Trends in Between-Country Health Equity in Sub-Saharan Africa from 1990 to 2011: Improvement, Convergence and Reversal
Abstract
:1. Introduction
2. Materials and Methods
2.1. Metrics Used for Tracking Health Inequity
2.2. Analysis Model
2.3. Data Source
3. Results
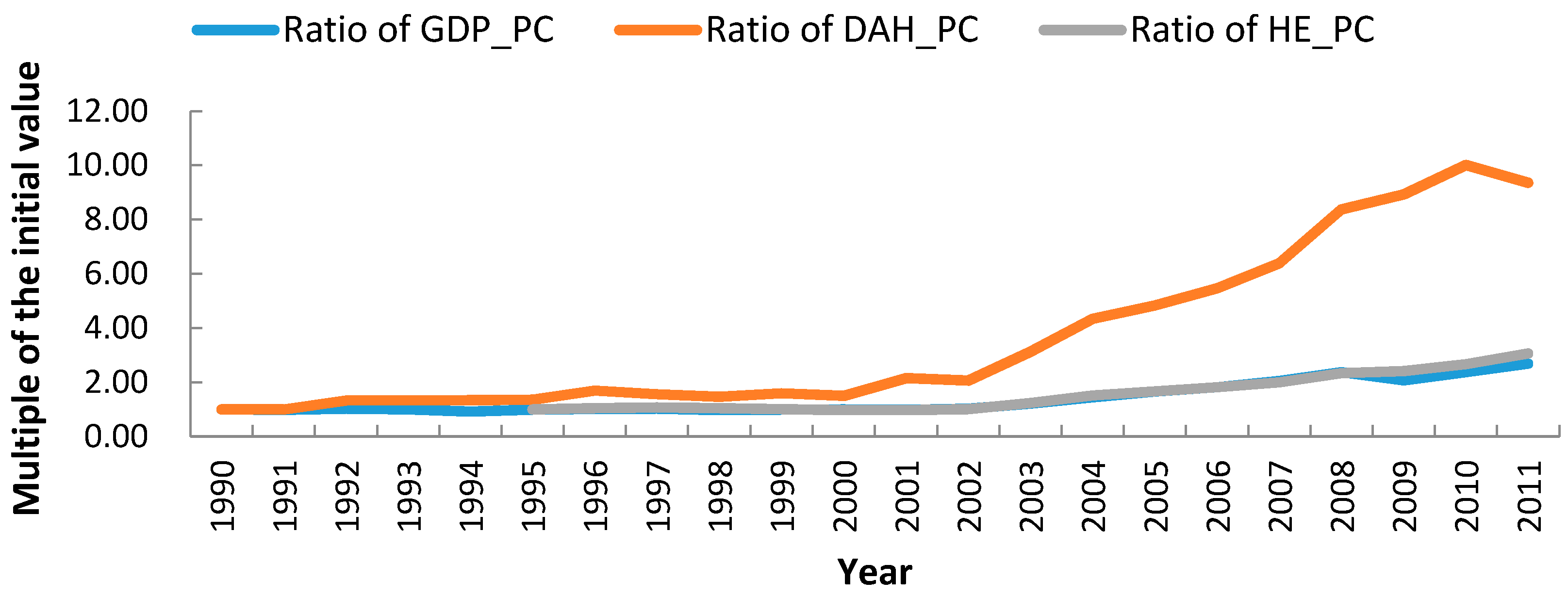
3.1. Overview of Health Expenditure in Africa
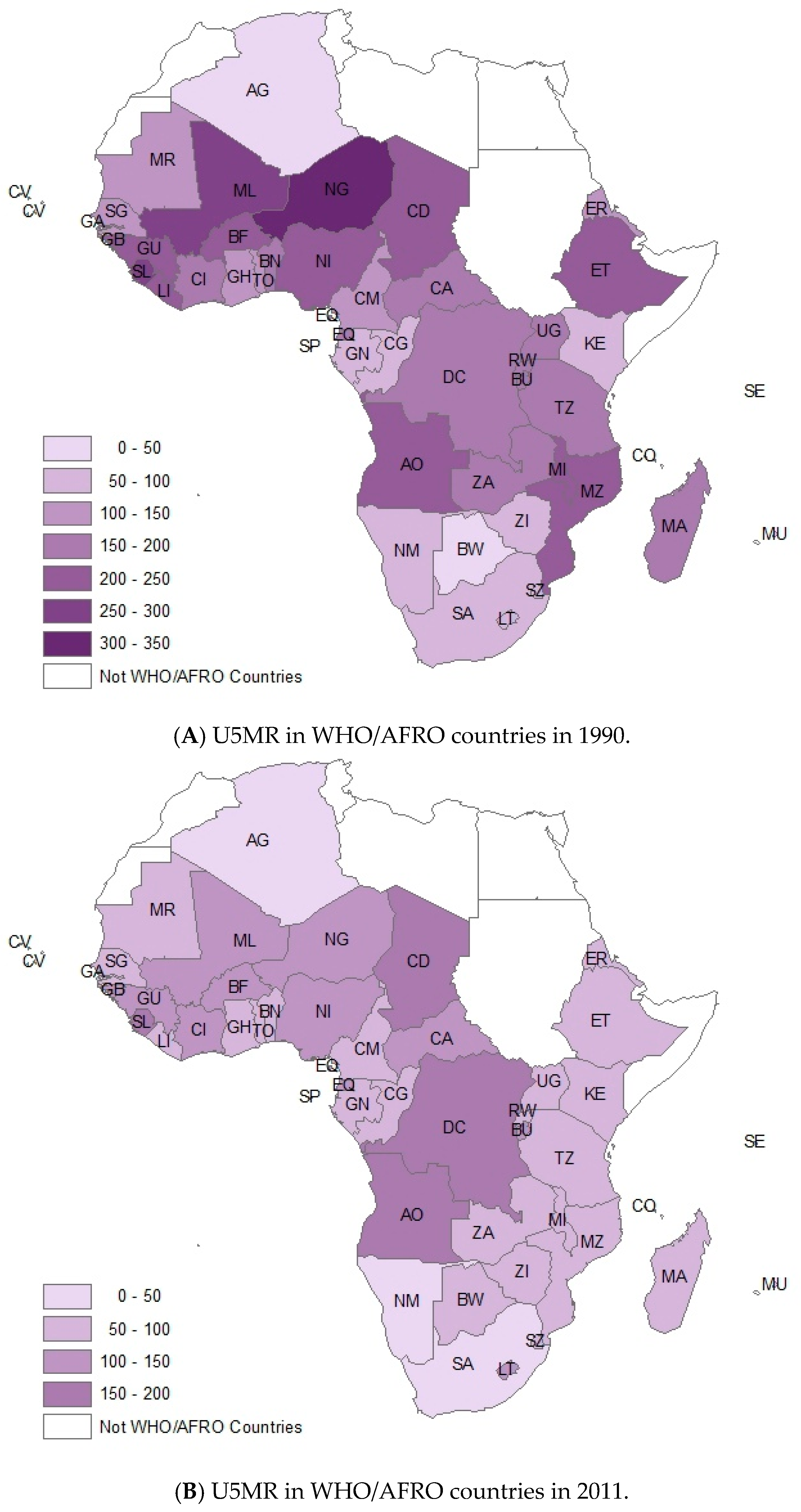
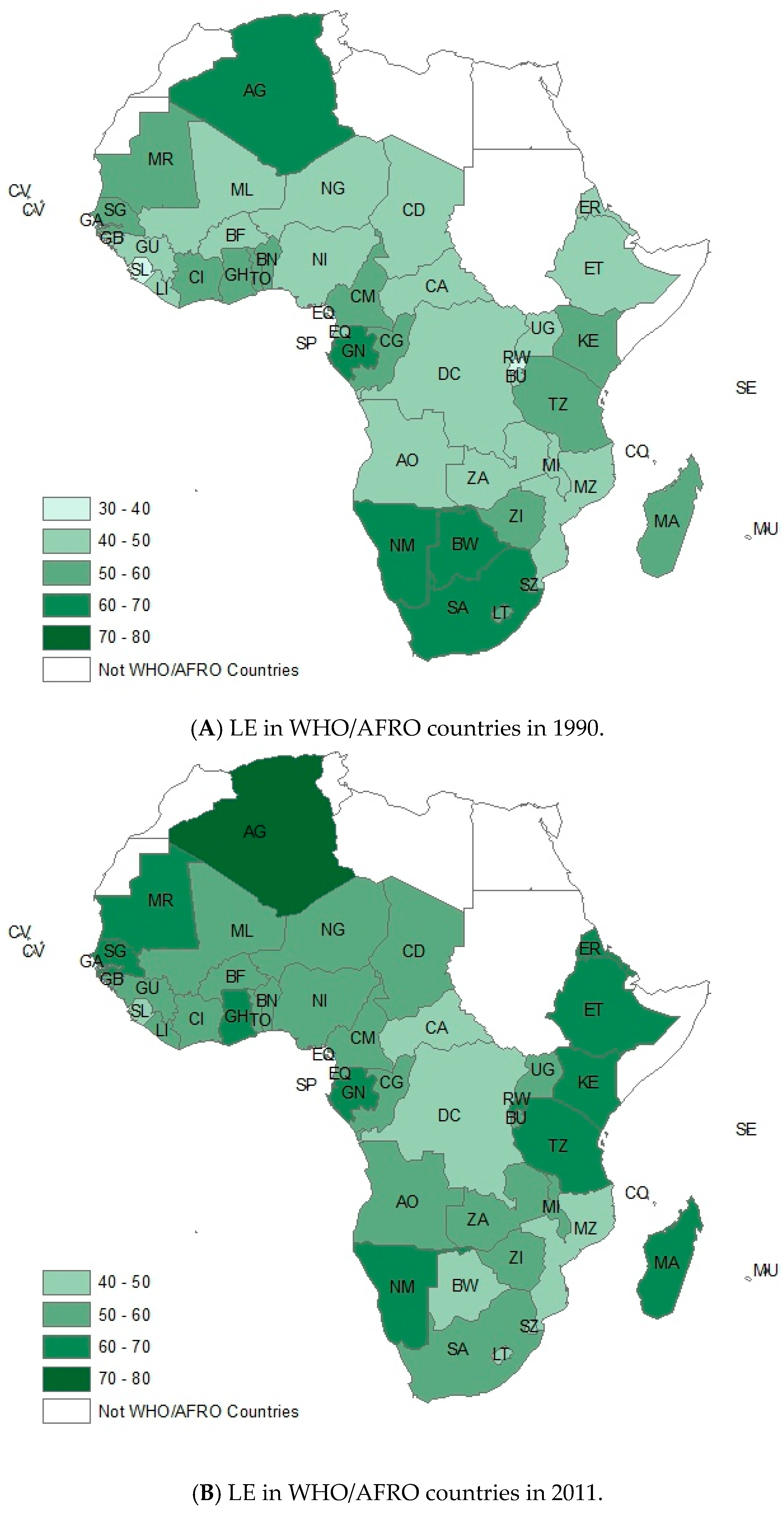
3.2. Variation of Health Outcomes in Africa
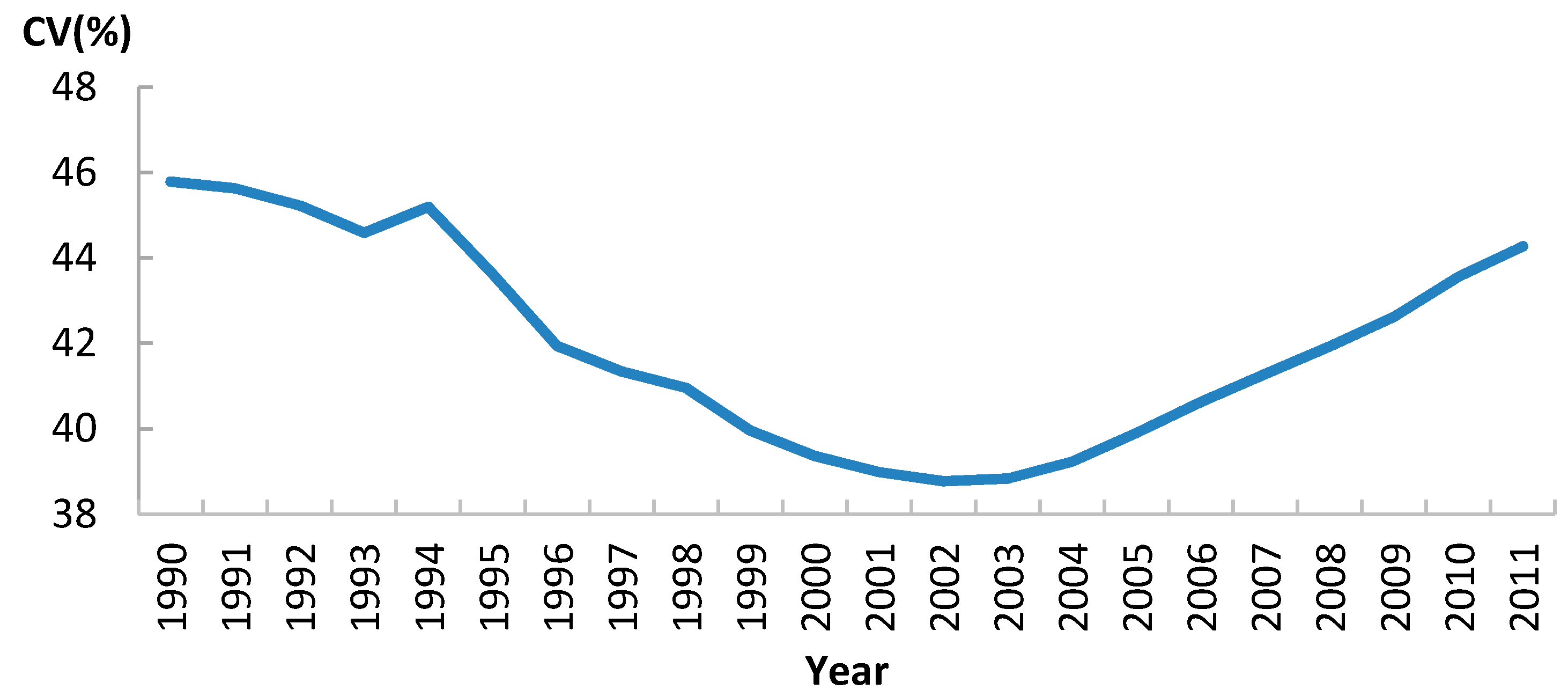
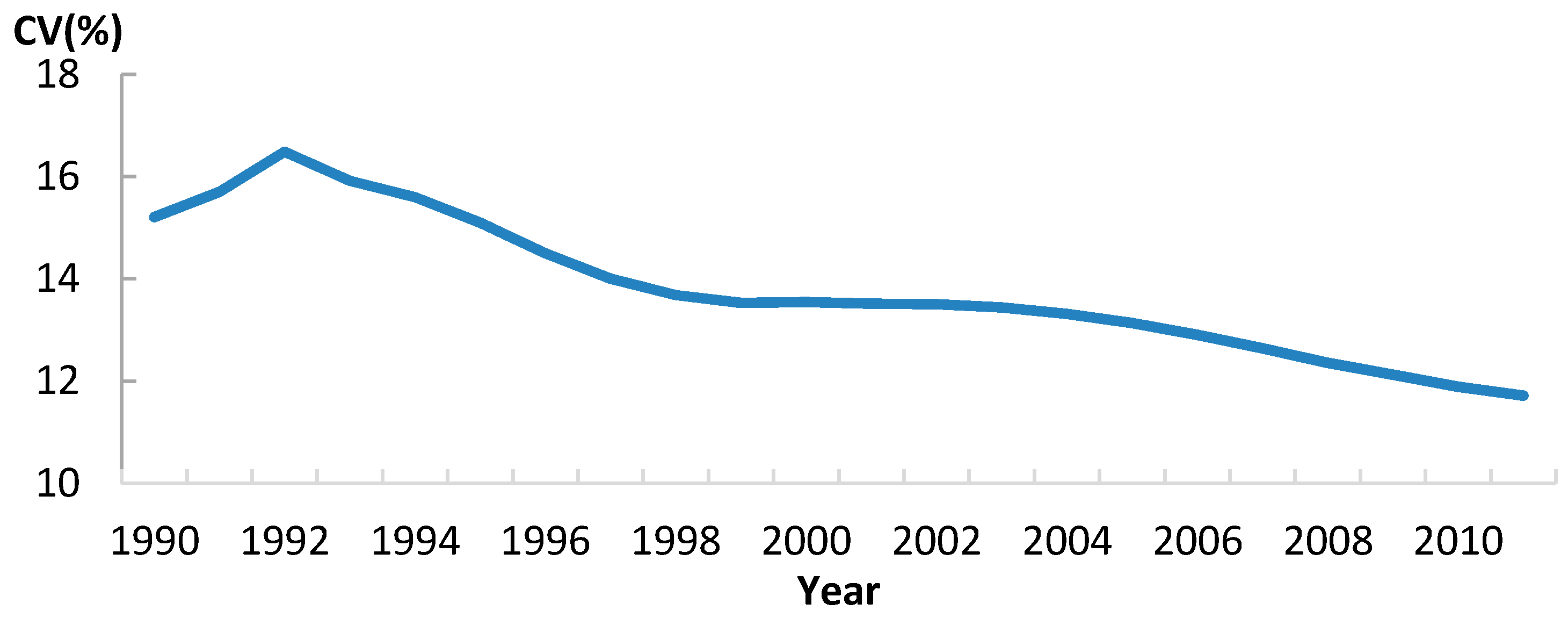
3.3. Convergence Analysis of U5MR
3.4. Convergence Analysis of LE
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| DAH_PC | development assistant for health per capita |
| GDP-PC | Gross domestic product per capita |
| HE-PC | health expenditure per capita |
| HIV-PR | HIV prevalence rate |
| LE | Life expectancy |
| MDG | Millennium Development Goals |
| U5MR | under-5 mortality |
References
- Sambo, L.G.; Kirigia, J.M.; Orem, J.N. Health financing in the African Region: 2000–2009 data analysis. Int. Arch. Med. 2012, 6, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S. Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Braveman, P. Health disparities and health equity: Concepts and measurement. Annu. Rev. Public Health 2006, 27, 167–194. [Google Scholar] [CrossRef] [PubMed]
- Olafsdottir, A.E.; Reidpath, D.D.; Pokhrel, S.; Allotey, P. Health systems performance in Sub-Saharan Africa: Governance, outcome and equity. BMC Public Health 2011, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Boutayeb, A.; Helmert, U. Social inequalities, regional disparities and health inequity in North African countries. Int. J. Equity Health 2011, 10, 410–426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schellenberg, J.A.; Victora, C.G.; Mushi, A.; de Savigny, D.; Schellenberg, D.; Mshinda, H.; Bryce, J. Tanzania Integrated Management of Childhood Illness MCE Baseline Household Survey Study Group. Inequities among the very poor: Health care for children in rural southern Tanzania. Lancet 2003, 361, 561–566. [Google Scholar] [CrossRef]
- Murray, C.J.; Evans, D. Health Systems Performance Assessment; Office of Health Economics: Geneva, Switzerland, 2006. [Google Scholar]
- Abdesslam, B. Evolution of rural-urban health gaps in Morocco: 1992–2011. BMC Res. Notes 2012, 5, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Mtei, G.; Makawia, S.; Ally, M.; Kuwawenaruwa, A.; Meheus, F.; Borghi, J. Who pays and who benefits from health care? An assessment of equity in health care financing and benefit distribution in Tanzania. Health Policy Plann. 2012, 27, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Ewelukwa, O.; Onoka, C.; Onwujekwe, O. Viewing health expenditures, payment and coping mechanisms with an equity lens in Nigeria. BMC Health Serv. Res. 2013, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ataguba, J.E.; McIntyre, D. Paying for and receiving benefits from health services in South Africa: Is the health system equitable? Health Policy Plann. 2012, 27, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Wabiri, N.; Chersich, M.; Zuma, K.; Blaauw, D.; Goudge, J.; Dwane, N. Equity in maternal health in South Africa: Analysis of health service access and health status in a national household survey. PLoS ONE 2013, 8, e73864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odeyemi, I.; Nixon, J. Assessing equity in health care through the national health insurance schemes of Nigeria and Ghana: A review-based comparative analysis. Int. J. Equity Health 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Hofman, K.; Blomstedt, Y.; Addei, S.; Kalage, R.; Maredza, M.; Sankoh, O.; Bangha, M.; Kahn, K.; Becher, H.; Haafkens, J. Addressing research capacity for health equity and the social determinants of health in three African countries: The INTREC programme. Glob. Health Act 2013, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hyder, A.A.; Maman, S.; Nyoni, J.E.; Khasiani, S.A.; Teoh, N.; Premji, Z.; Sohani, S. The pervasive triad of food security, gender inequity and women’s health: Exploratory research from Sub-Saharan Africa. Afr. Health Sci. 2007, 5, 328–334. [Google Scholar]
- Zere, E.; Kirigia, J.M.; Duale, S.; Akazili, J. Inequities in maternal and child health outcomes and interventions in Ghana. BMC Public Health 2012, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Barro, R.J.; Sala-i-Martin, X. Convergence. J. Polit. Econ. 1992, 100, 223–251. [Google Scholar] [CrossRef]
- Sala-i-Martin, X.X. The classical approach to convergence analysis. Econ. J. 1995, 106, 1019–1036. [Google Scholar] [CrossRef]
- Wang, D.H.-M.; Yu, T.H.-K. A cluster analysis and time series approach to examine the healthcare expenditure convergence among Taiwan and the OECD countries. Int. J. Behav. Health Care Res. 2008, 1, 61–69. [Google Scholar] [CrossRef]
- Hitiris, T.; Nixon, J. Convergence of health care expenditure in the EU countries. Appl. Econ. Lett. 2001, 8, 223–228. [Google Scholar] [CrossRef]
- Wang, Z. The convergence of health care expenditure in the U.S. states. Health Econ. 2009, 18, 55–70. [Google Scholar] [CrossRef] [PubMed]
- Clark, R. World health inequality: Convergence, divergence, and development. Soc. Sci. Med. 2011, 72, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Neumayer, E. HIV/AIDS and Its Impact on Convergence in Life Expectancy, Infant and Child Survival Rates; EconWPA: London, UK, 2004. [Google Scholar]
- United Nations. The Millennium Development Goals Report; United Nations: New York, NY, USA, 2015; pp. 32–37. [Google Scholar]
- Bryce, J.; Pinto, C.B.; Shibuya, K.; Black, R.E.; WHO Child Health Epidemiology Reference Group. WHO estimates of the causes of death in children. Lancet 2005, 3, 1147–1152. [Google Scholar] [CrossRef]
- Grépin, K.A. HIV donor funding has both boosted and curbed the delivery of different non-HIV health services in Sub-Saharan Africa. Health Affair. 2012, 31, 1406–1414. [Google Scholar] [CrossRef] [PubMed]
- Ravishankar, N.; Gubbins, P.; Cooley, R.J.; Leach-Kemon, K.; Michaud, C.M.; Jamison, D.T.; Murray, C.J. Financing of global health: Tracking development assistance for health from 1990 to 2007. Lancet 2009, 373, 2113–2124. [Google Scholar] [CrossRef]
- Edwards, R.D. Changes in world inequality in length of life: 1970–2000. Pop. Dev. Rev. 2011, 37, 499–528. [Google Scholar] [CrossRef]
- Ngom, P.; Binka, F.N.; Phillips, J.F.; Pence, B.; Macleod, B. Demographic surveillance and health equity in Sub-Saharan Africa. Health Policy Plann. 2001, 16, 337–344. [Google Scholar] [CrossRef]
- UNAIDS. UNAIDS Report on the Global AIDS Epidemic; UNAIDS: New York, NY, USA, 2008. [Google Scholar]
- Lu, C.; Michaud, C.M.; Khan, K.; Murray, C.J. Absorptive capacity and disbursements by the Global Fund to Fight AIDS, Tuberculosis and Malaria: Analysis of grant implementation. Lancet 2006, 368, 483–488. [Google Scholar] [CrossRef]
- Marum, E.; Taegtmeyer, M.; Parekh, B.; Mugo, N.; Lembariti, S.; Phiri, M.; Moore, J.; Cheng, A.S. “What took you so long?” The impact of PEPFAR on the expansion of HIV testing and counseling services in Africa. J. Acq. Immune Defic. Syndr. 2012, 60, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Vickers, B. Towards a new aid paradigm: South Africa as African development partner. Cam. Rev. Int. Affair. 2012, 25, 535–556. [Google Scholar] [CrossRef]
- Murray, C.J.; Lopez, A.D. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997, 349, 1269–1276. [Google Scholar] [CrossRef]



| Coefficient | Long-Run Single Regression | Panel Estimates | ||||
|---|---|---|---|---|---|---|
| Absolute β-Convergence | Conditional β-Convergence | Conditional β-Convergence | ||||
| Value | 95% CI | Value | 95% CI | Value | 95% CI | |
| 0.138 (0.081) | (−0.025, 0.302) | 0.183 (0.292) | (−0.410, 0.775) | −0.036 (0.046) | (−0.127, 0.055) | |
| −0.050 * (0.004) | (−0.083, −0.017) | −0.035 (0.030) | (−0.096, 0.026) | 0.007 (0.005) | (−0.003, 0.017) | |
| 0.003 (0.008) | (−0.014, 0.019) | −0.005 *** (0.001) | (−0.001, 0.000) | |||
| −0.022 (0.028) | (−0.079, 0.035) | 0.002 (0.006) | (−0.008, −0.003) | |||
| 0.036 (0.022) | (−0.008, 0.080) | 0.001 (0.006) | (−0.009, 0.013) | |||
| −0.016 (0.024) | (−0.033, 0.065) | 0.001 (0.005) | (−0.009, 0.011) | |||
| −0.014 (0.006) | (−0.001, 0.026) | 0.004 ** (0.001) | (0.001, 0.007) | |||
| Annual convergence rate (b, %) | 3.37 | |||||
| R2 | 0.174 | 0.320 | 0.222 | |||
| Coefficient | Long-Run Single Regression | Panel Estimates | ||||
|---|---|---|---|---|---|---|
| Absolute β-Convergence | Conditional β-Convergence | Conditional β-Convergence | ||||
| Value | 95% CI | Value | 95% CI | Value | 95% CI | |
| 0.528 (0.078) | (−0.371, 0.685) | 0.422 ** (0.100) | (0.219, 0.625) | 0.102 *** (0.026) | (0.049, 0.154) | |
| −0.129 ** (0.020) | (−0.169, −0.089) | −0.126 *** (0.027) | (−0.180, 0.071) | −0.033 *** (0.007) | (−0.047, −0.019) | |
| 0.002 (0.002) | (−0.007, 0.003) | 0.001 *** (0.001) | (0.000, 0.002) | |||
| 0.017 * (0.007) | (−0.001, 0.034) | 0.004 (0.002) | (−0.001, 0.008) | |||
| −0.017 * (0.005) | (−0.031, 0.004) | −0.003 (0.002) | (−0.008, 0.002) | |||
| −0.010 (0.007) | (−0.025, 0.004) | −0.002 (0.002) | (−0.006, 0.002) | |||
| −0.004 * (0.002) | (−0.008, 0.000) | −0.003 (0.001) | (−0.004, −0.001) | |||
| Annual convergence rate (b, %) | 6.113 | 6.035 | 3.054 | |||
| R2 | 0.494 | 0.640 | 0.307 | |||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, J.; Liang, D.; Shi, L.; Huang, J. Trends in Between-Country Health Equity in Sub-Saharan Africa from 1990 to 2011: Improvement, Convergence and Reversal. Int. J. Environ. Res. Public Health 2016, 13, 620. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph13060620
Jin J, Liang D, Shi L, Huang J. Trends in Between-Country Health Equity in Sub-Saharan Africa from 1990 to 2011: Improvement, Convergence and Reversal. International Journal of Environmental Research and Public Health. 2016; 13(6):620. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph13060620
Chicago/Turabian StyleJin, Jiajie, Di Liang, Lu Shi, and Jiayan Huang. 2016. "Trends in Between-Country Health Equity in Sub-Saharan Africa from 1990 to 2011: Improvement, Convergence and Reversal" International Journal of Environmental Research and Public Health 13, no. 6: 620. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph13060620






