Smartphones and Threshold-Based Monitoring Methods Effectively Detect Falls Remotely: A Systematic Review
Abstract
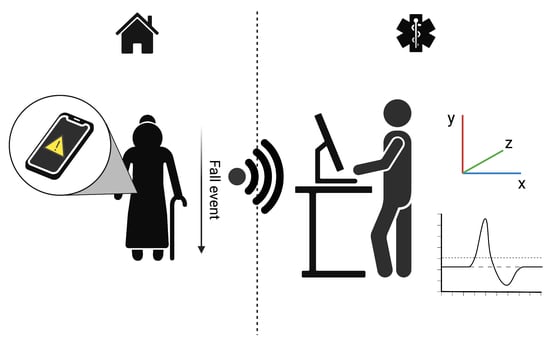
:1. Introduction
2. Material and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
2.3. Study Selection and Data Collection Process
2.4. Risk Bias Assessment
3. Results
3.1. Study Characteristics
3.2. Fall Prevention Studies
3.3. Fall Detection Studies
4. Discussion
4.1. Background on Fall Detection and Prevention
4.2. Smartphone Potential for Fall Detection and Prevention
4.3. Sensor Positioning
4.4. Methods to Determine a Threshold for Fall Detection and Prevention
4.5. Future Applications
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burns, E.; Kakara, R. Deaths from Falls Among Persons Aged ≥65 Years—United States, 2007–2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 509–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oh-Park, M.; Doan, T.; Dohle, C.; Vermiglio-Kohn, V.; Abdou, A. Technology Utilization in Fall Prevention. Am. J. Phys. Med. Rehabil. 2021, 100, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Burns, E.R.; Stevens, J.A.; Lee, R. The direct costs of fatal and non-fatal falls among older adults—United States. J. Saf. Res. 2016, 58, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.; Stevens, J.; Drake, C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [Green Version]
- Houry, D.; Florence, C.; Baldwin, G.; Stevens, J.; McClure, R. The CDC Injury Center’s response to the growing public health problem of falls among older adults. Am. J. Lifestyle Med. 2016, 10, 74–77. [Google Scholar] [CrossRef] [PubMed]
- Bouldin, E.L.; Andresen, E.M.; Dunton, N.E.; Simon, M.; Waters, T.M.; Liu, M.; Daniels, M.J.; Mion, L.C.; Shorr, R.I. Falls among adult patients hospitalized in the United States: Prevalence and trends. J. Patient Saf. 2013, 9, 13–27. [Google Scholar] [CrossRef] [Green Version]
- Rubenstein, L.Z.; Josephson, K.R. The epidemiology of falls and syncope. Clin. Geriatr. Med. 2002, 18, 141–158. [Google Scholar] [CrossRef]
- Bates, D.W.; Pruess, K.; Souney, P.; Platt, R. Serious falls in hospitalized patients: Correlates and resource utilization. Am. J. Med. 1995, 99, 137–143. [Google Scholar] [CrossRef]
- Brand, C.A.; Sundararajan, V. A 10-year cohort study of the burden and risk of in-hospital falls and fractures using routinely collected hospital data. Qual. Saf. Health Care 2010, 19, e51. [Google Scholar] [CrossRef] [Green Version]
- Turner, K.; Staggs, V.S.; Potter, C.; Cramer, E.; Shorr, R.I.; Mion, L.C. Fall Prevention Practices and Implementation Strategies: Examining Consistency Across Hospital Units. J. Patient Saf. 2022, 18, e236–e242. [Google Scholar] [CrossRef]
- Haines, T.P.; Bennell, K.L.; Osborne, R.H.; Hill, K.D. Effectiveness of targeted falls prevention programme in subacute hospital setting: Randomised controlled trial. BMJ 2004, 328, 676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coussement, J.; De Paepe, L.; Schwendimann, R.; Denhaerynck, K.; Dejaeger, E.; Milisen, K. Interventions for preventing falls in acute- and chronic-care hospitals: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2008, 56, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Miake-Lye, I.M.; Hempel, S.; Ganz, D.A.; Shekelle, P.G. Inpatient fall prevention programs as a patient safety strategy: A systematic review. Ann. Intern Med. 2013, 158 (5 Pt 2), 390–396. [Google Scholar] [CrossRef] [Green Version]
- Hempel, S.; Newberry, S.; Wang, Z.; Booth, M.; Shanman, R.; Johnsen, B.; Shier, V.; Saliba, D.; Spector, W.D.; Ganz, D.A. Hospital fall prevention: A systematic review of implementation, components, adherence, and effectiveness. J. Am. Geriatr. Soc. 2013, 61, 483–494. [Google Scholar] [CrossRef] [PubMed]
- Oliver, D.; Connelly, J.B.; Victor, C.R.; Shaw, F.E.; Whitehead, A.; Genc, Y.; Vanoli, A.; Martin, F.C.; Gosney, M.A. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: Systematic review and meta-analyses. BMJ 2007, 334, 82. [Google Scholar] [CrossRef] [Green Version]
- Oliver, D.; Daly, F.; Martin, F.C.; McMurdo, M.E. Risk factors and risk assessment tools for falls in hospital in-patients: A systematic review. Age Ageing 2004, 33, 122–130. [Google Scholar] [CrossRef] [Green Version]
- Oliver, D.; Hopper, A.; Seed, P. Do hospital fall prevention programs work? A systematic review. J. Am. Geriatr. Soc. 2000, 48, 1679–1689. [Google Scholar] [CrossRef]
- Shorr, R.I.; Chandler, A.M.; Mion, L.C.; Waters, T.M.; Liu, M.; Daniels, M.J.; Kessler, L.A.; Miller, S.T. Effects of an intervention to increase bed alarm use to prevent falls in hospitalized patients: A cluster randomized trial. Ann. Intern. Med. 2012, 157, 692–699. [Google Scholar] [CrossRef] [Green Version]
- LeLaurin, J.H.; Shorr, R.I. Preventing Falls in Hospitalized Patients: State of the Science. Clin. Geriatr. Med. 2019, 35, 273–283. [Google Scholar] [CrossRef]
- Schoen, M.W.; Cull, S.; Buckhold, F.R. False Bed Alarms: A Teachable Moment. JAMA Intern. Med. 2016, 176, 741–742. [Google Scholar] [CrossRef]
- Sendelbach, S.; Funk, M. Alarm fatigue: A patient safety concern. AACN Adv. Crit. Care 2013, 24, 378–386, quiz 387–388. [Google Scholar] [CrossRef] [PubMed]
- Shivers, J.P.; Mackowiak, L.; Anhalt, H.; Zisser, H. “Turn it off!”: Diabetes device alarm fatigue considerations for the present and the future. J. Diabetes Sci. Technol. 2013, 7, 789–794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DiBardino, D.; Cohen, E.R.; Didwania, A. Meta-analysis: Multidisciplinary fall prevention strategies in the acute care inpatient population. J. Hosp. Med. 2012, 7, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Cameron, I.D.; Dyer, S.M.; Panagoda, C.E.; Murray, G.R.; Hill, K.D.; Cumming, R.G.; Kerse, N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst. Rev. 2018, 9, Cd005465. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Bai, X.; Yang, Z.; Shen, Z.; Xuan, D. Mobile phone-based pervasive fall detection. Pers. Ubiquitous Comput. 2010, 14, 633–643. [Google Scholar] [CrossRef]
- Fontecha, J.; Navarro, F.J.; Hervás, R.; Bravo, J. Elderly frailty detection by using accelerometer-enabled smartphones and clinical information records. Pers. Ubiquitous Comput. 2013, 17, 1073–1083. [Google Scholar] [CrossRef]
- Mellone, S.; Tacconi, C.; Schwickert, L.; Klenk, J.; Becker, C.; Chiari, L. Smartphone-based solutions for fall detection and prevention: The FARSEEING approach. Z. Gerontol. Geriatr. 2012, 45, 722–727. [Google Scholar] [CrossRef]
- Bai, Y.-W.; Wu, S.-C.; Tsai, C.-L. Design and Implementation of a Fall Monitor System by Using a 3-Axis Accelerometer in a Smart Phone. IEEE Trans. Consum. Electron. 2012, 58, 1269–1275. [Google Scholar] [CrossRef]
- Castillo, J.C.; Carneiro, D.; Serrano-Cuerda, J.; Novais, P.; Fernández-Caballero, A.; Neves, J. A multi-modal approach for activity classification and fall detection. Int. J. Syst. Sci. 2014, 45, 810–824. [Google Scholar] [CrossRef] [Green Version]
- He, Y. Falling-Incident Detection and Alarm by Smartphone with Multimedia Messaging Service (MMS). E-Health Telecommun. Syst. Netw. 2012, 1, 1–5. [Google Scholar] [CrossRef]
- Hsieh, K.L.; Roach, K.L.; Wajda, D.A.; Sosnoff, J.J. Smartphone technology can measure postural stability and discriminate fall risk in older adults. Gait Posture 2019, 67, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Kwolek, B.; Kepski, M. Improving fall detection by the use of depth sensor and accelerometer. Neurocomputing 2015, 168, 637–645. [Google Scholar] [CrossRef]
- Lee, J.V.; Chuah, Y.D.; Chieng, K.T. Smart Elderly Home Monitoring System with an Android Phone. Int. J. Smart Home 2013, 7, 17–32. [Google Scholar]
- Lee, R.Y.; Carlisle, A.J. Detection of falls using accelerometers and mobile phone technology. Age Ageing 2011, 40, 690–696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopes, I.C.; Vaidya, B.; Rodrigues, J.J.P.C. Towards an autonomous fall detection and alerting system on a mobile and pervasive environment. Telecommun. Syst. 2011, 52, 2299–2310. [Google Scholar] [CrossRef]
- Suh, M.K.; Chen, C.A.; Woodbridge, J.; Tu, M.K.; Kim, J.I.; Nahapetian, A.; Evangelista, L.S.; Sarrafzadeh, M. A remote patient monitoring system for congestive heart failure. J. Med. Syst. 2011, 35, 1165–1179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aguiar, B.; Rocha, T.; Silva, J.; Sousa, I. Accelerometer-Based fall Detection for Smartphones. In Proceedings of the 2014 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Lisboa, Portugal, 11–12 June 2014; pp. 1–6. [Google Scholar]
- Boehner, A. A smartphone application for a portable fall detection system. In Proceedings of the 2013 NCUR, La Crosse, WI, USA, 11–13 April 2013. [Google Scholar]
- Cao, Y.; Yang, Y.; Liu, W. E-FallD: A fall detection system using android-based smartphone. In Proceedings of the 2012 9th International Conference on Fuzzy Systems and Knowledge Discovery, Chongqing, China, 29–31 May 2012; pp. 1509–1513. [Google Scholar]
- Casilari, E.; Oviedo-Jiménez, M.A. Automatic fall detection system based on the combined use of a smartphone and a smartwatch. PLoS ONE 2015, 10, e0140929. [Google Scholar] [CrossRef]
- Casilari, E.; Santoyo-Ramón, J.A.; Cano-García, J.M. Analysis of a smartphone-based architecture with multiple mobility sensors for fall detection. PLoS ONE 2016, 11, e0168069. [Google Scholar] [CrossRef] [Green Version]
- Colon, L.N.V.; DeLaHoz, Y.; Labrador, M. Human fall detection with smartphones. In Proceedings of the 2014 IEEE Latin-America Conference on Communications (LATINCOM), Cartagena, Colombia, 5–7 November 2014; pp. 1–7. [Google Scholar]
- Dogan, J.C.; Hossain, M.S. A novel two-step fall detection method using smartphone sensors. In Proceedings of the 2019 IEEE International Conference on Smart Computing (SMARTCOMP), Washington, DC, USA, 12–15 June 2019; pp. 434–438. [Google Scholar]
- Figueiredo, I.N.; Leal, C.; Pinto, L.; Bolito, J.; Lemos, A. Exploring smartphone sensors for fall detection. mUX: J. Mob. User Exp. 2016, 5, 2. [Google Scholar] [CrossRef] [Green Version]
- Hakim, A.; Huq, M.S.; Shanta, S.; Ibrahim, B. Smartphone based data mining for fall detection: Analysis and design. Procedia Comput. Sci. 2017, 105, 46–51. [Google Scholar] [CrossRef]
- Harari, Y.; Shawen, N.; Mummidisetty, C.K.; Albert, M.V.; Kording, K.P.; Jayaraman, A. A smartphone-based online system for fall detection with alert notifications and contextual information of real-life falls. J. Neuroeng. Rehabil. 2021, 18, 124. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Bai, S.; Wang, X. An unobtrusive fall detection and alerting system based on Kalman filter and Bayes network classifier. Sensors 2017, 17, 1393. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Li, Y.; Bao, S.-D. Fall detection by built-in tri-accelerometer of smartphone. In Proceedings of the 2012 IEEE-EMBS International Conference on Biomedical and Health Informatics, Hong Kong, China, 5–7 January 2012; pp. 184–187. [Google Scholar]
- Islam, Z.Z.; Tazwar, S.M.; Islam, M.Z.; Serikawa, S.; Ahad, M.A.R. Automatic fall detection system of unsupervised elderly people using smartphone. In Proceedings of the 5th IIAE International Conference on Intelligent Systems and Image Processing, Hawaii, HI, USA, 7–12 September 2017. [Google Scholar]
- Koshmak, G.A.; Linden, M.; Loutfi, A. Evaluation of the android-based fall detection system with physiological data monitoring. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July2013; pp. 1164–1168. [Google Scholar]
- Lee, J.-S.; Tseng, H.-H. Development of an enhanced threshold-based fall detection system using smartphones with built-in accelerometers. IEEE Sens. J. 2019, 19, 8293–8302. [Google Scholar] [CrossRef]
- Lee, Y.; Yeh, H.; Kim, K.-H.; Choi, O. A real-time fall detection system based on the acceleration sensor of smartphone. Int. J. Eng. Bus. Manag. 2018, 10, 1847979017750669. [Google Scholar] [CrossRef] [Green Version]
- Madansingh, S.; Thrasher, T.A.; Layne, C.S.; Lee, B.-C. Smartphone based fall detection system. In Proceedings of the 2015 15th International Conference on Control, Automation and Systems (ICCAS), Busan, Korea, 13–16 October 2015; pp. 370–374. [Google Scholar]
- Maglogiannis, I.; Ioannou, C.; Spyroglou, G.; Tsanakas, P. Fall detection using commodity smart watch and smart phone. In Proceedings of the IFIP International Conference on Artificial Intelligence Applications and Innovations, Rhodes, Greece, 19–21 September 2014; pp. 70–78. [Google Scholar]
- Mehner, S.; Klauck, R.; Koenig, H. Location-independent fall detection with smartphone. In Proceedings of the 6th International Conference on PErvasive Technologies Related to Assistive Environments, Rhodes, Greece, 29–31 May 2013; pp. 1–8. [Google Scholar]
- Mousavi, S.A.; Tahami, E.; Azarnoosh, M. Fall detection system via smart phone and send people location. In Proceedings of the 2020 28th European Signal Processing Conference (EUSIPCO), Amsterdam, The Netherlands, 18–21 January 2021; pp. 1605–1607. [Google Scholar]
- Pierleoni, P.; Pernini, L.; Belli, A.; Palma, L.; Valenti, S.; Paniccia, M. SVM-based fall detection method for elderly people using Android low-cost smartphones. In Proceedings of the 2015 IEEE Sensors Applications Symposium (SAS), Zadar, Croatia, 13–15 April 2015; pp. 1–5. [Google Scholar]
- Qu, W.; Lin, F.; Xu, W. A real-time low-complexity fall detection system on the smartphone. In Proceedings of the 2016 IEEE First International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE), Washington, DC, USA, 27–29 June 2016; pp. 354–356. [Google Scholar]
- Shahzad, A.; Kim, K. FallDroid: An automated smart-phone-based fall detection system using multiple kernel learning. IEEE Trans. Ind. Inform. 2018, 15, 35–44. [Google Scholar] [CrossRef]
- Tran, H.A.; Ngo, Q.T.; Tong, V. A new fall detection system on Android smartphone: Application to a SDN-based IoT system. In Proceedings of the 2017 9th International Conference on Knowledge and Systems Engineering (KSE), Hue, Vietnam, 19–21 October 2017; pp. 1–6. [Google Scholar]
- Tran, T.D.; Truong, H.; Dang, T.K. Automatic fall detection using smartphone acceleration sensor. Int. J. Adv. Comput. Sci. Appl. 2016, 7, 123–129. [Google Scholar]
- Tsinganos, P.; Skodras, A. A smartphone-based fall detection system for the elderly. In Proceedings of the 10th International Symposium on Image and Signal Processing and Analysis, Ljubljana, Slovenia, 18–20 September 2017; pp. 53–58. [Google Scholar]
- Viet, V.; Choi, D.-J. Fall detection with smart phone sensor. In Proceedings of the 3rd International Conference on Internet (ICONI), Sepang, Malaysia, 15–19 December 2011. [Google Scholar]
- Viet, V.Q.; Lee, G.; Choi, D. Fall detection based on movement and smart phone technology. In Proceedings of the IEEE RIVF International Conference on Computing and Communication Technologies, Research, Innovation, and Vision for the Future (RIVF), Ho Chi Minh City, Vietnam, 27 February–1 March 2012. [Google Scholar]
- Vilarinho, T.; Farshchian, B.; Bajer, D.G.; Dahl, O.H.; Egge, I.; Hegdal, S.S.; Lønes, A.; Slettevold, J.N.; Weggersen, S.M. A combined smartphone and smartwatch fall detection system. In Proceedings of the 2015 IEEE International Conference on Computer and Information Technology; Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing; Pervasive Intelligence and Computing, Liverpool, UK, 26–28 October 2015; pp. 1443–1448. [Google Scholar]
- Yavuz, G.; Kocak, M.; Ergun, G.; Alemdar, H.O.; Yalcin, H.; Incel, O.D.; Ersoy, C. A smartphone based fall detector with online location support. In Proceedings of the International Workshop on Sensing for App Phones, Association for Computing Machinery (ACM), Zurich, Switzerland, 3–5 November 2010; pp. 31–35. [Google Scholar]
- Yi, W.-J.; Saniie, J. Design flow of a wearable system for body posture assessment and fall detection with android smartphone. In Proceedings of the 2014 IEEE International Technology Management Conference, Chicago, IL, USA, 12–15 June 2014; pp. 1–4. [Google Scholar]
- Yildirim, K.; Gokhan, U.; Keskin, T.; Kavak, A. Fall detection using smartphone-based application. Int. J. Appl. Math. Electron. Comput. 2016, 4. [Google Scholar] [CrossRef]
- Hernandez, R. Demography of ageing. Bold 1992, 2, 8–12. [Google Scholar]
- Fried, T.R.; van Doorn, C.; O’Leary, J.R.; Tinetti, M.E.; Drickamer, M.A. Older person’s preferences for home vs hospital care in the treatment of acute illness. Arch. Intern Med. 2000, 160, 1501–1506. [Google Scholar] [CrossRef]
- Paulson, M.R.; Torres-Guzman, R.A.; Avila, F.R.; Maita, K.; Garcia, J.P.; Eldaly, A.; Palmieri-Serrano, L.; Forte, A.J.; Thompson, J.C.; Maniaci, M.J. 85-Year-Old Postsurgical Complex Patient Successfully Managed Remotely at the Novel Mayo Clinic’s Hospital at Home. Case Rep. Vasc. Med. 2022, 2022, 1439435. [Google Scholar] [CrossRef]
- Maniaci, M.J.; Torres-Guzman, R.A.; Garcia, J.P.; Avila, F.R.; Maita, K.C.; Forte, A.J.; Paulson, M.R. Overall patient experience with a virtual hybrid hospital at home program. SAGE Open Med. 2022, 10, 20503121221092589. [Google Scholar] [CrossRef] [PubMed]
- Maniaci, M.J.; Maita, K.; Torres-Guzman, R.A.; Avila, F.R.; Garcia, J.P.; Eldaly, A.; Forte, A.J.; Matcha, G.V.; Pagan, R.J.; Paulson, M.R. Provider Evaluation of a Novel Virtual Hybrid Hospital at Home Model. Int. J. Gen. Med. 2022, 15, 1909–1918. [Google Scholar] [CrossRef] [PubMed]
- Chadha, R.M.; Paulson, M.R.; Avila, F.R.; Torres-Guzman, R.A.; Maita, K.; Garcia, J.P.; Forte, A.J.; Maniaci, M.J. Surgical patient satisfaction with a virtual hybrid care hotel model: A retrospective cohort study. Ann. Med. Surg. 2022, 74, 103251. [Google Scholar] [CrossRef] [PubMed]
- Chadha, R.M.; Paulson, M.R.; Avila, F.R.; Torres-Guzman, R.A.; Maita, K.C.; Garcia, J.P.; Forte, A.J.; Matcha, G.V.; Pagan, R.J.; Maniaci, M.J. A Virtual Hybrid Care Hotel Model Supports the Recovery of Post-procedural Patients with Mild to Severe Systemic Diseases. Am. Surg. 2022. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Ruiz, L.; Jimenez, A.R.; Garcia-Villamil, G.; Seco, F. Detecting Fall Risk and Frailty in Elders with Inertial Motion Sensors: A Survey of Significant Gait Parameters. Sensors 2021, 21, 6918. [Google Scholar] [CrossRef]
- Usmani, S.; Saboor, A.; Haris, M.; Khan, M.A.; Park, H. Latest Research Trends in Fall Detection and Prevention Using Machine Learning: A Systematic Review. Sensors 2021, 21, 5134. [Google Scholar] [CrossRef]
- Shu, F.; Shu, J. An eight-camera fall detection system using human fall pattern recognition via machine learning by a low-cost android box. Sci. Rep. 2021, 11, 2471. [Google Scholar] [CrossRef]
- Tošić, A.; Hrovatin, N.; Vičič, J. Data about fall events and ordinary daily activities from a sensorized smart floor. Data Brief. 2021, 37, 107253. [Google Scholar] [CrossRef]
- Wang, Z.; Ramamoorthy, V.; Gal, U.; Guez, A. Possible Life Saver: A Review on Human Fall Detection Technology. Robotics 2020, 9, 55. [Google Scholar] [CrossRef]
- Klasnja, P.; Pratt, W. Healthcare in the pocket: Mapping the space of mobile-phone health interventions. J. Biomed. Inform. 2012, 45, 184–198. [Google Scholar] [CrossRef] [Green Version]
- Kulkarni, P.; Ozturk, Y. MPHASiS: Mobile patient healthcare and sensor information system. J. Netw. Comput. Appl. 2011, 34, 402–417. [Google Scholar] [CrossRef]
- Bielli, E.; Carminati, F.; La Capra, S.; Lina, M.; Brunelli, C.; Tamburini, M. A Wireless Health Outcomes Monitoring System (WHOMS): Development and field testing with cancer patients using mobile phones. BMC Med. Inform. Decis. Mak. 2004, 4, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monica Anderson, A.P. Technology Use Among Seniors 2017. Available online: https://www.pewresearch.org/internet/2017/05/17/technology-use-among-seniors/ (accessed on 15 December 2022).
- Sun, R.; Sosnoff, J.J. Novel sensing technology in fall risk assessment in older adults: A systematic review. BMC Geriatr. 2018, 18, 14. [Google Scholar] [CrossRef]
- Roeing, K.L.; Hsieh, K.L.; Sosnoff, J.J. A systematic review of balance and fall risk assessments with mobile phone technology. Arch. Gerontol. Geriatr. 2017, 73, 222–226. [Google Scholar] [CrossRef] [PubMed]





| Reference and Year | Smartphone Operative System | Device | Detection (D)/Prevention (P) | Consequence Triggered by the Fall | Parameter | Performance |
|---|---|---|---|---|---|---|
| Dai J. et al. [25] 2010 | Android OS | G1 | D and P | Speaker sound alert and alarm to guardian | Triaxis accelerometer, gyroscope, and magnetometer | Average false negative: 2.13% Average false positive value is 7.7% |
| Fontecha J. et al. [26] 2013 | Android OS | Not stated | P | Not stated | Triaxis accelerometer | Not stated |
| Mellone S. et al. [27] 2012 | Android OS | Samsung Galaxy SII (GT-I9100) | D and P | Alarm to guardian with GPS location | Accelerometer, gyroscope, and magnetometer | Not stated |
| Bai, Y-W et al. [28] 2012 | Not stated | Not stated | D | Alarm to guardian with GPS location and draw help path | Triaxis accelerometer | Not stated |
| Castillo J.C. et al. [29] 2014 | Android OS | SP (not stated) + external device | D | Alarm to guardian with GPS location | Triaxis accelerometer | Sensitivity: 92.7% Accuracy: 97.2% F-score: 94.8% |
| He, Y. et al. [30] 2012 | Android OS | Lenovo Le-phone | D | Alarm to guardian with GPS location | Triaxis accelerometer | Not stated |
| Hsieh, K.L. et al. [31] 2019 | Not stated | Not stated | D | Not stated | Accelerometer | Not stated |
| Kwolek, B. et al. [32] 2015 | Android OS | SP (not stated) + external device | D | Not stated | Accelerometer | k-nn + acceleration % Sensitivity: 100% Specificity: 92.86% Accuracy: 95.83% Precision: 90.91% SVM + acceleration % Sensitivity: 100% Specificity: 92.86% Accuracy: 91.67% Precision: 83.33% |
| Lee, J.V. et al. [33] 2013 | Android OS | HTC Desire A8181 | D | Alarm to guardian | Triaxis accelerometer | Not stated |
| Lee, R.Y.et al [34] 2011 | Android OS | Google G1 | D | Speaker sound alert and alarm to guardian with GPS location | Triaxis accelerometer | SP: Sensitivity: 81% Specificity: 77% External accelerometer: Sensitivity: 82% Specificity: 96% |
| Lopes, I.C. et al. [35] 2011 | Not stated | Not stated | D | Speaker sound alert and alarm to guardian with GPS location | Triaxis accelerometer | Not stated |
| Suh M.K. et al. [36] 2011 | iOS and Android | iPhone and Motorola Droid | D | Alarm to guardian | Triaxis accelerometer | Not stated |
| Aguiar, B. et al. [37] 2014 | Android OS | Samsung Galaxy Nexus | D | Alarm to guardian with GPS location | Triaxis accelerometer and biaxial gyroscope | Belt usage Sensitivity: 97.0% Specificity: 98.4% Accuracy: 97.6% Pocket usage Sensitivity: 96.6% Specificity: 98.6% Accuracy: 97.5% |
| Boehner et al. [38] 2013 | Not stated | EZ430 Chronos Texas Instruments Smartwatch | D | Alarm to guardian and EMS | Triaxis accelerometer | Not stated |
| Cao et al. [39] 2012 | Android v.2.2 OS | HTC A3366 | D | Alarm to guardian | Accelerometer | Classical algorithm: Sensitivity: 86.7% Specificity: 85.5% Adaptive algorithm: Sensitivity: 86.7% Specificity: 85.5% |
| Casilari, E. et al. [40] 2016 | Android OS | SP and external sensors | D | Alarm to guardian | 3-axis gyroscope, 3-axis accelerometer, and magnometer | Not stated |
| Casilari, E. et al. [41] 2015 | Android OS | LG Nexus 5 | D | Alarm to guardian | Triaxis accelerometer and gyroscope | Sensitivity: 89.6% Specificity: 95.8% |
| Colon L. et al. [42] 2014 | Android v.4.4.2 OS | Google Nexus 5 | D | Alarm to guardian | Triaxis accelerometer and biaxial gyroscope | Precision: 58.2% Specificity: 79% Accuracy: 81.3% Recall: 89% |
| Dogan, J. C. et al. [43] 2019 | Android OS | LG Nexus 5 | D | Not stated | Triaxis accelerometer | Accuracy: 95.65% |
| Figueiredo, I. et al. [44] 2016 | Android v.4.1.2 OS | Samsung Galaxy Nexus and Samsung Galaxy Nexus S | D | Alarm to guardian | Triaxis accelerometer | Sensitivity: 100% Specificity: 92.65% |
| Hakim, A. et al. [45] 2017 | Android OS | Sony C6002 Xperia Z | D | Not stated | Triaxis accelerometer | Accuracy: >90% |
| Harari, Y. et al. [46] 2021 | Android v.6.0.1 OS | Samsung Galaxy S5 | D | Alarm to guardian | Triaxis accelerometer and gyroscope | Sensitivity: 73% Specificity: >99.9% Accuracy: 97.81% |
| He, J. et al. [47] 2017 | Android OS | Not stated | D | Alarm to guardian with GPS location | Triaxis accelerometer and gyroscope | Sensitivity: 99% Specificity: 95% Accuracy: 95.67% |
| He, Y. et al. [48] 2012 | Android OS | Lenovo Le-phone | D | Alarm to guardian with GPS location | Triaxis accelerometer | Not stated |
| Islam, Z. Z. et al. [49] 2017 | Not stated | Not stated | D | Alarm to guardian | Triaxis accelerometer | Accuracy: >90% |
| Koshmak et al. [50] 2013 | Android OS | Not stated | D | Alarm to guardian with GPS location | Triaxis accelerometer | Senitivity: 90% Specificity: 100% Accuracy: 94% |
| Lee, J. S. et al. [51] 2019 | Android OS | Not stated | D | Alarm to guardian | Triaxis accelerometer | Accuracy: 99.38% Detection rates: 96% |
| Lee, Y. et al. [52] 2018 | Not stated | Not stated | D | Not stated | Triaxis accelerometer | Not stated |
| Madansingh, S. et al. [53] 2015 | iOS | iPhone 4 | D | Not stated | Accelerometer, gyroscope, and magnetometer | Not stated |
| Maglogiannis et al. [54] 2014 | Android OS | Pebble smartwatch | D | Alarm to guardian | Triaxis accelerometer | Not stated |
| Mehner et al. [55] 2013 | Android OS | Samsung Galaxy S and Sony Xperia ray | D | Alarm to guardian | Triaxis accelerometer | Detection rate: 83.33% Specificity: 100% |
| Mousavi, S. A. et al. [56] 2021 | iOS v.12.0.1 | iPhone 7+ | D | Alarm to guardian with GPS location | Triaxis accelerometer | Accuracy: 96.33% |
| Pierleoni, P. et al. [57] 2015 | Android v.4.4.4 OS | Motorola Moto G | D | Alarm to guardian | Triaxis accelerometer and magnetometer | Sensitivity: 99.3% Specificity: 96% Accuracy: 97.7% |
| Qu, W. et al. [58] 2016 | Android v.4.4.3 OS | LG Nexus 4 | D | Alarm to guardian with GPS location through social media | Triaxis accelerometer | Not sated |
| Shahzad, A. et al. [59] 2018 | Android v.4.4.2 OS | LG G3 | D | Alarm to guardian | Triaxis accelerometer and gyroscope | Sensitivity: 99.52% Specificity: 95.19% Accuracy: 97.81% |
| Tran, H. et al. [60] 2017 | Android v.5.0 OS | Sony Xperia C4 | D | Alarm to guardian with GPS location | Triaxis accelerometer | Sensitivity: 60.46% Specificity: 94.80% Accuracy: 82.50% |
| Tran, T. D. et al. [61] 2016 | Android OS | ASUS Zenfone 2 | D | Not stated | Triaxis accelerometer | Sensitivity: 93% |
| Tsinganos, P. et al. [62] 2017 | Android OS | LG D160 and ASUS Zenfone 2 | D | Not stated | Triaxis accelerometer | Sensitivity: 97.53% Specificity: 94.89% |
| Viet V. et al. [63] 2011 | Android OS | Google Nexus One | D | Not implemented | Accelerometer | Accuracy per category studied: C1: 75% C2: 87.5% C3: 77.9% C4: 84.2% |
| Viet V. Q. et al. [64] 2012 | Android OS | Google Nexus One | D | Not implemented | Accelerometer and orientation sensor. | Sensitivity: 80% Specificity: 96.2% Accuracy: 85% |
| Vilarinho, T. et al. [65] 2015 | Android OS | Samsung Galaxy S3 and Wear Smartwatch LG G Watch R | D | Alarm to guardian | 9-axis motion sensor combining a 3-axis gyroscope, 3-axis accelerometer, and 3-axis compass | Sensitivity: 63% Specificity: 78% Accuracy: 68% |
| Yavuz et al. [66] 2010 | Android v2.0 OS | Google Nexus One | D | Alarm to guardian with GPS location | Accelerometer | Meyer wavelet can distinguish falls from nonfalls with an 85% recall while retaining 95% precision |
| Yi, W. J.et al. [67] 2014 | Android OS | Not stated | D | Alarm to guardian | External triaxial accelerometer | Not stated |
| Yildirim, K. et al. [68] 2016 | Android v.2.2 OS | Samsung Galaxy SIII mini | D | Alarm to guardian | Triaxis accelerometer | Not stated |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torres-Guzman, R.A.; Paulson, M.R.; Avila, F.R.; Maita, K.; Garcia, J.P.; Forte, A.J.; Maniaci, M.J. Smartphones and Threshold-Based Monitoring Methods Effectively Detect Falls Remotely: A Systematic Review. Sensors 2023, 23, 1323. https://0-doi-org.brum.beds.ac.uk/10.3390/s23031323
Torres-Guzman RA, Paulson MR, Avila FR, Maita K, Garcia JP, Forte AJ, Maniaci MJ. Smartphones and Threshold-Based Monitoring Methods Effectively Detect Falls Remotely: A Systematic Review. Sensors. 2023; 23(3):1323. https://0-doi-org.brum.beds.ac.uk/10.3390/s23031323
Chicago/Turabian StyleTorres-Guzman, Ricardo A., Margaret R. Paulson, Francisco R. Avila, Karla Maita, John P. Garcia, Antonio J. Forte, and Michael J. Maniaci. 2023. "Smartphones and Threshold-Based Monitoring Methods Effectively Detect Falls Remotely: A Systematic Review" Sensors 23, no. 3: 1323. https://0-doi-org.brum.beds.ac.uk/10.3390/s23031323