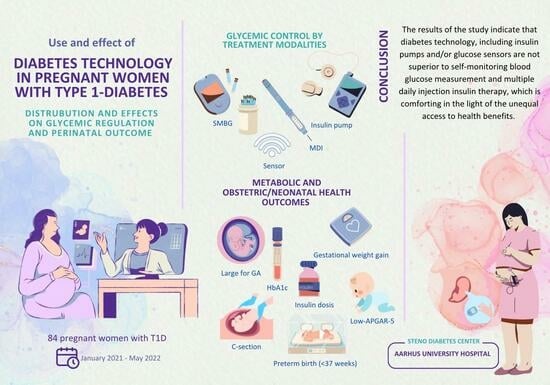
Diabetes Technology in Pregnant Women with Type 1 Diabetes—Distribution and Effects on Glycemic Regulation and Perinatal Outcomes
Abstract
:1. Introduction
2. Materials and Methods
- Exposure
- Outcomes
- Co-variates
- Statistical Analysis
3. Results
3.1. Continuous Outcomes
3.2. Dichotomous Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Evers, I.M.; de Valk, H.W.; Visser, G.H. Risk of complications of pregnancy in women with type 1 diabetes: Nationwide prospective study in the Netherlands. BMJ 2004, 328, 915. [Google Scholar] [CrossRef]
- Persson, M.; Norman, M.; Hanson, U. Obstetric and perinatal outcomes in type 1 diabetic pregnancies: A large, population-based study. Diabetes Care 2009, 32, 2005–2009. [Google Scholar] [CrossRef] [PubMed]
- Feig, D.S.; Hwee, J.; Shah, B.R.; Booth, G.L.; Bierman, A.S.; Lipscombe, L.L. Trends in incidence of diabetes in pregnancy and serious perinatal outcomes: A large, population-based study in Ontario, Canada, 1996–2010. Diabetes Care 2014, 37, 1590–1596. [Google Scholar] [CrossRef] [PubMed]
- Jensen, D.M.; Damm, P.; Moelsted-Pedersen, L.; Ovesen, P.; Westergaard, J.G.; Moeller, M.; Beck-Nielsen, H. Outcomes in type 1 diabetic pregnancies: A nationwide, population-based study. Diabetes Care 2004, 27, 2819–2823. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.; Nilsson, I.A.K.; Gissler, M.; Lavebratt, C. Associations of Maternal Diabetes and Body Mass Index With Offspring Birth Weight and Prematurity. JAMA Pediatr. 2019, 173, 371–378. [Google Scholar] [CrossRef] [PubMed]
- He, L.R.; Yu, L.; Guo, Y. Birth weight and large for gestational age trends in offspring of pregnant women with gestational diabetes mellitus in southern China, 2012–2021. Front. Endocrinol. 2023, 14, 1166533. [Google Scholar] [CrossRef] [PubMed]
- Litvinova, O.; Eitenberger, M.; Bilir, A.; Yeung, A.W.K.; Parvanov, E.D.; MohanaSundaram, A.; Horbańczuk, J.O.; Atanasov, A.G.; Willschke, H. Patent analysis of digital sensors for continuous glucose monitoring. Front. Public Health 2023, 11, 1205903. [Google Scholar] [CrossRef] [PubMed]
- Fazekas-Pongor, V.; Svébis, M.M.; Major, D.; Pártos, K.; Dósa, N.; Mészáros, Á.; Horváth, V.J.; Domján, B.A.; Zsirai, L.; Tabák, A.G. Trend of pregnancy outcomes in type 1 diabetes compared to control women: A register-based analysis in 1996–2018. Front. Endocrinol. 2023, 14, 1232618. [Google Scholar] [CrossRef] [PubMed]
- Murphy, H.R.; Howgate, C.; O’Keefe, J.; Myers, J.; Morgan, M.; Coleman, M.A.; Jolly, M.; Valabhji, J.; Scott, E.M.; Knighton, P.; et al. Characteristics and outcomes of pregnant women with type 1 or type 2 diabetes: A 5-year national population-based cohort study. Lancet Diabetes Endocrinol. 2021, 9, 153–164. [Google Scholar] [CrossRef]
- Mackin, S.T.; Nelson, S.M.; Kerssens, J.J.; Wood, R.; Wild, S.; Colhoun, H.M.; Leese, G.P.; Philip, S.; Lindsay, R.S. Diabetes and pregnancy: National trends over a 15 year period. Diabetologia 2018, 61, 1081–1088. [Google Scholar] [CrossRef]
- Fadl, H.E.; Simmons, D. Trends in diabetes in pregnancy in Sweden 1998–2012. BMJ Open Diabetes Res. Care 2016, 4, e000221. [Google Scholar] [CrossRef] [PubMed]
- Quaresima, P.; Fesslova, V.; Farina, A.; Kagan, K.O.; Candiani, M.; Morelli, M.; Crispi, F.; Cavoretto, P.I. How to do a fetal cardiac scan. Arch. Gynecol. Obstet. 2023, 307, 1269–1276. [Google Scholar] [CrossRef] [PubMed]
- Kuciene, R.; Dulskiene, V.; Medzioniene, J. Associations between high birth weight, being large for gestational age, and high blood pressure among adolescents: A cross-sectional study. Eur. J. Nutr. 2018, 57, 373–381. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, H.; Liu, S.J.; Fu, G.J.; Zhao, Y.; Xie, Y.J.; Zhang, Y.; Wang, Y.X. The associations of high birth weight with blood pressure and hypertension in later life: A systematic review and meta-analysis. Hypertens. Res. 2013, 36, 725–735. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Janszky, I.; Gissler, M.; Cnattingius, S.; Roos, N.; Miao, M.; Yuan, W.; Li, J.; László, K.D. Preterm Birth, Small for Gestational Age, and Large for Gestational Age and the Risk of Atrial Fibrillation Up to Middle Age. JAMA Pediatr. 2023, 177, 599–607. [Google Scholar] [CrossRef]
- Sparano, S.; Ahrens, W.; De Henauw, S.; Marild, S.; Molnar, D.; Moreno, L.A.; Suling, M.; Tornaritis, M.; Veidebaum, T.; Siani, A.; et al. Being macrosomic at birth is an independent predictor of overweight in children: Results from the IDEFICS study. Matern. Child Health J. 2013, 17, 1373–1381. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.H.; Lee, J.E. Large for Gestational Age and Obesity-Related Comorbidities. J. Obes. Metab. Syndr. 2021, 30, 124–131. [Google Scholar] [CrossRef]
- Hirsch, I.B. Introduction: History of Glucose Monitoring. In Role of Continuous Glucose Monitoring in Diabetes Treatment; American Diabetes Association: Arlington, VA, USA, 2018. [Google Scholar]
- Lind, M.; Polonsky, W.; Hirsch, I.B.; Heise, T.; Bolinder, J.; Dahlqvist, S.; Schwarz, E.; Ólafsdóttir, A.F.; Frid, A.; Wedel, H.; et al. Continuous Glucose Monitoring vs. Conventional Therapy for Glycemic Control in Adults with Type 1 Diabetes Treated with Multiple Daily Insulin Injections: The GOLD Randomized Clinical Trial. JAMA 2017, 317, 379–387. [Google Scholar] [CrossRef]
- Beck, R.W.; Riddlesworth, T.; Ruedy, K.; Ahmann, A.; Bergenstal, R.; Haller, S.; Kollman, C.; Kruger, D.; McGill, J.B.; Polonsky, W.; et al. Effect of Continuous Glucose Monitoring on Glycemic Control in Adults with Type 1 Diabetes Using Insulin Injections: The DIAMOND Randomized Clinical Trial. JAMA 2017, 317, 371–378. [Google Scholar] [CrossRef]
- Pickup, J.C.; Keen, H.; Parsons, J.A.; Alberti, K.G. Continuous subcutaneous insulin infusion: An approach to achieving normoglycaemia. Br. Med. J. 1978, 1, 204–207. [Google Scholar] [CrossRef]
- Pala, L.; Dicembrini, I.; Mannucci, E. Continuous subcutaneous insulin infusion vs modern multiple injection regimens in type 1 diabetes: An updated meta-analysis of randomized clinical trials. Acta Diabetol. 2019, 56, 973–980. [Google Scholar] [CrossRef]
- Thayer, S.M.; Williams, K.J.; Lawlor, M.L. The role of technology in the care of diabetes mellitus in pregnancy: An expert review. AJOG Glob. Rep. 2023, 3, 100245. [Google Scholar] [CrossRef]
- Lal, R.A.; Basina, M.; Maahs, D.M.; Hood, K.; Buckingham, B.; Wilson, D.M. One Year Clinical Experience of the First Commercial Hybrid Closed-Loop System. Diabetes Care 2019, 42, 2190–2196. [Google Scholar] [CrossRef]
- Lee, T.T.M.; Collett, C.; Bergford, S.; Hartnell, S.; Scott, E.M.; Lindsay, R.S.; Hunt, K.F.; McCance, D.R.; Barnard-Kelly, K.; Rankin, D.; et al. Automated Insulin Delivery in Women with Pregnancy Complicated by Type 1 Diabetes. N. Engl. J. Med. 2023, 389, 1566–1578. [Google Scholar] [CrossRef]
- Feig, D.S.; Donovan, L.E.; Corcoy, R.; Murphy, K.E.; Amiel, S.A.; Hunt, K.F.; Asztalos, E.; Barrett, J.F.R.; Sanchez, J.J.; de Leiva, A.; et al. Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): A multicentre international randomised controlled trial. Lancet 2017, 390, 2347–2359. [Google Scholar] [CrossRef]
- Thorius, I.H.; Husemoen, L.L.N.; Nordsborg, R.B.; Alibegovic, A.C.; Gall, M.A.; Petersen, J.; Mathiesen, E.R. Congenital malformations among offspring of women with type 1 diabetes who use insulin pumps: A prospective cohort study. Diabetologia 2023, 66, 826–836. [Google Scholar] [CrossRef]
- Żurawska-Kliś, M.; Kosiński, M.; Kuchnicka, A.; Rurka, M.; Hałucha, J.; Wójcik, M.; Cypryk, K. Continuous subcutaneous insulin infusion does not correspond with pregnancy outcomes despite better glycemic control as compared to multiple daily injections in type 1 diabetes—Significance of pregnancy planning and prepregnancy HbA1c. Diabetes Res. Clin. Pract. 2021, 172, 108628. [Google Scholar] [CrossRef] [PubMed]
- Danish Health Authority. Sunde Vaner. 2022. Available online: https://www.sst.dk/-/media/Udgivelser/2022/Foerste-1000-dage/Sunde_vaner_8_-udgave-2022.ashx (accessed on 20 December 2023).
- Marsál, K.; Persson, P.H.; Larsen, T.; Lilja, H.; Selbing, A.; Sultan, B. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr. 1996, 85, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Jiao, X.; Shen, Y.; Chen, Y. Better TIR, HbA1c, and less hypoglycemia in closed-loop insulin system in patients with type 1 diabetes: A meta-analysis. BMJ Open Diabetes Res. Care 2022, 10, e002633. [Google Scholar] [CrossRef]
- Abell, S.K.; Suen, M.; Pease, A.; Boyle, J.A.; Soldatos, G.; Regan, J.; Wallace, E.M.; Teede, H.J. Pregnancy Outcomes and Insulin Requirements in Women with Type 1 Diabetes Treated with Continuous Subcutaneous Insulin Infusion and Multiple Daily Injections: Cohort Study. Diabetes Technol. Ther. 2017, 19, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Ringholm, L.; Damm, P.; Mathiesen, E.R. Improving pregnancy outcomes in women with diabetes mellitus: Modern management. Nat. Rev. Endocrinol. 2019, 15, 406–416. [Google Scholar] [CrossRef]
- Pratley, R.E.; Kanapka, L.G.; Rickels, M.R.; Ahmann, A.; Aleppo, G.; Beck, R.; Bhargava, A.; Bode, B.W.; Carlson, A.; Chaytor, N.S.; et al. Effect of Continuous Glucose Monitoring on Hypoglycemia in Older Adults with Type 1 Diabetes: A Randomized Clinical Trial. JAMA 2020, 323, 2397–2406. [Google Scholar] [CrossRef]
- Mathiesen, J.M.; Secher, A.L.; Ringholm, L.; Nørgaard, K.; Hommel, E.; Andersen, H.U.; Damm, P.; Mathiesen, E.R. Changes in basal rates and bolus calculator settings in insulin pumps during pregnancy in women with type 1 diabetes. J. Matern. Fetal Neonatal Med. 2014, 27, 724–728. [Google Scholar] [CrossRef]
- Kallas-Koeman, M.M.; Kong, J.M.; Klinke, J.A.; Butalia, S.; Lodha, A.K.; Lim, K.I.; Duan, Q.M.; Donovan, L.E. Insulin pump use in pregnancy is associated with lower HbA1c without increasing the rate of severe hypoglycaemia or diabetic ketoacidosis in women with type 1 diabetes. Diabetologia 2014, 57, 681–689. [Google Scholar] [CrossRef]
- Rys, P.M.; Ludwig-Slomczynska, A.H.; Cyganek, K.; Malecki, M.T. Continuous subcutaneous insulin infusion vs multiple daily injections in pregnant women with type 1 diabetes mellitus: A systematic review and meta-analysis of randomised controlled trials and observational studies. Eur. J. Endocrinol. 2018, 178, 545–563. [Google Scholar] [CrossRef] [PubMed]
- Lurie, S.; Mamet, Y. Red blood cell survival and kinetics during pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2000, 93, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, L.R.; Ekbom, P.; Damm, P.; Glümer, C.; Frandsen, M.M.; Jensen, D.M.; Mathiesen, E.R. HbA1c levels are significantly lower in early and late pregnancy. Diabetes Care 2004, 27, 1200–1201. [Google Scholar] [CrossRef]
- Kerssen, A.; Evers, I.M.; de Valk, H.W.; Visser, G.H. Poor glucose control in women with type 1 diabetes mellitus and ‘safe’ hemoglobin A1c values in the first trimester of pregnancy. J. Matern. Fetal Neonatal Med. 2003, 13, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Law, G.R.; Gilthorpe, M.S.; Secher, A.L.; Temple, R.; Bilous, R.; Mathiesen, E.R.; Murphy, H.R.; Scott, E.M. Translating HbA(1c) measurements into estimated average glucose values in pregnant women with diabetes. Diabetologia 2017, 60, 618–624. [Google Scholar] [CrossRef]
- Dansk Endokrinologisk Selskab. Kontinuerlig Glukosemåling (CGM). 2020. Available online: https://endocrinology.dk/nbv/diabetes-melitus/kontinuerlig-glukosemaaling-cgm-og-flash-glukosemaaling-fgm-til-boern-unge-og-voksne/ (accessed on 23 November 2022).
- Lomax, K.E.; Taplin, C.E.; Abraham, M.B.; Smith, G.J.; Haynes, A.; Zomer, E.; Ellis, K.L.; Clapin, H.; Zoungas, S.; Jenkins, A.J.; et al. Socioeconomic status and diabetes technology use in youth with type 1 diabetes: A comparison of two funding models. Front. Endocrinol. 2023, 14, 1178958. [Google Scholar] [CrossRef]
- Agarwal, S.; Simmonds, I.; Myers, A.K. The Use of Diabetes Technology to Address Inequity in Health Outcomes: Limitations and Opportunities. Curr. Diabetes Rep. 2022, 22, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, D.; Bellini, N.J.; Biba, U.; Cai, A.; Close, K.L. Health Care Disparities in Use of Continuous Glucose Monitoring. Diabetes Technol. Ther. 2021, 23, S81–S87. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | SMBG + MDI, n = 23 1 | Sensor + MDI, n = 47 1 | Sensor + Pump, n = 15 1 | p-Value 2 |
|---|---|---|---|---|
| Maternal age (years) | 31.0 (4.7) | 31.0 (5.1) | 29.5 (2.9) | 0.5 |
| Pre-pregnancy BMI (kg/m2) | 27.0 (5.2) | 26.5 (5.9) | 27.2 (2.9) | 0.3 |
| Smoking (yes) | 2 (8.7%) | 2 (4.3%) | 1 (7.1%) | 0.7 |
| Educational level (low) | 12 (55%) | 12 (26%) | 5 (36%) | 0.072 |
| Nullipara | 11 (48%) | 21 (45%) | 4 (29%) | 0.5 |
| Diabetes duration (years) | 11 (8) | 15 (7) | 17 (7) | 0.015 |
| Gestational age (days) | 263 (12) | 263 (8) | 260 (10) | 0.4 |
| Pre-gestational HbA1c (mmol/mol) | 59 (14) | 57 (15) | 55 (12) | 0.7 |
| Pre-gestational insulin (IE/kg/day) | 0.74 (0.28) | 0.64 (0.23) | 0.63 (0.22) | 0.3 |
| SMBG + MDI (SE) | Sensor + MDI (SE) | Sensor + Pump (SE) | Sensor + MDI vs. SMBG + MDI (CI) | Sensor + Pump vs. SMBG + MDI (CI) | Sensor + MDI vs. Sensor + Pump (CI) | |
|---|---|---|---|---|---|---|
| Birthweight Z-score | 1.38 (0.29) | 2.25 (0.20) | 2.69 (0.37) | 0.86 (0.18–1.55) | 1.30 (0.39–2.22) | −0.44 (−1.26–0.39) |
| Gestational weight gain (kg) | 11.37 (1.22) | 15.90 (0.84) | 15.36 (1.65) | 4.53 (1.63–7.44) | 3.99 (−0.03–8.01) | 0.54 (−3.09–4.17) |
| HbA1c, 3rd trimester (mmol/mol) | 49.96 (2.11) | 47.87 (1.48) | 48.29 (2.71) | −2.08 (−7.14–2.97) | −1.67 (−8.40–5.06) | −0.41 (−6.46–5.63) |
| Insulin, 3rd trimester (IU/kg/day) | 1.06 (0.09) | 0.97 (0.06) | 1.03 (0.12) | −0.10 (−0.31–0.12) | −0.03 (−0.32–0.26) | −0.06 (−0.32–0.19) |
| Gestational age (days) | 263.43 (2.00) | 263.09 (1.40) | 259.71 (2.56) | − 0.35 (−5.13–4.43) | −3.72 (−10.09–2.65) | 3.37 (−2.35–9.09) |
| Sensor + MDI vs. SMBG + MDI OR (CI) | Sensor + Pump vs. SMBG + MDI OR (CI) | Sensor + Pump vs. Sensor + MDI OR (CI) | |
|---|---|---|---|
| C-section | 1.04 (0.38–2.83) | 0.92 (0.24–3.46) | 0.88 (0.27–2.90) |
| LGA (≥2 SD) | 3.68 (1.27–10.69) | 3.05 (0.77–12.14) | 0.83 (0.25–2.78) |
| Pre-term birth (<37 weeks) | 1.23 (0.38–4.05) | 2.70 (0.63–11.51) | 2.19 (0.63–7.60) |
| Low APGAR-5 (<7) | 1.50 (0.15–15.26) | 3.67 (0.30–44.72) | 2.44 (0.37–16.34) |
| GWG above recommendation | 2.12 (0.76–5.92) | 3.00 (0.72–12.55) | 1.42 (0.38–5.22) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghaur, S.Y.; Grinderslev, P.B.; Leth-Møller, M.; Ovesen, P.G.; Fuglsang, J.; Fisker, S.; McIntyre, H.D.; Kampmann, U. Diabetes Technology in Pregnant Women with Type 1 Diabetes—Distribution and Effects on Glycemic Regulation and Perinatal Outcomes. Reprod. Med. 2024, 5, 12-22. https://0-doi-org.brum.beds.ac.uk/10.3390/reprodmed5010002
Ghaur SY, Grinderslev PB, Leth-Møller M, Ovesen PG, Fuglsang J, Fisker S, McIntyre HD, Kampmann U. Diabetes Technology in Pregnant Women with Type 1 Diabetes—Distribution and Effects on Glycemic Regulation and Perinatal Outcomes. Reproductive Medicine. 2024; 5(1):12-22. https://0-doi-org.brum.beds.ac.uk/10.3390/reprodmed5010002
Chicago/Turabian StyleGhaur, Sara Yalda, Pernille Bundgaard Grinderslev, Magnus Leth-Møller, Per Glud Ovesen, Jens Fuglsang, Sanne Fisker, H. David McIntyre, and Ulla Kampmann. 2024. "Diabetes Technology in Pregnant Women with Type 1 Diabetes—Distribution and Effects on Glycemic Regulation and Perinatal Outcomes" Reproductive Medicine 5, no. 1: 12-22. https://0-doi-org.brum.beds.ac.uk/10.3390/reprodmed5010002