Metabolic Syndrome and Reproduction
Abstract
:1. Introduction
2. Methods
3. MetS Definitions
4. MetS and Associated Conditions
5. MetS Prevalence in Infertile and Fertile Men
5.1. MetS Prevalence in Infertile Men
5.2. MetS Prevalence in Fertile Men
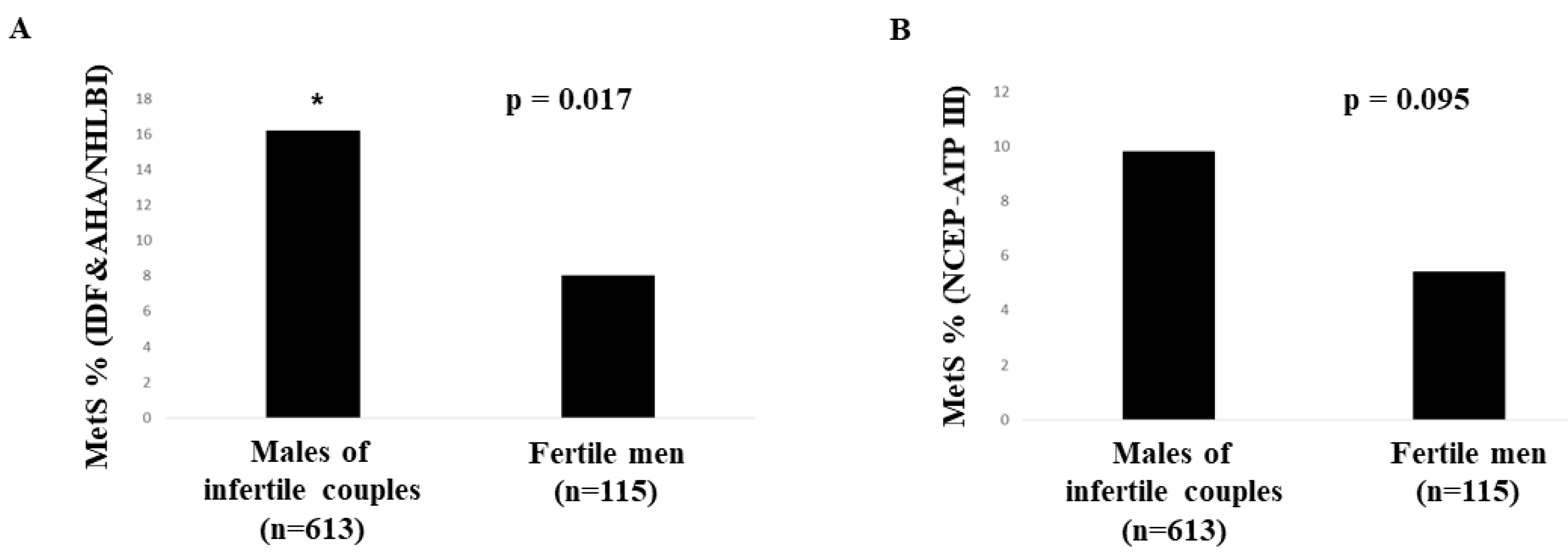
5.3. Studies Comparing MetS Prevalence in Fertile and Infertile Men
6. MetS and Semen Parameters
6.1. Cross-Sectional Studies
6.1.1. Analytical Description of the Cross-Sectional Studies
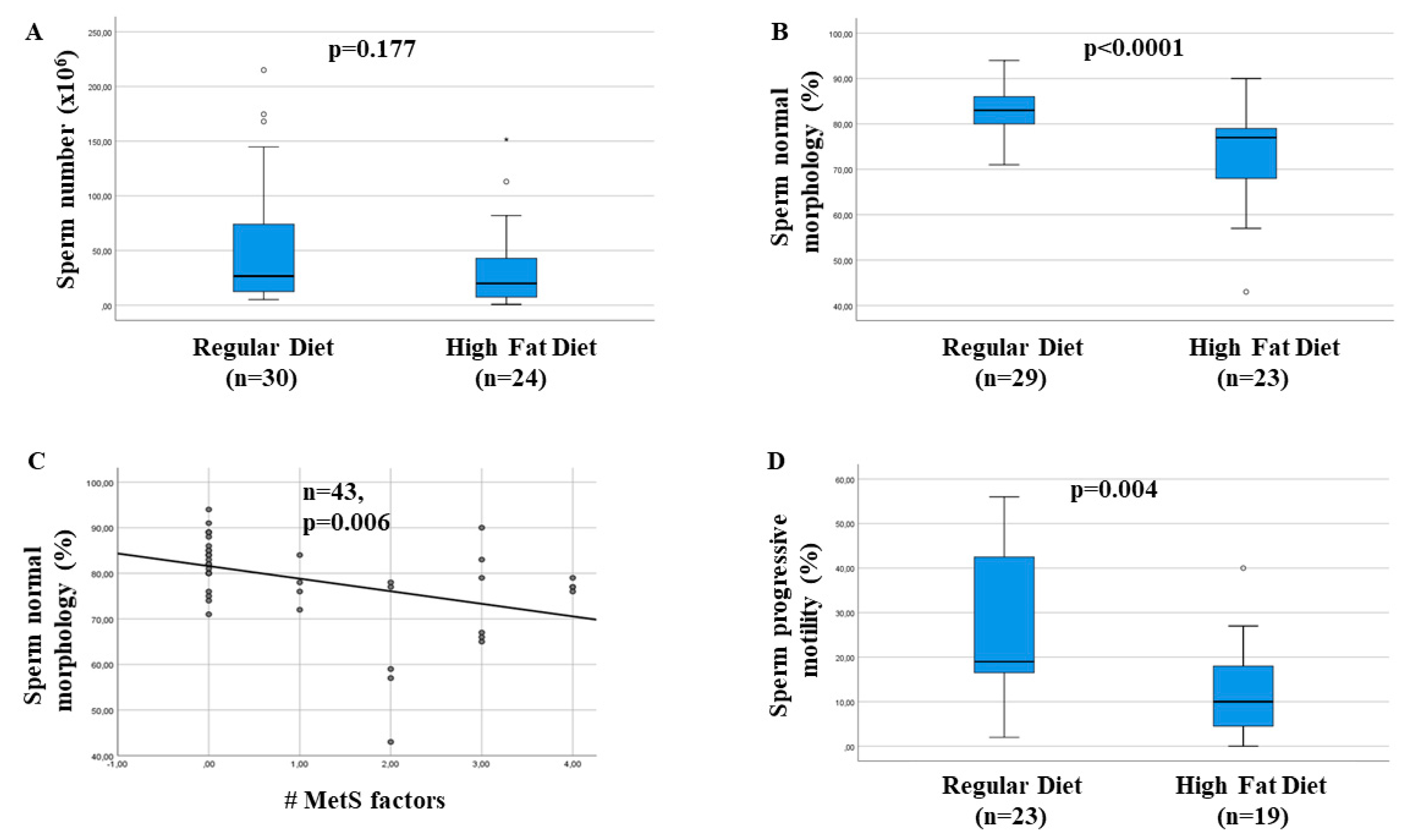
6.1.2. Summary of the Significant Associations Between MetS and Seminal Parameters Investigated
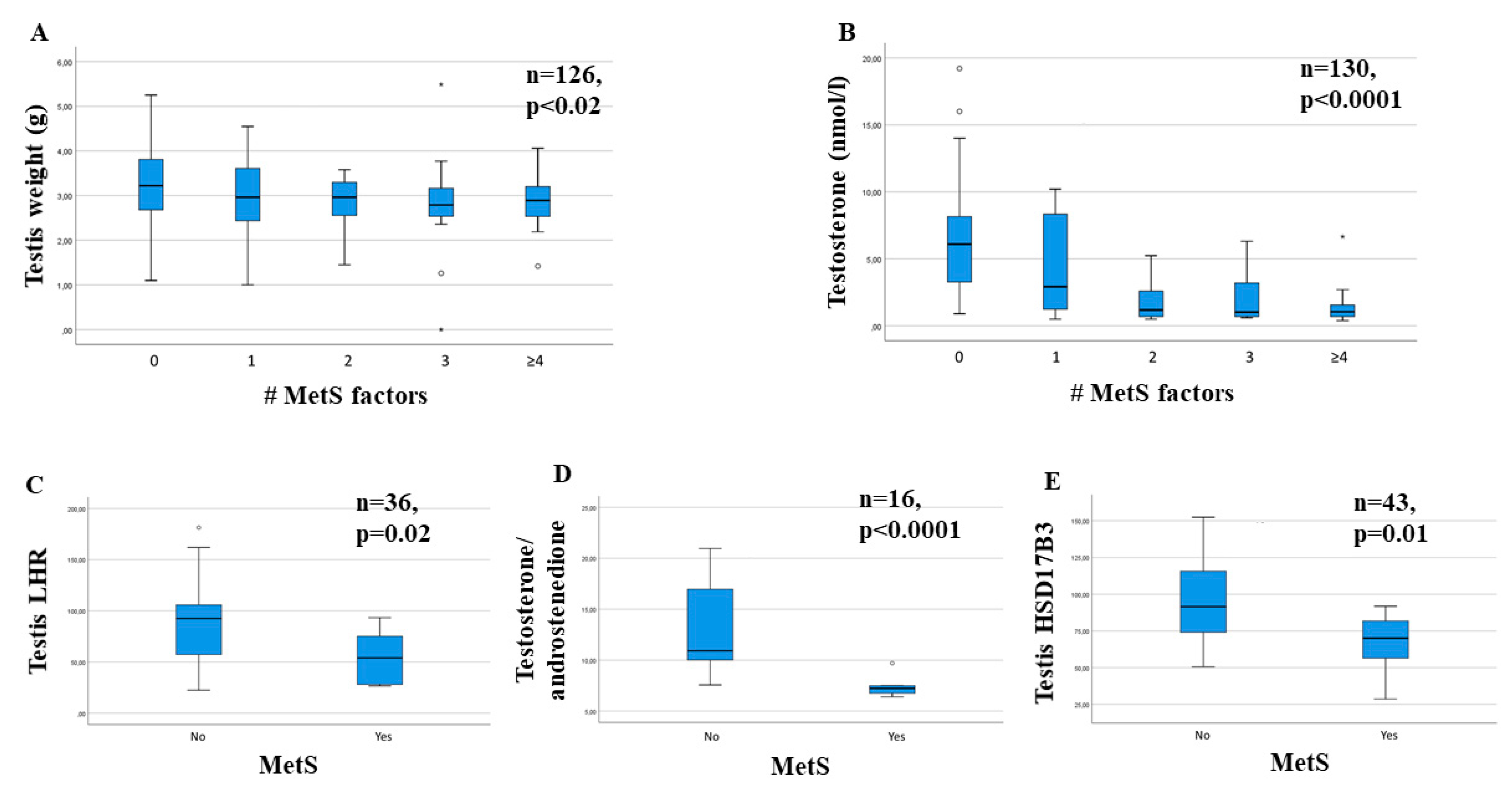
6.1.3. Summary of the Significant Associations Between MetS and Hormonal Parameters Investigated
7. Preclinical Studies
8. Treatment of MetS and Its Impact on Semen Quality
8.1. Treatment of Impaired Glucose Metabolism and Its Impact on Semen Quality
8.2. Treatment of Hypertension and Its Impact on Semen Quality
8.3. Treatment of Dyslipidemia and Its Impact on Semen Quality
8.4. Treatment of Obesity and Its Impact on Semen Quality
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cornier, M.A.; Dabelea, D.; Hernandez, T.L.; Lindstrom, R.C.; Steig, A.J.; Stob, N.R.; Van Pelt, R.E.; Wang, H.; Eckel, R.H. The metabolic syndrome. Endocr. Rev. 2008, 29, 777–822. [Google Scholar] [CrossRef]
- Eckel, R.H.; Alberti, K.G.M.M.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2010, 375, 181–183. [Google Scholar] [CrossRef]
- Lam, D.W.; LeRoith, D. Metabolic Syndrome. 2019 Feb 11. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dungan, K., Grossman, A., Hershman, J.M., Hofland, H.J., Kaltsas, G., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Cameron, A.J.; Shaw, J.E.; Zimmet, P.Z. The metabolic syndrome: Prevalence in worldwide populations. Endocrinol. Metab. Clin. N. Am. 2004, 33, 351–375. [Google Scholar] [CrossRef]
- Martins, A.D.; Majzoub, A.; Agawal, A. Metabolic syndrome and male fertility. World J. Mens Health 2019, 37, 113–127. [Google Scholar] [CrossRef]
- Reaven, G.M. Role of insulin resistance in human disease. Diabetes 1988, 37, 1595–1607. [Google Scholar] [CrossRef] [PubMed]
- Reaven, G.M. Role of insulin resistance in human disease (syndrome X): An expanded definition. Annu. Rev. Med. 1993, 44, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Pajunen, P.; Rissanen, H.; Härkänen, T.; Jula, A.; Reunanen, A.; Salomaa, V. The metabolic syndrome as a predictor of incident diabetes and cardiovascular events in the Health 2000 Study. Diabetes Metab. 2010, 36, 395–401. [Google Scholar] [CrossRef]
- Gale, E.A.M. Should we dump the metabolic syndrome?: Yes. BMJ 2008, 336, 640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kahn, R. Metabolic syndrome-what is the clinical usefulness? Lancet 2008, 371, 1892–1893. [Google Scholar] [CrossRef]
- Beltrán-Sánchez, H.; Harhay, M.O.; Harhay, M.M.; McElligott, S. Prevalence and Trends of Metabolic Syndrome in the Adult U.S. Population, 1999–2010. J. Am. Coll. Cardiol. 2013, 62, 697–703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simmons, R.K.; Alberti, K.G.M.M.; Gale, E.A.M.; Colagiuri, S.; Tuomilehto, J.; Qiao, Q.; Ramachandran, A.; Tajima, N.; Brajkovich Mirchov, I.; Ben-Nakhi, A.; et al. The metabolic syndrome: Useful concept or clinical tool? Report of a WHO expert consultation. Diabetologia 2010, 53, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Maseroli, E.; Corona, G.; Rastrelli, G.; Lotti, F.; Cipriani, S.; Forti, G.; Mannucci, E.; Maggi, M. Prevalence of endocrine and metabolic disorders in subjects with erectile dysfunction: A comparative study. J. Sex. Med. 2015, 12, 956–965. [Google Scholar] [CrossRef]
- Corona, G.; Rastrelli, G.; Balercia, G.; Lotti, F.; Sforza, A.; Monami, M.; Forti, G.; Mannucci, E.; Maggi, M. Hormonal Association and Sexual Dysfunction in Patients with Impaired Fasting Glucose: A Cross-Sectional and Longitudinal Study. J. Sex. Med. 2012, 9, 1669–1680. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Rastrelli, G.; Isidori, A.M.; Pivonello, R.; Bettocchi, C.; Reisman, Y.; Sforza, A.; Maggi, M. Erectile dysfunction and cardiovascular risk: A review of current findings. Expert Rev. Cardiovasc. Ther. 2020, 18, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Vlachopoulos, C.V.; Terentes-Printzios, D.G.; Ioakeimidis, N.K.; Aznaouridis, K.A.; Stefanadis, C.I. Prediction of cardiovascular events and all-cause mortality with erectile dysfunction a systematic review and meta-analysis of cohort studies. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 99–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corona, G.; Monami, M.; Rastrelli, G.; Melani, C.; Balzi, D.; Sforza, A.; Forti, G.; Mannucci, E.; Maggi, M. Is Metabolic Syndrome a Useless Category in Subjects with High Cardiovascular Risk? Results from a Cohort Study in Men with Erectile Dysfunction. J. Sex. Med. 2011, 8, 504–511. [Google Scholar] [CrossRef]
- Rastrelli, G.; Lotti, F.; Reisman, Y.; Sforza, A.; Maggi, M.; Corona, G. Metabolically healthy and unhealthy obesity in erectile dysfunction and male infertility. Expert Rev. Endocrinol. Metab. 2019, 14, 321–334. [Google Scholar] [CrossRef]
- Jensen, T.K.; Jacobsen, R.; Christensen, K.; Nielsen, N.C.; Bostofte, E. Good Semen Quality and Life Expectancy: A Cohort Study of 43,277 Men. Am. J. Epidemiol. 2009, 170, 559–565. [Google Scholar] [CrossRef] [Green Version]
- Eisenberg, M.L.; Li, S.; Behr, B.; Cullen, M.R.; Galusha, D.; Lamb, D.J.; Lipshultz, L.I. Semen quality, infertility and mortality in the USA. Hum. Reprod. 2014, 29, 1567–1574. [Google Scholar] [CrossRef] [Green Version]
- Latif, T.; Lindahl-Jacobsen, R.; Mehlsen, J.; Eisenberg, M.L.; Holmboe, S.A.; Pors, K.; Brinth, L.; Skouby, S.O.; Jørgensen, N.; Jensen, T.K. Semen quality associated with subsequent hospitalizations–Can the effect be explained by socio-economic status and lifestyle factors? Andrology 2018, 6, 428–435. [Google Scholar] [CrossRef] [Green Version]
- Ferlin, A.; Garolla, A.; Ghezzi, M.; Selice, R.; Palego, P.; Caretta, N.; Di Mambro, A.; Valente, U.; De Rocco Ponce, M.; Dipresa, S.; et al. Sperm Count and Hypogonadism as Markers of General Male Health. Eur. Urol. Focus 2019. [Google Scholar] [CrossRef]
- Cleeman, J.I. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). J. Am. Med. Assoc. 2001, 285, 2486–2497. [Google Scholar]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. The metabolic syndrome–A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- World Health Organization. Definition and Classification of Diabetes Mellitus and Its Complications Report of a WHO Consultation. Part 1: Diagnosis and Classification of Diabetes Mellitus; World Health Organization: Geneva, Switzerland, 1999; Document number WHO/NCD/NCS/99.2; Available online: https://apps.who.int/iris/bitstream/handle/10665/66040/WHO_NCD_NCS_99.2.pdf?sequence=1&isAllowed=y (accessed on 8 February 2021).
- Einhorn, D.; Reaven, G.M.; Cobin, R.H.; Ford, E.; Ganda, O.P.; Handelsman, Y.; Hellman, R.; Jellinger, P.S.; Kendall, D.; Krauss, R.M.; et al. American College of Endocrinology Position Statement on the Insulin Resistance Syndrome. Endocr. Pract. 2003, 9, 237–252. [Google Scholar]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [Green Version]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; American heart association; World heart federation; International atherosclerosis society; And international association for the study of obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- Corona, G.; Mannucci, E.; Forti, G.; Maggi, M. Hypogonadism, ED, metabolic syndrome and obesity: A pathological link supporting cardiovascular diseases. Int. J. Androl. 2009, 32, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Rastrelli, G.; Morelli, A.; Vignozzi, L.; Mannucci, E.; Maggi, M. Hypogonadism and metabolic syndrome. J. Endocrinol. Investig. 2011, 34, 557–567. [Google Scholar]
- Jaggers, J.R.; Sui, X.; Hooker, S.P.; LaMonte, M.J.; Matthews, C.E.; Hand, G.A.; Blair, S.N. Metabolic syndrome and risk of cancer mortality in men. Eur. J. Cancer 2009, 45, 1831–1838. [Google Scholar] [CrossRef] [Green Version]
- Esposito, K.; Chiodini, P.; Colao, A.; Lenzi, A.; Giugliano, D. Metabolic syndrome and risk of cancer: A systematic review and meta-analysis. Diabetes Care 2012, 35, 2402–2411. [Google Scholar] [CrossRef] [Green Version]
- Legro, R.S. A 27-year-old woman with a diagnosis of polycystic ovary syndrome. J. Am. Med. Assoc. 2007, 297, 509–519. [Google Scholar] [CrossRef]
- Norman, R.J.; Dewailly, D.; Legro, R.S.; Hickey, T.E. Polycystic ovary syndrome. Lancet 2007, 370, 685–697. [Google Scholar] [CrossRef] [Green Version]
- Corona, G.; Rastrelli, G.; Vignozzi, L.; Mannucci, E.; Maggi, M. Testosterone, cardiovascular disease and the metabolic syndrome. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 337–353. [Google Scholar] [CrossRef]
- Corona, G.; Monami, M.; Rastrelli, G.; Aversa, A.; Tishova, Y.; Saad, F.; Lenzi, A.; Forti, G.; Mannucci, E.; Maggi, M. Testosterone and Metabolic Syndrome: A Meta-Analysis Study. J. Sex. Med. 2011, 8, 272–283. [Google Scholar] [CrossRef]
- Dimopoulou, C.; Goulis, D.G.; Corona, G.; Maggi, M. The complex association between metabolic syndrome and male hypogonadism. Metabolism 2018, 86, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Rastrelli, G.; Filippi, S.; Sforza, A.; Maggi, M.; Corona, G. Metabolic Syndrome in Male Hypogonadism. Front. Horm. Res. 2018, 49, 131–155. [Google Scholar]
- Liu, L.H.; Zhang, T.; Zhang, Y.R.; Liu, T.S.; Zhang, H.B.; Chen, F.Z.; He, S.H.; Wei, A.Y. Metabolic syndrome and risk for ED: A meta-analysis. Int. J. Impot. Res. 2014, 26, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Besiroglu, H.; Otunctemur, A.; Ozbek, E. The Relationship between Metabolic Syndrome, Its Components, and Erectile Dysfunction: A Systematic Review and a Meta-Analysis of Observational Studies. J. Sex. Med. 2015, 12, 1309–1318. [Google Scholar] [CrossRef] [PubMed]
- Gacci, M.; Vignozzi, L.; Sebastianelli, A.; Salvi, M.; Giannessi, C.; De Nunzio, C.; Tubaro, A.; Corona, G.; Rastrelli, G.; Santi, R.; et al. Metabolic syndrome and lower urinary tract symptoms: The role of inflammation. Prostate Cancer Prostatic Dis. 2013, 16, 100–105. [Google Scholar] [CrossRef] [Green Version]
- Gacci, M.; Corona, G.; Vignozzi, L.; Salvi, M.; Serni, S.; De Nunzio, C.; Tubaro, A.; Oelke, M.; Carini, M.; Maggi, M. Metabolic syndrome and benign prostatic enlargement: A systematic review and meta-analysis. BJU Int. 2015, 115, 24–31. [Google Scholar] [CrossRef]
- Gacci, M.; De Nunzio, C.; Sebastianelli, A.; Salvi, M.; Vignozzi, L.; Tubaro, A.; Morgia, G.; Serni, S. Meta-Analysis of metabolic syndrome and prostate cancer. Prostate Cancer Prostatic Dis. 2017, 20, 146–155. [Google Scholar] [CrossRef]
- Wu, S.; He, H.; Wang, Y.; Xu, R.; Zhu, B.; Zhao, X. Association between benign prostate hyperplasia and metabolic syndrome in men under 60 years old: A meta-analysis. J. Int. Med. Res. 2019, 47, 5389–5399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corona, G.; Mannucci, E.; Schulman, C.; Petrone, L.; Mansani, R.; Cilotti, A.; Balercia, G.; Chiarini, V.; Forti, G.; Maggi, M. Psychobiologic Correlates of the Metabolic Syndrome and Associated Sexual Dysfunction. Eur. Urol. 2006, 50, 595–604. [Google Scholar] [CrossRef]
- Bagherniya, M.; Khayyatzadeh, S.S.; Avan, A.; Safarian, M.; Nematy, M.; Ferns, G.A.; Mokhber, N.; Ghayour-Mobarhan, M. Metabolic syndrome and its components are related to psychological disorders: A population based study. Diabetes Metab. Syndr. Clin. Res. Rev. 2017, 11, S561–S566. [Google Scholar] [CrossRef] [PubMed]
- Lotti, F.; Corona, G.; Degli Innocenti, S.; Filimberti, E.; Scognamiglio, V.; Vignozzi, L.; Forti, G.; Maggi, M. Seminal, ultrasound and psychobiological parameters correlate with metabolic syndrome in male members of infertile couples. Andrology 2013, 1, 229–239. [Google Scholar] [CrossRef]
- Kasturi, S.S.; Tannir, J.; Brannigan, R.E. The metabolic syndrome and male infertility. J. Androl. 2008, 29, 251–259. [Google Scholar] [CrossRef]
- Baskaran, S.; Agarwal, A.; Leisegang, K.; Pushparaj, P.N.; Panner Selvam, M.K.; Henkel, R. An in-depth bibliometric analysis and current perspective on male infertility research. World J. Mens Health 2019, 37. [Google Scholar] [CrossRef] [PubMed]
- Lotti, F.; Maggi, M. Sexual dysfunction and male infertility. Nat. Rev. Urol. 2018, 15, 287–307. [Google Scholar] [CrossRef]
- Friend, A.; Craig, L.; Turner, S. The prevalence of metabolic syndrome in children: A systematic review of the literature. Metab. Syndr. Relat. Disord. 2013, 11, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Rauner, A.; Mess, F.; Woll, A. The relationship between physical activity, physical fitness and overweight in adolescents: A systematic review of studies published in or after 2000. BMC Pediatr. 2013, 13, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hart, R.J.; Doherty, D.A.; Mori, T.A.; Adams, L.A.; Huang, R.C.; Minaee, N.; Handelsman, D.J.; McLachlan, R.; Norman, R.J.; Dickinson, J.E.; et al. Features of the metabolic syndrome in late adolescence are associated with impaired testicular function at 20 years of age. Hum. Reprod. 2019, 34, 389–402. [Google Scholar] [CrossRef] [Green Version]
- Bitew, Z.W.; Alemu, A.; Ayele, E.G.; Tenaw, Z.; Alebel, A.; Worku, T. Metabolic syndrome among children and adolescents in low and middle income countries: A systematic review and meta-analysis. Diabetol. Metab. Syndr. 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, U.; Sener, N.C.; Nalbant, I.; Karabacak, O.R.; Ulusoy, M.G.; Imamoglu, M.A. The effect of metabolic syndrome upon the success of varicocelectomy. Sci. World J. 2012, 2012. [Google Scholar] [CrossRef]
- Lotti, F.; Corona, G.; Vignozzi, L.; Rossi, M.; Maseroli, E.; Cipriani, S.; Gacci, M.; Forti, G.; Maggi, M. Metabolic syndrome and prostate abnormalities in male subjects of infertile couples. Asian J. Androl. 2014, 16, 295–304. [Google Scholar]
- Ventimiglia, E.; Capogrosso, P.; Colicchia, M.; Boeri, L.; Serino, A.; Castagna, G.; Clementi, M.C.; La Croce, G.; Regina, C.; Bianchi, M.; et al. Metabolic syndrome in white European men presenting for primary couple’s infertility: Investigation of the clinical and reproductive burden. Andrology 2016, 4, 944–951. [Google Scholar] [CrossRef] [Green Version]
- Ventimiglia, E.; Capogrosso, P.; Serino, A.; Boeri, L.; Colicchia, M.; La Croce, G.; Scano, R.; Papaleo, E.; Damiano, R.; Montorsi, F.; et al. Metabolic syndrome in White-European men presenting for secondary couple’s infertility: An investigation of the clinical and reproductive burden. Asian J. Androl. 2016, 18, 368. [Google Scholar]
- Ehala-Aleksejev, K.; Punab, M. The effect of metabolic syndrome on male reproductive health: A cross-sectional study in a group of fertile men and male partners of infertile couples. PLoS ONE 2018, 13, e0194395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dupont, C.; Faure, C.; Daoud, F.; Gautier, B.; Czernichow, S.; Lévy, R.; Aknin, I.; Cedrin-Durnerin, I.; Cens, S.; Chavatte-Palmer, P.; et al. Metabolic syndrome and smoking are independent risk factors of male idiopathic infertility. Basic Clin. Androl. 2019, 29, 1–7. [Google Scholar] [CrossRef]
- Elfassy, Y.; Bongrani, A.; Levy, P.; Foissac, F.; Fellahi, S.; Faure, C.; McAvoy, C.; Capeau, J.; Dupont, J.; Fève, B.; et al. Relationships between metabolic status, seminal adipokines, and reproductive functions in men from infertile couples. Eur. J. Endocrinol. 2019, 182, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Le, M.T.; Nguyen, D.N.; Le, D.D.; Tran, N.Q.T. Impact of body mass index and metabolic syndrome on sperm DNA fragmentation in males from infertile couples: A cross-sectional study from Vietnam. Metab. Open 2020, 7, 100054. [Google Scholar] [CrossRef]
- Lotti, F.; Frizza, F.; Balercia, G.; Barbonetti, A.; Behre, H.M.; Calogero, A.E.; Cremers, J.F.; Francavilla, F.; Isidori, A.M.; Kliesch, S.; et al. The European Academy of Andrology (EAA) ultrasound study on healthy, fertile men: Clinical, seminal and biochemical characteristics. Andrology 2020, 8, 1005–1020. [Google Scholar] [CrossRef]
- Leisegang, K.; Udodong, A.; Bouic, P.J.D.; Henkel, R.R. Effect of the metabolic syndrome on male reproductive function: A case-controlled pilot study. Andrologia 2014, 46, 167–176. [Google Scholar] [CrossRef] [Green Version]
- Leisegang, K.; Bouic, P.J.D.; Henkel, R.R. Metabolic syndrome is associated with increased seminal inflammatory cytokines and reproductive dysfunction in a case-controlled male cohort. Am. J. Reprod. Immunol. 2016, 76, 155–163. [Google Scholar] [CrossRef]
- Elsamanoudy, A.Z.; Abdalla, H.A.; Hassanien, M.; Gaballah, M.A. Spermatozoal cell death-inducing DNA fragmentation factor-α-like effector A (CIDEA) gene expression and DNA fragmentation in infertile men with metabolic syndrome and normal seminogram. Diabetol. Metab. Syndr. 2016, 8. [Google Scholar] [CrossRef] [Green Version]
- Pilatz, A.; Hudemann, C.; Wolf, J.; Halefeld, I.; Paradowska-Dogan, A.; Schuppe, H.C.; Hossain, H.; Jiang, Q.; Schultheiss, D.; Renz, H.; et al. Metabolic syndrome and the seminal cytokine network in morbidly obese males. Andrology 2017, 5, 23–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.Y.; Kao, T.W.; Peng, T.C.; Yang, H.F.; Chen-Jung, W.U.; Chen, W.L. Metabolic syndrome and semen quality in adult population. J. Diabetes 2020, 12, 294–304. [Google Scholar] [CrossRef] [PubMed]
- Saikia, U.; Saikia, K.; Sarma, D.; Appaiah, S. Sertoli cell function in young males with metabolic syndrome. Indian J. Endocrinol. Metab. 2019, 23, 251. [Google Scholar] [CrossRef]
- Zhao, L.; Pang, A. Effects of Metabolic Syndrome on Semen Quality and Circulating Sex Hormones: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction, 4th ed.; Cambridge University Press: New York, NY, USA, 1999. [Google Scholar]
- World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen, 5th ed.; WHO Press: Geneva, Switzerland, 2010. [Google Scholar]
- World Health Organization. WHO Manual for the Standardized Investigation and Diagnosis of the Infertile Couple; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Bungum, A.B.; Glazer, C.H.; Bonde, J.P.; Nilsson, P.M.; Giwercman, A.; Tøttenborg, S.S. Risk of metabolic disorders in childless men: A population-based cohort study. BMJ Open 2018, 8, e020293. [Google Scholar] [CrossRef] [Green Version]
- Elenkov, A.; Al-Jebari, Y.; Giwercman, A. More Prevalent Prescription of Medicine for Hypertension and Metabolic Syndrome in Males from Couples Undergoing Intracytoplasmic Sperm Injection. Sci. Rep. 2018, 8, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Muciaccia, B.; Pensini, S.; Culasso, F.; Padula, F.; Paoli, D.; Gandini, L.; Di Veroli, C.; Bianchini, G.; Stefanini, M.; D’Agostino, A. Higher clusterin immunolabeling and sperm DNA damage levels in hypertensive men compared with controls. Hum. Reprod. 2012, 27, 2267–2276. [Google Scholar] [CrossRef] [Green Version]
- Mbah, A.U.; Ndukwu, G.O.; Ghasi, S.I.; Shu, E.N.; Ozoemena, F.N.; Mbah, J.O.; Onodugo, O.D.; Ejim, E.C.; Eze, M.I.; Nkwo, P.O.; et al. Low-dose lisinopril in normotensive men with idiopathic oligospermia and infertility: A 5-year randomized, controlled, crossover pilot study. Clin. Pharmacol. Ther. 2012, 91, 582–589. [Google Scholar] [CrossRef]
- Cazzaniga, W.; Capogrosso, P.; Ventimiglia, E.; Pederzoli, F.; Boeri, L.; Frego, N.; Abbate, C.; Alfano, M.; Viganò, P.; Montorsi, F.; et al. High Blood Pressure Is a Highly Prevalent but Unrecognised Condition in Primary Infertile Men: Results of a Cross-sectional Study. Eur. Urol. Focus 2020, 6, 178–183. [Google Scholar] [CrossRef]
- Guo, D.; Li, S.; Behr, B.; Eisenberg, M.L. Hypertension and Male Fertility. World J. Mens Health 2017, 35, 59. [Google Scholar] [CrossRef]
- Lotti, F.; Maggi, M. Interleukin 8 and the male genital tract. J. Reprod. Immunol. 2013, 100, 54–65. [Google Scholar] [CrossRef]
- Lotti, F.; Corona, G.; Colpi, G.M.; Filimberti, E.; Degli Innocenti, S.; Mancini, M.; Baldi, E.; Noci, I.; Forti, G.; Adorini, L.; et al. Elevated body mass index correlates with higher seminal plasma interleukin 8 levels and ultrasonographic abnormalities of the prostate in men attending an andrology clinic for infertility. J. Endocrinol. Investig. 2011, 34, e336–e342. [Google Scholar]
- Lotti, F.; Corona, G.; Mancini, M.; Filimberti, E.; Degli Innocenti, S.; Colpi, G.M.; Baldi, E.; Noci, I.; Forti, G.; Adorini, L.; et al. Ultrasonographic and clinical correlates of seminal plasma interleukin-8 levels in patients attending an andrology clinic for infertility. Int. J. Androl. 2011, 34, 600–613. [Google Scholar] [CrossRef] [PubMed]
- Lotti, F.; Rastrelli, G.; Maseroli, E.; Cipriani, S.; Guaraldi, F.; Krausz, C.; Reisman, Y.; Sforza, A.; Maggi, M.; Corona, G. Impact of Metabolically Healthy Obesity in Patients with Andrological Problems. J. Sex. Med. 2019, 16, 821–832. [Google Scholar] [CrossRef]
- Lotti, F.; Corona, G.; Rastrelli, G.; Forti, G.; Jannini, E.A.; Maggi, M. Clinical Correlates of Erectile Dysfunction and Premature Ejaculation in Men with Couple Infertility. J. Sex. Med. 2012, 9, 2698–2707. [Google Scholar] [CrossRef]
- Lotti, F.; Maggi, M. Ultrasound of the male genital tract in relation to male reproductive health. Hum. Reprod. Update 2015, 21, 56–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nordström, E.A.; Rydén, M.; Backlund, E.C.; Dahlman, I.; Kaaman, M.; Blomqvist, L.; Cannon, B.; Nedergaard, J.; Arner, P. A human-specific role of cell death-inducing DFFA (DNA fragmentation factor-α)-like effector A (CIDEA) in adipocyte lipolysis and obesity. Diabetes 2005, 54, 1726–1734. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Dai, Y.; Bian, L.; Wang, W.; Wang, W.; Muramatsu, M.; Hua, Q. Association of the cell death-inducing DNA fragmentation factor alpha-like effector A (CIDEA) gene V115F (G/T) polymorphism with phenotypes of metabolic syndrome in a Chinese population. Diabetes Res. Clin. Pract. 2011, 91, 233–238. [Google Scholar] [CrossRef]
- Lotti, F.; Frizza, F.; Balercia, G.; Barbonetti, A.; Behre, H.M.; Calogero, A.E.; Cremers, J.; Francavilla, F.; Isidori, A.M.; Kliesch, S.; et al. The European Academy of Andrology (EAA) ultrasound study on healthy, fertile men: Scrotal ultrasound reference ranges and associations with clinical, seminal and biochemical characteristics. Andrology 2020. [Google Scholar] [CrossRef] [PubMed]
- Crean, A.J.; Senior, A.M. High-fat diets reduce male reproductive success in animal models: A systematic review and meta-analysis. Obes. Rev. 2019, 20, 921–933. [Google Scholar] [CrossRef]
- Filippi, S.; Vignozzi, L.; Morelli, A.; Chavalmane, A.K.; Sarchielli, E.; Fibbi, B.; Saad, F.; Sandner, P.; Ruggiano, P.; Vannelli, G.B.; et al. Testosterone partially ameliorates metabolic profile and erectile responsiveness to PDE5 inhibitors in an animal model of male metabolic syndrome. J. Sex. Med. 2009, 6, 3274–3288. [Google Scholar] [CrossRef] [PubMed]
- Morelli, A.; Filippi, S.; Comeglio, P.; Sarchielli, E.; Cellai, I.; Pallecchi, M.; Bartolucci, G.; Danza, G.; Rastrelli, G.; Corno, C.; et al. Physical activity counteracts metabolic syndrome-induced hypogonadotropic hypogonadism and erectile dysfunction in the rabbit. Am. J. Physiol. Endocrinol. Metab. 2019, 316, E519–E535. [Google Scholar] [CrossRef]
- Marchiani, S.; Vignozzi, L.; Filippi, S.; Gurrieri, B.; Comeglio, P.; Morelli, A.; Danza, G.; Bartolucci, G.; Maggi, M.; Baldi, E. Metabolic syndrome-associated sperm alterations in an experimental rabbit model: Relation with metabolic profile, testis and epididymis gene expression and effect of tamoxifen treatment. Mol. Cell. Endocrinol. 2015, 401, 12–24. [Google Scholar] [CrossRef]
- Mallidis, C.; Czerwiec, A.; Filippi, S.; O’Neill, J.; Maggi, M.; McClure, N. Spermatogenic and sperm quality differences in an experimental model of metabolic syndrome and hypogonadal hypogonadism. Reproduction 2011, 142, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Morelli, A.; Sarchielli, E.; Comeglio, P.; Filippi, S.; Vignozzi, L.; Marini, M.; Rastrelli, G.; Maneschi, E.; Cellai, I.; Persani, L.; et al. Metabolic syndrome induces inflammation and impairs gonadotropin-releasing hormone neurons in the preoptic area of the hypothalamus in rabbits. Mol. Cell. Endocrinol. 2014, 382, 107–119. [Google Scholar] [CrossRef]
- Morgante, G.; Tosti, C.; Orvieto, R.; Musacchio, M.C.; Piomboni, P.; De Leo, V. Metformin improves semen characteristics of oligo-terato-asthenozoospermic men with metabolic syndrome. Fertil. Steril. 2011, 95, 2150–2152. [Google Scholar] [CrossRef]
- Bosman, E.; Esterhuizen, A.D.; Rodrigues, F.A.; Becker, P.J.; Hoffmann, W.A. Effect of metformin therapy and dietary supplements on semen parameters in hyperinsulinaemic males. Andrologia 2015, 47, 974–979. [Google Scholar] [CrossRef] [Green Version]
- La Vignera, S.; Condorelli, R.A.; Duca, Y.; Cannarella, R.; Giacone, F.; Calogero, A.E. FSH treatment for normogonadotropic male infertility: A synergistic role for metformin? Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 5994–5998. [Google Scholar] [PubMed]
- Talebi, A.R.; Vahidi, S.; Aflatoonian, A.; Ghasemi, N.; Ghasemzadeh, J.; Firoozabadi, R.D.; Moein, M.R. Cytochemical evaluation of sperm chromatin and DNA integrity in couples with unexplained recurrent spontaneous abortions. Andrologia 2012, 44 (Suppl. 1), 462–470. [Google Scholar] [CrossRef]
- Calle-Guisado, V.; Gonzalez-Fernandez, L.; Martin-Hidalgo, D.; Garcia-Marin, L.J.; Bragado, M.J. Metformin inhibits human spermatozoa motility and signalling pathways mediated by protein kinase A and tyrosine phosphorylation without affecting mitochondrial function. Reprod. Fertil. Dev. 2019, 31, 787–795. [Google Scholar] [CrossRef]
- Liu, C.Y.; Chang, T.C.; Lin, S.H.; Wu, S.T.; Cha, T.L.; Tsao, C.W. Metformin Ameliorates Testicular Function and Spermatogenesis in Male Mice with High-Fat and High-Cholesterol Diet-Induced Obesity. Nutrients 2020, 12, 1932. [Google Scholar] [CrossRef]
- McPherson, N.O.; Lane, M. Metformin treatment of high-fat diet-fed obese male mice restores sperm function and fetal growth, without requiring weight loss. Asian J. Androl. 2020, 22, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Leisegang, K.; Almaghrawi, W.; Henkel, R. The effect of Nigella sativa oil and metformin on male seminal parameters and testosterone in Wistar rats exposed to an obesogenic diet. Biomed. Pharmacother. 2021, 133, 111085. [Google Scholar] [CrossRef] [PubMed]
- Derkach, K.V.; Bakhtyukov, A.A.; Bayunova, L.V.; Zorina, I.I.; Shpakov, A.O. Normalization of Testicular Steroidogenesis and Spermatogenesis in Male Rats with Type 2 Diabetes Mellitus under the Conditions of Metformin Therapy. Dokl. Biol. Sci. 2020, 493, 110–113. [Google Scholar] [CrossRef]
- Yan, W.J.; Mu, Y.; Yu, N.; Yi, T.L.; Zhang, Y.; Pang, X.L.; Cheng, D.; Yang, J. Protective effects of metformin on reproductive function in obese male rats induced by high-fat diet. J. Assist. Reprod. Genet. 2015, 32, 1097–1104. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Elías, M.D.; Rainero Cáceres, T.S.; Giaccagli, M.M.; Guazzone, V.A.; Dalton, G.N.; De Siervi, A.; Cuasnicú, P.S.; Cohen, D.J.; Da Ros, V.G. Association between high-fat diet feeding and male fertility in high reproductive performance mice. Sci. Rep. 2019, 9, 18546. [Google Scholar] [CrossRef]
- Abd El-Hakim, Y.M.; Abdel-Rahman Mohamed, A.; Khater, S.I.; Hamed Arisha, A.; Metwally, M.M.M.; Nassan, M.A.; Hassan, M.E. Chitosan-Stabilized Selenium Nanoparticles and Metformin Synergistically Rescue Testicular Oxidative Damage and Steroidogenesis-Related Genes Dysregulation in High-Fat Diet/Streptozotocin-Induced Diabetic Rats. Antioxidants 2020, 10, 17. [Google Scholar] [CrossRef]
- Ebokaiwe, A.P.; Obeten, K.E.; Okori, S.O.; David, E.E.; Olusanya, O.; Chukwu, C.J.; Okoro, N.; Ehiri, R.C. Co-administration of Selenium Nanoparticles and Metformin Abrogate Testicular Oxidative Injury by Suppressing Redox Imbalance, Augmenting Sperm Quality and Nrf2 Protein Expression in Streptozotocin-Induced Diabetic Rats. Biol. Trace Elem. Res. 2020, 198, 544–556. [Google Scholar] [CrossRef]
- Nna, V.U.; Bakar, A.B.A.; Ahmad, A.; Umar, U.Z.; Suleiman, J.B.; Zakaria, Z.; Othman, Z.A.; Mohamed, M. Malaysian propolis and metformin mitigate subfertility in streptozotocin-induced diabetic male rats by targeting steroidogenesis, testicular lactate transport, spermatogenesis and mating behaviour. Andrology 2020, 8, 731–746. [Google Scholar] [CrossRef]
- Rindone, G.M.; Gorga, A.; Pellizzari, E.H.; Del Carmen Camberos, M.; Galardo, M.N.; Da Ros, V.G.; Buffone, M.G.; Meroni, S.B.; Riera, M.F. Postnatal metformin treatment alters rat Sertoli cell proliferation and daily sperm production. Andrology 2020. Dec 11. Epub ahead of print. [Google Scholar]
- Fontoura, P.; Cardoso, M.C.; Erthal-Martins, M.C.; Werneck, C.; Sartorio, C.; Ramos, C.F. The effects of liraglutide on male fertility: A case report. Reprod. Biomed. Online 2014, 29, 644–646. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Öztaş, E.; Yılmaz, T.E.; Güzel, E.; Sezer, Z.; Okyar, A.; Özhan, G. Gliclazide alone or in combination with atorvastatin ameliorated reproductive damage in streptozotocin-induced type 2 diabetic male rats. Saudi Pharm. J. 2019, 27, 422–431. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Takaba, H.; Hashimoto, J.; Miyake, K.; Mitsuya, H. Successful treatment of oligospermic and azoospermic men with alpha 1-blocker and beta-stimulator: New treatment for idiopathic male infertility. Fertil Steril 1986, 46, 1162–1164. [Google Scholar] [CrossRef]
- Miyake, K.; Yamamoto, M.; Narita, H.; Hashimoto, J.; Mitsuya, H. Evidence for contractility of the human seminiferous tubule confirmed by its response to noradrenaline and acetylcholine. Fertil. Steril. 1986, 46, 734–737. [Google Scholar] [CrossRef]
- Gülmez, I.; Tatlişen, A.; Karacagil, M.; Kesekci, S. Seminal parameters of ejaculates collected successively with sixty minute interval in infertile men: Effect of combination of prazosin and terbutaline on these parameters. Andrologia 1991, 23, 167–169. [Google Scholar] [CrossRef]
- Banihani, S.A. Effect of captopril on semen quality. Andrologia 2017, 49, e12641. [Google Scholar] [CrossRef]
- Samplaski, M.K.; Nangia, A.K. Adverse effects of common medications on male fertility. Nat. Rev. Urol. 2015, 12, 401–413. [Google Scholar] [CrossRef] [PubMed]
- Semet, M.; Paci, M.; Saïas-Magnan, J.; Metzler-Guillemain, C.; Boissier, R.; Lejeune, H.; Perrin, J. The impact of drugs on male fertility: A review. Andrology 2017, 5, 640–663. [Google Scholar] [CrossRef] [PubMed]
- Akagashi, K.; Kumamoto, Y.; Itoh, N.; Tsukamoto, T.; Suzuki, T.; Ohta, Y. Manidipine improves spermatogenesis in the stroke-prone spontaneously hypertensive rat. J. Androl. 1997, 18, 210–216. [Google Scholar]
- Banihani, S.A. Effect of statin on semen quality characteristics. Andrologia 2020, 52, e13592. [Google Scholar]
- Keihani, S.; Martin, C.; Craig, J.R.; Zhang, C.; Presson, A.P.; Myers, J.B.; Aston, K.I.; Emery, B.R.; Carrell, D.T.; Hotaling, J.M. Semen parameters are unaffected by statin use in men evaluated for infertility. Andrologia 2018, 50, e12995. [Google Scholar] [CrossRef]
- Cai, T.; Mondaini, N.; Mazzoli, S.; Bartoletti, R. A possible negative effect of co-administered amlodipine and atorvastatin on semen volume and spermatozoa in men. J. Pharm. Pharmacol. 2008, 60, 1431–1432. [Google Scholar] [CrossRef]
- Dobs, A.S.; Sarma, P.S.; Schteingart, D. Long-term endocrine function in hypercholesterolemic patients treated with pravastatin, a new 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor. Metabolism 1993, 42, 1146–1152. [Google Scholar] [CrossRef]
- Cui, X.; Long, C.; Zhu, J.; Tian, J. Protective Effects of Fluvastatin on Reproductive Function in Obese Male Rats Induced by High-Fat Diet through Enhanced Signaling of mTOR. Cell. Physiol. Biochem. 2017, 41, 598–608. [Google Scholar] [CrossRef] [PubMed]
- Heeba, G.H.; Hamza, A.A. Rosuvastatin ameliorates diabetes-induced reproductive damage via suppression of oxidative stress, inflammatory and apoptotic pathways in male rats. Life Sci. 2015, 141, 13–19. [Google Scholar] [CrossRef]
- Delashoub, M.; Ziaee, M.; Khorrami, A.; Banan-Khojasteh, S.M. Comparison of the Effects of Clofibrate and Silafibrate on Sperm Parameters Quality and Sex Hormones in Male Rats. Urol. J. 2018, 15, 38–43. [Google Scholar] [PubMed]
- Lee, Y.; Dang, J.T.; Switzer, N.; Yu, J.; Tian, C.; Birch, D.W.; Karmali, S. Impact of Bariatric Surgery on Male Sex Hormones and Sperm Quality: A Systematic Review and Meta-Analysis. Obes. Surg. 2019, 29, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Mannucci, E.; Forti, G.; Maggi, M. Following the common association between testosterone deficiency and diabetes mellitus, can testosterone be regarded as a new therapy for diabetes? Int. J. Androl. 2009, 32, 431–441. [Google Scholar] [CrossRef] [PubMed]


| NCEP-ATPIII [23] | IDF [24] | WHO [25] | ACE [26] | AHA/NHLBI [27] | IDF&AHA/NHLBI [28] |
|---|---|---|---|---|---|
| 3 or more of the following | Central obesity (waist circumference ≥ 94 cm) and 2 or more of the following | Fasting insulin in top 25%; fasting glucose ≥ 100 mg/dL (6.1 mmol/L); 2 h glucose ≥ 140 mg/dL (7.8 mmol/L) and 2 or more of the following | High risk of insulin resistance: 2h plasma glucose ≥ 140 (7.8 mmol/L) and < 200 mg/dL (11 mmol/L) and 2 or more of the following | 3 or more of the following | 3 or more of the following |
|
|
|
| ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Author | Cohort Studied (# Men, Country, Mean Age) | MetS Definition Used | MetS Prevalence |
|---|---|---|---|
| Infertile Men | |||
| Ozturk et al., (2012) [55] | 104 infertile men (Turkey) (28.2 years) | Arbitrary § | 46.0% |
| Lotti et al., (2013) [47] | 351 males of infertile couples (Italy) (36.0 ± 8.0 years) | IDF & AHA/NHLBI | 7.7% |
| Lotti et al., (2014) [56] | 171 males of infertile couples (Italy) (36.6 ± 8.4 years) | NCEP-ATPIII | 12.9% |
| Ventimiglia et al., 2016 [57] | 1337 men with primary infertility (Italy) (36.5 years) | NCEP-ATPIII | 9.6% |
| Ventimiglia et al., 2017 [58] | 167 men with secondary infertility (Italy) (22−68 years) | NCEP-ATPIII | 12.0% |
| Ehala-Aleksejev and Punab (2018) [59] | 2642 males of infertile couples (Estonia) (32.6 ± 5.7 years) | NCEP-ATPIII | 17.8% |
| Ferlin et al. (2019) [22] | 5177 males of infertile couples (Italy) (31.7 ± 7.9 years) | NCEP-ATPIII | 7.4% |
| Dupont et al. (2019) [60] | 96 fertile men (France) (33.3 years) | IDF & AHA/NHLBI | 17.8% |
| Elfassy et al. (2020) [61] | 154 males of infertile couples (France) (37.1 ± 0.4 years) | IDF & AHA/NHLBI | 29.0% |
| Le et al. (2020) [62] | 290 males of infertile couples (Vietnam) (35.3 ± 5.9 years) | AHA/NHLBI | 22.0% |
| Fertile men | |||
| Ehala-Aleksejev and Punab (2018) [59] | 238 fertile men (Estonia) (32.0 ± 6.1 years) | NCEP-ATPIII | 12.2% |
| Dupont et al. (2019) [60] | 100 fertile men (France) (34.4 years) | IDF & AHA/NHLBI | 6.1% |
| Lotti et al. (2020) [63] | 248 fertile men (Italy) (35.3 ± 5.9 years) | IDF & AHA/NHLBI | 12.9% |
| NCEP-ATPIII | 6.9% | ||
| Comparison of MetS prevalence of fertile and infertile men | |||
| Ehala-Aleksejev and Punab (2018) [59] | 2642 males of infertile couples vs. 238 fertile men | NCEP-ATPIII | 17.% vs. 12.2% (p = 0.028) |
| Dupont et al. (2019) [60] | 96 infertile vs. 100 fertile men | IDF & AHA/NHLBI | 17.9% vs. 6.1% (p = 0.012) |
| Author | Cohort Studied | MetS Definition | # Subjects | Type of Analysis | Semen Volume | Sperm Concentration | Sperm Total Count | Sperm Motility | Sperm Normal Morphology | Sperm Vitality |
|---|---|---|---|---|---|---|---|---|---|---|
| Ozturk et al., 2012 [55] ^ | Men with infertility and varicocele (Turkey) | Arbitrary § | MetS, 48 No-MetS, 56 | Comparison of MetS vs. no-MetS men | NE | NE | Lower in MetS men | Lower in MetS men | No difference | NE |
| Lotti et al., 2013 * [47] | Males of infertile couples (Italy) | IDF & AHA/NHLBI | MetS, 27 No-MetS, 324 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference (p) | Lower in MetS men | NE |
| Correlation between # of MetS components and seminal parameters | No correlation | No correlation | No correlation | No correlation | Negative correlation | NE | ||||
| Lotti et al., 2014 [56] | Males of infertile couples (Italy) | NCEP-ATPIII | MetS, 22 No-MetS, 149 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference (p) | Lower in MetS men | NE |
| Correlation between # of MetS components and seminal parameters | No correlation | No correlation | No correlation | No correlation | Negative correlation | NE | ||||
| Leisegang et al., 2014 * [64] | Men from the general population (South Africa) | IDF & AHA/NHLBI | MetS, 26 No-MetS, 28 | Comparison of MetS vs. no-MetS men | No difference | Lower in MetS men | Lower in MetS men | Total (but not progressive) motility lower in MetS men | NE | Lower in MetS men |
| Leisegang et al., 2016 * [65] | Men from the general population (South Africa) | IDF & AHA/NHLBI | MetS, 42 No-MetS, 32 | Comparison of MetS vs. no-MetS men | Lower in MetS men | Lower in MetS men | Lower in MetS men | Total and progressive motility lower in MetS men | NE | NE |
| Ventimiglia et al., 2016 * [57] | Men with primary infertility (Italy) | NCEP-ATPIII | MetS, 128 No-MetS, 1209 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference (p) | No difference | NE |
| Elsamanoudy et al., 2016 * [66] | 37 infertile men with MetS and 45 fertile men w/o MetS (Egypt) | IDF & AHA/NHLBI | MetS, 37 No-MetS, 45 | Comparison of MetS vs. no-MetS men | No difference | NE | No difference | Lower in MetS men (p) | Lower in MetS men | Lower in MetS men |
| 38 fertile men with MetS and 45 fertile men w/o MetS (Egypt) | IDF & AHA/NHLBI | MetS, 38 No-MetS, 45 | Comparison of MetS vs. no-MetS men | No difference | NE | No difference | No difference (p) | No difference | Lower in MetS men | |
| Pilatz et al., 2017 * [67] | 27 MetS men and 27 healthy men (Germany) | IDF | MetS, 27 No-MetS, 27 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference (p) | No difference | NE |
| Ventimiglia et al., 2017 * [58] | Men with secondary infertility (Italy) | NCEP-ATPIII | MetS, 20 No-MetS, 147 | Comparison of MetS vs. no-MetS men | Lower in MetS men | Lower in MetS men | No difference | No difference (p) | Lower in MetS men | NE |
| Ehala-Aleksejev and Punab, 2018 * [59] | Males of infertile couples (Estonia) | NCEP-ATPIII | MetS, 471 No-MetS, 2171 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference | No difference | NE |
| Fertile men (Estonia) | NCEP-ATPIII | MetS, 29 No-MetS, 209 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference | No difference | NE | |
| Chen et al., 2019 * [68] | Men from the general population (China) | IDF & AHA/NHLBI | MetS, 885 No-MetS, 7510 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | Total (but not progressive) motility lower in MetS men | Lower in MetS men | NE |
| Correlation between # of MetS components and seminal parameters | No correlation | No correlation | No correlation | Inverse relationship with men with ≥ 4 MetS components | Inverse relationship with men with 3 MetS components | NE | ||||
| Saikia et al., 2019 * [69] | 50 Young adult males with MetS and 30 age-matched healthy males (India) | IDF | MetS, 50 No-MetS, 30 | Comparison of MetS vs. no-MetS men | Lower in MetS men | NE | Lower in MetS men | Total and progressive motility lower in MetS men | No difference | NE |
| Elfassy et al., 2020 [61] | Males of infertile couples (France) | IDF & AHA/NHLBI | MetS, 45 No-MetS, 109 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference (p) | No difference | No difference |
| Le et al., 2020 [62] | Males of infertile couples (Vietnam) | AHA/NHLBI | MetS, 65 No-MetS, 225 | Comparison of MetS vs. no-MetS men | NE | No difference | NE | No difference (p) | No difference | No difference |
| Zhao and Pang, 2020 [70] | Meta-analysis | Various | MetS, 1731 No-MetS, 11740 | Comparison of MetS vs. no-MetS men | Lower in MetS men | Lower in MetS men | Lower in MetS men | Lower in MetS men | Lower in MetS men | Lower in MetS men |
| Lotti et al., 2020 [63] | 248 fertile men (Italy) | IDF & AHA/NHLBI | MetS, 32 No-MetS, 216 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference (p) | No difference | No difference |
| NCEP-ATPIII | MetS, 17 No-MetS, 231 | Comparison of MetS vs. no-MetS men | No difference | No difference | No difference | No difference (p) | No difference | No difference |
| Author | Cohort Studied | MetS Definition | # Subjects | Type of Analysis | Sperm DNA Fragmentation | MMP | Testosterone Levels | LH Levels | FSH Levels | Inhibin B Levels |
|---|---|---|---|---|---|---|---|---|---|---|
| Lotti et al., 2013 * [47] | Males of infertile couples | IDF & AHA/NHLBI | MetS, 27 No-MetS, 324 | Comparison of MetS vs. no-MetS men | NE | NE | Lower in MetS men | No difference | No difference | NE |
| Correlation between # of MetS components and seminal or hormonal parameters | NE | NE | Negative correlation | No correlation | No correlation | NE | ||||
| Lotti et al., 2014 [56] | Males of infertile couples | NCEP-ATPIII | MetS, 22 No-MetS, 149 | Comparison of MetS vs. no-MetS men | NE | NE | No difference | No difference | No difference | NE |
| Correlation between # of MetS components and seminal or hormonal parameters | NE | NE | NE | No correlation | No correlation | NE | ||||
| Leisegang et al., 2014 * [64] | Men from the general population | IDF & AHA/NHLBI | MetS, 26 No-MetS, 28 | Comparison of MetS vs. no-MetS men | Higher in MetS men | Lower in MetS men | Lower in MetS men (saliva) | NE | NE | NE |
| Leisegang et al., 2016 * [65] | Men from the general population | IDF & AHA/NHLBI | MetS, 42 No-MetS, 32 | Comparison of MetS vs. no-MetS men | Higher in MetS men | Lower in MetS men | NE | NE | NE | NE |
| Ventimiglia et al., 2016 * [57] | Men with primary infertility | NCEP-ATPIII | MetS, 128 No-MetS, 1209 | Comparison of MetS vs. no-MetS men | NE | NE | Lower in MetS men | No difference | No difference | Lower in MetS men |
| Ventimiglia et al., 2017 * [58] | Men with secondary infertility | NCEP-ATPIII | MetS, 20 No-MetS, 147 | Comparison of MetS vs. no-MetS men | NE | NE | Lower in MetS men | No difference | No difference | Lower in MetS men |
| Pilatz et al., 2017 * [67] | 27 MetS men and 27 healthy men | IDF | MetS, 27 No-MetS, 27 | Comparison of MetS vs. no-MetS men | NE | NE | Lower in MetS men | No difference | No difference | NE |
| Ehala-Aleksejev and Punab, 2018 * [59] | Males of infertile couples | NCEP-ATPIII | MetS, 471 No-MetS, 2171 | Comparison of MetS vs. no-MetS men | NE | NE | Lower in MetS men | Lower in MetS men | No difference | NE |
| Fertile men | NCEP-ATPIII | MetS, 29 No-MetS, 209 | Comparison of MetS vs. no-MetS men | NE | NE | Lower in MetS men | No difference | No difference | NE | |
| Saikia et al., 2019 * [69] | 50 young adult males with MetS and 30 age-matched healthy males | IDF | MetS, 50 No-MetS, 30 | Comparison of MetS vs. no-MetS men | NE | NE | Lower in MetS men | NE | Lower in MetS men | Lower in MetS men |
| Elfassy et al., 2020 [61] | Males of infertile couples | IDF & AHA/NHLBI | MetS, 45 No-MetS, 109 | Comparison of MetS vs. no-MetS men | No difference | NE | Lower in MetS men | No difference | No difference | Lower in MetS men |
| Zhao and Pang, 2020 [70] | Meta-analysis | Various | MetS, 1731 No-MetS, 11740 | Comparison of MetS vs. no-MetS men | Higher in MetS men | Lower in MetS men | Lower in MetS men | No difference | Lower in MetS men | Lower in MetS men |
| Lotti et al., 2020 [63] | 248 fertile men | IDF & AHA/NHLBI | MetS, 32 No-MetS, 216 | Comparison of MetS vs. no-MetS men | NE | NE | No difference | No difference | No difference | NE |
| NCEP-ATPIII | MetS, 17 No-MetS, 231 | Comparison of MetS vs. no-MetS men | NE | NE | No difference | No difference | No difference | NE |

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lotti, F.; Marchiani, S.; Corona, G.; Maggi, M. Metabolic Syndrome and Reproduction. Int. J. Mol. Sci. 2021, 22, 1988. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms22041988
Lotti F, Marchiani S, Corona G, Maggi M. Metabolic Syndrome and Reproduction. International Journal of Molecular Sciences. 2021; 22(4):1988. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms22041988
Chicago/Turabian StyleLotti, Francesco, Sara Marchiani, Giovanni Corona, and Mario Maggi. 2021. "Metabolic Syndrome and Reproduction" International Journal of Molecular Sciences 22, no. 4: 1988. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms22041988






