14 | ||
| 3a | 2.97 | ||
| 3b | 3.41 | ||
| Converging | 4a | 2.87 | 2.84 ± 0.25 |
| 4b | 3.04 | ||
| 5a | 2.85 | ||
| 5b | 2.55 | ||
| 6a | 3.17 | ||
| 6b | 2.58 | ||
| Diverging | 7a | 3.53 | 3.47 ± 0.51 |
| 7b | 4.03 | ||
| 8a | 3.52 | ||
| 8b | 2.52 | ||
| 9a | 3.45 | ||
| 9b | 3.74 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klemeit, A.; Weber, A.; Bourauel, C.; Welle, K.; Burger, C.; Schildberg, F.A.; Deborre, C. The Influence of Sagittal Pin Angulation on the Stiffness and Pull-Out Strength of a Monolateral Fixator Construct. Bioengineering 2023, 10, 982. https://0-doi-org.brum.beds.ac.uk/10.3390/bioengineering10080982
Klemeit A, Weber A, Bourauel C, Welle K, Burger C, Schildberg FA, Deborre C. The Influence of Sagittal Pin Angulation on the Stiffness and Pull-Out Strength of a Monolateral Fixator Construct. Bioengineering. 2023; 10(8):982. https://0-doi-org.brum.beds.ac.uk/10.3390/bioengineering10080982
Chicago/Turabian StyleKlemeit, Axel, Anna Weber, Christoph Bourauel, Kristian Welle, Christof Burger, Frank A. Schildberg, and Christoph Deborre. 2023. "The Influence of Sagittal Pin Angulation on the Stiffness and Pull-Out Strength of a Monolateral Fixator Construct" Bioengineering 10, no. 8: 982. https://0-doi-org.brum.beds.ac.uk/10.3390/bioengineering10080982