Estimated Acute Effects of Ozone on Mortality in a Rural District of Beijing, China, 2005–2013: A Time-Stratified Case-Crossover Study
Abstract
:1. Introduction
2. Materials and Methods
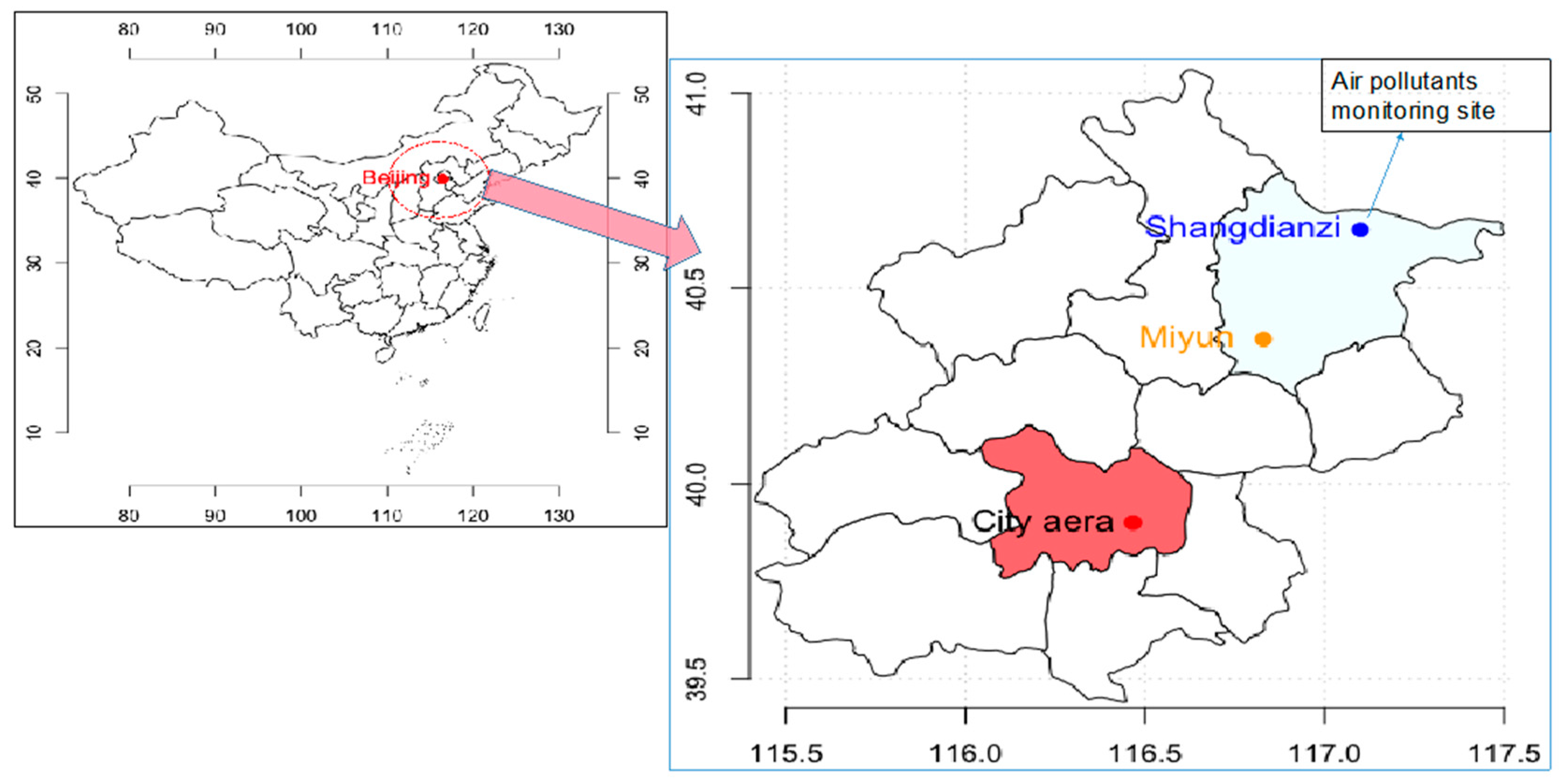
2.1. Study Area
2.2. Data Collection
2.3. Statistical Methods
2.4. Sensitivity Analysis
3. Results
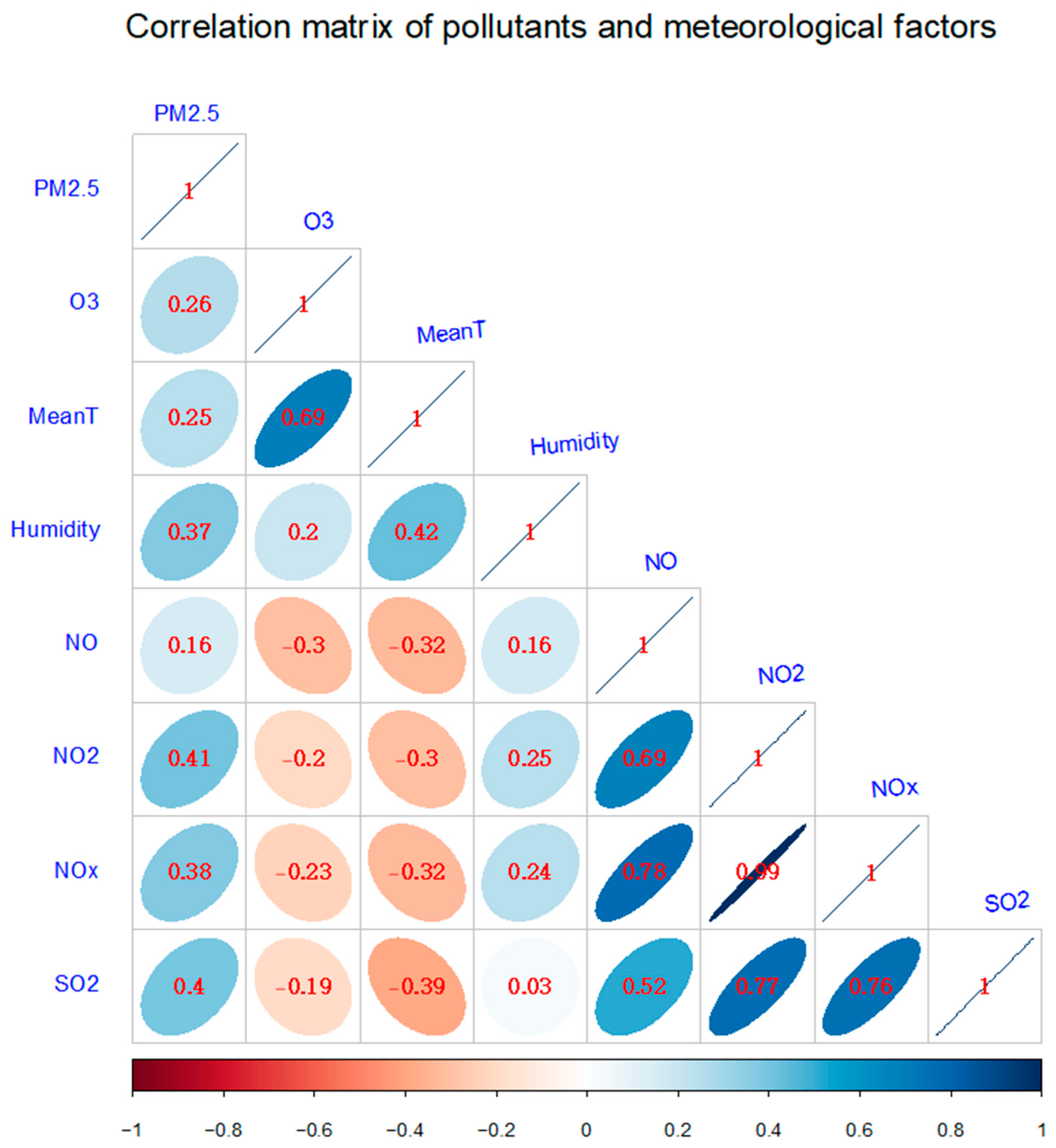
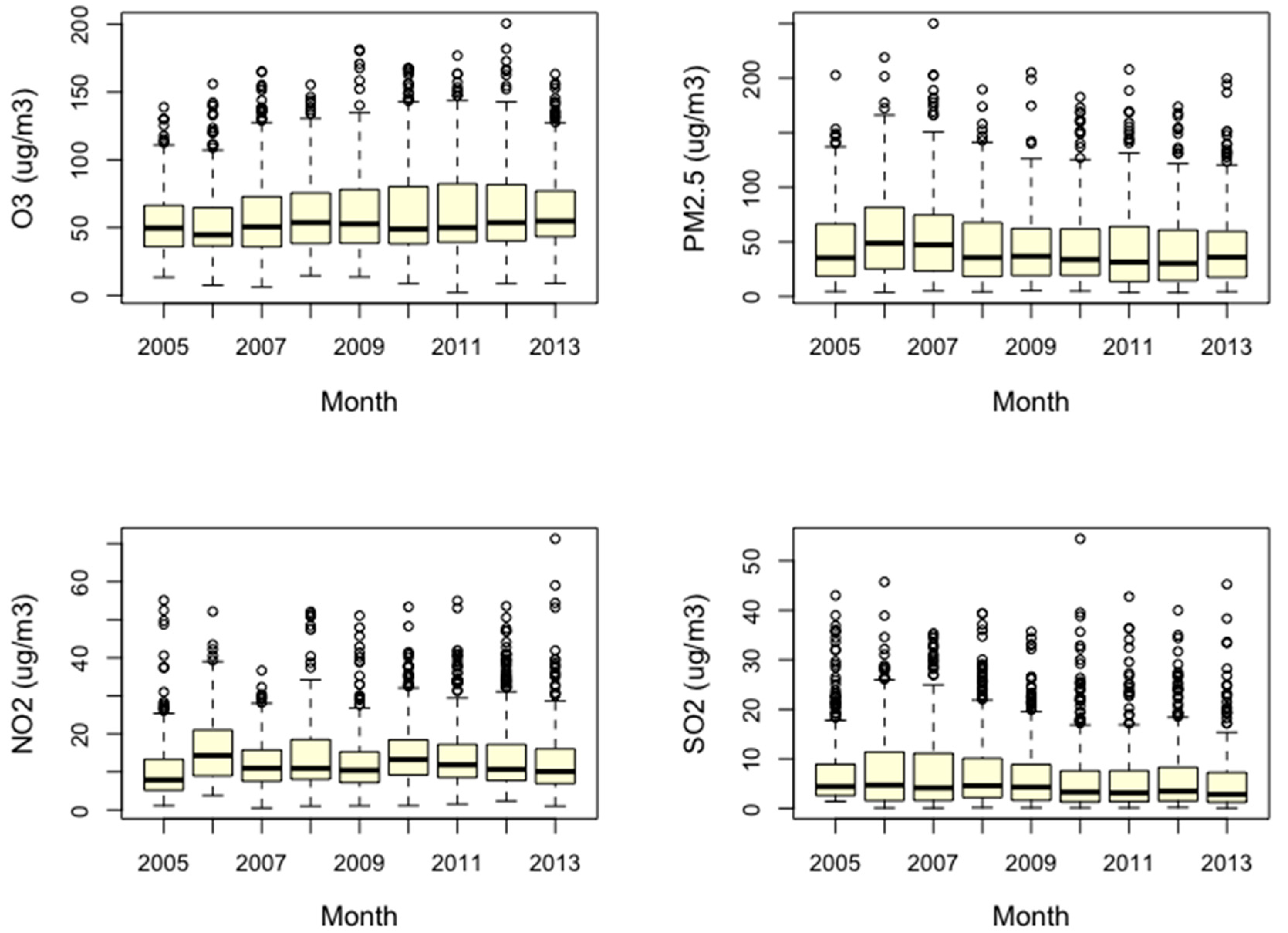
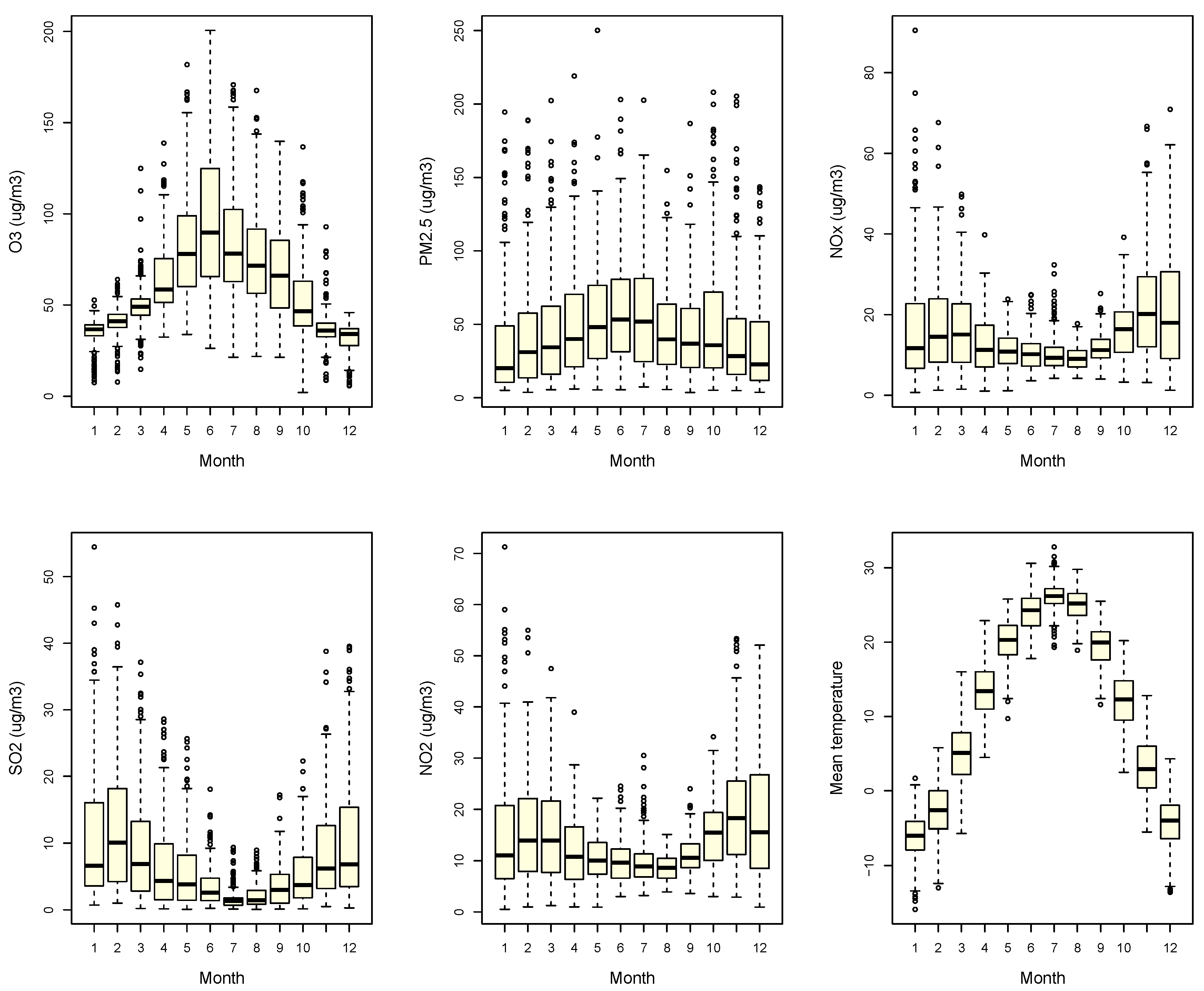
3.1. Seasonal Characteristics of Health Outcomes, Temperature and Air Pollutants
3.2. Time-Stratified Case-Crossover
3.3. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Bell, M.L.; Dominici, F.; Samet, J.M. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology 2005, 16, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Franklin, M.; Zeka, A.; Schwartz, J. Association between PM2.5 and all-cause and specific-cause mortality in 27 US communities. J. Expo. Sci. Environ. 2007, 17, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Environmental Protection of the People’s Republic of China. China Environment Bulletin; Ministry of Environmental Protection of the People’s Republic of China: Beijing, China, 2016.
- Ministry of Environmental Protection of the People’s Republic of China. China Environment Bulletin; Ministry of Environmental Protection of the People’s Republic of China: Beijing, China, 2015.
- Ministry of Environmental Protection of the People’s Republic of China. China Environment Bulletin; Ministry of Environmental Protection of the People’s Republic of China: Beijing, China, 2014.
- Ministry of Environmental Protection of the People’s Republic of China. China Environment Bulletin; Ministry of Environmental Protection of the People’s Republic of China: Beijing, China, 2013.
- Ministry of Environmental Protection of the People’s Republic of China. China Environment Bulletin; Ministry of Environmental Protection of the People’s Republic of China: Beijing, China, 2012.
- Ministry of Environmental Protection of the People’s Republic of China. China Environment Bulletin; Ministry of Environmental Protection of the People’s Republic of China: Beijing, China, 2011.
- Ministry of Environmental Protection of the People’s Republic of China. China Environment Bulletin; Ministry of Environmental Protection of the People’s Republic of China: Beijing, China, 2010.
- Zhao, H.; Wang, S.S.; Wang, W.X.; Liu, R.; Zhou, B. Investigation of Ground-Level Ozone and High-Pollution Episodes in a Megacity of Eastern China. PLoS ONE 2015, 10, e0131878. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.P.; Balluz, L.; Strosnider, H.; Wen, X.J.; Li, C.Y.; Qualters, J.R. Ozone, Fine Particulate Matter, and Chronic Lower Respiratory Disease Mortality in the United States. Am. J. Respir. Crit. Care Med. 2015, 192, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; McDermott, A.; Zeger, S.L.; Samet, J.M.; Dominici, F. Ozone and short-term mortality in 95 US urban communities, 1987–2000. JAMA 2004, 292, 2372–2378. [Google Scholar] [CrossRef] [PubMed]
- Jerrett, M.; Burnett, R.T.; Pope, C.A.; Ito, K.; Thurston, G.; Krewski, D.; Shi, Y.L.; Calle, E.; Thun, M. Long-Term Ozone Exposure and Mortality. N. Engl. J. Med. 2009, 360, 1085–1095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Air Quality Guidelines Global Update 2005: Particulate Matter, O3, Nitrogen Dioxide and Sulfur Dioxide. Available online: http://apps.who.int/iris/handle/10665/107823 (accessed on 2 July 2018).
- Zhang, Y.H.; Huang, W.; London, S.J.; Song, G.X.; Chen, G.H.; Jiang, L.L.; Zhao, N.Q.; Chen, B.H.; Kan, H.D. Ozone and daily mortality in Shanghai, China. Environ. Health Perspect. 2006, 114, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.X.; Yang, H.B.; Guo, S.; Wang, Z.S.; Xu, X.H.; Duan, X.L.; Kan, H.D. Alternative ozone metrics and daily mortality in Suzhou: The China Air Pollution and Health Effects Study (CAPES). Sci. Total Environ. 2012, 426, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.M.; Vichit-Vadakan, N.; Kan, H.D.; Qian, Z.M.; Teams, P.P. Public Health and Air Pollution in Asia (PAPA): A multicity study of short-term effects of air pollution on mortality. Environ. Health Perspect. 2008, 116, 1195–1202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tao, Y.B.; Huang, W.; Huang, X.L.; Zhong, L.J.; Lu, S.E.; Li, Y.; Dai, L.Z.; Zhang, Y.H.; Zhul, T. Estimated Acute Effects of Ambient Ozone and Nitrogen Dioxide on Mortality in the Pearl River Delta of Southern China. Environ. Health Perspect. 2012, 120, 393–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, W.; Xu, X.; Zhang, X.; Tang, J. Contributions of pollutants from north china plain to surface ozone at the shangdianzi GAW station. Atmos. Chem. Phys. 2008, 8, 5889–5898. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, X.; Gong, D.; Quan, W.; Zhao, X.; Ma, Z.; Kim, S. Evolution of surface O3 and PM2.5 concentrations and their relationships with meteorological conditions over the last decade in Beijing. Atmos. Environ. 2015, 108, 67–75. [Google Scholar] [CrossRef]
- R Development Core Team. 2015. Available online: http://www.R-project.org/ (accessed on 2 July 2018).
- Barnett, A.G.; Baker, P.; Dobson, A.J. Analysing Seasonal Data. Available online: https://journal.r-project.org/archive/2012/RJ-2012-001/RJ-2012-001.pdf (accessed on 30 June 2012).
- Barnett, A.G.; Dobson, A.J. Analysing Seasonal Health Data; Springer: Berlin, Germany, 2010. [Google Scholar]
- Bell, M.L.; Kim, J.Y.; Dominici, F. Potential confounding of particulate matter on the short-term association between ozone and mortality in multisite time-series studies. Environ. Health Perspect. 2007, 115, 1591–1595. [Google Scholar] [CrossRef] [PubMed]
- Jhun, I.; Fann, N.; Zanobetti, A.; Hubbell, B. Effect modification of ozone-related mortality risks by temperature in 97 US cities. Environ. Int. 2014, 73, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Katsouyanni, K. APHEA project: Air pollution and health: A European approach. Epidemiology 2006, 17, S19. [Google Scholar] [CrossRef]
- Yan, M.L.; Liu, Z.R.; Liu, X.T.; Duan, H.Y.; Li, T.T. Meta-analysis of the Chinese studies of the association between ambient ozone and mortality. Chemosphere 2013, 93, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Xue, L.K.; Brimblecombe, P.; Lam, Y.F.; Li, L.; Zhang, L. Ozone pollution in China: A review of concentrations, meteorological influences, chemical precursors, and effects. Sci. Total Environ. 2017, 575, 1582–1596. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.K.; Lu, W.Z.; Wang, W.J.; Leung, A.Y.T. A study of ozone variation trend within area of affecting human health in Hong Kong. Chemosphere 2003, 52, 1405–1410. [Google Scholar] [CrossRef]
- Chen, K.; Zhou, L.; Chen, X.D.; Bi, J.; Kinney, P.L. Acute effect of ozone exposure on daily mortality in seven cities of Jiangsu Province, China: No clear evidence for threshold. Environ. Res. 2017, 155, 235–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qian, Z.; He, Q.C.; Lin, H.M.; Kong, L.L.; Liao, D.; Yang, N.N.; Bentley, C.M.; Xu, S.Q. Short-term effects of gaseous pollutants on cause-specific mortality in Wuhan, China. J. Air Waste Manag. 2007, 57, 785–793. [Google Scholar] [CrossRef]
- Qin, L.J.; Gu, J.Q.; Liang, S.J.; Fang, F.; Bai, W.M.; Liu, X.; Zhao, T.; Walline, J.; Zhang, S.L.; Cui, Y.J.; et al. Seasonal association between ambient ozone and mortality in Zhengzhou, China. Int. J. Biometeorol. 2017, 61, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; De Leon, S.F.; Lippmann, M. Associations between ozone and daily mortality—Analysis and meta-analysis. Epidemiology 2005, 16, 446–457. [Google Scholar] [CrossRef] [PubMed]
| Min | 25% | Median | Mean | 75% | Max | |
|---|---|---|---|---|---|---|
| All-cause mortality | 1 | 5 | 6 | 7 | 9 | 21 |
| Cardiovascular mortality | 1 | 2 | 4 | 4 | 5 | 15 |
| Respiratory mortality | 1 | 1 | 1 | 1 | 2 | 7 |
| PM2.5 | 3.63 | 18.61 | 36.89 | 47.70 | 66.48 | 250.13 |
| O3(8 h maximum concentration) | 2.10 | 38.10 | 50.50 | 59.95 | 74.85 | 200.60 |
| Maximum temperature | −9.20 | 7.20 | 20.15 | 18.00 | 28.50 | 40.80 |
| Mean temperature | −15.90 | 0.20 | 12.90 | 11.37 | 22.45 | 32.80 |
| Relative humidity | 8.00 | 43.00 | 60.00 | 58.68 | 74.00 | 98.00 |
| SO2 | 0.07 | 1.62 | 3.90 | 6.72 | 8.91 | 54.45 |
| NO | 0.02 | 0.36 | 0.61 | 1.16 | 1.15 | 19.23 |
| NO2 | 0.51 | 7.54 | 11.10 | 13.48 | 17.17 | 71.28 |
| NOx | 0.70 | 8.04 | 11.75 | 14.64 | 18.41 | 90.51 |
| All-Cause Mortality | Cardiovascular Mortality | ||||
|---|---|---|---|---|---|
| Whole Year | Warm Season | Whole Year | Warm Season | ||
| single O3 | lag0 | 1.020 (1.013,1.029) ** | 1.031(1.005,1.045) ** | 1.017 (1.007,1.029) ** | 1.024 (1.005,1.045) * |
| lag1 | 1.010 (1.002,1.019) ** | 1.028 (1.006,1.046) ** | 1.013 (1.002,1.024) * | 1.025 (1.007,1.045) * | |
| lag2 | 1.009 (1.001,1.018) * | 1.028 (1.001,1.041) ** | 1.011 (1,1.022) * | 1.020 (1.002,1.043) * | |
| lag3 | 1.006 (0.999,1.015) | 1.025 (0.995,1.035) ** | 1.011 (1.001,1.023) * | 1.015 (0.995,1.035) | |
| lag4 | 1.001 (0.993,1.01) | 1.006 (0.979,1.019) | 0.997 (0.986,1.008) | 0.999 (0.979,1.019) | |
| adjusted for PM2.5 | lag0 | 1.025 (1.016,1.034) * | 1.016 (0.999,1.033) * | 1.012 (1,1.025) * | 1.021 (1.003,1.053) * |
| lag1 | 1.018(1.009,1.028) ** | 1.007 (0.989,1.024) | 1.008 (0.996,1.021) | 1.030 (1.003,1.059) * | |
| lag2 | 1.013 (1.004,1.023) ** | 1.013 (0.996,1.03) | 1.010 (0.998,1.023) * | 1.019 (0.992,1.048) | |
| lag3 | 1.009 (1,1.019) * | 1.026 (1.008,1.044) ** | 1.015 (1.003,1.028) * | 1.044 (1.015,1.075) ** | |
| lag4 | 1.000 (0.992,1.01) | 1.007 (0.989,1.024) | 0.995 (0.983,1.008) | 1.001 (0.973,1.03) | |
| adjusted for SO2 | lag0 | 1.017 (1.009,1.026) ** | 1.090 (1.037,1.146) ** | 1.017 (1.006,1.029) ** | 1.078 (1.012,1.15) * |
| lag1 | 1.009 (1.001,1.018) * | 1.033 (0.982,1.087) | 1.010 (0.999,1.022) * | 1.028 (0.965,1.095) | |
| lag2 | 1.008 (1,1.017) * | 1.032 (0.981,1.086) | 1.016 (1.004,1.028) * | 1.076 (1.01,1.148) * | |
| lag3 | 1.003 (0.995,1.012) | 1.043 (0.992,1.099) * | 1.010 (0.999,1.022) * | 1.000 (0.94,1.063) | |
| lag4 | 0.998 (0.99,1.007) | 1.050 (0.998,1.106) | 0.997 (0.986,1.009) | 0.989 (0.926,1.057) | |
| adjusted for NO2 | lag0 | 1.021 (1.013,1.03) ** | 1.01 (0.939,1.087) | 1.014 (1.003,1.026) * | 1.037 (0.965,1.116) |
| lag1 | 1.014 (1.006,1.023) ** | 0.962 (0.895,1.035) | 1.010 (0.999,1.022) * | 0.999 (0.93,1.075) | |
| lag2 | 1.015 (1.007,1.024) ** | 1.01 (0.936,1.091) | 1.012 (1.001,1.024) * | 0.933 (0.865,1.008) | |
| lag3 | 1.007 (0.999,1.016) | 0.991 (0.921,1.066) | 1.006 (0.995,1.018) | 0.955 (0.888,1.028) | |
| lag4 | 1.001 (0.993,1.01) | 1.033 (0.964,1.108) | 0.996 (0.985,1.008) | 0.987 (0.921,1.059) | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Shang, Y.; Zheng, C.; Ma, Z. Estimated Acute Effects of Ozone on Mortality in a Rural District of Beijing, China, 2005–2013: A Time-Stratified Case-Crossover Study. Int. J. Environ. Res. Public Health 2018, 15, 2460. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15112460
Li Y, Shang Y, Zheng C, Ma Z. Estimated Acute Effects of Ozone on Mortality in a Rural District of Beijing, China, 2005–2013: A Time-Stratified Case-Crossover Study. International Journal of Environmental Research and Public Health. 2018; 15(11):2460. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15112460
Chicago/Turabian StyleLi, Yi, Yu Shang, Canjun Zheng, and Zhiqiang Ma. 2018. "Estimated Acute Effects of Ozone on Mortality in a Rural District of Beijing, China, 2005–2013: A Time-Stratified Case-Crossover Study" International Journal of Environmental Research and Public Health 15, no. 11: 2460. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15112460





