1. Introduction
Globally, inflammation is a major issue because of its crippling signs, leading to the loss of productivity and significant suffering [
1]. Inflammation, derived from the Latin word ‘
inflammatio’, is a defence mechanism of the body against diseases or undesired external substances that infiltrate tissue cells [
2]; with five vital indications- redness, swelling, heat, pain, and loss of function [
3]. There are a variety of chemical mediators (which are either cell or plasma-derived) from the circulatory damaged tissue, inflammatory cells, and the immune system that actively participates in, and adjusts inflammatory responses [
4]. They include vasoactive amines such as histamine and serotonin, peptides such as bradykinin; and eicosanoids such as thromboxane, leukotrienes, and prostaglandins. Inflammation could be acute [
5] or chronic [
6].
Acute inflammation occurs when there is tissue damage as a result of injury, microbial invasion or toxic compounds. It begins rapidly and becomes severe within a little duration of time and symptoms may persist for a few days, such as in the case of cellulitis or acute pneumonia [
7]. When acute inflammation becomes non-regulated, it may advance to chronic inflammation. Chronic inflammation is a protracted inflammation that lasts for longer than a few months or a few years. The reason for the injury and the body’s capacity to heal and overcome the damage are the main determinants of the degree and consequences of chronic inflammation. [
7]. It is essential for the emergence of several pathological conditions, including cancer, rheumatoid arthritis, obesity, diabetes type 2, Alzheimer’s disease, along with pulmonary and cardiovascular diseases [
8].
The leading cause of death globally has been associated with chronic disorders [
9], with 60% of these deaths due to chronic inflammatory diseases [
7]. Although, there are several classes of drugs currently available for the treatment of inflammation, non-steroidal anti-inflammatory medications (NSAIDs) continue to be the most widely utilized treatment for these ailments. Unfortunately, the clinical use NSAIDs is often associated with some undesirable side effects [
7] and hence, the need for the search for alternative therapies are essential. NSAIDs provide pain relief and anti-inflammatory activity of great value and therefore, the goal is not to replace NSAIDs altogether, but to decrease the frequency of dosages. According to WHO, it is estimated that in developing countries, about 80% of the population uses traditional medicines for their health care [
10]. For thousands of years, medicinal plants have been utilized as traditional remedies for a wide range of human ailments in many different parts of the world. In rural areas, medicinal plants are still the primary source of medicine since they have anti-inflammatory properties with minimal to no adverse effects. [
11].
Entandrophragma utile is a species of flowering plant in the Meliaceae family known by the local names- Igi jebo (Yoruba); Sipo, Assie, Acajou (French); Mukola, Muyovu (Luganda) [
12]. The plant is widely distributed in the Guinea-Congolese region, particularly growing in the evergreens and semi-deciduous dense rainforests. It is found in large areas that stretches both north and south of the equator, extending from the Atlantic coast across the Congo basin to the eastern side of the Kivin Ridge. It may also be found in Angola, Cameroon, Central African Republic, Congo DR, Cote d’Ivoire, Gabon, Ghana, Liberia, Nigeria, Sierra Leone, and South of the African Sahara [
13]. In Nigeria, people have long utilized the stem bark of
E. utile to cure conditions like rheumatism, ocular irritation, sickle cell illness, stomach, and duodenal ulcers, and more [
14,
15]. Phytochemical analysis of this plant has led to the identification of secondary metabolites such as saponins, flavonoids, phenols, and tannins, with alkaloids and phytosterols both absent [
16].
Despite reports of the traditional use of
E. utile to treat gastrointestinal diseases, sickle cell anaemia, and rheumatism in local communities across Africa, only a few studies have been able to corroborate these claims using standard pharmacological experiments. Unlike some other Meliaceae species like
Azadirachta indica that have been well-studied for their therapeutic activity against inflammation [
17], there is still a dearth of data on the pharmacological application of
E. utile in the management of inflammation. This is the knowledge gap this research project seeks to fill. In addition to deploying an acceptable pharmacological model to establish the anti-inflammatory activity of
E. utile bark extract in rats, this research is particularly novel in its drug presentation approach. It constitutes the first attempt at formulating the stem bark extract of
E. utile into a versatile dosage form like an emulgel and delivering it for potential topical administration.
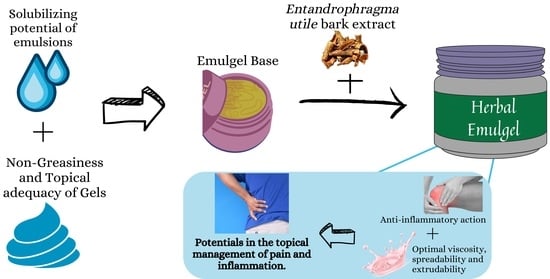
Drugs are designed in different ways to effectively deliver the active ingredients to their specific sites of action for the exertion of therapeutic action. Topical formulations which are directly applied to the skin have the advantage of bypassing first-pass metabolism, enhancing patient compliance also, preventing gastrointestinal incompatibility [
18]. Emulgels, a class of topical dosage forms, are formed when gels and emulsions are combined and their thixotropic, greaseless, easily spreadable, readily removable, emollient, non-staining, water-soluble, longer shelf life, bio-friendly, translucent, and aesthetically pleasant nature are just a few of the advantageous qualities for dermatological use. In this research, the anti-inflammatory activity of
Entandrophragma utile will be studied towards the formulation of an herbal-based topical dosage form which can potentially become a suitable alternative to the use of NSAIDs in the management of pain and inflammation.
4. Materials and Method
4.1. Chemicals and Equipment
Ethanol (BDH Chemicals Ltd., Dorset, England), Tween 80 (BDH Chemicals Ltd., Dorset, England), Span 20 (BDH Chemicals Ltd., Dorset, England), Methylparaben (BDH Chemicals Ltd., Dorset, England), Ethylparaben (BDH Chemicals Ltd., Dorset, England), Carbopol 940 (Guangdong Weng Jiang Chemical Reagent Co. Ltd., Guangdong, China), Ultrez Carbopol 20 (BDH Chemicals Ltd., Dorset, England), Liquid paraffin (BDH Chemicals Ltd., Dorset, England), Propylene glycol (BDH Chemicals Ltd., Dorset, England), triethanolamine (BDH Chemicals Ltd., Dorset, England), Clove oil (Ashifaul-Haqi Ltd., Oyo, Nigeria), Mentha oil (Ashifaul-Haqi Ltd., Oyo, Nigeria), Distilled water (Department of Pharmaceutical Chemistry, University of Ilorin, Kwara, Nigeria), Water bath (Fisher Scientific Company, Pittsburgh, PA, USA), Analytical weighing balance (Ohaus, Parsippany, NJ, USA), pH meter (Hanna Instruments Ltd., Bedfordshire, England),Viscometer (NDJ-5S, Rinch Industrial Co. Limited, Shanghai, China).
4.2. Collection and Identification of Plant
Fresh stem barks of Entandrophragma utile were gathered at Olokemeje, Oyo State (Nigeria). They were identified and verified at the Department of Plant Biology Herbarium Unit, University of Ilorin, Nigeria, in which voucher specimen (UILH/001/1325) was logged in.
4.3. Preparation of Extract
The stem barks were dried and ground using a mechanical grinder. The powdered plant materials were exhaustively extracted by maceration for 72 h using 90%
v/
v ethanol at room temperature with occasional stirring [
35], after which it was filtered and concentrated using a rotary evaporator. The dried extract which was reddish brown in colour was stored for later use. The percentage yield of the extract was determined using the formula:
4.4. Characterization of Extract
The extract of Entandrophragma utile was assessed for physical attributes like color, feel, and scent.
4.5. Anti-Inflammatory Assay of Extract
Every experiment was conducted in compliance with the recommendations set by University’s Ethical Review Committee (UERC). Using animal models, the anti-inflammatory assay was conducted. For the anti-inflammatory investigation, albino Wistar rats were allowed to acclimatize to the laboratory environment for seven days and were fasted for 18 h prior to the trial.
Carrageenan-Induced Rat Paw Edema Method
Five groups of twenty (20) rats each were equally divided. Four test groups received oral pretreatment with plant extract of dose levels of 50, 100, 200 mg/kg and diclofenac respectively an hour before Carrageenan (0.1 mL of 1% suspension in normal saline) was injected sub-plantarly into the rats’ right hind paws to produce acute inflammation. The measurements of the paw circumference were taken 24 h following the injection of carrageenan. The volume of oedema and the percentage of anti-inflammatory activity were computed using the difference between the readings [
36]. Using the following formula, the percentage value of oedema inhibition was determined:
where a = Initial paw thickness of the test group animal; b = Paw thickness of the control group animal following treatment; and x = Initial paw thickness of the test group animal [
37].
4.6. Emulgel Formulation
The emulgel was made using Mohamed’s (2004) methodology with a little modification [
38]. To create the gel bases, dispersing a weighed and sieved quantity of Carbopol 940 in a measured quantity of distilled utilizing a mechanical shaker to stir continuously at a reasonable speed, and letting it soak for the entire night. The Ultrez Carbopol 20 was dispersed in a measured quantity of distilled water and constantly stirred using mechanical shaker until gel formed. Both gels were mixed and properly stirred until a homogenous mixture was obtained. The pH of the gel was tested and adjusted by adding drops of triethanolamine. The emulsion’s aqueous phase was created by dissolving Tween 80 in filtered water, while the oil phase was created by dissolving Span 80 in light liquid paraffin. Propylene glycol was used to dissolve methyl and propylparaben before being combined with the aqueous phase. Because it was hydrophilic, the plant extract dissolved in the aqueous phase. The aqueous and oily phases were heated to 70–80 °C individually. Then, the oily phase was introduced to the aqueous phase and stirred continuously until it cooled to room temperature. To create the emulgel, the emulsion was combined with the gel in a 1:1 ratio while being gently stirred.
Table 6 shows the composition of several formulations.
4.7. Characterization of Emulgels
4.7.1. Physical Appearance
Visual inspection was conducted to assess the pH, color, homogeneity, consistency, grittiness, and phase separation of the manufactured emulgel formulations.
4.7.2. Measurement of pH
A digital pH meter (Hanna, England) was used to measure the pH of the emulgel formulations. The probe was left in the test preparation for two hours after one gram of gel was dissolved in 100 millilitres of distilled water. Each formulation’s pH was measured three times, and the average results were determined.
4.7.3. Spreadability
The diameter of the emulgel circle formed when emulgels are sandwiched between two glass plates of a specific weight were used to gauge how spreadable emulgels are. One glass plate was used to weigh an amount of each emulgel, while another glass plate was dropped from seven centimetres. The diameter of the emulgel spread’s circle was measured.
4.7.4. Viscosity
Utilizing an NDJ-5S viscometer (Spindle type no. 3) at 12 and 30 rpm, the estimation of viscosity was carried out. A significant amount of emulgel was placed in a beaker, and the spindle was plunged into it for five minutes before readings were obtained.
4.7.5. Extrudability
The extrudability test measures the weight needed to extrude a 0.5 cm emulgel ribbon from a lacquered collapsible aluminum tube in 10 s. The test was run three times, and the average values were determined. The following formula was then used to determine the extrudability:
4.7.6. Swelling Index
This is accomplished by adding 1 g of the emulgel to a 25 mL stoppered cylinder, adding water to reach the 20 mL mark, gently shaking the cylinder every 24 h, and letting it stand. The weights of the swollen mass were then calculated.
where % {SW} = Perfect Swelling Equilibrium.
4.7.7. Skin Irritation Test
The formulations were rubbed on the back of the palm and observed for any irritation.
4.8. Anti-Inflammatory Assay of Emulgels
CFA-Induced Arthritic Model
Experimental rats were divided into six (6) groups (Group 1–6), and they were treated with the formulated emulgels (EUE1–EUE5) and diclofenac (positive standard) respectively. EUE1 containing 0% of extract served as the negative control. Each animal’s paw volume at 0 days was measured before the experiment. Then, each rat’s right hind paw’s subplantar tissue was subcutaneously injected with 0.1 mL of CFA to cause adjuvant arthritis. For 27 days, the circumference of each paw was measured every day with a vernier caliper.
Using the following formula, the percentage value of oedema inhibition was determined:
where a = Initial paw thickness of the test group animal; b = Paw thickness of the control group animal following treatment; and x = Initial paw thickness of the test group animal. [
37,
39].
4.9. Statistical Analysis
Mean ± SEM was used to present the obtained results. For the statistical comparison, one-way analysis of variance (ANOVA) was employed, followed by the Dunnett post hoc multiple comparison tests for the anti-inflammatory examination. Graph-Pad Prism version 6 (GraphPad Software, Inc., San Diego, CA, USA) was used for statistical analysis. A significance threshold of p < 0.05 was used for analysis.