Advances in Cancer Disparities
A topical collection in Cancers (ISSN 2072-6694). This collection belongs to the section "Cancer Survivorship and Quality of Life".
Viewed by 24189Editors
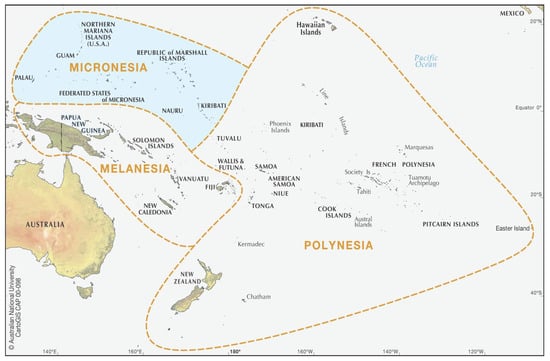
Interests: native Hawaiian and other pacific islander health; data disaggregation; breast cancer
Interests: community-based participatory research; clinical trials to address cancer health disparities; value-based cancer care delivery
Interests: structural and social determinants of health; Asian American health; data disaggregation; neighborhood environment
Topical Collection Information
Dear Colleagues,
Significant progress has been made in the identification of cancer health disparities in the United States, and areas for improvement, particularly among Black and Hispanic populations. In this Special Issue of Cancers, we aim to highlight advances in research that sheds light on overlooked cancer health disparities or demonstrates solutions to overcoming these challenges to equitable cancer care. We are pleased to invite you to submit your unpublished research on your field of cancer disparities. In this Special Issue, original research articles and reviews are welcome. The issue will highlight novel research focused on underappreciated cancer disparities among populations from racial, ethnic, sexual orientation, gender, or age (pediatric, AYA, elderly) minority populations, as well as those disproportionately impacted by structural and social determinants of health. The scope of the issue will cover any unpublished and novel cancer disparities research including but not limited to clinical trials, interventional studies, observational studies, methodological research, reviews, and perspectives. Topics may also include patient centric disparities including financial toxicity and patient reported outcomes. Research emphasizing the importance of data disaggregation and assessment of intersectionality is encouraged.
We look forward to receiving your contributions,
Dr. Kekoa Taparra
Dr. Manali I. Patel
Prof. Dr. Scarlett Lin Gomez
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- race
- ethnicity
- gender
- structural and social determinants
- healthcare disparities
- cancer disparities