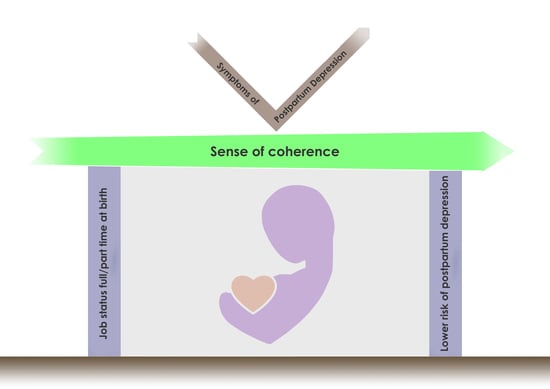
Sense of Coherence Mediates the Links between Job Status Prior to Birth and Postpartum Depression: A Structured Equation Modeling Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Data Analysis
2.5. Ethical Consideration
3. Results
Structural Model
4. Discussion
Limitations
5. Implications
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hahn-Holbrook, J.; Cornwell-Hinrichs, T.; Anaya, I. Economic and health predictors of national postpartum depression prevalence: A systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Front. Psychiatry 2018, 8, 248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira, A.T.; Marques, M.; Soares, M.J.; Maia, B.R.; Bos, S.; Valente, J.; Nogueira, V.; Roque, C.; Madeira, N.; Macedo, A. Profile of depressive symptoms in women in the perinatal and outside the perinatal period: Similar or not? J. Affect. Disord. 2014, 166, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Schmied, V.; Johnson, M.; Naidoo, N.; Austin, M.P.; Matthey, S.; Kemp, L.; Yeo, A. Maternal mental health in Australia and New Zealand: A review of longitudinal studies. Women Birth 2013, 26, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Simhi, M.; Sarid, O.; Cwikel, J. Preferences for mental health treatment for post-partum depression among new mothers. Isr. J. Health Policy Res. 2019, 8, 84. [Google Scholar] [CrossRef] [Green Version]
- Wisner, K.L.; Sit, D.K.; McShea, M.C.; Rizzo, D.M.; Zoretich, R.A.; Hughes, C.L.; Confer, A.L. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013, 70, 490–498. [Google Scholar] [CrossRef]
- Glasser, S. Postpartum depression: A chronicle of health policy development. Isr. J. Psychiatry Relat. Sci. 2010, 47, 254–259. [Google Scholar]
- Bauer, A.; Parsonage, M.; Knapp, M.; Iemmi, V.; Adelaja, B. Costs of Perinatal Mental Health Problems. London School of Economics and Political Science, Care Policy and Evaluation Centre, 2014. Available online: http://eprints.lse.ac.uk/59885/1/__lse.ac.uk_storage_LIBRARY_Secondary_libfile_shared_repository_Content_Bauer%2C%20M_Bauer_Costs_perinatal_%20mental_2014_Bauer_Costs_perinatal_mental_2014_author.pdf (accessed on 1 May 2020).
- Moore Simas, T.A.; Huang, M.Y.; Patton, C.; Reinhart, M.; Chawla, A.J.; Clemson, C.; Eldar-Lissai, A. The humanistic burden of postpartum depression: A systematic literature review. Curr. Med. Res. Opin. 2019, 35, 383–393. [Google Scholar] [CrossRef]
- Putnam, K.T.; Wilcox, M.; Robertson-Blackmore, E.; Sharey, K.; Bergink, V.; Munk-Olsen, T.; Meltzer-Brody, S. Clinical phenotypes of perinatal depression and time of symptom onset: Analysis of data from an international consortium. Lancet Psychiatry 2017, 4, 477–485. [Google Scholar] [CrossRef] [Green Version]
- Vliegen, N.; Casalin, S.; Luyten, P. The course of postpartum depression: A review of longitudinal studies. Harv. Rev. Psychiatry 2014, 22, 1–22. [Google Scholar] [CrossRef]
- Underwood, L.; Waldie, K.; D’Souza, S.; Peterson, E.; Morton, S. A review of longitudinal studies on antenatal and postnatal depression. Arch. Women Ment. Health 2016, 19, 711–720. [Google Scholar] [CrossRef]
- Fazlagić, A. Psychological correlates of postpartum depression. Acta Med. Median 2011, 50, 62–68. [Google Scholar] [CrossRef]
- Chojenta, C.L.; Lucke, J.C.; Forder, P.M.; Loxton, D.J. Maternal Health Factors as Risks for Postnatal Depression: A Prospective Longitudinal Study. PLoS ONE 2016, 11, e0147246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yim, I.S.; Tanner Stapleton, L.R.; Guardino, C.M.; Hahn-Holbrook, J.; Dunkel Schetter, C. Biological and psychosocial predictors of postpartum depression: Systematic review and call for integration. Annu. Rev. Clin. Psychol. 2015, 11, 99–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mccall-Hosenfeld, J.S.; Phiri, K.; Schaefer, E.; Zhu, J.; Kjerulff, K. Trajectories of depressive symptoms throughout the peri- and postpartum period: Results from the first baby study. J. Women Health 2016, 25, 1112–1121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shrivastava, S.R.; Shrivastava, P.S.; Ramasamy, J. Antenatal and postnatal depression: A public health perspective. J. Neurosci. Rural Pract. 2015, 6, 116–119. [Google Scholar] [CrossRef] [Green Version]
- Tebeka, S.; Strat, Y.L.; Dubertret, C. Developmental trajectories of pregnant and postpartum depression in an epidemiologic survey. J. Affect. Disord. 2016, 203, 62–68. [Google Scholar] [CrossRef]
- Glasser, S.; Barell, V.; Boyko, V.; Ziv, A.; Lusky, A.; Shoham, A.; Hart, S. Postpartum depression in an Israeli cohort: Demographic, psychosocial & medical risk factors. J. Psychosom. Obst. Gyn. 2000, 21, 99–108. [Google Scholar] [CrossRef]
- Zhang, Y.; Jin, S. The impact of social support on postpartum depression: The mediator role of self-efficacy. J. Health Psychol. 2016, 21, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Brett, K.; Barfield, W.; Williams, C. Prevalence of self-reported postpartum depressive symptoms 17states, 2004–2005. Centers for Disease Control and Prevention. MMWR 2008, 57, 361. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5714a1.htm (accessed on 8 July 2020).
- De Baca, T.C.; Wojcicki, J.M.; Epel, E.S.; Adler, N.E. Lack of partner impacts newborn health through maternal depression: A pilot study of low-income immigrant Latina women. Midwifery 2018, 64, 63–68. [Google Scholar] [CrossRef]
- Hymas, R.; Girard, L.C. Predicting postpartum depression among adolescent mothers: A systematic review of risk. J. Affect. Disorders 2019, 246, 873–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dørheim, S.K.; Bondevik, G.T.; Eberhard-Gran, M.; Bjorvatn, B. Sleep and depression in postpartum women: A population-based study. Sleep 2009, 32, 847–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakano, M.; Sourander, A.; Luntamo, T.; Chudal, R.; Skokauskas, N.; Kaneko, H. Early risk factors for postpartum depression: A longitudinal Japanese population-based study. J. Affect. Disord. 2020, 269, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Kerstis, B.; Nohlert, E.; Öhrvik, J.; Widarsson, M. Association between depressive symptoms and parental stress among mothers and fathers in early parenthood: A Swedish cohort study. Upsala J. Med. Sci. 2016, 121, 60–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, F.; Lee, W.; Liu, Y.; Yang, J.; Chen, S.; Cheng, K.; Lin, Y.; Ho, T.; Chiu, F.; Hsu, R.; et al. The relationship between economic conditions and postpartum depression in Taiwan: A nationwide population-based study. J. Affect. Disord. 2016, 204, 174–179. [Google Scholar] [CrossRef]
- Goyal, D.; Gay, C.; Lee, K.A. How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first-time mothers? Women Health Issues 2010, 20, 96–104. [Google Scholar] [CrossRef] [Green Version]
- Fall, A.; Goulet, L.; Vézina, M. Comparative study of major depressive symptoms among pregnant women by employment status. Springerplus 2013, 2, 201–212. [Google Scholar] [CrossRef] [Green Version]
- Katon, W.; Russo, J.; Gavin, A. Predictors of postpartum depression. J. Women Health 2014, 23, 753–759. [Google Scholar] [CrossRef]
- Glasser, S.; Stoski, E.; Kneler, V.; Magnezi, R. Postpartum depression among Israeli Bedouin women. Arch. Women Ment. Health 2011, 14, 203–208. [Google Scholar] [CrossRef]
- Gjerdingen, D.; McGovern, P.; Attanasio, L.; Johnson, P.J.; Kozhimannil, K.B. Maternal depressive symptoms, employment, and social support. J. Am. Board Fam. Med. 2014, 27, 87–96. [Google Scholar] [CrossRef]
- Howell, E.A.; Mora, P.A.; DiBonaventura, M.D.; Leventhal, H. Modifiable factors associated with changes in postpartum depressive symptoms. Arch. Women Ment. Health 2009, 12, 113–120. [Google Scholar] [CrossRef]
- Xie, R.H.; He, G.; Koszycki, D.; Walker, M.; Wen, S.W. Prenatal social support, postnatal social support, and postpartum depression. Ann. Epidemiol. 2009, 19, 637–643. [Google Scholar] [CrossRef]
- O’Neill, P.; Cycon, A.; Friedman, L. Seeking social support and postpartum depression: A pilot retrospective study of perceived changes. Midwifery 2019, 71, 56–62. [Google Scholar] [CrossRef]
- Bielinski-Blattmann, D.; Lemola, S.; Jaussi, C.; Stadlmayr, W.; Grob, A. Postpartum depressive symptoms in the first 17 months after childbirth: The impact of an emotionally supportive partnership. Int. J. Public Health 2009, 54, 333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antonovsky, A. Health, Stress and Coping: New Perspectives on Mental and Physical Well-Being; Jossey-Bass: San Francisco, CA, USA, 1979; pp. 1–255. [Google Scholar]
- Antonovsky, A. The Health Psychology Reader; Marks, D.F., Ed.; Sage: London, UK, 2002; Chapter 9; pp. 127–139. [Google Scholar]
- Eriksson, M.; Lindström, B. Antonovsky’s sense of coherence scale and the relation with health: A systematic review. J. Epidemiol. Commun. Health 2006, 60, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Sinikallio, S.; Pakarinen, M.; Tuomainen, I.; Airaksinen, O.; Viinamäki, H.; Aalto, T.J. Preoperative sense of coherence associated with the 10-year outcomes of lumbar spinal stenosis surgery. J. Health Psychol. 2019, 24, 989–997. [Google Scholar] [CrossRef]
- Mutikainen, S.; Föhr, T.; Karhunen, L.; Kolehmainen, M.; Kainulainen, H.; Lappalainen, R.; Kujala, U.M. Predictors of increase in physical activity during a 6-month follow-up period among overweight and physically inactive healthy young adults. J. Exerc. Sci Fit. 2015, 13, 63–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oz, Y.; Sarid, O.; Peleg, R.; Sheiner, E. Sense of coherence predicts uncomplicated delivery: A prospective observational study. J. Psychosom. Obst. Gyn. 2009, 30, 29–33. [Google Scholar] [CrossRef]
- Ferguson, S.; Browne, J.; Taylor, J.; Davis, D. Sense of coherence and women׳ s birthing outcomes: A longitudinal survey. Midwifery 2016, 34, 158–165. [Google Scholar] [CrossRef]
- Van Heumen, M.A.; Hollander, M.H.; van Pampus, M.G.; van Dillen, J.; Stramrood, C.A. Psychosocial predictors of postpartum posttraumatic stress disorder in women with a traumatic childbirth experience. Front. Psychiatry 2018, 9, 348. [Google Scholar] [CrossRef] [Green Version]
- Ferguson, S.; Davis, D.; Browne, J.; Taylor, J. Sense of coherence and childbearing choices: A cross sectional survey. Midwifery 2015, 31, 1081–1086. [Google Scholar] [CrossRef]
- Staneva, A.; Morawska, A.; Bogossian, F.; Wittkowski, A. Pregnancy-specific distress: The role of maternal sense of coherence and antenatal mothering orientations. J. Ment. Health 2016, 25, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Kerstis, B.; Engström, G.; Edlund, B.; Aarts, C. Association between mothers’ and fathers’ depressive symptoms, sense of coherence and perception of their child’s temperament in early parenthood in Sweden. Scand. J. Public Health 2013, 41, 233–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noyman-Veksler, G.; Herishanu-Gilutz, S.; Kofman, O.; Holchberg, G.; Shahar, G. Post-natal psychopathology and bonding with the infant among first-time mothers undergoing a caesarian section and vaginal delivery: Sense of coherence and social support as moderators. Psychol. Health 2015, 30, 441–455. [Google Scholar] [CrossRef] [PubMed]
- Antonovsky, A. Psychosocial Factors at Work and Their Relation to Health; Kalimo, R., El-Batawi, M., Cooper, C.L., Eds.; World Health Organization: Geneva, Switzerland, 1987; pp. 153–167.
- Lövheim, H.; Graneheim, U.H.; Jonsén, E.; Strandberg, G.; Lundman, B. Changes in sense of coherence in old age–a 5-year follow-up of the Umeå 85+ study. Scand. J. Caring Sci. 2013, 27, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.; Sarid, O.; Hurvitz, N.; Anson, O. Sense of coherence and mood states: Exploring the causal relationships. J. Appl. Soc. Psychol. 2009, 39, 82–94. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Cox, J.L.; Holden, J. Perinatal Mental Health: A Guide to the Edinburgh Postnatal Depression Scale; RCPsych Publications: London, UK, 2003; pp. 1–126. [Google Scholar]
- Horowitz, J.A.; Goodman, J. A longitudinal study of maternal postpartum depression symptoms. Res. Theor. Nurs. Prac. 2004, 18, 149–163. [Google Scholar] [CrossRef]
- Bina, R.; Harrington, D. The Edinburgh postnatal depression scale: Screening tool for postpartum anxiety as well? Findings from a confirmatory factor analysis of the Hebrew version. Matern Child Health J. 2016, 20, 904–914. [Google Scholar] [CrossRef]
- Glasser, S.; Barell, V. Depression scale for research and identification of postpartum depression. Harefuah 1999, 136, 764–768. [Google Scholar]
- Gibson, J.; McKenzie-McHarg, K.; Shakespeare, J.; Price, J.; Gray, R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatry Scand. 2009, 119, 350–364. [Google Scholar] [CrossRef]
- Antonovsky, A. The structure and properties of the sense of coherence scale. Soc. Sci. Med. 1993, 36, 725–733. [Google Scholar] [CrossRef]
- Eriksson, M.; Lindström, B. Validity of Antonovsky’s sense of coherence scale: A systematic review. J. Epidemiol. Commun. Health 2005, 59, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, J.; Carmel, S. Trait anxiety and the sense of coherence. Psychol. Rep. 1987, 60, 1000. [Google Scholar] [CrossRef] [PubMed]
- Awang, Z.; Afthanorhan, A.; Asri, M.A.M. Parametric and non-parametric approach in structural equation modeling (SEM): The application of bootstrapping. Mod. Appl. Sci. 2015, 9, 58–67. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural equation modeling: Guidelines for determining model fit. Electron. J. Bus. Res. Method. 2008, 6, 53–60. [Google Scholar]
- Jahoda, M. Work, employment, and unemployment: Values, theories, and approaches in social research. Am. Psychol. 1981, 36, 184–191. [Google Scholar] [CrossRef]
- Liukkonen, V.; Virtanen, P.; Vahtera, J.; Suominen, S.; Sillanmäki, L.; Koskenvuo, M. Employment trajectories and changes in sense of coherence. Eur. J. Public Health 2010, 20, 293–298. [Google Scholar] [CrossRef]
- Gilbert-Ouimet, M.; Trudel, X.; Brisson, C.; Milot, A.; Vézina, M. Adverse effects of psychosocial work factors on blood pressure: Systematic review of studies on demand-control-support and effort-reward imbalance models. Scand. J. Work Environ. Health 2014, 40, 109–132. [Google Scholar] [CrossRef] [Green Version]
- Kivimäki, M.; Kawachi, I. Work stress as a risk factor for cardiovascular disease. Curr. Cardiol. Rep. 2015, 17, 74. [Google Scholar] [CrossRef] [Green Version]
- Schaufeli, W.B.; Salanova, M.; González-Romá, V.; Bakker, A.B. The measurement of engagement and burnout: A two sample confirmatory factor analytic approach. J. Happiness Stud. 2002, 3, 71–92. [Google Scholar] [CrossRef]
- Mäkikangas, A.; Hyvönen, K.; Feldt, T. The energy and identification continua of burnout and work engagement: Developmental profiles over eight years. Burnout Res. 2017, 5, 44–54. [Google Scholar] [CrossRef] [Green Version]
- Pratley, P. Associations between quantitative measures of women’s empowerment and access to care and health status for mothers and their children: A systematic review of evidence from the developing world. Soc. Sci. Med. 2016, 169, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Bales, M.; Pambrun, E.; Melchior, M.; Glangeaud-Freudenthal, N.C.; Charles, M.A.; Verdoux, H.; Sutter-Dallay, A.L. Prenatal psychological distress and access to mental health care in the ELFE cohort. Eur. Psychiatry 2015, 30, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Leahy-Warren, P.; Newham, J.; Alderdice, F. Perinatal social support: Panacea or a pitfall. J. Reprod. Infant Psychol. 2018, 36, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Jomeen, J.; Martin, C.R. Confirmation of an occluded anxiety component within the Edinburgh Postnatal Depression Scale (EPDS) during early pregnancy. J. Reprod. Infant Psychol. 2005, 23, 143–154. [Google Scholar] [CrossRef]
- Hobfoll, S.E. Conservation of resources: A new attempt at conceptualizing stress. Am. Psychol. 1989, 44, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Hobfoll, S.E. Social and Psychological Resources and Adaptation. Rev. Gen. Psychol. 2002, 6, 307–324. [Google Scholar] [CrossRef]
- Sarid, O.; Shraga, Y.; Cwikel, J.; Reuveni, H. Ethno-cultural origins, health beliefs and mothers’ behavior regarding infant vaccinations in Israel. Health Promot. Int. 2019, 34, 581–590. [Google Scholar] [CrossRef]
- Malm, D.; Fridlund, B.; Ekblad, H.; Karlström, P.; Hag, E.; Pakpour, A.H. Effects of brief mindfulness-based cognitive behavioural therapy on health-related quality of life and sense of coherence in atrial fibrillation patients. Eur. J. Cardiovasc. Nur. 2018, 17, 589–597. [Google Scholar] [CrossRef]
- Sarid, O.; Berger, R.; Segal-Engelchin, D. The impact of cognitive behavioral interventions on SOC, perceived stress and mood states of nurses. Procedia Soc. Behav. Sci. 2010, 2, 928–932. [Google Scholar] [CrossRef] [Green Version]

| Characteristic | % (n) | Mean (SD) | Range |
|---|---|---|---|
| Age | 29.51 (4.47) | 21–47 | |
| Country of origin | |||
| Israel | 82.5 (94) | ||
| Other | 17.5 (20) | ||
| Language | |||
| Hebrew | 85.1 (97) | ||
| Arabic | 0.9 (1) | ||
| Russian | 13.2 (15) | ||
| Other | 0.9 (1) | ||
| Family status | |||
| Married/cohabiting | 86.8 (99) | ||
| Alone | 13.2 (15) | ||
| Education | |||
| Elementary | 0.9 (1) | ||
| Highschool | 29.8 (33) | ||
| Above high school | 21.9 (25) | ||
| BA | 37.7 (43) | ||
| MA or higher | 10.5 (12) | ||
| Degree of religiosity | |||
| Secular | 39.5 (45) | ||
| Religious | 60.5 (69) | ||
| Work before birth | |||
| No | 20.2 (23) | ||
| Part-time | 24.6 (28) | ||
| Full-time | 55.3 (63) | ||
| Socioeconomic status | |||
| Not good (low) | 27.2 (31) | ||
| Good (high) | 72.8 (83) | ||
| Not stated | 1.8 (2) |
| Group | PPD T1 % (n) | PPD T2 % (n) |
|---|---|---|
| No PPD (EPDS < 10) | 84.2 (96) | 93.9 (107) |
| Mild PPD (EPDS 10–12) | 13.2 (15) | 4.4 (5) |
| Major PPD (EPDS ≥ 13) | 2.6 (3) | 1.8 (2) |
| Group | SOC T1 | SOC T2 | |||
|---|---|---|---|---|---|
| N | M | SD | M | SD | |
| Did not work | 23 | 67.98 | 10.57 | 74.70 | 9.53 |
| Part-time | 28 | 73.52 | 9.42 | 75.41 | 10.36 |
| Full-time | 63 | 73.42 | 9.18 | 76.24 | 9.22 |
| Variable | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Job status before birth | 1 | ||||
| SOC T1 | 0.192 * | 1 | |||
| SOC T2 | 0.049 | 0.486 ** | 1 | ||
| PPD T1 | −0.214 * | −0.471 ** | −0.415 ** | 1 | |
| PPD T2 | 0.062 | −0.282 ** | −0.535 ** | 0.325 ** | 1 |
| Fit Indices | Model Value | Indicative Range 1 |
|---|---|---|
| Likelihood ratio χ2 | X2(5) = 9.356 p = 0.096 | p-value > 0.05 |
| χ2/df | 1.871 | χ2/df < 3 |
| Goodness of Fit (GFI) | 0.971 | GFI ≥ 0.95 |
| Adjusted Goodness of Fit (AGFI) | 0.914 | AGFI ≥ 0.90 |
| Normed Fit Index (NFI) | 0.918 | NFI ≥ 0.95 |
| Tucker–Lewis Index (TLI) | 0.917 | TLI ≥ 0.95 |
| Comparative Fit Index (CFI) | 0.958 | CFI ≥ 0.90 |
| Root Mean Square Error of Approximation (RMSEA) | 0.088 | RMSEA < 0.08 |
| Standardized Root Mean Square Residual (SRMR) | 0.059 | SRMR < 0.08 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goren, G.; Sarid, O.; Philippou, P.; Taylor, A. Sense of Coherence Mediates the Links between Job Status Prior to Birth and Postpartum Depression: A Structured Equation Modeling Approach. Int. J. Environ. Res. Public Health 2020, 17, 6189. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17176189
Goren G, Sarid O, Philippou P, Taylor A. Sense of Coherence Mediates the Links between Job Status Prior to Birth and Postpartum Depression: A Structured Equation Modeling Approach. International Journal of Environmental Research and Public Health. 2020; 17(17):6189. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17176189
Chicago/Turabian StyleGoren, Ganit, Orly Sarid, Philippos Philippou, and Alyx Taylor. 2020. "Sense of Coherence Mediates the Links between Job Status Prior to Birth and Postpartum Depression: A Structured Equation Modeling Approach" International Journal of Environmental Research and Public Health 17, no. 17: 6189. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17176189