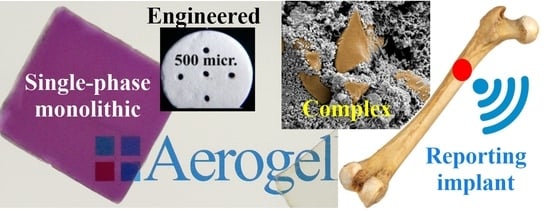
Aerogel-Based Materials in Bone and Cartilage Tissue Engineering—A Review with Future Implications
Abstract
:1. Introduction
2. Aerogel Microstructure
3. Formulation and Drying Methods
3.1. Formulation Methods
3.1.1. Casting, Molding
3.1.2. Freeze Casting
3.1.3. Supercritical Foaming
3.1.4. Stereolithography, 3D Printing
3.2. Drying Methods
3.2.1. Freeze Drying
3.2.2. Subcritical Drying
3.2.3. Supercritical Carbon Dioxide Drying
3.3. Post-Drying Workup and Shaping
4. Biomechanical, In Vitro and In Vivo Properties, Toxicity and Biocompatibility
4.1. Biomechanical Properties
4.2. In Vitro Testing Methods
4.2.1. Biocompatibility, Cell Viability
4.2.2. Antimicrobial Activity
4.2.3. Simulated Body Fluids
4.2.4. In Vitro Cell Studies
4.3. In Vivo Animal Testing Methods
4.3.1. General Considerations
4.3.2. The Role of Porosity
4.3.3. Selection of the Animal Species
4.3.4. Critical and Non-Critical Size Models
5. Aerogel-Based Materials and Structures for Bone Tissue Engineering
5.1. Building Materials of Aerogels and Their Scaffolds Used in Hard Tissue Engineering
5.2. Aerogel-Based Materials for Bone Substitution
5.2.1. Single-Component and Hybrid Aerogels
5.2.2. Nanofiber Aerogels
5.2.3. Aerogels as Matrix Materials
5.2.4. Aerogels as Guest Particles
5.2.5. Complex Aerogel Structures
6. Aerogel-Based Materials for Cartilage Tissue Engineering
7. Challenges, Opportunities and Future Trends
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jayakumar, P.; Di Silvio, L. Osteoblasts in Bone Tissue Engineering. Proc. Inst. Mech. Eng. 2010, 224, 1415–1440. [Google Scholar] [CrossRef]
- Ferreira, A.M.; Gentile, P.; Chiono, V.; Ciardelli, G. Collagen for Bone Tissue Regeneration. Acta Biomater. 2012, 8, 3191–3200. [Google Scholar] [CrossRef]
- Amini, A.R.; Laurencin, C.T.; Nukavarapu, S.P. Bone Tissue Engineering: Recent Advances and Challenges. Crit. Rev. Biomed. Eng. 2012, 40, 363–408. [Google Scholar] [CrossRef]
- Kazimierczak, P.; Przekora, A. Osteoconductive and Osteoinductive Surface Modifications of Biomaterials for Bone Regeneration: A Concise Review. Coatings 2020, 10, 971. [Google Scholar] [CrossRef]
- Lopes, D.; Martins-Cruz, C.; Oliveira, M.B.; Mano, J.F. Bone Physiology as Inspiration for Tissue Regenerative Therapies. Biomaterials 2018, 185, 240–275. [Google Scholar] [CrossRef]
- Albrektsson, T.; Johansson, C. Osteoinduction, Osteoconduction and Osseointegration. Eur. Spine J. 2001, 10, S96–S101. [Google Scholar] [CrossRef]
- Ansari, M. Bone Tissue Regeneration: Biology, Strategies and Interface Studies. Prog. Biomater. 2019, 8, 223–237. [Google Scholar] [CrossRef]
- Berrio, M.E.; Oñate, A.; Salas, A.; Fernández, K.; Meléndrez, M.F. Synthesis and Applications of Graphene Oxide Aerogels in Bone Tissue Regeneration: A Review. Mater. Today Chem. 2021, 20, 100422. [Google Scholar] [CrossRef]
- Matsiko, A.; Gleeson, J.P.; O’Brien, F.J. Scaffold Mean Pore Size Influences Mesenchymal Stem Cell Chondrogenic Differentiation and Matrix Deposition. Tissue Eng. Part A 2015, 21, 486–497. [Google Scholar] [CrossRef]
- Iglesias-Mejuto, A.; García-González, C.A. 3D-Printed Alginate-Hydroxyapatite Aerogel Scaffolds for Bone Tissue Engineering. Mater. Sci. Eng. C 2021, 131, 112525. [Google Scholar] [CrossRef]
- Włodarczyk-Biegun, M.K.; del Campo, A. 3D Bioprinting of Structural Proteins. Biomaterials 2017, 134, 180–201. [Google Scholar] [CrossRef] [PubMed]
- Puppi, D.; Chiellini, F.; Piras, A.M.; Chiellini, E. Polymeric Materials for Bone and Cartilage Repair. Prog. Polym. Sci. 2010, 35, 403–440. [Google Scholar] [CrossRef]
- Osorio, D.A.; Lee, B.E.J.; Kwiecien, J.M.; Wang, X.; Shahid, I.; Hurley, A.L.; Cranston, E.D.; Grandfield, K. Cross-Linked Cellulose Nanocrystal Aerogels as Viable Bone Tissue Scaffolds. Acta Biomater. 2019, 87, 152–165. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.-X.; Zhang, Y.; Hu, T.; Li, W.-X.; Li, Z.-L.; Hu, H.-J.; Zhu, S.-R.; Chen, W.-Z.; Zhou, C.-S.; Jiang, G.-B. Long-Term Antibacterial Composite via Alginate Aerogel Sustained Release of Antibiotics and Cu Used for Bone Tissue Bacteria Infection. Int. J. Biol. Macromol. 2021, 167, 1211–1220. [Google Scholar] [CrossRef] [PubMed]
- Horvat, G.; Xhanari, K.; Finšgar, M.; Gradišnik, L.; Maver, U.; Knez, Ž.; Novak, Z. Novel Ethanol-Induced Pectin–Xanthan Aerogel Coatings for Orthopedic Applications. Carbohydr. Polym. 2017, 166, 365–376. [Google Scholar] [CrossRef]
- Maleki, H.; Durães, L.; García-González, C.A.; del Gaudio, P.; Portugal, A.; Mahmoudi, M. Synthesis and Biomedical Applications of Aerogels: Possibilities and Challenges. Adv. Colloid Interface Sci. 2016, 236, 1–27. [Google Scholar] [CrossRef]
- Huang, G.-J.; Yu, H.-P.; Wang, X.-L.; Ning, B.-B.; Gao, J.; Shi, Y.-Q.; Zhu, Y.-J.; Duan, J.-L. Correction: Highly Porous and Elastic Aerogel Based on Ultralong Hydroxyapatite Nanowires for High-Performance Bone Regeneration and Neovascularization. J. Mater. Chem. B 2021, 9, 1277–1287. [Google Scholar] [CrossRef]
- Tevlek, A.; Atya, A.M.N.; Almemar, M.; Duman, M.; Gokcen, D.; Ganin, A.Y.; Yiu, H.H.P.; Aydin, H.M. Synthesis of Conductive Carbon Aerogels Decorated with β-Tricalcium Phosphate Nanocrystallites. Sci. Rep. 2020, 10, 5758. [Google Scholar] [CrossRef]
- Dong, S.; Zhang, Y.; Wan, J.; Cui, R.; Yu, X.; Zhao, G.; Lin, K. A Novel Multifunctional Carbon Aerogel-Coated Platform for Osteosarcoma Therapy and Enhanced Bone Regeneration. J. Mater. Chem. B 2020, 8, 368–379. [Google Scholar] [CrossRef]
- Wan, Y.; Chang, P.; Yang, Z.; Xiong, G.; Liu, P.; Luo, H. Constructing a Novel Three-Dimensional Scaffold with Mesoporous TiO 2 Nanotubes for Potential Bone Tissue Engineering. J. Mater. Chem. B 2015, 3, 5595–5602. [Google Scholar] [CrossRef]
- Richardson, J.B.; Caterson, B.; Evans, E.H.; Ashton, B.A.; Roberts, S. Repair of Human Articular Cartilage after Implantation of Autologous Chondrocytes. J. Bone Jt. Surg. Br. 1999, 81, 1064–1068. [Google Scholar] [CrossRef]
- Feng, B.; Ji, T.; Wang, X.; Fu, W.; Ye, L.; Zhang, H.; Li, F. Engineering Cartilage Tissue Based on Cartilage-Derived Extracellular Matrix cECM/PCL Hybrid Nanofibrous Scaffold. Mater. Des. 2020, 193, 108773. [Google Scholar] [CrossRef]
- Chen, Y.; Shafiq, M.; Liu, M.; Morsi, Y.; Mo, X. Advanced Fabrication for Electrospun Three-Dimensional Nanofiber Aerogels and Scaffolds. Bioact. Mater. 2020, 5, 963–979. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Fang, J.; Fu, L.; Chen, L.; Dai, W.; Huang, H.; Wang, J.; Zhang, X.; Cai, Q.; Yang, X. Gradient Fibrous Aerogel Conjugated with Chemokine Peptide for Regulating Cell Differentiation and Facilitating Osteochondral Regeneration. Chem. Eng. J. 2021, 422, 130428. [Google Scholar] [CrossRef]
- Chainani, A.; Hippensteel, K.J.; Kishan, A.; Garrigues, N.W.; Ruch, D.S.; Guilak, F.; Little, D. Multilayered Electrospun Scaffolds for Tendon Tissue Engineering. Tissue Eng. Part A 2013, 19, 2594–2604. [Google Scholar] [CrossRef]
- Shim, I.K.; Suh, W.H.; Lee, S.Y.; Lee, S.H.; Heo, S.J.; Lee, M.C.; Lee, S.J. Chitosan Nano-/Microfibrous Double-Layered Membrane with Rolled-up Three-Dimensional Structures for Chondrocyte Cultivation. J. Biomed. Mater. Res. A 2009, 90, 595–602. [Google Scholar] [CrossRef]
- Li, R.; Wang, H.; John, J.V.; Song, H.; Teusink, M.J.; Xie, J. 3D Hybrid Nanofiber Aerogels Combining with Nanoparticles Made of a Biocleavable and Targeting Polycation and MiR-26a for Bone Repair. Adv. Funct. Mater. 2020, 30, 2005531. [Google Scholar] [CrossRef]
- Wang, L.; Qiu, Y.; Lv, H.; Si, Y.; Liu, L.; Zhang, Q.; Cao, J.; Yu, J.; Li, X.; Ding, B. 3D Superelastic Scaffolds Constructed from Flexible Inorganic Nanofibers with Self-Fitting Capability and Tailorable Gradient for Bone Regeneration. Adv. Funct. Mater. 2019, 29, 1901407. [Google Scholar] [CrossRef]
- Kistler, S.S. Coherent Expanded Aerogels and Jellies. Nature 1931, 127, 741. [Google Scholar] [CrossRef]
- Hüsing, N.; Schubert, U. Aerogels—Airy Materials: Chemistry, Structure, and Properties. Angew. Chem. Int. Ed. 1998, 37, 22–45. [Google Scholar] [CrossRef]
- Karamikamkar, S.; Naguib, H.E.; Park, C.B. Advances in Precursor System for Silica-Based Aerogel Production toward Improved Mechanical Properties, Customized Morphology, and Multifunctionality: A Review. Adv. Colloid Interface Sci. 2020, 276, 102101. [Google Scholar] [CrossRef]
- Ganesamoorthy, R.; Vadivel, V.K.; Kumar, R.; Kushwaha, O.S.; Mamane, H. Aerogels for Water Treatment: A Review. J. Clean. Prod. 2021, 329, 129713. [Google Scholar] [CrossRef]
- Hong, J.-Y.; Yun, S.; Wie, J.J.; Zhang, X.; Dresselhaus, M.S.; Kong, J.; Park, H.S. Cartilage-Inspired Superelastic Ultradurable Graphene Aerogels Prepared by the Selective Gluing of Intersheet Joints. Nanoscale 2016, 8, 12900–12909. [Google Scholar] [CrossRef]
- Boday, D.J.; Keng, P.Y.; Muriithi, B.; Pyun, J.; Loy, D.A. Mechanically Reinforced Silica Aerogel Nanocomposites via Surface Initiated Atom Transfer Radical Polymerizations. J. Mater. Chem. 2010, 20, 6863. [Google Scholar] [CrossRef]
- Leventis, N. Three-Dimensional Core-Shell Superstructures: Mechanically Strong Aerogels. Acc. Chem. Res. 2007, 40, 874–884. [Google Scholar] [CrossRef]
- Randall, J.P.; Meador, M.A.B.; Jana, S.C. Tailoring Mechanical Properties of Aerogels for Aerospace Applications. ACS Appl. Mater. Interfaces 2011, 3, 613–626. [Google Scholar] [CrossRef] [PubMed]
- Leventis, N.; Sotiriou-Leventis, C.; Zhang, G.; Rawashdeh, A.-M.M. Nanoengineering Strong Silica Aerogels. Nano Lett. 2002, 2, 957–960. [Google Scholar] [CrossRef]
- Lázár, I.; Fábián, I. A Continuous Extraction and Pumpless Supercritical CO2 Drying System for Laboratory-Scale Aerogel Production. Gels 2016, 2, 26. [Google Scholar] [CrossRef] [PubMed]
- Scotti, K.L.; Dunand, D.C. Freeze Casting—A Review of Processing, Microstructure and Properties via the Open Data Repository, FreezeCasting.Net. Prog. Mater. Sci. 2018, 94, 243–305. [Google Scholar] [CrossRef]
- Li, W.L.; Lu, K.; Walz, J.Y. Freeze Casting of Porous Materials: Review of Critical Factors in Microstructure Evolution. Int. Mater. Rev. 2012, 57, 37–60. [Google Scholar] [CrossRef]
- Tetik, H.; Feng, D.; Oxandale, S.W.; Yang, G.; Zhao, K.; Feist, K.; Shah, N.; Liao, Y.; Leseman, Z.C.; Lin, D. Bioinspired Manufacturing of Aerogels with Precisely Manipulated Surface Microstructure through Controlled Local Temperature Gradients. ACS Appl. Mater. Interfaces 2021, 13, 924–931. [Google Scholar] [CrossRef] [PubMed]
- Maleki, H.; Shahbazi, M.-A.; Montes, S.; Hosseini, S.H.; Eskandari, M.R.; Zaunschirm, S.; Verwanger, T.; Mathur, S.; Milow, B.; Krammer, B.; et al. Mechanically Strong Silica-Silk Fibroin Bioaerogel: A Hybrid Scaffold with Ordered Honeycomb Micromorphology and Multiscale Porosity for Bone Regeneration. ACS Appl. Mater. Interfaces 2019, 11, 17256–17269. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Tian, Y.; Peng, X. Applications and Challenges of Supercritical Foaming Technology. Polymers 2023, 15, 402. [Google Scholar] [CrossRef] [PubMed]
- García-González, C.A.; Concheiro, A.; Alvarez-Lorenzo, C. Processing of Materials for Regenerative Medicine Using Supercritical Fluid Technology. Bioconjug. Chem. 2015, 26, 1159–1171. [Google Scholar] [CrossRef] [PubMed]
- Goimil, L.; Braga, M.E.M.; Dias, A.M.A.; Gómez-Amoza, J.L.; Concheiro, A.; Alvarez-Lorenzo, C.; de Sousa, H.C.; García-González, C.A. Supercritical Processing of Starch Aerogels and Aerogel-Loaded Poly(ε-Caprolactone) Scaffolds for Sustained Release of Ketoprofen for Bone Regeneration. J. CO2 Util. 2017, 18, 237–249. [Google Scholar] [CrossRef]
- Goimil, L.; Santos-Rosales, V.; Delgado, A.; Évora, C.; Reyes, R.; Lozano-Pérez, A.A.; Aznar-Cervantes, S.D.; Cenis, J.L.; Gómez-Amoza, J.L.; Concheiro, A.; et al. scCO2-Foamed Silk Fibroin Aerogel/Poly(ε-Caprolactone) Scaffolds Containing Dexamethasone for Bone Regeneration. J. CO2 Util. 2019, 31, 51–64. [Google Scholar] [CrossRef]
- Badhe, R.V.; Chatterjee, A.; Bijukumar, D.; Mathew, M.T. Current Advancements in Bio-Ink Technology for Cartilage and Bone Tissue Engineering. Bone 2023, 171, 116746. [Google Scholar] [CrossRef]
- Iglesias-Mejuto, A.; García-González, C.A. 3D-Printed, Dual Crosslinked and Sterile Aerogel Scaffolds for Bone Tissue Engineering. Polymers 2022, 14, 1211. [Google Scholar] [CrossRef]
- Ng, P.; Pinho, A.R.; Gomes, M.C.; Demidov, Y.; Krakor, E.; Grume, D.; Herb, M.; Lê, K.; Mano, J.; Mathur, S.; et al. Fabrication of Antibacterial, Osteo-Inductor 3D Printed Aerogel-Based Scaffolds by Incorporation of Drug Laden Hollow Mesoporous Silica Microparticles into the Self-Assembled Silk Fibroin Biopolymer. Macromol. Biosci. 2022, 22, 2100442. [Google Scholar] [CrossRef]
- Bhagat, S.D.; Oh, C.-S.; Kim, Y.-H.; Ahn, Y.-S.; Yeo, J.-G. Methyltrimethoxysilane Based Monolithic Silica Aerogels via Ambient Pressure Drying. Microporous Mesoporous Mater. 2007, 100, 350–355. [Google Scholar] [CrossRef]
- Kirkbir, F.; Murata, H.; Meyers, D.; Chaudhuri, S.R. Drying of Aerogels in Different Solvents between Atmospheric and Supercritical Pressures. J. Non-Cryst. Solids 1998, 225, 14–18. [Google Scholar] [CrossRef]
- Tang, A.; Ji, J.; Li, J.; Liu, W.; Wang, J.; Sun, Q.; Li, Q. Nanocellulose/PEGDA Aerogels with Tunable Poisson’s Ratio Fabricated by Stereolithography for Mouse Bone Marrow Mesenchymal Stem Cell Culture. Nanomaterials 2021, 11, 603. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, S.; Baheiraei, N.; Shahrezaee, M. Biomimetic Reduced Graphene Oxide Coated Collagen Scaffold for in Situ Bone Regeneration. Sci. Rep. 2021, 11, 16783. [Google Scholar] [CrossRef] [PubMed]
- Asha, S.; Ananth, A.N.; Jose, S.P.; Rajan, M.A.J. Reduced Graphene Oxide Aerogel Networks with Soft Interfacial Template for Applications in Bone Tissue Regeneration. Appl. Nanosci. 2018, 8, 395–405. [Google Scholar] [CrossRef]
- Sun, D.; Liu, W.; Tang, A.; Guo, F.; Xie, W. A New PEGDA/CNF Aerogel-Wet Hydrogel Scaffold Fabricated by a Two-Step Method. Soft Matter 2019, 15, 8092–8101. [Google Scholar] [CrossRef]
- Ferreira, F.V.; Souza, L.P.; Martins, T.M.M.; Lopes, J.H.; Mattos, B.D.; Mariano, M.; Pinheiro, I.F.; Valverde, T.M.; Livi, S.; Camilli, J.A.; et al. Nanocellulose/Bioactive Glass Cryogels as Scaffolds for Bone Regeneration. Nanoscale 2019, 11, 19842–19849. [Google Scholar] [CrossRef]
- Zhang, Y.; Yin, C.; Cheng, Y.; Huang, X.; Liu, K.; Cheng, G.; Li, Z. Electrospinning Nanofiber-Reinforced Aerogels for the Treatment of Bone Defects. Adv. Wound Care 2020, 9, 441–452. [Google Scholar] [CrossRef]
- Chen, Z.-J.; Shi, H.-H.; Zheng, L.; Zhang, H.; Cha, Y.-Y.; Ruan, H.-X.; Zhang, Y.; Zhang, X.-C. A New Cancellous Bone Material of Silk Fibroin/Cellulose Dual Network Composite Aerogel Reinforced by Nano-Hydroxyapatite Filler. Int. J. Biol. Macromol. 2021, 182, 286–297. [Google Scholar] [CrossRef]
- Singh, M.; Sandhu, B.; Scurto, A.; Berkland, C.; Detamore, M.S. Microsphere-Based Scaffolds for Cartilage Tissue Engineering: Using Subcritical CO2 as a Sintering Agent. Acta Biomater. 2010, 6, 137–143. [Google Scholar] [CrossRef]
- Bhamidipati, M.; Sridharan, B.; Scurto, A.M.; Detamore, M.S. Subcritical CO2 Sintering of Microspheres of Different Polymeric Materials to Fabricate Scaffolds for Tissue Engineering. Mater. Sci. Eng. C 2013, 33, 4892–4899. [Google Scholar] [CrossRef]
- Vazhayal, L.; Talasila, S.; Abdul Azeez, P.M.; Solaiappan, A. Mesochanneled Hierarchically Porous Aluminosiloxane Aerogel Microspheres as a Stable Support for pH-Responsive Controlled Drug Release. ACS Appl. Mater. Interfaces 2014, 6, 15564–15574. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Peces, M.V.; Pérez-Moreno, A.; de-los-Santos, D.M.; Mesa-Díaz, M.d.M.; Pinaglia-Tobaruela, G.; Vilches-Pérez, J.I.; Fernández-Montesinos, R.; Salido, M.; de la Rosa-Fox, N.; Piñero, M. Chitosan-GPTMS-Silica Hybrid Mesoporous Aerogels for Bone Tissue Engineering. Polymers 2020, 12, 2723. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Ruíz, A.; Escobar-García, D.M.; Quintana, M.; Pozos-Guillén, A.; Flores, H. Synthesis and Characterization of a New Collagen-Alginate Aerogel for Tissue Engineering. J. Nanomater. 2019, 2019, 2875375. [Google Scholar] [CrossRef]
- Quraishi, S.; Martins, M.; Barros, A.A.; Gurikov, P.; Raman, S.P.; Smirnova, I.; Duarte, A.R.C.; Reis, R.L. Novel Non-Cytotoxic Alginate–Lignin Hybrid Aerogels as Scaffolds for Tissue Engineering. J. Supercrit. Fluids 2015, 105, 1–8. [Google Scholar] [CrossRef]
- Martins, M.; Barros, A.A.; Quraishi, S.; Gurikov, P.; Raman, S.P.; Smirnova, I.; Duarte, A.R.C.; Reis, R.L. Preparation of Macroporous Alginate-Based Aerogels for Biomedical Applications. J. Supercrit. Fluids 2015, 106, 152–159. [Google Scholar] [CrossRef]
- Szabó, B.A.; Kiss, L.; Manó, S.; Jónás, Z.; Lázár, I.; Fábián, I.; Dezső, B.; Csernátony, Z. The Examination of Aerogel Composite Artificial Bone Substitutes in Animal Models. Biomech. Hung. 2013, 6, 52. [Google Scholar] [CrossRef]
- Hegedűs, C.; Czibulya, Z.; Tóth, F.; Dezső, B.; Hegedűs, V.; Boda, R.; Horváth, D.; Csík, A.; Fábián, I.; Tóth-Győri, E.; et al. The Effect of Heat Treatment of β-Tricalcium Phosphate-Containing Silica-Based Bioactive Aerogels on the Cellular Metabolism and Proliferation of MG63 Cells. Biomedicines 2022, 10, 662. [Google Scholar] [CrossRef]
- Kuttor, A.; Szalóki, M.; Rente, T.; Kerényi, F.; Bakó, J.; Fábián, I.; Lázár, I.; Jenei, A.; Hegedüs, C. Preparation and Application of Highly Porous Aerogel-Based Bioactive Materials in Dentistry. Front. Mater. Sci. 2014, 8, 46–52. [Google Scholar] [CrossRef]
- Lázár, I.; Manó, S.; Jónás, Z.; Kiss, L.; Fábián, I.; Csernátony, Z. Mesoporous Silica-Calcium Phosphate Composites for Experimental Bone Substitution. Biomech. Hung. 2010, 3, 151. [Google Scholar] [CrossRef]
- Hegedűs, V.; Kerényi, F.; Boda, R.; Horváth, D.; Lázár, I.; Tóth-Győri, E.; Dezső, B.; Hegedus, C. β-Tricalcium Phosphate-Silica Aerogel as an Alternative Bioactive Ceramic for the Potential Use in Dentistry. Adv. Appl. Ceram. 2020, 119, 364–371. [Google Scholar] [CrossRef]
- Rubenstein, D.A.; Lu, H.; Mahadik, S.S.; Leventis, N.; Yin, W. Characterization of the Physical Properties and Biocompatibility of Polybenzoxazine-Based Aerogels for Use as a Novel Hard-Tissue Scaffold. J. Biomater. Sci. Polym. Ed. 2012, 23, 1171–1184. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.; Zhang, X. (Eds.) Definitions of Biomaterials for the Twenty-First Century: Proceedings of a Consensus Conference Held in Chengdu, People’s Republic of China, June 11th and 12th 2018, Organized under the Auspices of the International Union of Societies for Biomaterials Science & Engineering; Hosted and Supported by Sichuan University, Chengdu and the Chinese Society for Biomaterials, China; Materials Today; Elsevier: Amsterdam, The Netherlands, 2019; ISBN 978-0-12-818291-8. [Google Scholar]
- Peters, K.; Unger, R.E.; Kirkpatrick, C.J. Biocompatibility Testing. In Biomedical Materials; Narayan, R., Ed.; Springer International Publishing: Cham, 2021; pp. 423–453. ISBN 978-3-030-49205-2. [Google Scholar]
- Bongio, M.; van den Beucken, J.J.J.P.; Leeuwenburgh, S.C.G.; Jansen, J.A. Development of Bone Substitute Materials: From ‘Biocompatible’ to ‘Instructive’. J. Mater. Chem. 2010, 20, 8747. [Google Scholar] [CrossRef]
- Cullinane, D.M.; Einhorn, T.A. Biomechanics of Bone. In Principles of Bone Biology; Elsevier: Amsterdam, The Netherlands, 2002; pp. 17–32. ISBN 978-0-12-098652-1. [Google Scholar]
- Manó, S.; Ferencz, G.; Lázár, I.; Fábián, I.; Csernátony, Z. Determination of the Application Characteristics of the Slooff-Technique with Nano-Composite Bone Substitution Material by Biomechanical Tests. Biomech. Hung. 2013, 6, 64. [Google Scholar] [CrossRef]
- Perez-Moreno, A.; Reyes-Peces, M.d.l.V.; de los Santos, D.M.; Pinaglia-Tobaruela, G.; de la Orden, E.; Vilches-Pérez, J.I.; Salido, M.; Piñero, M.; de la Rosa-Fox, N. Hydroxyl Groups Induce Bioactivity in Silica/Chitosan Aerogels Designed for Bone Tissue Engineering. In Vitro Model for the Assessment of Osteoblasts Behavior. Polymers 2020, 12, 2802. [Google Scholar] [CrossRef]
- Karamat-Ullah, N.; Demidov, Y.; Schramm, M.; Grumme, D.; Auer, J.; Bohr, C.; Brachvogel, B.; Maleki, H. 3D Printing of Antibacterial, Biocompatible, and Biomimetic Hybrid Aerogel-Based Scaffolds with Hierarchical Porosities via Integrating Antibacterial Peptide-Modified Silk Fibroin with Silica Nanostructure. ACS Biomater. Sci. Eng. 2021, 7, 4545–4556. [Google Scholar] [CrossRef]
- Weng, L.; Boda, S.K.; Wang, H.; Teusink, M.J.; Shuler, F.D.; Xie, J. Novel 3D Hybrid Nanofiber Aerogels Coupled with BMP-2 Peptides for Cranial Bone Regeneration. Adv. Healthc. Mater. 2018, 7, 1701415. [Google Scholar] [CrossRef]
- Liu, S.; Zhou, C.; Mou, S.; Li, J.; Zhou, M.; Zeng, Y.; Luo, C.; Sun, J.; Wang, Z.; Xu, W. Biocompatible Graphene Oxide–Collagen Composite Aerogel for Enhanced Stiffness and in Situ Bone Regeneration. Mater. Sci. Eng. C 2019, 105, 110137. [Google Scholar] [CrossRef]
- Liu, M.; Shafiq, M.; Sun, B.; Wu, J.; Wang, W.; EL-Newehy, M.; EL-Hamshary, H.; Morsi, Y.; Ali, O.; Khan, A.U.R.; et al. Composite Superelastic Aerogel Scaffolds Containing Flexible SiO 2 Nanofibers Promote Bone Regeneration. Adv. Healthc. Mater. 2022, 11, 2200499. [Google Scholar] [CrossRef]
- Souto-Lopes, M.; Grenho, L.; Manrique, Y.A.; Dias, M.M.; Fernandes, M.H.; Monteiro, F.J.; Salgado, C.L. Full Physicochemical and Biocompatibility Characterization of a Supercritical CO2 Sterilized Nano-Hydroxyapatite/Chitosan Biodegradable Scaffold for Periodontal Bone Regeneration. Biomater. Adv. 2023, 146, 213280. [Google Scholar] [CrossRef]
- Ruphuy, G.; Souto-Lopes, M.; Paiva, D.; Costa, P.; Rodrigues, A.E.; Monteiro, F.J.; Salgado, C.L.; Fernandes, M.H.; Lopes, J.C.; Dias, M.M.; et al. Supercritical CO 2 Assisted Process for the Production of High-purity and Sterile Nano-hydroxyapatite/Chitosan Hybrid Scaffolds. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 965–975. [Google Scholar] [CrossRef]
- Reyes-Peces, M.V.; Fernández-Montesinos, R.; Mesa-Díaz, M.D.M.; Vilches-Pérez, J.I.; Cárdenas-Leal, J.L.; De La Rosa-Fox, N.; Salido, M.; Piñero, M. Structure-Related Mechanical Properties and Bioactivity of Silica–Gelatin Hybrid Aerogels for Bone Regeneration. Gels 2023, 9, 67. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Moreno, A.; Piñero, M.; Fernández-Montesinos, R.; Pinaglia-Tobaruela, G.; Reyes-Peces, M.V.; Mesa-Díaz, M.D.M.; Vilches-Pérez, J.I.; Esquivias, L.; De La Rosa-Fox, N.; Salido, M. Chitosan-Silica Hybrid Biomaterials for Bone Tissue Engineering: A Comparative Study of Xerogels and Aerogels. Gels 2023, 9, 383. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.-J.; Zhang, Y.; Zheng, L.; Zhang, H.; Shi, H.-H.; Zhang, X.-C.; Liu, B. Mineralized Self-Assembled Silk Fibroin/Cellulose Interpenetrating Network Aerogel for Bone Tissue Engineering. Biomater. Adv. 2022, 134, 112549. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Li, D.; Chen, X.; Jiang, L. Biomimetic Cuttlebone Polyvinyl Alcohol/Carbon Nanotubes/Hydroxyapatite Aerogel Scaffolds Enhanced Bone Regeneration. Colloids Surf. B Biointerfaces 2022, 210, 112221. [Google Scholar] [CrossRef] [PubMed]
- Souto-Lopes, M.; Fernandes, M.H.; Monteiro, F.J.; Salgado, C.L. Bioengineering Composite Aerogel-Based Scaffolds That Influence Porous Microstructure, Mechanical Properties and In Vivo Regeneration for Bone Tissue Application. Materials 2023, 16, 4483. [Google Scholar] [CrossRef]
- Ibrahim, A.; Magliulo, N.; Groben, J.; Padilla, A.; Akbik, F.; Abdel Hamid, Z. Hardness, an Important Indicator of Bone Quality, and the Role of Collagen in Bone Hardness. J. Funct. Biomater. 2020, 11, 85. [Google Scholar] [CrossRef]
- Moner-Girona, M.; Roig, A.; Molins, E.; Martínez, E.; Esteve, J. Micromechanical Properties of Silica Aerogels. Appl. Phys. Lett. 1999, 75, 653–655. [Google Scholar] [CrossRef]
- Woignier, T.; Primera, J.; Alaoui, A.; Despetis, F.; Calas-Etienne, S.; Faivre, A.; Duffours, L.; Levelut, C.; Etienne, P. Techniques for Characterizing the Mechanical Properties of Aerogels. J. Sol-Gel Sci. Technol. 2020, 93, 6–27. [Google Scholar] [CrossRef]
- Revin, V.V.; Pestov, N.A.; Shchankin, M.V.; Mishkin, V.P.; Platonov, V.I.; Uglanov, D.A. A Study of the Physical and Mechanical Properties of Aerogels Obtained from Bacterial Cellulose. Biomacromolecules 2019, 20, 1401–1411. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Gao, C.; Gao, W. A Review on Elastic Graphene Aerogels: Design, Preparation, and Applications. J. Polym. Sci. 2022, 60, 2239–2261. [Google Scholar] [CrossRef]
- Liu, C.; Chu, D.; Kalantar-Zadeh, K.; George, J.; Young, H.A.; Liu, G. Cytokines: From Clinical Significance to Quantification. Adv. Sci. 2021, 8, 2004433. [Google Scholar] [CrossRef] [PubMed]
- Przekora, A. The Summary of the Most Important Cell-Biomaterial Interactions That Need to Be Considered during in Vitro Biocompatibility Testing of Bone Scaffolds for Tissue Engineering Applications. Mater. Sci. Eng. C 2019, 97, 1036–1051. [Google Scholar] [CrossRef] [PubMed]
- Kamiloglu, S.; Sari, G.; Ozdal, T.; Capanoglu, E. Guidelines for Cell Viability Assays. Food Front. 2020, 1, 332–349. [Google Scholar] [CrossRef]
- Tian, M.; Ma, Y.; Lin, W. Fluorescent Probes for the Visualization of Cell Viability. Acc. Chem. Res. 2019, 52, 2147–2157. [Google Scholar] [CrossRef]
- Confederat, L.G.; Tuchilus, C.G.; Dragan, M.; Sha’at, M.; Dragostin, O.M. Preparation and Antimicrobial Activity of Chitosan and Its Derivatives: A Concise Review. Molecules 2021, 26, 3694. [Google Scholar] [CrossRef]
- Yahya, E.B.; Jummaat, F.; Amirul, A.A.; Adnan, A.S.; Olaiya, N.G.; Abdullah, C.K.; Rizal, S.; Mohamad Haafiz, M.K.; Khalil, H.P.S.A. A Review on Revolutionary Natural Biopolymer-Based Aerogels for Antibacterial Delivery. Antibiotics 2020, 9, 648. [Google Scholar] [CrossRef]
- Abdul Khalil, H.P.S.; Adnan, A.S.; Yahya, E.B.; Olaiya, N.G.; Safrida, S.; Hossain, M.d.S.; Balakrishnan, V.; Gopakumar, D.A.; Abdullah, C.K.; Oyekanmi, A.A.; et al. A Review on Plant Cellulose Nanofibre-Based Aerogels for Biomedical Applications. Polymers 2020, 12, 1759. [Google Scholar] [CrossRef]
- García-González, C.A.; Barros, J.; Rey-Rico, A.; Redondo, P.; Gómez-Amoza, J.L.; Concheiro, A.; Alvarez-Lorenzo, C.; Monteiro, F.J. Antimicrobial Properties and Osteogenicity of Vancomycin-Loaded Synthetic Scaffolds Obtained by Supercritical Foaming. ACS Appl. Mater. Interfaces 2018, 10, 3349–3360. [Google Scholar] [CrossRef]
- Zahran, M.; Marei, A.H. Innovative Natural Polymer Metal Nanocomposites and Their Antimicrobial Activity. Int. J. Biol. Macromol. 2019, 136, 586–596. [Google Scholar] [CrossRef]
- Kokubo, T.; Miyaji, F.; Kim, H.-M.; Nakamura, T. Spontaneous Formation of Bonelike Apatite Layer on Chemically Treated Titanium Metals. J. Am. Ceram. Soc. 1996, 79, 1127–1129. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How Useful Is SBF in Predicting in Vivo Bone Bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef] [PubMed]
- Reséndiz-Hernández, P.J.; Cortés-Hernández, D.A.; Méndez Nonell, J.; Escobedo-Bocardo, J.C. Bioactive and Biocompatible Silica/Pseudowollastonite Aerogels. Adv. Sci. Technol. 2014, 96, 21–26. [Google Scholar] [CrossRef]
- Müller, L.; Müller, F.A. Preparation of SBF with Different HCO3- Content and Its Influence on the Composition of Biomimetic Apatites. Acta Biomater. 2006, 2, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Győri, E.; Fábián, I.; Lázár, I. Effect of the Chemical Composition of Simulated Body Fluids on Aerogel-Based Bioactive Composites. J. Compos. Sci. 2017, 1, 15. [Google Scholar] [CrossRef]
- Vallés Lluch, A.; Gallego Ferrer, G.; Monleón Pradas, M. Biomimetic Apatite Coating on P(EMA-Co-HEA)/SiO2 Hybrid Nanocomposites. Polymer 2009, 50, 2874–2884. [Google Scholar] [CrossRef]
- Pizzoferrato, A.; Ciapetti, G.; Stea, S.; Cenni, E.; Arciola, C.R.; Granchi, D. Lucia Cell Culture Methods for Testing Biocompatibility. Clin. Mater. 1994, 15, 173–190. [Google Scholar] [CrossRef]
- Kirkpatrick, C.J.; Bittinger, F.; Wagner, M.; Köhler, H.; van Kooten, T.G.; Klein, C.L.; Otto, M. Current Trends in Biocompatibility Testing. Proc. Inst. Mech. Eng. 1998, 212, 75–84. [Google Scholar] [CrossRef]
- Regenerative Medicine Institute, National Centre for Biomedical Engineering Science, National University of Ireland, Galway; Czekanska, E.; Stoddart, M.; Richards, R.; Hayes, J. In Search of an Osteoblast Cell Model for In Vitro Research. Eur. Cell Mater. 2012, 24, 1–17. [Google Scholar] [CrossRef]
- Lindner, C.; Pröhl, A.; Abels, M.; Löffler, T.; Batinic, M.; Jung, O.; Barbeck, M. Specialized Histological and Histomorphometrical Analytical Methods for Biocompatibility Testing of Biomaterials for Maxillofacial Surgery in (Pre-) Clinical Studies. Vivo 2020, 34, 3137–3152. [Google Scholar] [CrossRef]
- Wittkowske, C.; Reilly, G.C.; Lacroix, D.; Perrault, C.M. In Vitro Bone Cell Models: Impact of Fluid Shear Stress on Bone Formation. Front. Bioeng. Biotechnol. 2016, 4, 87. [Google Scholar] [CrossRef]
- Bellucci, D.; Veronesi, E.; Dominici, M.; Cannillo, V. On the in Vitro Biocompatibility Testing of Bioactive Glasses. Materials 2020, 13, 1816. [Google Scholar] [CrossRef] [PubMed]
- Kargozar, S.; Mozafari, M.; Hamzehlou, S.; Brouki Milan, P.; Kim, H.-W.; Baino, F. Bone Tissue Engineering Using Human Cells: A Comprehensive Review on Recent Trends, Current Prospects, and Recommendations. Appl. Sci. 2019, 9, 174. [Google Scholar] [CrossRef]
- Colnot, C. Cell Sources for Bone Tissue Engineering: Insights from Basic Science. Tissue Eng. Part B Rev. 2011, 17, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Christenson, R.H. Biochemical Markers of Bone Metabolism: An Overview. Clin. Biochem. 1997, 30, 573–593. [Google Scholar] [CrossRef]
- Ge, J.; Li, M.; Zhang, Q.; Yang, C.Z.; Wooley, P.H.; Chen, X.; Yang, S.-Y. Silica Aerogel Improves the Biocompatibility in a Poly-ε-Caprolactone Composite Used as a Tissue Engineering Scaffold. Int. J. Polym. Sci. 2013, 2013, 402859. [Google Scholar] [CrossRef]
- Ratner, B.D. A Pore Way to Heal and Regenerate: 21st Century Thinking on Biocompatibility. Regen. Biomater. 2016, 3, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Karageorgiou, V.; Kaplan, D. Porosity of 3D Biomaterial Scaffolds and Osteogenesis. Biomaterials 2005, 26, 5474–5491. [Google Scholar] [CrossRef]
- Nuss, K.M.; Auer, J.A.; Boos, A.; Rechenberg, B. von An Animal Model in Sheep for Biocompatibility Testing of Biomaterials in Cancellous Bones. BMC Musculoskelet. Disord. 2006, 7, 67. [Google Scholar] [CrossRef]
- Mendes, S.C.; Reis, R.L.; Bovell, Y.P.; Cunha, A.M.; van Blitterswijk, C.A.; de Bruijn, J.D. Biocompatibility Testing of Novel Starch-Based Materials with Potential Application in Orthopaedic Surgery: A Preliminary Study. Biomaterials 2001, 22, 2057–2064. [Google Scholar] [CrossRef]
- Peric, M.; Dumic-Cule, I.; Grcevic, D.; Matijasic, M.; Verbanac, D.; Paul, R.; Grgurevic, L.; Trkulja, V.; Bagi, C.M.; Vukicevic, S. The Rational Use of Animal Models in the Evaluation of Novel Bone Regenerative Therapies. Bone 2015, 70, 73–86. [Google Scholar] [CrossRef]
- Gomes, P.S.; Fernandes, M.H. Rodent Models in Bone-Related Research: The Relevance of Calvarial Defects in the Assessment of Bone Regeneration Strategies. Lab. Anim. 2011, 45, 14–24. [Google Scholar] [CrossRef] [PubMed]
- AO Research Institute, AO Foundation, Clavadelerstrasse 8, Davos, Switzerland; Pearce, A.; Richards, R.; Milz, S.; Schneider, E.; Pearce, S. Animal Models for Implant Biomaterial Research in Bone: A Review. Eur. Cells Mater. 2007, 13, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chen, S.-K.; Li, L.; Qin, L.; Wang, X.-L.; Lai, Y.-X. Bone Defect Animal Models for Testing Efficacy of Bone Substitute Biomaterials. J. Orthop. Transl. 2015, 3, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Spicer, P.P.; Kretlow, J.D.; Young, S.; Jansen, J.A.; Kasper, F.K.; Mikos, A.G. Evaluation of Bone Regeneration Using the Rat Critical Size Calvarial Defect. Nat. Protoc. 2012, 7, 1918–1929. [Google Scholar] [CrossRef]
- Vareda, J.P.; Lamy-Mendes, A.; Durães, L. A Reconsideration on the Definition of the Term Aerogel Based on Current Drying Trends. Microporous Mesoporous Mater. 2018, 258, 211–216. [Google Scholar] [CrossRef]
- García-González, C.A.; Budtova, T.; Durães, L.; Erkey, C.; Del Gaudio, P.; Gurikov, P.; Koebel, M.; Liebner, F.; Neagu, M.; Smirnova, I. An Opinion Paper on Aerogels for Biomedical and Environmental Applications. Molecules 2019, 24, 1815. [Google Scholar] [CrossRef]
- Sun, J.; Tan, H. Alginate-Based Biomaterials for Regenerative Medicine Applications. Materials 2013, 6, 1285–1309. [Google Scholar] [CrossRef]
- Martău, G.A.; Mihai, M.; Vodnar, D.C. The Use of Chitosan, Alginate, and Pectin in the Biomedical and Food Sector—Biocompatibility, Bioadhesiveness, and Biodegradability. Polymers 2019, 11, 1837. [Google Scholar] [CrossRef]
- Oudadesse, H.; Derrien, A.C.; Martin, S.; Chaair, H.; Cathelineau, G. Surface and Interface Investigation of Aluminosilicate Biomaterial by the “in Vivo” Experiments. Appl. Surf. Sci. 2008, 255, 593–596. [Google Scholar] [CrossRef]
- Gerhardt, L.-C.; Boccaccini, A.R. Bioactive Glass and Glass-Ceramic Scaffolds for Bone Tissue Engineering. Materials 2010, 3, 3867–3910. [Google Scholar] [CrossRef]
- Dubey, N.; Bentini, R.; Islam, I.; Cao, T.; Castro Neto, A.H.; Rosa, V. Graphene: A Versatile Carbon-Based Material for Bone Tissue Engineering. Stem Cells Int. 2015, 2015, 804213. [Google Scholar] [CrossRef] [PubMed]
- Laboy-López, S.; Méndez Fernández, P.O.; Padilla-Zayas, J.G.; Nicolau, E. Bioactive Cellulose Acetate Electrospun Mats as Scaffolds for Bone Tissue Regeneration. Int. J. Biomater. 2022, 2022, 3255039. [Google Scholar] [CrossRef]
- Shaban, N.Z.; Kenawy, M.Y.; Taha, N.A.; Abd El-Latif, M.M.; Ghareeb, D.A. Cellulose Acetate Nanofibers: Incorporating Hydroxyapatite (HA), HA/Berberine or HA/Moghat Composites, as Scaffolds to Enhance In Vitro Osteoporotic Bone Regeneration. Polymers 2021, 13, 4140. [Google Scholar] [CrossRef]
- Rubenstein, D.A.; Venkitachalam, S.M.; Zamfir, D.; Wang, F.; Lu, H.; Frame, M.D.; Yin, W. In Vitro Biocompatibility of Sheath–Core Cellulose-Acetate-Based Electrospun Scaffolds Towards Endothelial Cells and Platelets. J. Biomater. Sci. Polym. Ed. 2010, 21, 1713–1736. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A. Pharmaceutical and Biomedical Applications of Cellulose Nanofibers: A Review. Environ. Chem. Lett. 2021, 19, 2043–2055. [Google Scholar] [CrossRef]
- Torres, F.; Commeaux, S.; Troncoso, O. Biocompatibility of Bacterial Cellulose Based Biomaterials. J. Funct. Biomater. 2012, 3, 864–878. [Google Scholar] [CrossRef] [PubMed]
- Helenius, G.; Bäckdahl, H.; Bodin, A.; Nannmark, U.; Gatenholm, P.; Risberg, B. In Vivo Biocompatibility of Bacterial Cellulose. J. Biomed. Mater. Res. A 2006, 76A, 431–438. [Google Scholar] [CrossRef]
- Rodrigues, S.; Dionísio, M.; López, C.R.; Grenha, A. Biocompatibility of Chitosan Carriers with Application in Drug Delivery. J. Funct. Biomater. 2012, 3, 615–641. [Google Scholar] [CrossRef]
- Venkatesan, J.; Kim, S.-K. Chitosan Composites for Bone Tissue Engineering—An Overview. Mar. Drugs 2010, 8, 2252–2266. [Google Scholar] [CrossRef]
- Bojar, W.; Ciach, T.; Flis, S.; Szawiski, M.; Jagielak, M. Novel Chitosan-Based Bone Substitute. A Summary of in Vitro and in Vivo Evaluation. Dent. Res. Oral Health 2021, 4, 12–24. [Google Scholar] [CrossRef]
- Rezvani Ghomi, E.; Nourbakhsh, N.; Akbari Kenari, M.; Zare, M.; Ramakrishna, S. Collagen-based Biomaterials for Biomedical Applications. J. Biomed. Mater. Res. B Appl. Biomater. 2021, 109, 1986–1999. [Google Scholar] [CrossRef] [PubMed]
- Kilmer, C.E.; Battistoni, C.M.; Cox, A.; Breur, G.J.; Panitch, A.; Liu, J.C. Collagen Type I and II Blend Hydrogel with Autologous Mesenchymal Stem Cells as a Scaffold for Articular Cartilage Defect Repair. ACS Biomater. Sci. Eng. 2020, 6, 3464–3476. [Google Scholar] [CrossRef]
- Su, K.; Wang, C. Recent Advances in the Use of Gelatin in Biomedical Research. Biotechnol. Lett. 2015, 37, 2139–2145. [Google Scholar] [CrossRef] [PubMed]
- Peter, M.; Binulal, N.S.; Nair, S.V.; Selvamurugan, N.; Tamura, H.; Jayakumar, R. Novel Biodegradable Chitosan–Gelatin/Nano-Bioactive Glass Ceramic Composite Scaffolds for Alveolar Bone Tissue Engineering. Chem. Eng. J. 2010, 158, 353–361. [Google Scholar] [CrossRef]
- Köwitsch, A.; Zhou, G.; Groth, T. Medical Application of Glycosaminoglycans: A Review: Medical Application of Glycosaminoglycans. J. Tissue Eng. Regen. Med. 2018, 12, e23–e41. [Google Scholar] [CrossRef]
- Norahan, M.H.; Amroon, M.; Ghahremanzadeh, R.; Rabiee, N.; Baheiraei, N. Reduced Graphene Oxide: Osteogenic Potential for Bone Tissue Engineering. IET Nanobiotechnol. 2019, 13, 720–725. [Google Scholar] [CrossRef]
- Li, D.; Li, J.; Dong, H.; Li, X.; Zhang, J.; Ramaswamy, S.; Xu, F. Pectin in Biomedical and Drug Delivery Applications: A Review. Int. J. Biol. Macromol. 2021, 185, 49–65. [Google Scholar] [CrossRef]
- Tortorella, S.; Inzalaco, G.; Dapporto, F.; Maturi, M.; Sambri, L.; Vetri Buratti, V.; Chiariello, M.; Comes Franchini, M.; Locatelli, E. Biocompatible Pectin-Based Hybrid Hydrogels for Tissue Engineering Applications. New J. Chem. 2021, 45, 22386–22395. [Google Scholar] [CrossRef]
- Makadia, H.K.; Siegel, S.J. Poly Lactic-Co-Glycolic Acid (PLGA) as Biodegradable Controlled Drug Delivery Carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef]
- Zhao, D.; Zhu, T.; Li, J.; Cui, L.; Zhang, Z.; Zhuang, X.; Ding, J. Poly(Lactic-Co-Glycolic Acid)-Based Composite Bone-Substitute Materials. Bioact. Mater. 2021, 6, 346–360. [Google Scholar] [CrossRef]
- Elmowafy, E.M.; Tiboni, M.; Soliman, M.E. Biocompatibility, Biodegradation and Biomedical Applications of Poly(Lactic Acid)/Poly(Lactic-Co-Glycolic Acid) Micro and Nanoparticles. J. Pharm. Investig. 2019, 49, 347–380. [Google Scholar] [CrossRef]
- Gentile, P.; Chiono, V.; Carmagnola, I.; Hatton, P. An Overview of Poly(Lactic-Co-Glycolic) Acid (PLGA)-Based Biomaterials for Bone Tissue Engineering. Int. J. Mol. Sci. 2014, 15, 3640–3659. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.; Xia, X.; Huang, J.; Yuan, C.; Zuo, Y.; Li, Y.; Li, J. Recent Advances in PLGA-Based Biomaterials for Bone Tissue Regeneration. Acta Biomater. 2021, 127, 56–79. [Google Scholar] [CrossRef]
- Da Silva, D.; Kaduri, M.; Poley, M.; Adir, O.; Krinsky, N.; Shainsky-Roitman, J.; Schroeder, A. Biocompatibility, Biodegradation and Excretion of Polylactic Acid (PLA) in Medical Implants and Theranostic Systems. Chem. Eng. J. 2018, 340, 9–14. [Google Scholar] [CrossRef]
- Tyler, B.; Gullotti, D.; Mangraviti, A.; Utsuki, T.; Brem, H. Polylactic Acid (PLA) Controlled Delivery Carriers for Biomedical Applications. Adv. Drug Deliv. Rev. 2016, 107, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Böstman, O.; Pihlajamäki, H. Clinical Biocompatibility of Biodegradable Orthopaedic Implants for Internal Fixation: A Review. Biomaterials 2000, 21, 2615–2621. [Google Scholar] [CrossRef] [PubMed]
- Arora, M. Polymethylmethacrylate Bone Cements and Additives: A Review of the Literature. World J. Orthop. 2013, 4, 67. [Google Scholar] [CrossRef]
- Magnan, B.; Bondi, M.; Maluta, T.; Samaila, E.; Schirru, L.; Dall’Oca, C. Acrylic Bone Cement: Current Concept Review. Musculoskelet. Surg. 2013, 97, 93–100. [Google Scholar] [CrossRef]
- Janmohammadi, M.; Nourbakhsh, M.S. Electrospun Polycaprolactone Scaffolds for Tissue Engineering: A Review. Int. J. Polym. Mater. Polym. Biomater. 2019, 68, 527–539. [Google Scholar] [CrossRef]
- Dwivedi, R.; Kumar, S.; Pandey, R.; Mahajan, A.; Nandana, D.; Katti, D.S.; Mehrotra, D. Polycaprolactone as Biomaterial for Bone Scaffolds: Review of Literature. J. Oral Biol. Craniofacial Res. 2020, 10, 381–388. [Google Scholar] [CrossRef]
- Ghosh, N.N.; Kiskan, B.; Yagci, Y. Polybenzoxazines—New High Performance Thermosetting Resins: Synthesis and Properties. Prog. Polym. Sci. 2007, 32, 1344–1391. [Google Scholar] [CrossRef]
- Periyasamy, T.; Asrafali, S.; Shanmugam, M.; Kim, S.-C. Development of Sustainable and Antimicrobial Film Based on Polybenzoxazine and Cellulose. Int. J. Biol. Macromol. 2021, 170, 664–673. [Google Scholar] [CrossRef] [PubMed]
- Thirukumaran, P.; Shakila Parveen, A.; Atchudan, R.; Kim, S.-C. Sustainability and Antimicrobial Assessments of Bio Based Polybenzoxazine Film. Eur. Polym. J. 2018, 109, 248–256. [Google Scholar] [CrossRef]
- Lorjai, P.; Wongkasemjit, S.; Chaisuwan, T. Preparation of Polybenzoxazine Foam and Its Transformation to Carbon Foam. Mater. Sci. Eng. A 2009, 527, 77–84. [Google Scholar] [CrossRef]
- Rekowska, N.; Teske, M.; Arbeiter, D.; Brietzke, A.; Konasch, J.; Riess, A.; Mau, R.; Eickner, T.; Seitz, H.; Grabow, N. Biocompatibility and Thermodynamic Properties of PEGDA and Two of Its Copolymer. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; IEEE: Berlin, Germany, 2019; pp. 1093–1096. [Google Scholar]
- Warr, C.; Valdoz, J.C.; Bickham, B.P.; Knight, C.J.; Franks, N.A.; Chartrand, N.; Van Ry, P.M.; Christensen, K.A.; Nordin, G.P.; Cook, A.D. Biocompatible PEGDA Resin for 3D Printing. ACS Appl. Bio Mater. 2020, 3, 2239–2244. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; He, R.; Chen, H.; Fu, D.; Peng, Y.; Meng, S.; Chen, C.; Yang, L. Methacrylated Pullulan/Polyethylene (Glycol) Diacrylate Composite Hydrogel for Cartilage Tissue Engineering. J. Biomater. Sci. Polym. Ed. 2021, 32, 1057–1071. [Google Scholar] [CrossRef]
- Musumeci, G.; Loreto, C.; Castorina, S.; Imbesi, R.; Leonardi, R. New Perspectives in the Treatment of Cartilage Damage: Poly(Ethylene Glycol) Diacrylate (PEGDA) Scaffold: A Review. IJAE Ital. J. Anat. Embryol. 2013, 118, 204–210. [Google Scholar] [CrossRef]
- Zhou, X.; Zhang, N.; Mankoci, S.; Sahai, N. Silicates in Orthopedics and Bone Tissue Engineering Materials. J. Biomed. Mater. Res. A 2017, 105, 2090–2102. [Google Scholar] [CrossRef]
- Jurkić, L.M.; Cepanec, I.; Pavelić, S.K.; Pavelić, K. Biological and Therapeutic Effects of Ortho-Silicic Acid and Some Ortho-Silicic Acid-Releasing Compounds: New Perspectives for Therapy. Nutr. Metab. 2013, 10, 2. [Google Scholar] [CrossRef]
- Shadjou, N.; Hasanzadeh, M. Silica-Based Mesoporous Nanobiomaterials as Promoter of Bone Regeneration Process: Bone Regeneration Process Using Silica-Based Mesoporous Nanobiomaterials. J. Biomed. Mater. Res. A 2015, 103, 3703–3716. [Google Scholar] [CrossRef]
- Vareda, J.P.; García-González, C.A.; Valente, A.J.M.; Simón-Vázquez, R.; Stipetic, M.; Durães, L. Insights on Toxicity, Safe Handling and Disposal of Silica Aerogels and Amorphous Nanoparticles. Environ. Sci. Nano 2021, 8, 1177–1195. [Google Scholar] [CrossRef]
- Nguyen, T.P.; Nguyen, Q.V.; Nguyen, V.-H.; Le, T.-H.; Huynh, V.Q.N.; Vo, D.-V.N.; Trinh, Q.T.; Kim, S.Y.; Le, Q.V. Silk Fibroin-Based Biomaterials for Biomedical Applications: A Review. Polymers 2019, 11, 1933. [Google Scholar] [CrossRef]
- Wang, Y.; Rudym, D.D.; Walsh, A.; Abrahamsen, L.; Kim, H.-J.; Kim, H.S.; Kirker-Head, C.; Kaplan, D.L. In Vivo Degradation of Three-Dimensional Silk Fibroin Scaffolds. Biomaterials 2008, 29, 3415–3428. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Han, G.; Yan, S.; Zhang, Q. 3D Printing of Silk Fibroin for Biomedical Applications. Materials 2019, 12, 504. [Google Scholar] [CrossRef] [PubMed]
- Farokhi, M.; Mottaghitalab, F.; Fatahi, Y.; Saeb, M.R.; Zarrintaj, P.; Kundu, S.C.; Khademhosseini, A. Silk Fibroin Scaffolds for Common Cartilage Injuries: Possibilities for Future Clinical Applications. Eur. Polym. J. 2019, 115, 251–267. [Google Scholar] [CrossRef]
- Martins, A.; Chung, S.; Pedro, A.J.; Sousa, R.A.; Marques, A.P.; Reis, R.L.; Neves, N.M. Hierarchical Starch-Based Fibrous Scaffold for Bone Tissue Engineering Applications. J. Tissue Eng. Regen. Med. 2009, 3, 37–42. [Google Scholar] [CrossRef]
- Salgado, A.J.; Coutinho, O.P.; Reis, R.L. Novel Starch-Based Scaffolds for Bone Tissue Engineering: Cytotoxicity, Cell Culture, and Protein Expression. Tissue Eng. 2004, 10, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Pilmane, M.; Salma-Ancane, K.; Loca, D.; Locs, J.; Berzina-Cimdina, L. Strontium and Strontium Ranelate: Historical Review of Some of Their Functions. Mater. Sci. Eng. C 2017, 78, 1222–1230. [Google Scholar] [CrossRef]
- Kaufman, J.-M.; Audran, M.; Bianchi, G.; Braga, V.; Diaz-Curiel, M.; Francis, R.M.; Goemaere, S.; Josse, R.; Palacios, S.; Ringe, J.D.; et al. Efficacy and Safety of Strontium Ranelate in the Treatment of Osteoporosis in Men. J. Clin. Endocrinol. Metab. 2013, 98, 592–601. [Google Scholar] [CrossRef]
- Cianferotti, L.; D’Asta, F.; Brandi, M.L. A Review on Strontium Ranelate Long-Term Antifracture Efficacy in the Treatment of Postmenopausal Osteoporosis. Ther. Adv. Musculoskelet. Dis. 2013, 5, 127–139. [Google Scholar] [CrossRef]
- Lu, H.; Zhou, Y.; Ma, Y.; Xiao, L.; Ji, W.; Zhang, Y.; Wang, X. Current Application of Beta-Tricalcium Phosphate in Bone Repair and Its Mechanism to Regulate Osteogenesis. Front. Mater. 2021, 8, 698915. [Google Scholar] [CrossRef]
- Bohner, M.; Santoni, B.L.G.; Döbelin, N. β-Tricalcium Phosphate for Bone Substitution: Synthesis and Properties. Acta Biomater. 2020, 113, 23–41. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Komaki, H.; Chazono, M.; Kitasato, S.; Kakuta, A.; Akiyama, S.; Marumo, K. Basic Research and Clinical Application of Beta-Tricalcium Phosphate (β-TCP). Morphologie 2017, 101, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Gillman, C.E.; Jayasuriya, A.C. FDA-Approved Bone Grafts and Bone Graft Substitute Devices in Bone Regeneration. Mater. Sci. Eng. C 2021, 130, 112466. [Google Scholar] [CrossRef] [PubMed]
- Petri, D.F.S. Xanthan Gum: A Versatile Biopolymer for Biomedical and Technological Applications. J. Appl. Polym. Sci. 2015, 132, 42035. [Google Scholar] [CrossRef]
- Chen, W.; Chen, S.; Morsi, Y.; El-Hamshary, H.; El-Newhy, M.; Fan, C.; Mo, X. Superabsorbent 3D Scaffold Based on Electrospun Nanofibers for Cartilage Tissue Engineering. ACS Appl. Mater. Interfaces 2016, 8, 24415–24425. [Google Scholar] [CrossRef]
- Li, D.; Chen, K.; Duan, L.; Fu, T.; Li, J.; Mu, Z.; Wang, S.; Zou, Q.; Chen, L.; Feng, Y.; et al. Strontium Ranelate Incorporated Enzyme-Cross-Linked Gelatin Nanoparticle/Silk Fibroin Aerogel for Osteogenesis in OVX-Induced Osteoporosis. ACS Biomater. Sci. Eng. 2019, 5, 1440–1451. [Google Scholar] [CrossRef]
- Lázár, I.; Bereczki, H.F.; Manó, S.; Daróczi, L.; Deák, G.; Fábián, I.; Csernátony, Z. Synthesis and Study of New Functionalized Silica Aerogel Poly(Methyl Methacrylate) Composites for Biomedical Use. Polym. Compos. 2015, 36, 348–358. [Google Scholar] [CrossRef]
- Xu, T.; Miszuk, J.M.; Zhao, Y.; Sun, H.; Fong, H. Electrospun Polycaprolactone 3D Nanofibrous Scaffold with Interconnected and Hierarchically Structured Pores for Bone Tissue Engineering. Adv. Healthc. Mater. 2015, 4, 2238–2246. [Google Scholar] [CrossRef]
- Rong, R.; Li, H.; Dong, X.; Hu, L.; Shi, X.; Du, Y.; Deng, H.; Sa, Y. Silk Fibroin-Chitosan Aerogel Reinforced by Nanofibers for Enhanced Osteogenic Differentiation in MC3T3-E1 Cells. Int. J. Biol. Macromol. 2023, 233, 123501. [Google Scholar] [CrossRef]
- Boda, R.; Lázár, I.; Keczánné-Üveges, A.; Bakó, J.; Tóth, F.; Trencsényi, G.; Kálmán-Szabó, I.; Béresová, M.; Sajtos, Z.; Tóth, E.D.; et al. β-Tricalcium Phosphate-Modified Aerogel Containing PVA/Chitosan Hybrid Nanospun Scaffolds for Bone Regeneration. Int. J. Mol. Sci. 2023, 24, 7562. [Google Scholar] [CrossRef]
- Wasyłeczko, M.; Sikorska, W.; Chwojnowski, A. Review of Synthetic and Hybrid Scaffolds in Cartilage Tissue Engineering. Membranes 2020, 10, 348. [Google Scholar] [CrossRef] [PubMed]
- Balko, S.; Weber, J.F.; Waldman, S.D. Mechanical Stimulation Methods for Cartilage Tissue Engineering. In Orthopedic Biomaterials; Li, B., Webster, T., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 123–147. ISBN 978-3-319-89541-3. [Google Scholar]
- Naseri, N.; Poirier, J.-M.; Girandon, L.; Fröhlich, M.; Oksman, K.; Mathew, A.P. 3-Dimensional Porous Nanocomposite Scaffolds Based on Cellulose Nanofibers for Cartilage Tissue Engineering: Tailoring of Porosity and Mechanical Performance. RSC Adv. 2016, 6, 5999–6007. [Google Scholar] [CrossRef]
- Hench, L.L.; Polak, J.M. Third-Generation Biomedical Materials. Science 2002, 295, 1014–1017. [Google Scholar] [CrossRef]
- Ning, C.; Zhou, L.; Tan, G. Fourth-Generation Biomedical Materials. Mater. Today 2016, 19, 2–3. [Google Scholar] [CrossRef]
- Caliogna, L.; Medetti, M.; Bina, V.; Brancato, A.M.; Castelli, A.; Jannelli, E.; Ivone, A.; Gastaldi, G.; Annunziata, S.; Mosconi, M.; et al. Pulsed Electromagnetic Fields in Bone Healing: Molecular Pathways and Clinical Applications. Int. J. Mol. Sci. 2021, 22, 7403. [Google Scholar] [CrossRef] [PubMed]
- Akdoğan, V.; Özkaner, V.; Alkurt, F.Ö.; Karaaslan, M. Theoretical and Experimental Sensing of Bone Healing by Microwave Approach. Int. J. Imaging Syst. Technol. 2022, 32, 2255–2261. [Google Scholar] [CrossRef]
- Ye, D.; Xu, Y.; Zhang, H.; Fu, T.; Jiang, L.; Bai, Y. Effects of Low-Dose Microwave on Healing of Fractures with Titanium Alloy Internal Fixation: An Experimental Study in a Rabbit Model. PLoS ONE 2013, 8, e75756. [Google Scholar] [CrossRef]
- Leon, S.A.; Asbell, S.O.; Arastu, H.H.; Edelstein, G.; Packel, A.J.; Sheehan, S.; Daskai, I.; Guttmann, G.G.; Santos, I. Effects of Hyperthermia on Bone. II. Heating of Bone in Vivo and Stimulation of Bone Growth. Int. J. Hyperth. 1993, 9, 77–87. [Google Scholar] [CrossRef]
- Khalifeh, J.M.; Zohny, Z.; MacEwan, M.; Stephen, M.; Johnston, W.; Gamble, P.; Zeng, Y.; Yan, Y.; Ray, W.Z. Electrical Stimulation and Bone Healing: A Review of Current Technology and Clinical Applications. IEEE Rev. Biomed. Eng. 2018, 11, 217–232. [Google Scholar] [CrossRef]
- Pinheiro, A.L.B.; Gerbi, M.E.M.; Ponzi, E.A.C.; Ramalho, L.M.P.; Marques, A.M.C.; Carvalho, C.M.; Santos, R.D.C.; Oliveira, P.C.; Nóia, M. Infrared Laser Light Further Improves Bone Healing When Associated with Bone Morphogenetic Proteins and Guided Bone Regeneration: An In Vivo Study in a Rodent Model. Photomed. Laser Surg. 2008, 26, 167–174. [Google Scholar] [CrossRef]
- Garavello-Freitas, I.; Baranauskas, V.; Joazeiro, P.P.; Padovani, C.R.; Dal Pai-Silva, M.; Da Cruz-Höfling, M.A. Low-Power Laser Irradiation Improves Histomorphometrical Parameters and Bone Matrix Organization during Tibia Wound Healing in Rats. J. Photochem. Photobiol. B 2003, 70, 81–89. [Google Scholar] [CrossRef] [PubMed]




| Name | Properties | References |
|---|---|---|
| Alginate | The β-D-mannuronic acid and α-L-guluronic acid-containing alginates can be formulated into gels, particulate solids, nanofibers, or ordered microstructures. They are frequently combined with other biomolecules or chemically modified. Alginates exhibit excellent biocompatibility, biodegradability, and tunable cell-binding affinity, making them versatile materials in wound healing, drug delivery, cartilage, or bone tissue repair. | Sun and Tan; Martau et al. [130,131] |
| Aluminosilicate | Aluminosilicates show zeolite-like structures and link to the bone matrix. The coating on the alumina surface shows good biocompatibility with the osteoblasts that can sustain their bioactivity. | Oudadesse et al. [132] |
| Bioactive glass, Bioglass | Bioactive glasses exhibit excellent tissue binding and good bone regeneration properties. Their chemical composition is described with different SiO2, Na2O, CaO and P2O5 ratios. Depending on the composition, they may also bind to soft tissues. In combination with other bioactive materials, they are frequently used in bone scaffolds. Silicate ions liberated in the degradation process promote the formation of Type I collagen. Bioactive glasses are FDA-approved bone graft materials. | Bellucci et al.; Gerhardt and Boccaccini [114,133] |
| Carbon (amorphous, graphitized) | Carbon forms are insoluble and non-resorbable (thus permanent) bioinert materials made by high-temperature carbonization of resorcinol–formaldehyde or polybenzoxazine resins. Due to their electric conductance, they may find future applications as building materials in communicating fourth generation devices. | Dubey et al. [134] |
| Cellulose acetate (CA) | Cellulose acetate is a hydrophilic and thermoplastic biodegradable cellulose derivative. It can be conveniently formulated into sheets, nanofibers, etc. CA scaffolds combined with other bioactive molecules, biopolymers, drugs, etc., support endothelial cell migration and adhesion, and do not promote platelet activation. Chemically modified CA mats bolster osteoconduction and osteoinduction and may help bone regeneration. | Laboy-López and Frenández; Shaban et al.; Rubenstein et al. [135,136,137] |
| Cellulose, bacterial cellulose nanofibrils (CNF) | Cellulose nanofibers (from plant or bacterial sources) are nontoxic, biocompatible, and biodegradable materials that can be produced in large quantities at low cost. Pristine and chemically modified or crosslinked CNFs have applications in controlled drug delivery, antibacterial wound dressing, and skin and bone tissue engineering. | Pandey; Torres et al.; Helenius et al. [138,139,140] |
| Chitosan | Chitosan is an amino group-containing polysaccharide derived from the natural chitin sources by deacetylation. It contains randomly ordered D-glucosamine and N-acetyl-D-glucosamine units. Chitosan is a highly biocompatible and biodegradable material that can be digested by either lysozyme or chitinase enzymes in the body. It is frequently used for drug delivery, antibacterial wound dressing, tissue engineering, and bone substitution purposes, in combination with other biopolymers like PEGDA, PLA, gelatin, and alginate. The higher degree of deacetylation increases the strength of cell membrane interactions and cellular uptake. | Rodrigues et al.; Venkatesan and Kim; Bojar et al. [141,142,143] |
| Collagen, Type-I and II | Collagen is a natural fibrous protein with excellent biocompatibility, biodegradability and bioactivity. Type I collagen is the major component of the extracellular matrix and the bones, while Type II collagen can be found in the cartilage tissues. Due to their excellent cellular interactions, both types were applied in bone scaffolds and cartilage repair preparations. | Ferreira et al.; Rezvani Ghomi et al.; Kilmer et al. [2,144,145] |
| Gelatin | Gelatin is a partly hydrolyzed form of collagen containing interconnecting protein chains. It is isolated from animal skin, bone, or connecting tissues. The amino acid composition and sequence is changing with the origin of the tissue. Gelatin is mostly used with other bioactive polymers, i.e., alginate, chitosan, PLLA, and PCL. In scaffolds, it improves cell adhesion, proliferation, and infiltration. | Su and Wang; Peter et al. [146,147] |
| Glycosaminoglycan (GAG) | Glycosaminoglycans are long-chained polysaccharides built from repeating disaccharide units. They are present on cell surfaces and in the extracellular matrix. Due to their role in regulating the growth factor signaling, interaction with cytokines, and cell surface receptors, GAGs affect, for instance, the inflammation and cell growth processes. They are used in hydrogels, antibacterial surface layers, and porous scaffolds in tissue engineering. | Köwitsch et al. [148] |
| Graphene | Graphene nanosheets are made from graphite and consist of only a single layer of carbon atoms. Graphene is biocompatible, although it is not biodegradable. Graphene promotes stem cell growth and proliferation, as well as osteogenic differentiation. High concentrations of pristine graphene may decrease cell viability, but PEGylation may reduce that effect. Due to its electrical conductance, it might find application in the fourth generation of bioactive materials. | Dubey et al. [134] |
| Graphene oxide (GO) | GO is prepared from graphite or graphene by strong chemical oxidation. Epoxides, hydroxyl, and carboxylic groups are generated on the surface, providing connecting points to anchorage-dependent cells to adhere, spread and function. | Berrio et al.; Dubey et al. [8,134] |
| Graphene oxide, reduced (rGO) | rGO is made from GO by thermal decomposition or chemical reduction. Epoxide rings are removed, but carboxylic and phenolic groups remain on the perimeter. When combined with collagen type-I, the material becomes mechanically more robust and activates the differentiation of human osteoblast stem cells. Scaffolds made with them could be used in bone substitution. | Bahrami et al.; Norahan et al. [53,149] |
| Pectin, Methoxyl pectin | Pectin is a highly hydrophilic, biocompatible, and biodegradable natural polysaccharide rich in carboxylic group-containing galacturonic acid. When more than half of the carboxylate groups are in the methyl ester form, the material is called high methoxyl pectin; otherwise, we talk about low methoxyl pectin. High methoxyl pectin can form hydrogels under mildly acidic conditions. Low methoxyl pectins can be crosslinked with calcium ions to make them less polar drug carriers. Pectins are used alone or in combination with other natural polymers in the 3D printing of scaffolds. | Martau et al.; Li et al.; Tortorella et al. [131,150,151] |
| Poly(lactic-co-glycolic acid) (PLGA) | PLGA is a highly biocompatible and biodegradable material approved by the FDA for drug delivery, gene engineering, and biomedical uses. Pristine polyglycolic acid would hydrolyze readily. Thus, it is blended with PLA or other polymers to improve hydrolytic and degradation properties. PLGA is combined with different bioactive materials (TCP, HA, gelatin, etc.) or bone morphogenetic proteins (BMPs) and is extensively used in artificial bone substitution applications to facilitate cell adhesion and proliferation. PLGA can easily be formulated into various matrices, from solid scaffolds to nanofiber mats. | Makadia and Siegel; Zhao et al.; Elmowafy et al.; Gentile et al.; Jin et al. [152,153,154,155,156] |
| Poly(lactic acid and poly(L-lactic acid) (PLA and PLLA) | PLA is a highly biocompatible and biodegradable thermoplastic polymeric material approved by the FDA for biomedical, drug delivery, and tissue engineering applications. Due to the less polar nature of PLA, it is frequently used in co-polymers with hydrophilic polyglycolic acid to improve hydrolytic behavior. When pristine PLA is used alone in the body, it often induces foreign body reactions. Electrospun PLA-copolymers and their microspheres and nanoparticles provide bioactive materials for drug delivery, wound healing, or bone substitution. PLA is widely used in 3D printing. In the human body, PLA implants degrade significantly slower than polyglycolic acid. | Makadia and Siegel; Zhao et al.; Elmowafy et al.; Gentile et al.; DaSilva et al.; Tyler et al.; Böstman and Pihlajamaki [152,153,154,155,157,158,159] |
| Poly(methyl methacrylate) (PMMA) | PMMA is a bioinert polymeric material, the main component of acrylic bone cement. The mechanical properties can be improved by blending, i.e., with polystyrene. PMMA-based bone cement can be injected into the position and cured at room temperature. It can be mixed with antibiotics. PMMA is not biodegradable; it usually works as a spacer in joining implants. Fixation properties can be improved by chemical modification of the PMMA structure and by loading with TCP or other bioactive and degradable materials. PMMA cements are FDA-approved bone graft materials. | Arora; Magnan et al. [160,161] |
| Poly(ε-caprolactone) (PCL) | PCL is an FDA-approved biocompatible and biodegradable synthetic material for human drug delivery, suture, and adhesion barrier applications. The biodegradation is the slowest among the ester-type bone substitute materials. Thus, PCL is used in long-term implants. Orthopedics frequently combines it with bioactive components like silk fibroin, bioactive glasses, or TCP to improve cell adhesion. It can be formulated by molding, pressing, 3D printing, solution or melt electrospinning. | Janmohammadi and Nourbakhsh; Dwivedi et al. [162,163] |
| Polybenzoxazine (PBO) | The name polybenzoxazine covers a wide range of polymers in which the benzoxazine/polybenzoxazine moiety is the standard building block. PBO resins are prepared by thermal or catalytic ring opening and polymerization of substituted benzoxazine structures derived from synthetic or natural precursors, i.e., cellulose or chitosan. In thin films, PBOs show good antibacterial and antifungal activity. Carbonization at high temperatures results in carbon foams that offer good biocompatibility. | Ghosh et al.; Periyasamy et al.; Thirukumaran et al.; Lorjai et al. [164,165,166,167] |
| Poly(ethylene glycol diacrylate) (PEGDA) | Ethylene glycol diacrylate alone or combined with other acrylates can be easily polymerized or photopolymerized to PEGDA and copolymers. Crosslinking may increase the mechanical strength. PEGDA is a hydrophilic and low-immunogenic compound suitable for scaffolds and hydrogels. It is a good drug depot, and the drug release profile can be finely tuned. It can be used in bio-inks for 3D printing to provide biocompatible flow-through devices. It forms hydrogels that are used in cartilage tissue regeneration. | Rekowska et al.; Warr et al.; Qin et al.; Musumeci et al. [168,169,170,171] |
| Silica | Silica is a biocompatible, biodegradable, and osteoconductive material. Silica enhances the osteogenic differentiation of stem cells and bone regeneration by promoting Type I collagen formation, stabilization, and matrix mineralization. Porous silica can be combined with various polymers, biomaterials, proteins, enzymes, drugs, and hormones. The surface can be covalently functionalized with bioactive agents. Higher concentrations of nano-silica particles may lead to bioaccumulation and cellular damage. | Zhou et al.; Jurkic et al.; Shadjou et al.; Vareda et al. [172,173,174,175] |
| Silk fibroin | Silk fibroin is a natural protein produced by insects. It is a lightweight but mechanically strong material and can be found, i.e., in spider webs and prepared from the cocoon of the domestic silkworm. Scaffolds made of it are biodegradable, can be functionalized, and support the attachment and growth of cells. In the form of fibers, nanofibers, mats, films, and porous structures, silk fibroin has many applications in cell cultures, tissue engineering, and cartilage tissue regeneration. | Nguyen et al.; Wang et al.; Wang et al.; Farokhi et al. [176,177,178,179] |
| Starch | Starch is a natural polysaccharide consisting of d-glucose units. It is produced mainly from potatoes, manioc, or seeds like rice, wheat, and corn. Starch is an edible, biocompatible, and readily biodegradable material. It supports cell growth on the surface. It can be formulated in different shapes and porosities with biodegradable polymeric materials. By 3D prototyping, custom-shaped bioactive scaffolds are created. | Martins et al.; Salgado et al. [180,181] |
| Strontium ranelate (SR) | SR is a medical drug to treat osteoporosis in men and women, regardless of age. It is capable of reducing the risk of fracture. Strontium ranelate promotes the osteoblastic differentiation of stem cells, inhibits osteoclasts, and improves the structure of bones. | Pilmane et al.; Kaufman et al.; Cianferotti et al. [182,183,184] |
| Tricalcium phosphate (βTCP, TCP) | Beta tricalcium phosphate is the “gold standard” of bone grafts approved by the FDA. It is osteoinductive, biodegradable, and one of the most extensively used bone substitute materials in clinical practice. The physical appearance of TCP covers a wide range, from low-strength porous bodies to hard grafts. TCP shows no adverse effects and maintains normal calcium and phosphate ions level in the blood. The apparent in vivo behavior is affected to some extent by the purity and the way TCP was produced. TCP is insoluble under physiological conditions at pH 7.4 and is dissolved and resorbed by cell-mediated processes. The resorption time is in the 6–24 month range. | Lu et al.; Bohner et al.; Tanaka et al.; Gilmann and Jayasuriya [185,186,187,188] |
| Xanthan gum | Xanthan gum is a biodegradable branched polysaccharide produced in large quantities by industrial fermentation with the bacteria Xanthomonas campestris. The backbone is cellobiose, and the branches contain D-mannoses and D-glucuronic acid. The structure of the chain in solutions can be tuned from coiled to helical by increasing the temperature and the ionic strength. High-molecular-weight xanthan gums, frequently in combination with other biopolymers, have found application in the biomedical field, from drug delivery to bone substitute scaffolds. | Petri [189] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lázár, I.; Čelko, L.; Menelaou, M. Aerogel-Based Materials in Bone and Cartilage Tissue Engineering—A Review with Future Implications. Gels 2023, 9, 746. https://0-doi-org.brum.beds.ac.uk/10.3390/gels9090746
Lázár I, Čelko L, Menelaou M. Aerogel-Based Materials in Bone and Cartilage Tissue Engineering—A Review with Future Implications. Gels. 2023; 9(9):746. https://0-doi-org.brum.beds.ac.uk/10.3390/gels9090746
Chicago/Turabian StyleLázár, István, Ladislav Čelko, and Melita Menelaou. 2023. "Aerogel-Based Materials in Bone and Cartilage Tissue Engineering—A Review with Future Implications" Gels 9, no. 9: 746. https://0-doi-org.brum.beds.ac.uk/10.3390/gels9090746