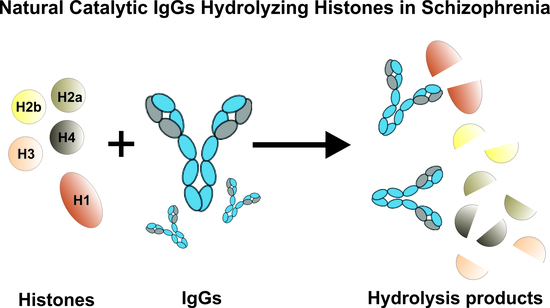
Natural Catalytic IgGs Hydrolyzing Histones in Schizophrenia: Are They the Link between Humoral Immunity and Inflammation?
Abstract
:1. Introduction
2. Results
2.1. Characterization of Schizophrenia Patients and Healthy Donors Participating in the Study
2.2. IgGs Purification and Evidence of Their Histone Hydrolyzing Activity
2.3. Comparison of IgGs Histone-Hydrolyzing Activity of Healthy Individuals and Patients
2.4. The Catalytic Properties of Histone-Hydrolyzing IgGs in Schizophrenia
3. Discussion
4. Materials and Methods
4.1. Materials and Reagents
4.2. Patients, Healthy Donors, and Biological Material
4.3. IgGs Purification from Human Serum
4.4. IgGs Histone-Hydrolyzing Proteolytic Activity Assay
4.5. Verification Assay That Antibodies Possess Proteolytic Activity
4.6. Analysis of Substrate Specificity of Antibodies
4.7. The Effect of pH on the Proteolytic Activity of IgG
4.8. Determination of Metal Dependence
4.9. Kinetic Parameter Analysis
4.10. Statistical Analysis of the Data
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CDR | Complementarity-determining Regions |
| cfDNA | Cell-free DNA |
| DAMPs | Damage-associated Molecular Patterns |
| DTT | Dithiothreitol |
| EDTA | Ethylenediaminetetraacetic Acid |
| MS | Multiple Sclerosis |
| PANSS | Positive And Negative Syndrome Scale |
| SLE | Systemic Lupus Erythematosus |
References
- Hou, W.; Zhang, Q.; Yan, Z.; Chen, R.; Zeh Iii, H.J.; Kang, R.; Lotze, M.T.; Tang, D. Strange attractors: DAMPs and autophagy link tumor cell death and immunity. Cell Death Dis. 2013, 4, e966. [Google Scholar] [CrossRef]
- Tang, D.; Kang, R.; Coyne, C.B.; Zeh, H.J.; Lotze, M.T. PAMPs and DAMPs: Signal 0s that spurautophagy and immunity. Immunol. Rev. 2012, 249, 158–175. [Google Scholar] [CrossRef]
- Allam, R.; Kumar, S.V.; Darisipudi, M.N.; Anders, H.J. Extracellular histones in tissue injury and inflammation. J. Mol. Med. 2014, 92, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhang, X.; Pelayo, R.; Monestier, M.; Ammollo, C.T.; Semeraro, F.; Taylor, F.B.; Esmon, N.L.; Lupu, F.; Esmon, C.T. Extracellular histones are major mediators of death in sepsis. Nat. Med. 2009, 15, 1318–1321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, R.; Kang, R.; Fan, X.-G.; Tang, D. Release and activity of histone in diseases. Cell Death Dis. 2014, 5, e1370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denning, N.L.; Aziz, M.; Gurien, S.D.; Wang, P. DAMPs and NETs in sepsis. Front. Immunol. 2019, 10, 2536. [Google Scholar] [CrossRef]
- Demers, M.; Krause, D.S.; Schatzberg, D.; Martinod, K.; Voorhees, J.R.; Fuchs, T.A.; Scadden, D.T.; Wagner, D.D. Cancers predispose neutrophils to release extracellular DNA traps that contribute to cancer-associated thrombosis. Proc. Natl. Acad. Sci. USA 2012, 109, 13076–13081. [Google Scholar] [CrossRef] [Green Version]
- Parseghian, M.H.; Luhrs, K.A. Beyond the walls of the nucleus: The role of histones in cellular signaling and innate immunity. Biochem. Cell Biol. 2006, 84, 589–604. [Google Scholar] [CrossRef]
- Remijsen, Q.; Kuijper, T.W.; Wirawan, E.; Lippens, S.; Vandenabeele, P.; Vanden Berghe, T. Dying for a cause: NETosis, mechanisms behind an antimicrobial cell death modality. Cell Death Differ. 2011, 18, 581–588. [Google Scholar] [CrossRef] [Green Version]
- Jiang, J.; Chen, X.; Sun, L.; Qing, Y.; Yang, X.; Hu, X.; Yang, C.; Xu, T.; Wang, J.; Wang, P.; et al. Analysis of the concentrations and size distributions of cell-free DNA in schizophrenia using fluorescence correlation spectroscopy. Transl. Psychiatry 2018, 8, 104. [Google Scholar] [CrossRef]
- Ershova, E.S.; Jestkova, E.M.; Martynov, A.V.; Shmarina, G.V.; Umriukhin, P.E.; Bravve, L.V.; Zakharova, N.V.; Kostyuk, G.P.; Saveliev, D.V.; Orlova, M.D.; et al. Accumulation of circulating cell-free CpG-enriched ribosomal DNA fragments on the background of high endonuclease activity of blood plasma in schizophrenic patients. Int. J. Genom. 2019, 2019, 8390585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horváth, S.; Mirnics, R. Immune system disturbances in schizophrenia. Biol. Psychiatry 2014, 75, 316–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khandaker, G.M.; Cousins, L.; Deakin, J.; Lennox, B.R.; Yolken, R.; Jones, P.B. Inflammation and immunity in schizophrenia: Implications for pathophysiology and treatment. Lancet Psychiatry 2015, 2, 258–270. [Google Scholar] [CrossRef] [Green Version]
- Miller, B.J.; Goldsmith, D.R. Inflammatory Biomarkers in Schizophrenia: Implications for Heterogeneity and Neurobiology. Biomark. Neuropsychiatry 2019, 1, 100006. [Google Scholar] [CrossRef]
- Mongan, D.; Ramesar, M.; Föcking, M.; Cannon, M.; Cotter, D. Role of inflammation in the pathogenesis of schizophrenia: A review of the evidence, proposed mechanisms and implications for treatment. Early Interv. Psychiatry 2020, 14, 385–397. [Google Scholar] [CrossRef]
- Buneva, V.N.; Ermakov, E.A.; Nevinsky, G.A. Immune System Dysregulation and Autoimmunity in Schizophrenia: IgGs from Sera of Patients with Several Catalytic Activities. In Psychotic Disorders–An Update; InTechOpen: London, UK, 2018; pp. 41–101. [Google Scholar] [CrossRef] [Green Version]
- Ermakov, E.A.; Smirnova, L.P.; Parkhomenko, T.A.; Dmitrenok, P.S.; Krotenko, N.M.; Fattakhov, N.S.; Bokhan, N.A.; Semke, A.V.; Ivanova, S.A.; Buneva, V.N.; et al. DNA-hydrolysing activity of IgG antibodies from the sera of patients with schizophrenia. Open Biol. 2015, 5, 150064. [Google Scholar] [CrossRef] [Green Version]
- Sirota, P.; Firer, M.A.; Schild, K.; Tanay, A.; Elizur, A.; Meytes, D.; Slor, H. Autoantibodies to DNA in multicase families with schizophrenia. Biol. Psychiatry 1993, 33, 450–455. [Google Scholar] [CrossRef]
- Laske, C.; Zank, M.; Klein, R.; Stransky, E.; Batra, A.; Buchkremer, G.; Schott, K. Autoantibody reactivity in serum of patients with major depression, schizophrenia and healthy controls. Psychiatry Res. 2008, 158, 83–86. [Google Scholar] [CrossRef]
- Ter Borg, E.J.; Horst, G.; Hummel, E.J.; Limburg, P.C.; Kallenberg, C.G. Measurement of increases in anti-double-stranded DNA antibody levels as a predictor of disease exacerbation in systemic lupus erythematosus. Arthritis Rheum. 1990, 33, 634–643. [Google Scholar] [CrossRef]
- Tan, E.M.; Schur, P.H.; Carr, R.I.; Kunkel, H.G. Deoxybonucleic acid (DNA) and antibodies to DNA in the serum of patients with systemic lupus erythematosus. J. Clin. Investig. 1966, 45, 1732–1740. [Google Scholar] [CrossRef]
- Kozora, E.; Thompson, L.L.; West, S.G.; Kotzin, B.L. Analysis of cognitive and psychological deficits in systemic lupus erythematosus patients without overt central nervous system disease. Arthritis Rheum. 1996, 39, 2035–2045. [Google Scholar] [CrossRef] [PubMed]
- Hanly, J.G.; Liang, M.H. Cognitive Disorders in Systemic Lupus Erythematosus: Epidemiologic and Clinical Issues. Ann. N. Y. Acad. Sci. 1997, 823, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Founel, S.; Muller, S. Antinucleosome antibodies and T-cell response in systemic lupus erythematosus. Ann. Med. Int. 2002, 153, 513–519. [Google Scholar]
- Rekvig, O.P. The anti-DNA antibody: Origin and impact, dogmas and controversies. Nat. Rev. Rheumatol. 2015, 11, 530–540. [Google Scholar] [CrossRef]
- Paul, S.; Volle, D.J.; Beach, C.M.; Johnson, D.R.; Powell, M.J.; Massey, R.J. Catalytic hydrolysis of vasoactive intestinal peptide by human autoantibody. Science 1989, 244, 1158–1162. [Google Scholar] [CrossRef]
- Shuster, A.M.; Gololobov, G.V.; Kvashuk, O.A.; Bogomolova, A.E.; Smirnov, I.V.; Gabibov, A.G. DNA hydrolyzing autoantibodies. Science 1992, 256, 665–667. [Google Scholar] [CrossRef]
- Gabibov, A.G.; Ponomarenko, N.A.; Tretyak, E.B.; Paltsev, M.A.; Suchkov, S.V. Catalytic autoantibodies in clinical autoimmunity and modern medicine. Autoimmun. Rev. 2006, 5, 324–3304. [Google Scholar] [CrossRef]
- Bowen, A.; Wear, M.; Casadevall, A. Antibody-mediated catalysis in infection and immunity. Infect. Immun. 2017, 85, e00202–e00217. [Google Scholar] [CrossRef] [Green Version]
- Nevinsky, G.A.; Buneva, V.N. Natural catalytic antibodies abzymes. In Catalytic Antibodies; Keinan, E., Ed.; WILEY-VCH Verlag GmbH&Co: Weinheim, Israel, 2005; pp. 505–569. [Google Scholar]
- Nevinsky, G.A. Natural catalytic antibodies in norm and in autoimmune diseases. In Autoimmune Diseases: Symptoms, Diagnosis and Treatment; Brenner, K.J., Ed.; Nova Science Publishers, Inc.: Huappauge, NY, USA, 2010; pp. 1–107. [Google Scholar]
- Nevinsky, G.A. Autoimmune processes in multiple sclerosis: Production of harmful catalytic antibodies associated with significant changes in the hematopoietic stem cell differentiation and proliferation. In Multiple Sclerosis; Conzalez-Quevedo, A., Ed.; InTech: Rijeka, Croatia, 2016; pp. 100–147. [Google Scholar]
- Nevinsky, G.A. Natural catalytic antibodies in norm and in HIV-infected patients. In Understanding HIV/AIDS Management and Care—Pandemic Approaches the 21st Century; Kasenga, F.H., Ed.; InTech: Rijeka, Croatia, 2011; pp. 151–192. [Google Scholar]
- Nevinsky, G.A. Catalytic antibodies in norm and systemic lupus erythematosus. In Lupus; Khan, W.A., Ed.; InTech: Rijeka, Croatia, 2017; pp. 41–101. [Google Scholar]
- Dimitrov, J.D.; Lacroix-Desmazes, S. Noncanonical Functions of Antibodies. Trends Immunol. 2020, 41, 379–393. [Google Scholar] [CrossRef]
- Ermakov, E.A.; Nevinsky, G.A.; Buneva, V.N. Immunoglobulins with non-canonical functions in inflammatory and autoimmune disease states. Int. J. Mol. Sci. 2020, 21, 5392. [Google Scholar] [CrossRef]
- Ermakov, E.A.; Ivanova, S.A.; Buneva, V.N.; Nevinsky, G.A. Hydrolysi s by catalytic IgGs of microRNA specific for patients with schizophrenia. IUBMB Life 2018, 70, 153–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ermakov, E.A.; Ivanova, S.A.; Buneva, V.N.; Nevinsky, G.A. Blood-Derived RNA and microRNA-Hydrolyzing IgG Antibodies in Schizophrenia Patients. Biochemistry 2018, 83, 507–526. [Google Scholar] [CrossRef]
- Baranova, S.V.; Mikheeva, E.V.; Buneva, V.N.; Nevinsky, G.A. Antibodies from the sera of multiple sclerosis patients efficiently hydrolyze five histones. Biomolecules 2019, 9, 741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kit, Y.Y.; Starykovych, M.A.; Richter, V.A.; Stoika, R.S. Finding and characterization of IgG- and sIgA- abzymes possessing capacity to hydrolyze histone H1. Biochemistry 2008, 73, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Magorivska, I.B.; Bilyy, R.O.; Havrylyuk, A.M.; Chop’yakb, V.V.; Stoika, R.S.; Kit, Y.Y. Anti-histone H1 IgGs from blood serum of systemic lupus erythematosus patients are capable of hydrolyzing histone H1 and myelin basic protein. J. Mol. Recognit. 2010, 23, 495–502. [Google Scholar] [CrossRef]
- Baranova, S.V.; Buneva, V.N.; Nevinsky, G.A. Antibodies from the sera of HIV-infected patients efficiently hydrolyze all human histones. J. Mol. Recognit. 2016, 29, 346–362. [Google Scholar] [CrossRef]
- Baranova, S.V.; Dmitrienok, P.S.; Ivanisenko, N.V.; Buneva, V.N.; Nevinsky, G.A. Antibodies to H2a and H2b histones from the sera of HIV-infected patients catalyze site-specific degradation of these histones. Mol. Biosyst. 2017, 13, 1090–1101. [Google Scholar] [CrossRef]
- Baranova, S.V.; Dmitrienok, P.S.; Ivanisenko, N.V.; Buneva, V.N.; Nevinsky, G.A. Antibodies to H1 histone from the sera of HIV-infected patients recognize and catalyze site-specific degradation of this histone. J. Mol. Recognit. 2017, 30. [Google Scholar] [CrossRef]
- Baranova, S.V.; Dmitrenok, P.S.; Zubkova, A.D.; Ivanisenko, N.V.; Odintsova, E.S.; Buneva, V.N.; Nevinsky, G.A. Antibodies against H3 and H4 histones from the sera of HIV-infected patients catalyze site-specific degradation of these histones. J. Mol. Recognit. 2018, 31, e2703. [Google Scholar] [CrossRef]
- Whittingham, S.; Bencina, B.; Carnegie, P.R.; McPherson, T.A. Properties of Antibodies Produced in Rabbits to Human Myelin and Myelin Basic Protein. Int. Arch. Allergy Appl. Immunol. 1972, 42, 250–263. [Google Scholar] [CrossRef]
- Baranova, S.V.; Dmitrienok, P.S.; Buneva, V.N.; Nevinsky, G.A. Autoantibodies in HIV-infected patients: Cross site-specific hydrolysis of H1 histone and myelin basic protein. BioFactors 2019, 45, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Parshukova, D.; Smirnova, L.P.; Ermakov, E.A.; Bokhan, N.A.; Semke, A.V.; Ivanova, S.A.; Buneva, V.N.; Nevinsky, G.A. Autoimmunity and immune system dysregulation in schizophrenia: IgGs from sera of patients hydrolyze myelin basic protein. J. Mol. Recognit. 2019, 32, e2759. [Google Scholar] [CrossRef] [PubMed]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Ermakov, E.A.; Smirnova, L.P.; Bokhan, N.A.; Semke, A.V.; Ivanova, S.A.; Buneva, V.N.; Nevinsky, G.A. Catalase activity of IgG antibodies from the sera of healthy donors and patients with schizophrenia. PLoS ONE 2017, 12, e0183867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smirnova, L.P.; Ermakov, E.A.; Boyko, A.S.; Bokhan, N.A.; Semke, A.V.; Ivanova, S.A. Antibodies to native and denatured DNA in the serum of patients with schizophrenia depending on the clinical features of the disease. Zhurnal Nevrol. Psikhiatrii Im. SS Korsakova 2016, 116, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Chengappa, K.R.; Carpenter, A.B.; Yang, Z.W.; Brar, J.S.; Rabin, B.S.; Ganguli, R. Elevated IgG anti-histone antibodies in a subgroup of medicated schizophrenic patients. Schizophr. Res. 1992, 7, 49–54. [Google Scholar] [CrossRef]
- Brix, K.; Dunkhorst, A.; Mayer, K.; Jordans, S. Cysteine cathepsins: Cellular roadmap to different functions. Biochimie 2008, 90, 194–207. [Google Scholar] [CrossRef]
- Lockshin, R.A.; Zakeri, Z. Caspase-independent cell death? Oncogene 2004, 23, 2766–2773. [Google Scholar] [CrossRef] [Green Version]
- Conus, S.; Simon, H.U. Cathepsins and their involvement in immune responses. Swiss Med. Wkly. 2010, 140, w13042. [Google Scholar] [CrossRef]
- Turk, V.; Turk, B.; Turk, D. Lysosomal cysteine proteases: Facts and opportunities. EMBO J. 2001, 20, 4629–4633. [Google Scholar] [CrossRef]
- Fonović, M.; Turk, B. Cysteine cathepsins and extracellular matrix degradation. Biochim. Biophys. Acta Gen. Subj. 2014, 1840, 2560–2570. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, T.; Akasu, R.; Miyazaki, A. Calpain proteolytic systems counteract endothelial cell adaptation to inflammatory environments. Inflamm. Regen. 2020, 40, 5. [Google Scholar] [CrossRef] [PubMed]
- Eisen, H. Affinity enhancement of antibodies: How low-affinity antibodies produced early in immune responses are followed by high-affinity antibodies later and in memory B-cell responses. Cancer Immunol. Res. 2014, 2, 381–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukunaga, A.; Maeta, S.; Reema, B.; Nakakido, M.; Tsumoto, K. Improvement of antibody affinity by introduction of basic amino acid residues into the framework region. Biochem. Biophys. Rep. 2018, 15, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Doronin, V.B.; Parkhomenko, T.A.; Korablev, A.; Toporkova, L.B.; Lopatnikova, J.A.; Alshevskaja, A.A.; Sennikov, S.V.; Buneva, V.N.; Budde, T.; Meuth, S.G.; et al. Changes in different parameters, lymphocyte proliferation, and hematopoietic progenitor colony formation in EAE mice treated with myelin oligodendrocyte glycoprotein. J. Cell. Mol. Med. 2016, 20, 81–94. [Google Scholar] [CrossRef]
- Aulova, K.S.; Toporkova, L.B.; Lopatnikova, J.A.; Alshevskaya, A.A.; Sedykh, S.E.; Buneva, V.N.; Budde, T.; Meuth, S.G.; Popova, N.A.; Orlovskaya, I.A.; et al. Changes in cell differentiation and proliferation lead to production of abzymes in EAE mice treated with DNA–Histone complexes. J. Cell. Mol. Med. 2018, 22, 5816–5832. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Löffler, S.; Klimke, A.; Kronenwett, R.; Kobbe, G.; Haas, R.; Fehsel, K. Clozapine mobilizes CD34+ hematopoietic stem and progenitor cells and increases plasma concentration of interleukin 6 in patients with schizophrenia. J. Clin. Psychopharmacol. 2010, 30, 591–595. [Google Scholar] [CrossRef]
- Miyaoka, T.; Wake, R.; Hashioka, S.; Hayashida, M.; Oh-Nishi, A.; Azis, I.A.; Izuhara, M.; Tsuchie, K.; Araki, T.; Arauchi, R.; et al. Remission of psychosis in treatment-resistant schizophrenia following bone marrow transplantation: A case report. Front. Psychiatry 2017, 8, 174. [Google Scholar] [CrossRef] [Green Version]
- Flynn, S.W.; Lang, D.J.; Mackay, A.L.; Goghari, V.; Vavasour, I.M.; Whittall, K.P.; Smith, G.N.; Arango, V.; Mann, J.J.; Dwork, A.J. Abnormalities of myelination in schizophrenia detected in vivo with MRI, and post-mortem with analysis of oligodendrocyte proteins. Mol. Psychiatry 2003, 8, 811–820. [Google Scholar] [CrossRef]
- Morrissey, J.H. Silver stain for proteins in polyacrylamide gels: A modified procedure with enhanced uniform sensitivity. Anal. Biochem. 1981, 117, 307–310. [Google Scholar] [CrossRef]
- Sambrook, J.; Russell, D.W. Molecular Cloning: A Laboratory Manual; Cold Spring Harbor Laboratory Press: New York, NY, USA, 2001. [Google Scholar]
- Lineweaver, H.; Burk, D. The determination of enzyme dissociation constants. J. Am. Chem. Soc. 1934, 56, 658–666. [Google Scholar] [CrossRef]
- Schmidt, A.; Borgwardt, S. Implementing MR Imaging into Clinical Routine Screening in Patients with Psychosis? Neuroimaging Clin. N. Am. 2020, 30, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Pollak, T.A.; Lennox, B.R.; Müller, S.; Benros, M.E.; Prüss, H.; van Elst, L.T.; Klein, H.; Steiner, J.; Frodl, T.; Bogerts, B.; et al. Autoimmune psychosis: An international consensus on an approach to the diagnosis and management of psychosis of suspected autoimmune origin. Lancet Psychiatry 2020, 7, 93–108. [Google Scholar] [CrossRef]







| Groups of Patients | Histone-Hydrolysing Activity of IgGs, % | |||||
|---|---|---|---|---|---|---|
| H1 | H2a | H2b | H3 | H4 | ||
| Total group of patients (n = 50) | Mean ± SD | 18.6 ± 25.3 | 16.0 ± 22.7 | 15.7 ± 23.5 | 12.8 ± 22.0 | 19.2 ± 26.3 |
| Median [Q1; Q3] | 8.5 [6.1; 15.5] | 8.5 [4.3; 13.2] | 6.7 [3.3; 15.4] | 6.5 [3.6; 8.5] | 7.9 [5.7; 16.8] | |
| Mean ± SD for H1–H4 | 16.4 ± 23.9 | |||||
| Median [Q1; Q3] for H1–H4 | 7.6 [4.3; 14.4] | |||||
| Patients with leading Positive symptoms (n = 22) | Mean ± SD | 13.4 ± 14.2 | 12.0 ± 11.0 | 13.0 ± 9.9 | 8.6 ± 6.6 | 17.2 ± 22.0 |
| Median [Q1; Q3] | 7.8 [6.1; 10.7] | 10.6 [5.2; 13.0] | 9.9 [3.4; 13.5] | 7.1 [6.1; 11.3] | 7.8 [6.4; 12.8] | |
| Mean ± SD for H1–H4 | 12.8 ± 14.3 | |||||
| Median [Q1; Q3] for H1–H4 | 7.8 [5.9; 13.0] | |||||
| Patients with leading Negative symptoms (n = 28) | Mean ± SD | 22.6 ± 31.0 | 19.2 ± 28.6 | 18.0 ± 29.3 | 16.1 ± 28.6 | 20.8 ± 29.6 |
| Median [Q1; Q3] | 9.3 [6.3; 17.6] | 7.3 [4.2; 15.6] | 5.6 [3.3; 17.0] | 5.3 [3.1; 8.4] | 8.8 [5.0; 18.7] | |
| Mean ± SD for H1–H4 | 19.3 ± 29.1 | |||||
| Median [Q1; Q3] for H1–H4 | 7.3 [4.0; 17.1] | |||||
| Significance of differences (p-value) between patients with positive and negative symptoms 1 | 0.374 | 0.664 | 0.498 | 0.341 | 0.92 | |
| Codes of Schizophrenia According to ICD-10 1 | Histone-Hydrolysing Activity of IgGs, % | |||||
|---|---|---|---|---|---|---|
| H1 | H2a | H2b | H3 | H4 | ||
| F20.00 Paranoid schizophrenia with continuous course (n = 11) | Mean ± SD | 24.3 ± 31.9 | 21.6 ± 27.5 | 16.1 ± 27.3 | 21.6 ± 28.3 | 23.3 ± 31.2 |
| Median [Q1; Q3] | 11.0 [6.4; 26.4] | 12.4 [5.1; 27.8] | 5.4 [0; 16.4] | 10.6 [5.2; 27.8] | 7.8 [6.9; 28.2] | |
| Mean ± SD for H1–H4 | 21.4 ± 28.4 | |||||
| Median [Q1; Q3] for H1–H4 | 7.8 [5.1; 27.8] | |||||
| F20.01 Paranoid schizophrenia, episodic with progressive deficit (n = 14) | Mean ± SD | 12.8 ± 13.5 | 9.3 ± 9.1 | 9.9 ± 10.4 | 9.0 ± 4.7 | 16.6 ± 22.7 |
| Median [Q1; Q3] | 8.4 [6.0; 11.9] | 7.0 [2.8; 12.0] | 7.8 [4.0; 11.5] | 7.4 [6.6; 11.3] | 7.6 [4.6; 13.0] | |
| Mean ± SD for H1–H4 | 11.5 ± 13.4 | |||||
| Median [Q1; Q3] for H1–H4 | 7.5 [5.1; 12.4] | |||||
| F20.02 Paranoid schizophrenia, episodic with stable deficit (n = 11) | Mean ± SD | 22.7 ± 31.3 | 17.8 ± 28.0 | 17.5 ± 30.5 | 15.6 ± 28.7 | 21.6 ± 30.7 |
| Median [Q1; Q3] | 7.3 [4.4; 30.9] | 6.3 [3.5; 17.9] | 3.2 [1.4; 17.3] | 3.4 [0; 13.4] | 6.5 [2.7; 28.0] | |
| Mean ± SD for H1–H4 | 19.0 ± 28.9 | |||||
| Median [Q1; Q3] for H1–H4 | 6.3 [1.7; 21.6] | |||||
| F20.09 Paranoid schizophrenia; course uncertain, period of observation too short (n = 8) | Mean ± SD | 23.1 ± 31.6 | 22.2 ± 31.0 | 18.9 ± 32.7 | 17.0 ± 31.2 | 22.5 ± 31.4 |
| Median [Q1; Q3] | 9.9 [8.4; 19.3] | 10.3 [8.1; 16.3] | 7.2 [4.8; 14.8] | 7.1 [5.3; 8.1] | 11.5 [9.1; 17.4] | |
| Mean ± SD for H1–H4 | 20.7 ± 30.0 | |||||
| Median [Q1; Q3] for H1–H4 | 9.2 [6.1; 16.0] | |||||
| F20.6 Simple schizophrenia (n = 6) | Mean ± SD | 7.7 ± 2.7 | 9.8 ± 3.7 | 11.6± 6.7 | 4.9 ± 2.8 | 9.3 ± 4.9 |
| Median [Q1; Q3] | 7.6 [6.3; 8.8] | 10.5 [7.6; 12.9] | 10.9 [5.1; 15.6] | 5.3 [4.5; 6.0] | 7.5 [7.2; 9.2] | |
| Mean ± SD for H1–H4 | 8.5 ± 4.6 | |||||
| Median [Q1; Q3] for H1–H4 | 7.6 [5.3; 11.3] | |||||
| Significance of differences (p-value) between different types of schizophrenia 2 | 0.631 | 0.661 | 0.444 | 0.421 | 0.684 | |
| Parameters | Histone-Hydrolyzing Activity of IgGs 1 | |||||
|---|---|---|---|---|---|---|
| H1 | H3 | H2a | H2b | H4 | ||
| Clinical data | Disease duration | −0.031 | −0.016 | 0.024 | 0.035 | −0.037 |
| Age | −0.116 | 0.073 | −0.077 | −0.094 | −0.111 | |
| PANSS Positive 2 | 0.008 | 0.086 | 0.130 | 0.078 | 0.085 | |
| PANSS Negative 2 | 0.113 | −0.084 | 0.136 | 0.178 | 0.190 | |
| Composite index 2 | −0.077 | 0.208 | 0.002 | −0.009 | −0.060 | |
| PANSS General 2 | 0.248 | 0.136 | 0.264 | 0.288 | 0.314 | |
| PANSS Total 2 | 0.115 | 0.023 | 0.195 | 0.177 | 0.191 | |
| Histone-hydrolyzing activity of IgGs | H1 | 1 | 0.728 | 0.847 | 0.667 | 0.839 |
| H3 | 0.728 | 1 | 0.670 | 0.624 | 0.703 | |
| H2a | 0.847 | 0.670 | 1 | 0.801 | 0.813 | |
| H2b | 0.667 | 0.624 | 0.801 | 1 | 0.697 | |
| H4 | 0.839 | 0.703 | 0.813 | 0.697 | 1 | |
| Parameters | Histone-Hydrolysing Activity of IgGs 1 | ||||
|---|---|---|---|---|---|
| H1 | H3 | H2a | H2b | H4 | |
| DNAse activity of IgG 2 | 0.467 | −0.002 | 0.478 | 0.256 | 0.558 |
| RNAse activity of IgG in the hydrolysis of miR-219a-5p 3 | 0.542 | 0.120 | 0.273 | 0.221 | 0.506 |
| RNAse activity of IgG in the hydrolysis of miR-219a-2-3p 3 | 0.474 | 0.089 | 0.214 | 0.190 | 0.453 |
| RNAse activity of IgG in the hydrolysis of miR-9-5p 3 | 0.377 | 0.058 | 0.088 | 0.110 | 0.367 |
| RNAse activity of IgG in the hydrolysis of miR-137 3 | −0.352 | −0.161 | −0.303 | −0.293 | −0.217 |
| Histones as Substrates | Kinetics Parameters | IgG-1 1 | IgG-2 1 |
|---|---|---|---|
| H1 | Km, μM | 2.8 ± 0.4 | 4.8 ± 0.2 |
| kcat, min−1 | (6.8 ± 0.2) × 10−3 | (6.5 ± 0.1) × 10−3 | |
| H2a | Km, μM | 7.1 ± 1.1 | 8.9 ± 1.0 |
| kcat, min−1 | (10.2 ± 0.7) × 10−3 | (8.4 ± 0.4) × 10−3 | |
| H2b | Km, μM | 6.4 ± 0.6 | 8.0 ± 1.1 |
| kcat, min−1 | (10.7 ± 0.4) × 10−3 | (8.0 ± 0.5) × 10−3 | |
| H3 | Km, μM | 2.3 ± 0.4 | 5.6 ± 0.8 |
| kcat, min−1 | (4.4 ± 0.2) × 10−3 | (3.9 ± 0.2) × 10−3 | |
| H4 | Km, μM | 4.7 ± 0.3 | 24.1 ± 4.2 |
| kcat, min−1 | (6.6 ± 0.1) × 10−3 | (11.1 ± 1.2) × 10−3 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ermakov, E.A.; Parshukova, D.A.; Nevinsky, G.A.; Buneva, V.N. Natural Catalytic IgGs Hydrolyzing Histones in Schizophrenia: Are They the Link between Humoral Immunity and Inflammation? Int. J. Mol. Sci. 2020, 21, 7238. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21197238
Ermakov EA, Parshukova DA, Nevinsky GA, Buneva VN. Natural Catalytic IgGs Hydrolyzing Histones in Schizophrenia: Are They the Link between Humoral Immunity and Inflammation? International Journal of Molecular Sciences. 2020; 21(19):7238. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21197238
Chicago/Turabian StyleErmakov, Evgeny A., Daria A. Parshukova, Georgy A. Nevinsky, and Valentina N. Buneva. 2020. "Natural Catalytic IgGs Hydrolyzing Histones in Schizophrenia: Are They the Link between Humoral Immunity and Inflammation?" International Journal of Molecular Sciences 21, no. 19: 7238. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21197238