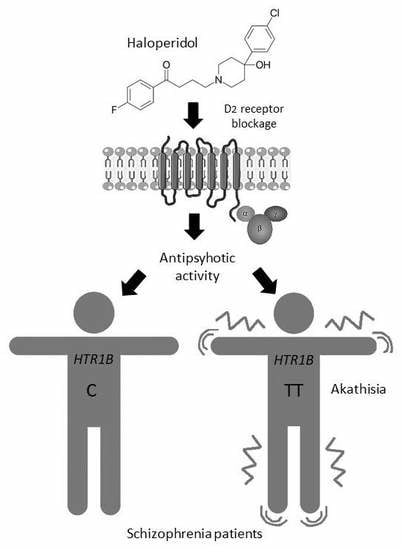
HTR1A, HTR1B, HTR2A, HTR2C and HTR6 Gene Polymorphisms and Extrapyramidal Side Effects in Haloperidol-Treated Patients with Schizophrenia
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Subjects and Clinical Evaluation
4.2. Blood Collection and Genotyping
4.3. Data Analyses
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BARS | Barnes Akathisia Rating Scale |
| BMI | Body mass index |
| DSM-IV | Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition |
| EPS | Extrapyramidal side effects |
| ESRS | Extrapyramidal Symptom Rating Scale |
| FGAs | Typical or first-generation antipsychotics |
| 5-HT | 5-hydroxytryptamine; Serotonin |
| HWE | Hardy–Weinberg equilibrium |
| PANSS | Positive and Negative Syndrome Scale |
| PCR | Polymerase chain reaction |
| SAS | Simpson–Angus Rating Scale for Extrapyramidal Side Effects |
| SGAs | Atypical or second-generation antipsychotics |
| WHO | World Health Organization |
References
- Marder, S.R.; Cannon, T.D. Schizophrenia. N. Engl. J. Med. 2019, 381, 1753–1761. [Google Scholar] [CrossRef] [PubMed]
- Dold, M.; Samara, M.T.; Li, C.; Tardy, M.; Leucht, S. Haloperidol versus first-generation antipsychotics for the treatment of schizophrenia and other psychotic disorders. Cochrane Database Syst. Rev. 2015, 1, CD009831. [Google Scholar] [CrossRef] [PubMed]
- Uchida, H.; Takeuchi, H.; Graff-Guerrero, A.; Suzuki, T.; Watanabe, K.; Mamo, D.C. Dopamine D2 receptor occupancy and clinical effects: A systematic review and pooled analysis. J. Clin. Psychopharm. 2011, 31, 497–502. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Organization Model List of Essential Medicines, 21st List, 2019; License: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Leucht, S.; Cipriani, A.; Spineli, L.; Mavridis, D.; Orey, D.; Richter, F.; Samara, M.; Barbui, C.; Engel, R.R.; Geddes, J.R.; et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. Lancet 2013, 382, 951–962. [Google Scholar] [CrossRef]
- Lally, J.; MacCabe, J.H. Antipsychotic medication in schizophrenia: A review. Br. Med. Bull. 2015, 114, 169–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kapur, S.; Seeman, P. Antipsychotic agents differ in how fast they come off the dopamine D2 receptors. Implications for atypical antipsychotic action. J. Psychiatry Neurosci. 2000, 25, 161–166. [Google Scholar] [PubMed]
- Farde, L.; Nordstrom, A.L.; Wiesel, F.A.; Pauli, S.; Halldin, C.; Sedvall, G. Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch. Gen. Psychiatry 1992, 49, 538–544. [Google Scholar] [CrossRef]
- Lewis, R. Typical and atypical antipsychotics in adolescent schizophrenia: Efficacy, tolerability, and differential sensitivity to extrapyramidal symptoms. Can. J. Psychiatry 1998, 43, 596–604. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Konarski, J.Z. Tolerability profiles of atypical antipsychotics in the treatment of bipolar disorders. J. Clin. Psychiatry 2005, 66, 28–36. [Google Scholar]
- Muscettola, G.; Barbato, G.; Pampallona, S.; Casiello, M.; Bollini, P. Extrapyramidal syndromes in neuroleptic-treated patients: Prevalence, risk factors, and association with tardive dyskinesia. J. Clin. Psychopharmacol. 1999, 19, 203–208. [Google Scholar] [CrossRef]
- Brockmoller, J.; Kirchheiner, J.; Schmider, J.; Walter, S.; Sachse, C.; Muller- Oerlinghausen, B.; Roots, I. The impact of the CYP2D6 polymorphism on haloperidol pharmacokinetics and on the outcome of haloperidol treatment. Clin. Pharm. Ther. 2002, 72, 438–452. [Google Scholar] [CrossRef] [PubMed]
- Crescenti, A.; Mas, S.; Gasso, P.; Parellada, E.; Bernardo, M.; Lafuente, A. CYP2D6*3, *4, *5 and *6 polymorphisms and antipsychotic-induced extrapyramidal side-effects in patients receiving antipsychotic therapy. Clin. Exper. Pharm. Physiol. 2008, 35, 807–811. [Google Scholar] [CrossRef] [PubMed]
- Bakker, P.R.; Van Harten, P.N.; Van Os, J. Antipsychotic-induced tardive dyskinesia and polymorphic variations in COMT, DRD2, CYP1A2 and MnSOD genes: A meta-analysis of pharmacogenetic interactions. Mol. Psychiatry 2008, 13, 544–556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lafuente, A.; Bernardo, M.; Mas, S.; Crescenti, A.; Aparici, M.; Gasso, P.; Deulofeu, R.; Mane, A.; Catalan, R.; Carne, X. Polymorphism of dopamine D2 receptor (TaqIA, TaqIB, and-141C Ins/ Del) and dopamine degradation enzyme (COMT G158A, A-278G) genes and extrapyramidal symptoms in patients with schizophrenia and bipolar disorders. Psychiatry Res. 2008, 161, 131–141. [Google Scholar] [CrossRef]
- Zivković, M.; Mihaljević-Peles, A.; Bozina, N.; Saqud, M.; Nikolac-Perkovic, M.; Vuksan-Cusa, B.; Muck-Seler, D. The association study of polymorphisms in DAT, DRD2, and COMT genes and acute extrapyramidal adverse effects in male schizophrenic patients treated with haloperidol. J. Clin. Psychopharmacol. 2013, 33, 593–599. [Google Scholar] [CrossRef]
- Güzey, C.; Scordo, M.G.; Spina, E.; Landsem, V.M.; Spigset, O. Antipsychotic-induced extrapyramidal symptoms in patients with schizophrenia: Associations with dopamine and serotonin receptor and transporter polymorphisms. Eur. J. Clin. Pharm. 2007, 63, 233–241. [Google Scholar] [CrossRef]
- D’Souza, R.S.; Hooten, W.M. Extrapyramidal Symptoms (EPS). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available online: https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/books/NBK534115/ (accessed on 28 March 2020).
- Givens, C.J. Adverse Drug Reactions Associated with Antipsychotics, Antidepressants, Mood Stabilizers, and Stimulants. Nurs. Clin. North. Am. 2016, 51, 309–321. [Google Scholar] [CrossRef]
- Malhotra, A.K.; Litman, R.E.; Pickar, D. Adverse effects of antipsychotic drugs. Drug Saf. 1993, 9, 429–436. [Google Scholar] [CrossRef]
- Miyamoto, S.; Duncan, G.E.; Marx, C.E.; Lieberman, J.A. Treatment of schizophrenia; a critical review of pharmacology and mechanism of action of antipsychotic drugs. Mol. Psychiatry 2005, 10, 79–104. [Google Scholar] [CrossRef]
- Di Giovanni, G.; Svob Strac, D.; Sole, M.; Unzeta, M.; Tipton, K.F.; Mück-Šeler, D.; Bolea, I.; Della Corte, L.; Nikolac Perkovic, M.; Pivac, N.; et al. Monoaminergic and Histaminergic Strategies and Treatments in Brain Diseases. Front. Neurosci. 2016, 10, 541. [Google Scholar] [CrossRef] [Green Version]
- Alex, K.D.; Pehek, E.A. Pharmacologic mechanisms of serotonergic regulation of dopamine neurotransmission. Pharm 2007, 113, 296–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Deurwaerdere, P.; Di Giovanni, G. Serotonergic modulation of the activity of mesencephalic dopaminergic systems: Therapeutic implications. Prog. Neurobiol. 2017, 151, 175–236. [Google Scholar] [CrossRef] [PubMed]
- Di Giovanni, G.; De Deurwaerdere, P. New therapeutic opportunities for 5-HT2C receptor ligands in neuropsychiatric disorders. Pharm 2016, 157, 125–162. [Google Scholar] [CrossRef] [PubMed]
- Lerer, B.; Segman, R.H.; Tan, E.C.; Basile, V.S.; Cavallaro, R.; Aschauer, H.N.; Strous, R.; Chong, S.A.; Heresco-Levy, U.; Verga, M.; et al. Combined analysis of 635 patients confirms an age-related association of the serotonin 2A receptor gene with tardive dyskinesia and specificity for the non-orofacial subtype. Int. J. Neuropsychopharmacol. 2005, 8, 411–425. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.J.; Zhang, X.B.; Sha, W.W.; Zhang, X.B.; Reynolds, G.P. Association of a polymorphism in the promoter region of the serotonin 5-HT2C receptor gene with tardive dyskinesia in patients with schizophrenia. Mol. Psychiatry 2002, 7, 670–671. [Google Scholar] [CrossRef] [PubMed]
- Gunes, A.; Scordo, M.G.; Jaanson, P.; Dahl, M.L. Serotonin and dopamine receptor gene polymorphisms and the risk of extrapyramidal side effects in perphenazinetreated schizophrenic patients. Psychopharmacol. (Berl) 2007, 190, 479–484. [Google Scholar] [CrossRef]
- Mas, S.; Gassó, P.; Lafuente, A.; Bioque, M.; Lobo, A.; Gonzàlez-Pinto, A.; Olmeda, M.S.; Corripio, I.; Llerena, A.; Cabrera, B.; et al. Pharmacogenetic study of antipsychotic induced acute extrapyramidal symptoms in a first episode psychosis cohort: Role of dopamine, serotonin and glutamate candidate genes. Pharm. J. 2016, 16, 439–445. [Google Scholar] [CrossRef]
- Zhang, J.P.; Malhotra, A.K. Pharmacogenetics and antipsychotics: Therapeutic efficacy and side effects prediction. Expert Opin. Drug Metab. Toxicol. 2011, 7, 9–37. [Google Scholar] [CrossRef] [Green Version]
- Miller, C.H.; Fleischhacker, W.W. Managing antipsychotic-induced acute and chronic akathisia. Drug Saf. 2000, 22, 73–81. [Google Scholar] [CrossRef]
- Dayalu, P.; Chou, K.L. Antipsychotic-induced extrapyramidal symptoms and their management. Expert Opin. Pharm. 2008, 9, 1451–1462. [Google Scholar] [CrossRef]
- Salem, H.; Nagpal, C.; Pigott, T.; Teixeira, A.L. Revisiting Antipsychotic-induced Akathisia: Current Issues and Prospective Challenges. Curr. Neuropharmacol. 2017, 15, 789–798. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caroff, S.N.; Mann, S.C.; Campbell, E.C.; Sullivan, K.A. Movement disorders associated with atypical antipsychotic drugs. J. Clin. Psychiatry 2002, 63, 12–19. [Google Scholar] [PubMed]
- Ohno, Y.; Shimizu, S.; Tokudome, K. Pathophysiological roles of serotonergic system in regulating extrapyramidal motor functions. Biol. Pharm. Bull. 2013, 36, 1396–1400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gunes, A.; Dahl, M.L.; Spina, E.; Scordo, M.G. Further evidence for the association between 5-HT2C receptor gene polymorphisms and extrapyramidal side effects in male schizophrenic patients. Eur. J. Clin. Pharm. 2008, 64, 477–482. [Google Scholar] [CrossRef]
- Al-Janabi, I.; Arranz, M.J.; Blakemore, A.I.; Saiz, P.A.; Susce, M.T.; Glasser, P.E.; Clark, D.; De Leon, J. Association study of serotonergic gene variants with antipsychotic-induced adverse reactions. Psychiatr. Genet. 2009, 19, 305–311. [Google Scholar] [CrossRef] [Green Version]
- Al Hadithy, A.F.; Ivanova, S.A.; Pechlivanoglou, P.; Semke, A.; Fedorenko, O.; Kornetova, E.; Ryadovaya, L.; Brouwers, J.R.; Wilffert, B.; Bruggeman, R.; et al. Tardive dyskinesia and DRD3, HTR2A and HTR2C gene polymorphisms in Russian psychiatric inpatients from Siberia. Prog. Neuropsychopharmacol. Biol. Psychiatry 2009, 33, 475–481. [Google Scholar] [CrossRef]
- Knol, W.; Van Marum, R.J.; Jansen, P.A.; Strengman, E.; Al Hadithy, A.F.; Wilffert, B.; Schobben, A.F.; Ophoff, R.A.; Egberts, T.C. Genetic variation and the risk of haloperidol-related parkinsonism in elderly patients: A candidate gene approach. J. Clin. Psychopharmacol. 2013, 33, 405–410. [Google Scholar] [CrossRef]
- Jensen, K.P.; Covault, J.; Conner, T.S.; Tennen, H.; Kranzler, H.R.; Furneaux, H.M. A common polymorphism in serotonin receptor 1B mRNA moderates regulation by miR-96 and associates with aggressive human behaviors. Mol. Psychiatry 2009, 14, 381–389. [Google Scholar] [CrossRef] [Green Version]
- Sempere, L.F.; Freemantle, S.; Pitha-Rowe, I.; Moss, E.; Dmitrovsky, E.; Ambros, V. Expression profiling of mammalian microRNAs uncovers a subset of brain-expressed microRNAs with possible roles in murine and human neuronal differentiation. Genome Biol. 2004, 5, R13. [Google Scholar] [CrossRef] [Green Version]
- Tang, H.; Dalton, C.F.; Srisawat, U.; Zhang, Z.J.; Reynolds, G.P. Methylation at a transcription factor-binding site on the 5-HT1A receptor gene correlates with negative symptom treatment response in first episode schizophrenia. Int. J. Neuropsychopharmacol. 2014, 17, 645–649. [Google Scholar] [CrossRef] [Green Version]
- Swathy, B.; Banerjee, M. Haloperidol induces pharmacoepigenetic response by modulating miRNA expression, global DNA methylation and expression profiles of methylation maintenance genes and genes involved in neurotransmission in neuronal cells. PLoS ONE 2017, 12, e0184209. [Google Scholar] [CrossRef] [PubMed]
- Melas, P.A.; Rogdaki, M.; Osby, U.; Schalling, M.; Lavebratt, C.; Ekstrom, T.J. Epigenetic aberrations in leukocytes of patients with schizophrenia: Association of global DNA methylation with antipsychotic drug treatment and disease onset. Faseb. J. 2012, 26, 2712–2718. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Guo, Y.; Schroeder, F.A.; Youngs, R.M.; Schmidt, T.W.; Ferris, C.; Konradi, C.; Akbarian, S. Dopamine D2-like antagonists induce chromatin remodeling in striatal neurons through cyclic AMP-protein kinase A and NMDA receptor signaling. J. Neurochem. 2004, 90, 1117–1131. [Google Scholar] [CrossRef] [PubMed]
- Santarelli, D.M.; Liu, B.; Duncan, C.E.; Beveridge, N.J.; Tooney, P.A.; Schofield, P.R.; Cairns, M.J. Gene-microRNA interactions associated with antipsychotic mechanisms and the metabolic side effects of olanzapine. Psychopharmacol (Berl) 2013, 67–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perkins, D.O.; Jeffries, C.D.; Jarskog, L.F.; Thomson, J.M.; Woods, K.; Newman, M.A.; Parker, J.S.; Jin, J.; Hammond, S.M. microRNA expression in the prefrontal cortex of individuals with schizophrenia and schizoaffective disorder. Genome Biol. 2007, 8, R27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fehér, L.Z.; Kálmán, J.; Puskás, L.G.; Gyülvészi, G.; Kitajka, K.; Penke, B.; Palotás, M.; Samarova, E.I.; Molnár, J.; Zvara, A.; et al. Impact of haloperidol and risperidone on gene expression profile in the rat cortex. Neurochem. Int. 2005, 47, 271–280. [Google Scholar] [CrossRef]
- MacGibbon, G.; Lawlor, P.; Bravo, R.; Dragunow, M. Clozapine and haloperidol produce a differential pattern of immediate early gene expression in rat caudate-putamen, nucleus accumbens, lateral septum and islands of Calleja. Brain Res. Mol. Brain Res. 1994, 23, 21–32. [Google Scholar] [CrossRef]
- Audinot, V.; Newman-Tancredi, A.; Cussac, D.; Millan, M.J. Inverse agonist properties of antipsychotic agents at cloned, human (h) serotonin (5-HT)(1B) and h5-HT(1D) receptors. Neuropsychopharmacology 2001, 25, 410–422. [Google Scholar] [CrossRef]
- De Deurwaerdere, P.; Bharatiya, R.; Chagraoui, A.; Di Giovanni, G. Constitutive activity of 5-HT receptors: Factual analysis. Neuropharmacology 2020, 107967. [Google Scholar] [CrossRef]
- Bonhomme, N.; De Deurwaerdere, P.; Le Moal, M.; Spampinato, U. Evidence for 5-HT4 receptor subtype involvement in the enhancement of striatal dopamine release induced by serotonin: A microdialysis study in the halothane-anesthetized rat. Neuropharmacology 1995, 34, 269–279. [Google Scholar] [CrossRef]
- Navailles, S.; De Deurwaerdere, P. Presynaptic control of serotonin on striatal dopamine function. Psychopharmacol. (Berl). 2011, 213, 213–242. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.J.; Segu, L.; Hen, R. 5-Hydroxytryptamine1B receptors modulate the effect of cocaine on c-fos expression: Converging evidence using 5-hydroxytryptamine1B knockout mice and the 5-hydroxytryptamine1B/1D antagonist GR127935. Mol. Pharmacol. 1997, 51, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Jackson, M.J.; Al-Barghouthy, G.; Pearce, R.K.; Smith, L.; Hagan, J.J.; Jenner, P. Effect of 5-HT1B/D receptor agonist and antagonist administration on motor function in haloperidol and MPTP-treated common marmosets. Pharm. Biochem. Behav. 2004, 79, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Jaunarajs, K.L.; Dupre, K.B.; Steiniger, A.; Klioueva, A.; Moore, A.; Kelly, C.; Bishop, C. Serotonin 1B receptor stimulation reduces D1 receptor agonist-induced dyskinesia. Neuroreport 2009, 20, 1265–1269. [Google Scholar] [CrossRef] [PubMed]
- Barnes, N.M.; Sharp, T. A review of central 5-HT receptors and their function. Neuropharmacology 1999, 38, 1083–1152. [Google Scholar] [CrossRef]
- Rainier-Pope, C.R. Treatment with diazepam of children with drug-induced extrapyramidal symptoms. S. Afr. Med. J. 1979, 55, 328–330. [Google Scholar] [PubMed]
- Director, K.L.; Muniz, C.E. Diazepam in the treatment of extrapyramidal symptoms: A case report. J. Clin. Psychiatry 1982, 43, 160–161. [Google Scholar] [PubMed]
- Aichhorn, W.; Gasser, M.; Weiss, E.M.; Adlassnig, C.; Marksteiner, J. Gender Differences in Pharmacokinetics and Side Effects of Second Generation Antipsychotic Drugs. Curr. Neuropharmacol. 2005, 3, 73–85. [Google Scholar] [CrossRef]
- Li, R.; Ma, X.; Wang, G.; Yang, J.; Wang, C. Why sex differences in schizophrenia? J. Transl. Neurosci. (Beijing). 2016, 1, 37–42. [Google Scholar] [CrossRef]
- Xia, X.; Ding, M.; Xuan, J.F.; Xing, J.X.; Pang, H.; Wang, B.J.; Yao, J. Polymorphisms in the human serotonin receptor 1B (HTR1B) gene are associated with schizophrenia: A case control study. BMC Psychiatry 2018, 18, 303. [Google Scholar] [CrossRef] [Green Version]
- Kumar, R.; Sachdev, P. Akathisia and second-generation antipsychotic drugs. Curr. Opin. Psychiatry 2009, 22, 293–299. [Google Scholar] [CrossRef] [PubMed]
- De Deurwaerdere, P. Cariprazine: New dopamine biased agonist for neuropsychiatric disorders. Drugs Today (Barc). 2016, 52, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Hawthorne, J.M.; Caley, C.F. Extrapyramidal reactions associated with serotonergic antidepressants. Ann. Pharm. 2015, 49, 1136–1152. [Google Scholar] [CrossRef] [PubMed]
- Anderson, H.D.; Pace, W.D.; Libby, A.M.; West, D.R.; Valuck, R.J. Rates of 5 common antidepressant side effects among new adult and adolescent cases of depression: A retrospective US claims study. Clin 2012, 34, 113–123. [Google Scholar] [CrossRef]
- Madhusoodanan, S.; Alexeenko, L.; Sanders, R.; Brenner, R. Extrapyramidal symptoms associated with antidepressants: A review of the literature and an analysis of spontaneous reports. Ann. Clin. Psychiatry 2010, 22, 148–156. [Google Scholar] [PubMed]
- Cem Atbasoglu, E.C.; Schultz, S.K.; Andreasen, N.C. The relationship of akathisia with suicidality and depersonalization among patients with schizophrenia. J. Neuropsychiatry Clin. Neurosci. 2001, 13, 336–341. [Google Scholar] [CrossRef]
- Stroup, T.S.; Gray, N. Management of common adverse effects of antipsychotic medications. World Psychiatry 2018, 17, 341–356. [Google Scholar] [CrossRef]
- Poyurovsky, M.; Shardorodsky, M.; Fuchs, C.; Schneidman, M.; Weizman, A. Treatment of neuroleptic induced akathisia with the 5-HT2 antagonist mianserin. Double-blind, placebo-controlled study. Br. J. Psychiatry 1999, 174, 238–242. [Google Scholar] [CrossRef]
- Praharaj, S.K.; Kongasseri, S.; Behere, R.V.; Sharma, P.S. Mirtazapine for antipsychotic induced acute akathisia: A systematic review and meta-analysis of randomized placebo-controlled trials. Adv. Psychopharmacol. 2015, 5, 307–313. [Google Scholar] [CrossRef] [Green Version]
- Miller, C.H.; Hummer, M.; Pycha, R.; Fleischhacker, W.W. The effect of ritanserin on treatment resistant neuroleptic induced akathisia: Case reports. Pro. G Neuropsychopharmacol. Biol. Psychiatry 1992, 16, 247–251. [Google Scholar] [CrossRef]
- Fischel, T.; Hermesh, H.; Aizenberg, D.; Zemishlany, Z.; Munitz, H.; Benjamini, Y.; Weizman, A. Cyproheptadine versus propranolol for the treatment of acute neuroleptic-induced akathisia: A comparative double-blind study. J. Clin. Psychopharmacol. 2001, 21, 612–615. [Google Scholar] [CrossRef] [PubMed]
- Avital, A.; Gross-Isseroff, R.; Stryjer, R.; Hermesh, H.; Weizman, A.; Shiloh, R. Zolmitriptan compared to propranolol in the treatment of acute neuroleptic-induced akathisia: A comparative double-blind study. Eur. Neuropsychopharmacol. 2009, 19, 476–482. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Press: Washington, DC, USA, 1994. [Google Scholar]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Simpson, G.M.; Angus, J.W.S. A rating scale for extrapyramidal side effects. Acta Psychiatr. Scand. 1970, 212, 11–19. [Google Scholar] [CrossRef]
- Barnes, T.R.E. A rating scale for drug-induced akathisia. Br. J. Psychiatry 1989, 154, 672–676. [Google Scholar] [CrossRef]
- Chouinard, G.; Ross-Chouinard, A.; Annable, L.; Jones, B. The extrapyramidal symptom rating scale. Can. J. Neurol. Sci. 1980, 7, 233–244. [Google Scholar]
- Miller, S.A.; Dykes, D.D.; Polesky, H.F. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acid Res. 1988, 16, 1215. [Google Scholar] [CrossRef] [Green Version]


| Male Schizophrenia Patients | n = 229 |
|---|---|
| Age (years, mean ± SD) | 36.49 ± 10.40 |
| BMI (mean ± SD) | 26.54 ± 9.18 |
| Secondary education (n, %) | 163 (71.18%) |
| Not working (unemployed or retired) (n, %) | 181 (79.04%) |
| Not married (n, %) | 206 (89.96%) |
| Without children (n, %) | 192 (83.84%) |
| Alcohol consumption (n, %) | 111 (48.47%) |
| Smoking (n, %) | 154 (67.25%) |
| Illegal drug consumption (n, %) * | 49 (21.40%) |
| PANSS positive scores (mean ± SD) | 35.76 ± 4.74 |
| PANSS negative scores (mean ± SD) | 34.41 ± 4.97 |
| PANSS general psychopathology scores (mean ± SD) | 61.57 ± 7.40 |
| PANSS total scores (mean ± SD) | 131.70 ± 13.12 |
| Suicide attempt (n, %) | 57 (24.89%) |
| Previous antipsychotic medication (n, %) ** | 205 (89.52%) |
| Previous complete or partial disease remission (n, %) *** | 199 (86.90%) |
| Time of acute EPS onset after haloperidol therapy (days, mean ± SD) | 5.04 ± 2.76 |
| Acute EPS occurrence after haloperidol therapy (n, %) | 153 (66.81%) |
| EPS | Number of Patients (%) | Scores (Mean ± SD) |
|---|---|---|
| SAS scale | ||
| Gait | 82 (35.81 %) | 0.635 ± 0.936 |
| Arm dropping | 68 (29.69%) | 0.446 ± 0.758 |
| Shoulder shaking | 47 (20.52%) | 0.338 ± 0.730 |
| Elbow rigidity | 67 (29.26%) | 0.459 ± 0.788 |
| Wrist rigidity | 66 (28.82%) | 0.441 ± 0.763 |
| Head rotation | 64 (27.95%) | 0.464 ± 0.838 |
| Glabella tap | 44 (19.21%) | 0.231 ± 0.524 |
| Tremor | 87 (37.99%) | 0.878 ± 1.193 |
| Salivation | 81 (35.37%) | 0.790 ± 1.151 |
| Akathisia | 53 (23.14%) | 0.402 ± 0.798 |
| Total SAS scores | 145 (63.32%) | 4.965 ± 5.643 |
| Significant acute EPS after haloperidol therapy * | 111 (48.47%) | SAS score >3 |
| BARS scale | ||
| Objective | 52 (22.71%) | 0.367 ± 0.735 |
| Subjective: Awareness of restlessness | 52 (22.71%) | 0.375 ± 0.777 |
| Subjective: Distress related to restlessness | 51 (23.14%) | 0.367 ± 0.770 |
| Global clinical assessment of akathisia | 53 (23.14%) | 0.377 ± 0.755 |
| Total BARS scores | 53 (23.14%) | 1.489 ± 2.989 |
| ESRS scale ** | ||
| I. Parkinsonism, dystonia, dyskinesia and akathisia —questionnaire and behavioral scale | 150 (65.50%) | 5.018 ± 4.774 |
| II. Parkinsonism and akathisia exam—physician’s examination | ||
| Expressive automatic movements (facial mask/speech) | 90 (39.30%) | 0.797 ± 1.097 |
| Bradykinesia | 99 (43.23%) | 0.860 ± 1.143 |
| Rigidity | 91 (39.74%) | 3.081 ± 4.333 |
| Gait and posture | 95 (41.48%) | 0.851 ± 1.185 |
| Tremor | 79 (34.50%) | 3.383 ± 5.198 |
| Akathisia | 54 (23.58%) | 0.495 ± 1.015 |
| Sialorrhea | 76 (33.19%) | 1.054 ± 1.521 |
| Postural stability | 58 (25.33%) | 0.423 ± 0.824 |
| III. Dystonia—physician´s examination—1. Acute torsion dystonia | 40 (17.47%) | 1.680 ± 4.745 |
| VI. Clinical global impression of severity of parkinsonism | 135 (58.95%) | 2.077 ± 1.905 |
| VII. Clinical global impression of severity of dystonia | 44 (19.21%) | 0.874 ± 1.889 |
| VIII. Stage of parkinsonism | 132 (57.64%) | 1.473 ± 1.334 |
| Total ESRS scores | 150 (65.50%) | 21.49 ± 21.24 |
| SNP | Genotype (n, %) | χ2-Test | Allele (n, %) | Fisher’s Test | |||
|---|---|---|---|---|---|---|---|
| HTR2Ars6313 | CC | CT | TT | p = 0.183 | C | T | p = 0.183 |
| Significant acute EPS * | 32 (28.83%) | 60 (54.05%) | 19 (17.12%) | 120 (55.05%) | 98 (44.95%) | ||
| No significant acute EPS | 47 (39.83%) | 51 (43.22%) | 20 (16.95%) | 145 (61.44%) | 91 (38.56%) | ||
| HTR2Crs3813929** | C | T | p = 0.510 | ||||
| Significant acute EPS * | 91 (81.98%) | 20 (18.02%) | |||||
| No significant acute EPS | 92 (77.97%) | 26 (22:03%) | |||||
| HTR1Ars6295 | CC | CG | GG | p = 0.585 | C | G | p = 0.433 |
| Significant acute EPS * | 30 (29.70%) | 51 (50.50%) | 20 (19.80%) | 111 (54.95%) | 91 (45.05%) | ||
| No significant acute EPS | 25 (23.36%) | 59 (55.14%) | 23 (21.50%) | 109 (50.93%) | 105 (49.07%) | ||
| HTR1Brs13212041 | CC | CT | TT | p = 0.055 | C | T | p = 0.330 |
| Significant acute EPS * | 4 (3.88%) | 29 (28.15%) | 70 (67.96%) | 37 (17.96%) | 169 (82.04%) | ||
| No significant acute EPS | 1 (0.93%) | 45 (42.06%) | 61 (57.01%) | 47 (21.96%) | 167 (78.04%) | ||
| HTR6rs1805054 | CC | CT | TT | p = 0.246 | C | T | p = 0.120 |
| Significant acute EPS * | 55 (55.56%) | 39 (39.39%) | 5 (5.05%) | 149 (75.25%) | 49 (24.75%) | ||
| No significant acute EPS | 73 (66.36%) | 34 (30.91%) | 3 (2.73%) | 180 (81.82%) | 40 (18.18%) | ||
| SNP | Genotype/Allele | Statistics | ||
|---|---|---|---|---|
| HTR2Ars6313 | CC | CT | TT | |
| SAS score (mean ± SD) | 4.177 ± 5.257 | 5.802 ± 6.145 | 4.179 ± 4.588 | p = 0.111; Kruskal–Wallis test |
| BARS score (mean ± SD) | 1.304 ± 2.695 | 1.595 ± 3:203 | 1.564 ± 2.981 | p = 0.857; Kruskal–Wallis test |
| ESRS score (mean ± SD) | 19.22 ± 21.13 | 24.62 ± 22.16 | 17.10 ± 17.62 | p = 0.083; Kruskal–Wallis test |
| HTR2Crs3813929 | / | C | T | |
| SAS score (mean ± SD) | 4.951 ± 5.502 | 5.022 ± 6.238 | p = 0.702; Mann–Whitney test | |
| BARS score (mean ± SD) | 1.596 ± 3:094 | 1.065 ± 2.516 | p = 0.294; Mann–Whitney test | |
| ESRS score (mean ± SD) | 21.96 ± 21.26 | 19.63 ± 21.32 | p = 0.364; Mann–Whitney test | |
| HTR1Ars6295 | CC | CG | GG | |
| SAS score (mean ± SD) | 5.491 ± 5.316 | 4.682 ± 5.525 | 4.814 ± 6.013 | p = 0.451; Kruskal–Wallis test |
| BARS score (mean ± SD) | 1.927 ± 3.271 | 1.655 ± 3.303 | 0.953 ± 2.104 | p = 0.393; Kruskal–Wallis test |
| ESRS score (mean ± SD) | 21.26 ± 19.37 | 22.03 ± 21.37 | 21.29 ± 23.00 | p = 0.962; Kruskal–Wallis test |
| HTR1Brs13212041 | CC | CT | TT | |
| SAS score (mean ± SD) | 6.200 ± 4.764 | 3.797 ± 4.728 | 5.580 ± 6.027 | p = 0.077; Kruskal–Wallis test |
| BARS score (mean ± SD) | 0.800 ± 1.789 | 0.7838 ± 2.383 | 1.931 ± 3.228 | p = 0.009; Kruskal–Wallis test * |
| ESRS score (mean ± SD) | 22.40 ± 17.40 | 16.92 ± 17.51 | 24.78 ± 23.22 | p = 0.089; Kruskal–Wallis test |
| HTR6rs1805054 | CC | CT | TT | |
| SAS score (mean ± SD) | 4.359 ± 5.246 | 5.178 ± 5.414 | 9.143 ± 8.275 | p = 0.094; Kruskal–Wallis test |
| BARS score (mean ± SD) | 1.617 ± 2.986 | 1.315 ± 2.990 | 2.000 ± 4.276 | p = 0.513; Kruskal–Wallis test |
| ESRS score (mean ± SD) | 19.68 ± 19.79 | 24.04 ± 23.13 | 26.13 ± 20.93 | p = 0.340; Kruskal–Wallis test |
| HTR1B rs13212041 | Genotypes | Statistics | ||
|---|---|---|---|---|
| BARS Scale Scores | CC | CT | TT | Kruskal–Wallis Test |
| Objective (mean ± SD) | 0.200 ± 0.447 | 0.189 ± 0.589 | 0.481 ± 0.798 | p = 0.010 a |
| Subjective: Awareness of restlessness (mean ± SD) | 0.200 ± 0.447 | 0.203 ± 0.619 | 0.481 ± 0.844 | p = 0.012 b |
| Subjective: Distress related to restlessness (mean ± SD) | 0.200 ± 0.447 | 0.203 ± 0.619 | 0.473 ± 0.844 | p = 0.016 c |
| Global clinical assessment of akathisia (mean ± SD) | 0.200 ± 0.447 | 0.189 ± 0.589 | 0.500 ± 0.828 | p = 0.007d |
| SNP ID | Assay ID | Location | SNP Type | Context Sequence [VIC/FAM] |
|---|---|---|---|---|
| HTR2Ars6313 | C___3042197_1_ | Chr. 13: 46895805 on GRCh38 | Intron, Transition Substitution, Silent Mutation, Intragenic | ATGCATCAGAAGTGTTAGCTTCTCC[A/G]GAGTTAAAGTCATTACTGTAGAGCC |
| HTR2Crs3813929 | C__27488117_10 | Chr. X: 114584047 on GRCh38 | Transition Substitution, Intron, Intragenic | CTGCTCTTGGCTCCTCCCCTCATCC[C/T]GCTTTTGGCCCAAGAGCGTGGTGCA |
| HTR1Ars6295 | C__11904666_10 | Chr. 5: 63962738 on GRCh38 | Intron, Transversion Substitution, Intragenic | ATGGAAGAAGACCGAGTGTGTCTTC[C/G]TTTTTAAAAAGCTACCTCCGTTCTC |
| HTR1Brs13212041 | C__32252506_10 | Chr. 6: 77461407 on GRCh38 | Transition Substitution, UTR 3, Intragenic | AAAAAATAAAGCAGTCTGCAGACTT[C/T]GGCACTAGCACACATAATGGTTTGT |
| HTR6rs1805054 | C___1264819_10 | Chr. 1: 19666020 on GRCh38 | Transition Substitution, Silent Mutation, Intragenic | CGCCGGCCATGCTGAACGCGCTGTA[C/T]GGGCGCTGGGTGCTGGCGCGCGGCC |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grubor, M.; Zivkovic, M.; Sagud, M.; Nikolac Perkovic, M.; Mihaljevic-Peles, A.; Pivac, N.; Muck-Seler, D.; Svob Strac, D. HTR1A, HTR1B, HTR2A, HTR2C and HTR6 Gene Polymorphisms and Extrapyramidal Side Effects in Haloperidol-Treated Patients with Schizophrenia. Int. J. Mol. Sci. 2020, 21, 2345. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21072345
Grubor M, Zivkovic M, Sagud M, Nikolac Perkovic M, Mihaljevic-Peles A, Pivac N, Muck-Seler D, Svob Strac D. HTR1A, HTR1B, HTR2A, HTR2C and HTR6 Gene Polymorphisms and Extrapyramidal Side Effects in Haloperidol-Treated Patients with Schizophrenia. International Journal of Molecular Sciences. 2020; 21(7):2345. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21072345
Chicago/Turabian StyleGrubor, Mirko, Maja Zivkovic, Marina Sagud, Matea Nikolac Perkovic, Alma Mihaljevic-Peles, Nela Pivac, Dorotea Muck-Seler, and Dubravka Svob Strac. 2020. "HTR1A, HTR1B, HTR2A, HTR2C and HTR6 Gene Polymorphisms and Extrapyramidal Side Effects in Haloperidol-Treated Patients with Schizophrenia" International Journal of Molecular Sciences 21, no. 7: 2345. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21072345