Intervertebral Disc Tissue Engineering Using Additive Manufacturing
Abstract
:1. Introduction
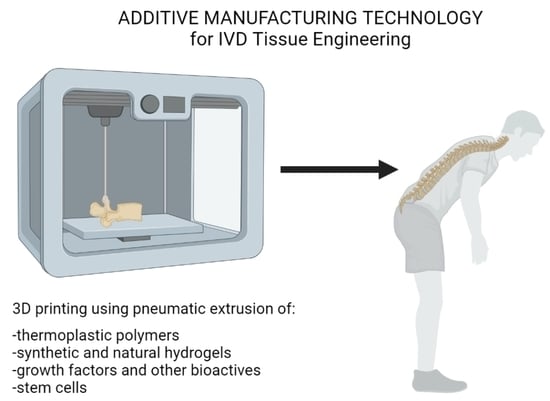
2. Regenerative Medicine
3. Additive Manufacturing in IVD Tissue Engineering
| AM Technology | Advantages | Disadvantages |
|---|---|---|
| 3D bioprinting | High cell viability; able to encapsulate cells, growth factors and nutrients; zone-specific distribution of cells. | Limited structural integrity; limited mechanical strength. |
| Fused deposition modelling | Able to fabricate scaffolds with various porosity; cost effective; minimum waste [40]. | Limited biomaterial range as ink; high temperature; potential exposure to toxic fumes. |
| Melt electrowriting | High control over scaffold microarchitecture with microfibers. | High temperature; limited biomaterial range as ink. |
| SLS | Reliable, fast, requiring no support structures with excellent mechanical properties. | Limited material selection, high shrink rate, higher waste than other AM techniques. |
4. Future Perspectives and Challenges of Utilising Additive Manufacturing in Whole IVD Tissue Engineering
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Whatley, B.R.; Kuo, J.; Shuai, C.; Damon, B.J.; Wen, X. Fabrication of a biomimetic elastic intervertebral disk scaffold using additive manufacturing. Biofabrication 2011, 3, 015004. [Google Scholar] [CrossRef] [PubMed]
- Costa, J.B.; Silva-Correia, J.; Ribeiro, V.P.; da Silva Morais, A.; Oliveira, J.M.; Reis, R.L. Engineering patient-specific bioprinted constructs for treatment of degenerated intervertebral disc. Mater. Today Commun. 2019, 19, 506–512. [Google Scholar] [CrossRef]
- Nerurkar, N.L.; Sen, S.; Huang, A.H.; Elliott, D.M.; Mauck, R.L. Engineered disc-like angle-ply structures for intervertebral disc replacement. Spine 2010, 35, 867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mizuno, H.; Roy, A.K.; Vacanti, C.A.; Kojima, K.; Ueda, M.; Bonassar, L.J. Tissue-engineered composites of anulus fibrosus and nucleus pulposus for intervertebral disc replacement. Spine 2004, 29, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Lyu, F.-J.; Cui, H.; Pan, H.; Cheung, K.M.; Cao, X.; Iatridis, J.C.; Zheng, Z. Painful intervertebral disc degeneration and inflammation: From laboratory evidence to clinical interventions. Bone Res. 2021, 9, 7. [Google Scholar] [CrossRef]
- Adams, M.A.; Roughley, P.J. What is intervertebral disc degeneration, and what causes it? Spine 2006, 31, 2151–2161. [Google Scholar] [CrossRef] [Green Version]
- Ligorio, C.; Hoyland, J.A.; Saiani, A. Self-Assembling Peptide Hydrogels as Functional Tools to Tackle Intervertebral Disc Degeneration. Gels 2022, 8, 211. [Google Scholar] [CrossRef]
- Wang, F.; Cai, F.; Shi, R.; Wang, X.-H.; Wu, X.-T. Aging and age related stresses: A senescence mechanism of intervertebral disc degeneration. Osteoarthr. Cartil. 2016, 24, 398–408. [Google Scholar] [CrossRef] [Green Version]
- Doraiswamy, R.; Pillai, J.; Krishnamurthy, K. Genetics of intervertebral disc disease: A review. Clin. Anat. 2022, 35, 116–120. [Google Scholar]
- Yang, X.; Li, X. Nucleus pulposus tissue engineering: A brief review. Eur. Spine J. 2009, 18, 1564. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.C.; Hu, Y.; Li, Z.; Luk, K.D. Biomaterials for intervertebral disc regeneration: Current status and looming challenges. J. Tissue Eng. Regen. Med. 2018, 12, 2188–2202. [Google Scholar] [CrossRef] [PubMed]
- de Beer, N.; van der Merwe, A. Patient-specific intervertebral disc implants using rapid manufacturing technology. Rapid Prototyp. J. 2013, 19, 126–139. [Google Scholar] [CrossRef]
- Reeks, J.; Liang, H. Materials and their failure mechanisms in total disc replacement. Lubricants 2015, 3, 346–364. [Google Scholar] [CrossRef] [Green Version]
- O’Halloran, D.M.; Pandit, A.S. Tissue-engineering approach to regenerating the intervertebral disc. Tissue Eng. 2007, 13, 1927–1954. [Google Scholar] [CrossRef]
- Stergar, J.; Gradisnik, L.; Velnar, T.; Maver, U. Intervertebral disc tissue engineering: A brief review. Bosn. J. Basic Med. Sci. 2019, 19, 130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Uden, S.; Silva-Correia, J.; Correlo, V.; Oliveira, J.; Reis, R. Custom-tailored tissue engineered polycaprolactone scaffolds for total disc replacement. Biofabrication 2015, 7, 015008. [Google Scholar] [CrossRef]
- Henry, N.; Clouet, J.; Le Bideau, J.; Le Visage, C.; Guicheux, J. Innovative strategies for intervertebral disc regenerative medicine: From cell therapies to multiscale delivery systems. Biotechnol. Adv. 2018, 36, 281–294. [Google Scholar] [CrossRef]
- Baumgartner, L.; Wuertz-Kozak, K.; Le Maitre, C.L.; Wignall, F.; Richardson, S.M.; Hoyland, J.; Ruiz Wills, C.; González Ballester, M.A.; Neidlin, M.; Alexopoulos, L.G.; et al. Multiscale Regulation of the Intervertebral Disc: Achievements in Experimental, In Silico, and Regenerative Research. Int. J. Mol. Sci. 2021, 22, 703. [Google Scholar] [CrossRef]
- Tian, A.; Yi, X.; Sun, N. Application of mesenchymal stem cells combined with nano-polypeptide hydrogel in tissue engineering blood vessel. Regen. Ther. 2022, 21, 277–281. [Google Scholar] [CrossRef]
- Shen, S.; Chen, M.; Guo, W.; Li, H.; Li, X.; Huang, S.; Luo, X.; Wang, Z.; Wen, Y.; Yuan, Z. Three dimensional printing-based strategies for functional cartilage regeneration. Tissue Eng. Part B Rev. 2019, 25, 187–201. [Google Scholar] [CrossRef] [Green Version]
- Subia, B.; Kundu, J.; Kundu, S. Biomaterial scaffold fabrication techniques for potential tissue engineering applications. In Tissue Engineering; InTech: London, UK, 2010. [Google Scholar]
- Yoshida, M.; Turner, P.R.; Ali, M.A.; Cabral, J.D. Three-Dimensional Melt-Electrowritten Polycaprolactone/Chitosan Scaffolds Enhance Mesenchymal Stem Cell Behavior. ACS Appl. Bio Mater. 2021, 4, 1319–1329. [Google Scholar] [CrossRef] [PubMed]
- Ventola, C.L. Medical applications for 3D printing: Current and projected uses. Pharm. Ther. 2014, 39, 704. [Google Scholar]
- Hu, D.; Wu, D.; Huang, L.; Jiao, Y.; Li, L.; Lu, L.; Zhou, C. 3D bioprinting of cell-laden scaffolds for intervertebral disc regeneration. Mater. Lett. 2018, 223, 219–222. [Google Scholar] [CrossRef]
- Sun, B.; Lian, M.; Han, Y.; Mo, X.; Jiang, W.; Qiao, Z.; Dai, K. A 3D-Bioprinted dual growth factor-releasing intervertebral disc scaffold induces nucleus pulposus and annulus fibrosus reconstruction. Bioact. Mater. 2021, 6, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Schuurman, W.; Khristov, V.; Pot, M.W.; van Weeren, P.R.; Dhert, W.J.; Malda, J. Bioprinting of hybrid tissue constructs with tailorable mechanical properties. Biofabrication 2011, 3, 021001. [Google Scholar] [CrossRef] [PubMed]
- Gloria, A.; Russo, T.; D’Amora, U.; Santin, M.; De Santis, R.; Ambrosio, L. Customised multiphasic nucleus/annulus scaffold for intervertebral disc repair/regeneration. Connect. Tissue Res. 2020, 61, 152–162. [Google Scholar] [CrossRef]
- Marshall, S.L.; Jacobsen, T.D.; Emsbo, E.; Murali, A.; Anton, K.; Liu, J.Z.; Lu, H.H.; Chahine, N.O. Three-Dimensional-Printed Flexible Scaffolds Have Tunable Biomimetic Mechanical Properties for Intervertebral Disc Tissue Engineering. ACS Biomater. Sci. Eng. 2021, 7, 5836–5849. [Google Scholar] [CrossRef]
- Zhu, M.; Tan, J.; Liu, L.; Tian, J.; Li, L.; Luo, B.; Zhou, C.; Lu, L. Construction of biomimetic artificial intervertebral disc scaffold via 3D printing and electrospinning. Mater. Sci. Eng. C 2021, 128, 112310. [Google Scholar] [CrossRef]
- Wu, D.; Tan, J.; Yao, L.; Tian, J.; Luo, B.; Li, L.; Zhou, C.; Lu, L. Customized composite intervertebral disc scaffolds by integrated 3D bioprinting for therapeutic implantation. Compos. Part A Appl. Sci. Manuf. 2021, 147, 106468. [Google Scholar] [CrossRef]
- Jiang, Y.; Shi, K.; Zhou, L.; He, M.; Zhu, C.; Wang, J.; Li, J.; Li, Y.; Liu, L.; Sun, D.; et al. 3D-printed auxetic-structured intervertebral disc implant for potential treatment of lumbar herniated disc. Bioact. Mater. 2023, 20, 528–538. [Google Scholar] [CrossRef]
- Shirazi, S.F.; Gharehkhani, S.; Mehrali, M.; Yarmand, H.; Metselaar, H.S.; Adib Kadri, N.; Osman, N.A. A review on powder-based additive manufacturing for tissue engineering: Selective laser sintering and inkjet 3D printing. Sci. Technol. Adv. Mater. 2015, 16, 033502. [Google Scholar] [CrossRef] [PubMed]
- Moroni, L.; Boland, T.; Burdick, J.A.; De Maria, C.; Derby, B.; Forgacs, G.; Groll, J.; Li, Q.; Malda, J.; Mironov, V.A. Biofabrication: A guide to technology and terminology. Trends Biotechnol. 2018, 36, 384–402. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, P.; Schweller, R.M.; Khademhosseini, A.; West, J.L.; Bashir, R. 3D biofabrication strategies for tissue engineering and regenerative medicine. Annu. Rev. Biomed. Eng. 2014, 16, 247–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zein, I.; Hutmacher, D.W.; Tan, K.C.; Teoh, S.H. Fused deposition modeling of novel scaffold architectures for tissue engineering applications. Biomaterials 2002, 23, 1169–1185. [Google Scholar] [CrossRef]
- Yoshida, M.; Turner, P.R.; McAdam, C.J.; Ali, M.A.; Cabral, J.D. A comparison between β-tricalcium phosphate and chitosan poly-caprolactone-based 3D melt extruded composite scaffolds. Biopolymers 2022, 113, e23482. [Google Scholar] [CrossRef]
- Yang, J.; Wang, L.; Zhang, W.; Sun, Z.; Li, Y.; Yang, M.; Zeng, D.; Peng, B.; Zheng, W.; Jiang, X. Reverse Reconstruction and Bioprinting of Bacterial Cellulose-Based Functional Total Intervertebral Disc for Therapeutic Implantation. Small 2018, 14, 1702582. [Google Scholar] [CrossRef]
- Moriguchi, Y.; Mojica-Santiago, J.; Grunert, P.; Pennicooke, B.; Berlin, C.; Khair, T.; Navarro-Ramirez, R.; Ricart Arbona, R.J.; Nguyen, J.; Härtl, R.; et al. Total disc replacement using tissue-engineered intervertebral discs in the canine cervical spine. PLoS ONE 2017, 12, e0185716. [Google Scholar] [CrossRef] [Green Version]
- Turner, P.; Yoshida, M.; Ali, A.; Cabral, J. Melt electrowritten sandwich technique using sulforhodamine B to monitor stem cell behavior. Tissue Eng. Part C Methods 2020, 26, 519–527. [Google Scholar] [CrossRef]
- O’brien, F.J. Biomaterials & scaffolds for tissue engineering. Mater. Today 2011, 14, 88–95. [Google Scholar]
- D’Este, M.; Eglin, D.; Alini, M. Lessons to be learned and future directions for intervertebral disc biomaterials. Acta Biomater. 2018, 78, 13–22. [Google Scholar] [CrossRef]
- Gauvin, R.; Chen, Y.-C.; Lee, J.W.; Soman, P.; Zorlutuna, P.; Nichol, J.W.; Bae, H.; Chen, S.; Khademhosseini, A. Microfabrication of complex porous tissue engineering scaffolds using 3D projection stereolithography. Biomaterials 2012, 33, 3824–3834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inzana, J.A.; Olvera, D.; Fuller, S.M.; Kelly, J.P.; Graeve, O.A.; Schwarz, E.M.; Kates, S.L.; Awad, H.A. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials 2014, 35, 4026–4034. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kantaros, A.; Piromalis, D. Fabricating Lattice Structures via 3D Printing: The Case of Porous Bio-Engineered Scaffolds. Appl. Mech. 2021, 2, 289–302. [Google Scholar] [CrossRef]
- Buckley, C.T.; Hoyland, J.A.; Fujii, K.; Pandit, A.; Iatridis, J.C.; Grad, S. Critical aspects and challenges for intervertebral disc repair and regeneration—Harnessing advances in tissue engineering. Jor Spine 2018, 1, e1029. [Google Scholar] [CrossRef] [PubMed]
- Bliley, J.M.; Marra, K.G. Chapter 11—Polymeric Biomaterials as Tissue Scaffolds. In Stem Cell Biology and Tissue Engineering in Dental Sciences; Vishwakarma, A., Sharpe, P., Shi, S., Ramalingam, M., Eds.; Academic Press: Boston, MA, USA, 2015; pp. 149–161. [Google Scholar] [CrossRef]
- Jungst, T.; Pennings, I.; Schmitz, M.; Rosenberg, A.J.; Groll, J.; Gawlitta, D. Heterotypic scaffold design orchestrates primary cell organization and phenotypes in cocultured small diameter vascular grafts. Adv. Funct. Mater. 2019, 29, 1905987. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, K.; Aizawa, T.; Kanno, H.; Itoi, E. Adjacent segment degeneration after fusion spinal surgery—A systematic review. Int. Orthop. 2019, 43, 987–993. [Google Scholar] [CrossRef]
- Ghiselli, G.; Wang, J.C.; Bhatia, N.N.; Hsu, W.K.; Dawson, E.G. Adjacent segment degeneration in the lumbar spine. JBJS 2004, 86, 1497–1503. [Google Scholar] [CrossRef]
- Cox, S.C.; Thornby, J.A.; Gibbons, G.J.; Williams, M.A.; Mallick, K.K. 3D printing of porous hydroxyapatite scaffolds intended for use in bone tissue engineering applications. Mater. Sci. Eng. C 2015, 47, 237–247. [Google Scholar] [CrossRef]
- Gullbrand, S.E.; Ashinsky, B.G.; Bonnevie, E.D.; Kim, D.H.; Engiles, J.B.; Smith, L.J.; Elliott, D.M.; Schaer, T.P.; Smith, H.E.; Mauck, R.L. Long-term mechanical function and integration of an implanted tissue-engineered intervertebral disc. Sci. Transl. Med. 2018, 10, eaau0670. [Google Scholar] [CrossRef]
- Maroudas, A. Biophysical chemistry of cartilaginous tissues with special reference to solute and fluid transport. Biorheology 1975, 12, 233–248. [Google Scholar] [CrossRef]
- Martin, J.T.; Gullbrand, S.E.; Mohanraj, B.; Ashinsky, B.G.; Kim, D.H.; Ikuta, K.; Elliott, D.M.; Smith, L.J.; Mauck, R.L.; Smith, H.E. Optimization of Preculture Conditions to Maximize the In Vivo Performance of Cell-Seeded Engineered Intervertebral Discs. Tissue Eng. Part A 2017, 23, 923–934. [Google Scholar] [CrossRef] [PubMed]
- Alini, M.; Li, W.; Markovic, P.; Aebi, M.; Spiro, R.C.; Roughley, P.J. The potential and limitations of a cell-seeded collagen/hyaluronan scaffold to engineer an intervertebral disc-like matrix. Spine 2003, 28, 446–453. [Google Scholar] [CrossRef] [PubMed]


| Fabrication Method | Material | Findings | Ref. |
|---|---|---|---|
| 3D printing and lyophilisation | Degradable Polyurethane | Cells aligned along the concentric lamellae. Scaffold did not degrade after 19 days. | [1] |
| 3D melt extrusion | PCL | Reconstructed IVD showed the same zone specific matrix as natural tissue with good biomechanics. | [25] |
| 3D bioprinting | GF loaded on to polydopamine (PDA) nanoparticles (NPs) mixed with hydrogel | ||
| FDM | PCL | Fibre-reinforced hybrid hydrogel structures allowed for a wider range of potential in hydrogels. | [26] |
| 3D bioprinting | Cell-laden (C20A4) alginate hydrogel | ||
| FDM | PLA | High cell proliferation rate and remained viability > 90% during the culture. | [24] |
| 3D bioprinting | Gellan gum-poly (ethylene glycol) diacrylate (GG-PEGDA) double network hydrogel with murine bone marrow stromal cells. | ||
| FDM (CEP, AF) | PCL | Compressive modulus was within the range of lumbar disc. | [27] |
| Hydrogel fill | hMSC cell-laden collagen-LMW HA-4S-Star_PEG_CNP hydrogel | ||
| FDM | FlexiFil PLA (FPLA) | Scaffolds were stable, biocompatible, and allowed fibrocartilaginous matrix expression by MSCs and proteoglycan-rich ECM deposition by NP cells. | [28] |
| Hydrogel fill | Alginate hydrogel | ||
| electrospinning | PLLA/POSS-(PLLA) nanofiber | A 6-month in vivo rat C3/C4 disc space implantation demonstrated maintenance of disc height and deposition of proteoglycan. Mechanical properties similar to that of native IVD. | [29] |
| FDM | PLA | ||
| 3D bioprinting | Gellan gum/polyethylene glycol diacrylate (GG/PEGDA) double network | ||
| FDM (CEP, AF) | PCL | CTGF in AF region promoted fibrocartilage such as differentiation, and TGF-β3 in NP region promoted differentiation to hyaline cartilage-like cells. Bone marrow MSCs in IVD scaffold promotes Collagen type I deposition. TGF-β3 in NP region promoted deposition of glycosaminoglycans and collagen type II. CTGF in AF region promoted deposition of glycosaminoglycans and collagen type I. | [25] |
| 3D bioprinting | Gelatin-hyaluronic acid-sodium alginate mixed with growth factors | ||
| FDM | PLA | After 6 months implantation in rat C3/C4 space, scaffolds maintained their height and promoted deposition of proteoglycan and collagen. | [30] |
| 3D bioprinting | GG-PEGDA hydrogel with rBMSC cells | ||
| Selective laser sintering (SLS) | Polyurethane with modified “Bucklicrystal” structure | Showed appropriate mechanical behaviour along with in vitro and in vivo ability to restore physiological function. | [31,32] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshida, M.; Turner, P.R.; Cabral, J.D. Intervertebral Disc Tissue Engineering Using Additive Manufacturing. Gels 2023, 9, 25. https://0-doi-org.brum.beds.ac.uk/10.3390/gels9010025
Yoshida M, Turner PR, Cabral JD. Intervertebral Disc Tissue Engineering Using Additive Manufacturing. Gels. 2023; 9(1):25. https://0-doi-org.brum.beds.ac.uk/10.3390/gels9010025
Chicago/Turabian StyleYoshida, Minami, Paul Richard Turner, and Jaydee Dones Cabral. 2023. "Intervertebral Disc Tissue Engineering Using Additive Manufacturing" Gels 9, no. 1: 25. https://0-doi-org.brum.beds.ac.uk/10.3390/gels9010025