Passive Smokers’ Support for Stronger Tobacco Control in Indonesia
Abstract
:1. Introduction
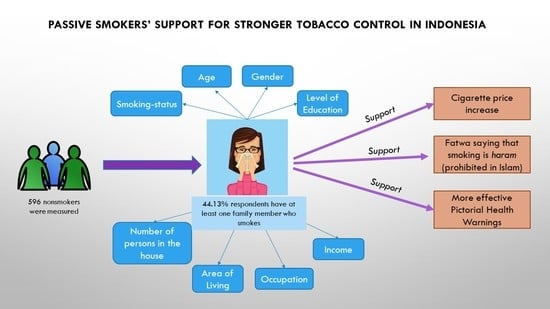
2. Methods
3. Results
3.1. Demographic Characteristics of Passive Smokers
3.2. Attitude towards Smoking Behavior
3.3. Support towards Stronger Tobacco Control
4. Discussion
4.1. Demographic Characteristics of Passive Smokers
4.2. Attitude towards Smoking Behavior
4.3. Support towards Stronger Tobacco Control
5. Conclusions
Declaration
Consent to Participate
Consent for Publication
Availability of Data and Materials
Competing Interests
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Southeast Asia Tobacco Control Alliance. Tobacco Control Atlas ASEAN Region. 4th Ed September 2018. Available online: https://seatca.org/dmdocuments/TobaccoControlAtlas_ASEANRegion_4thEd_Dec2019.pdf (accessed on 20 February 2019).
- Surbakti, P. Indonesia’s National Socio-Economic Survey: A Continual Data Source for Analysis on Welfare Development; Central Bureau of Statistics: Jakarta, Indonesia, 1995. [Google Scholar]
- National Intitute of Health Research and Development (NIHRD). National Report on Basic Health Research (RISKESDAS) 2013. 2013. Available online: https://www.depkes.go.id/resources/download/general/Hasil%20Riskesdas%202013.pdf (accessed on 3 April 2018).
- National Intitute of Health Research and Development (NIHRD). National Report on Basic Health Research (RISKESDAS) 2018. 2018. Available online: http://www.depkes.go.id/resources/download/info-terkini/materi_rakorpop_2018/Hasil%20Riskesdas%202018.pdf (accessed on 19 February 2019).
- DiGiacomo, S.; Jazayeri, M.A.; Barua, R.; Ambrose, J. Environmental tobacco smoke and cardiovascular disease. Int. J. Environ. Res. Public Health 2019, 16, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poirier, A.E.; Ruan, Y.; Grevers, X.; Walter, S.D.; Villeneuve, P.J.; Friedenreich, C.M.; Brenner, D.R.; ComPARe Study Team. Estimates of the current and future burden of cancer attributable to active and passive tobacco smoking in Canada. Prev. Med. 2019, 122, 9–19. [Google Scholar] [CrossRef]
- Ghazali, S.M.; Huey, T.C.; Cheong, K.C.; Li, L.H.; Yusoff, M.F.; Yusoff, A.F.; Hock, L.K. Prevalence and factors associated with secondhand smoke exposure among Malaysian adolescents. Tob. Induc. Dis. 2019, 17, 22. [Google Scholar]
- Center for Social Security Studies Universitas Indonesia. Parental Smoking Behavior and Its Impact on Children Development; Center for Social Security Studies Universitas Indonesia: Jakarta, Indonesia, 2018. [Google Scholar]
- Karmee, N.; Satapathy, S.P.; Tripathy, R.M. Association between socio-demographic characteristics and preventable lifestyle related risk factors of non-communicable diseases among adolescents: A school based study in Berhampur, Odisha. Int. J. Community Med. Public Health 2017, 4, 2905–2911. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Yao, Y.; Yu, Y.; Shi, J.; Liu, Y.; Tao, Y.; Kou, C.; Zhang, H.; Han, W.; Yin, Y.; et al. Prevalence and associated factors of passive smoking among women in Jilin Province, China: A cross-sectional study. Int. J. Environ. Res. Public Health 2015, 12, 13970–13980. [Google Scholar] [CrossRef] [PubMed]
- Jallow, I.K.; Britton, J.; Langley, T. Prevalence and factors associated with exposure to secondhand smoke (SHS) among young people: A cross-sectional study from the Gambia. BMJ Open 2018, 8, e019524. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Factsheet 2018 Indonesia: Heart Disease and Stroke are the Commonest Ways by Which Tobacco Kills People. Available online: https://apps.who.int/iris/bitstream/handle/10665/272673/wntd_2018_indonesia_fs.pdf?sequence=1 (accessed on 22 August 2019).
- Reece, S.; Morgan, C.; Parascandola, M.; Siddiqi, K. Secondhand smoke exposure during pregnancy: A cross-sectional analysis of data from Demographic and Health Survey from 30 low-income and middle-income countries. Tob. Control 2019, 28, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Hajizadeh, M.; Nandi, A. The socioeconomic gradient of secondhand smoke exposure in children: Evidence from 26 low-income and middle-income countries. Tob. Control 2016, 25, e146–e155. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, G.; Gorely, T.; Ozakinci, G.; Polson, R.; Forbat, L. A systematic review and narrative summary of family-based smoking cessation interventions to help adults quit smoking. BMC Fam. Pract. 2016, 17, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, S.S.; Cheung, Y.T.; Fong, D.Y.; Emmons, K.; Leung, A.Y.; Leung, D.Y.; Lam, T.H. Family-based smoking cessation intervention for smoking fathers and nonsmoking mothers with a child: A randomized controlled trial. J. Pediatrics 2017, 182, 260–266. [Google Scholar] [CrossRef] [PubMed]
- U.S. National Cancer Institute and World Health Organization. The Economics of Tobacco and Tobacco Control; Monograph 21 NIH Publication No. 16-CA-8029A; U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute: Bethesda, MD, USA; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Chaloupka, F.J.; Yurekli, A.; Fong, G.T. Tobacco taxes as a tobacco control strategy. Tob. Control 2012, 21, 172–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, L.M.; Schafferer, C.; Lee, J.M.; Yeh, C.Y.; Hsieh, C.J. Raising cigarette excise tax to reduce consumption in low-and middle-income countries of the Asia-Pacific region: A simulation of the anticipated health and taxation revenues impacts. BMC Public Health 2018, 18, 1187. [Google Scholar] [CrossRef] [PubMed]
- Nargis, N.; Manneh, Y.; Krubally, B.; Jobe, B.; Ouma, A.E.; Tcha-Kondor, N.; Blecher, E.H. How effective has tobacco tax increase been in the Gambia? A case study of tobacco control. BMJ Open 2016, 6, e010413. [Google Scholar] [CrossRef] [PubMed]
- Tobacco Control Support Center. Opini Publik: Efektivitas Peringatan Kesehatan Bergambar di Indonesia (Public Opinion: The Effectiveness of Pictorial Health Warnings in Indonesia). 2019. Available online: www.tcsc-indonesia.org/wp-content/uploads/2019/03/TCSC-A4-ISBN-02-1.pdf (accessed on 5 Desember 2019).
- Ratih, S.P.; Susanna, D. Perceived effectiveness of pictorial health warnings on changes in smoking behaviour in Asia: A literature review. BMC Public Health 2018, 18, 1165. [Google Scholar] [CrossRef] [PubMed]
| Classification | Total Population | Percentage | Sample | Final Sample |
|---|---|---|---|---|
| Wireless Network Provider | ||||
| Telkomsel | 139,934,665 | 47.2% | 472 | 473 |
| Indosat | 100,538,309 | 33.9% | 339 | 339 |
| XL | 42,362,769 | 14.3% | 143 | 142 |
| Tri | 12,782,993 | 4.3% | 43 | 42 |
| Smartfren | 588,086 | 0.2% | 2 | 0 |
| Others | 63,447 | 0.0% | 0 | 0 |
| TOTAL | 296,270,269 | 100.0% | 1000 | 1000 |
| Region | ||||
| Western Indonesia | 207,702,000 | 79.3% | 793 | 803 |
| Central Indonesia | 42,126,000 | 16.0% | 160 | 170 |
| Eastern Indonesia | 12,062,900 | 4.7% | 47 | 17 |
| TOTAL | 261,890,900 | 100.000% | 1000 | 1000 |
| Characteristics | Measurement | Passive Smoker | Odds Ratio (95% CI) | p Value | |||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| n | % | n | % | ||||
| Smoking Status | Never-smoke* | 226 | 45.1 | 275 | 54.9 | ||
| Ex-smoker | 37 | 39.0 | 58 | 61.1 | 0.8 (0.5–1.4) | 0.391 | |
| Age | 18–24* | 94 | 54.0 | 80 | 46.0 | ||
| 25–38 | 115 | 39.9 | 172 | 60.1 | 1.8 (1.2–2.7) | 0.008 | |
| ≥39 | 54 | 40.3 | 80 | 59.7 | 2.1 (1.3–3.5) | 0.005 | |
| Gender | Male* | 79 | 32.2 | 166 | 67.8 | ||
| Female | 184 | 52.4 | 167 | 47.6 | 0.4 (0.3–0.6) | 0.000 | |
| Level of Education | Low* | 14 | 58.3 | 10 | 41.7 | ||
| Middle | 137 | 52.7 | 133 | 47.3 | 1.4 (0.5–3.5) | 0.496 | |
| High | 112 | 35.9 | 200 | 64.1 | 2.8 (1.1–7.2) | 0.036 | |
| Income (million rupiah) | <2.9* | 85 | 44.7 | 105 | 55.3 | ||
| 3–6.9 | 122 | 48.0 | 132 | 52.0 | 0.6 (0.4–0.9) | 0.013 | |
| >7 | 56 | 36.8 | 96 | 63.2 | 0.9 (0.5–1.6) | 0.753 | |
| Occupation | Unemployed/student* | 87 | 50.9 | 84 | 49.1 | ||
| Self-employed | 34 | 37.4 | 57 | 62.6 | 1.0 (0.6–1.8) | 0.977 | |
| Employee (Private and Gov’t sectors) | 94 | 39.2 | 146 | 60.8 | 0.9 (0.6–1.5) | 0.721 | |
| Laborer | 48 | 51.1 | 46 | 48.9 | 0.6 (0.3–1.1) | 0.093 | |
| Area of Living | Municipality* | 88 | 45.1 | 107 | 54.9 | ||
| District | 175 | 43.6 | 226 | 56.4 | 1.1 (0.7–1.6) | 0.699 | |
| Number of Persons in the House | <3 persons* | 71 | 37.2 | 120 | 62.8 | ||
| 4–5 persons | 131 | 43.2 | 172 | 56.8 | 0.8 (0.5–1.1) | 0.153 | |
| >5 persons | 61 | 59.8 | 41 | 40.2 | 0.4 (0.2–0.7) | 0.001 | |
| Variables | n | % |
|---|---|---|
| Family members who smoke | ||
| Father | 86 | 32.7 |
| Husband | 75 | 28.5 |
| Older brother | 48 | 18.3 |
| Little brother | 17 | 6.5 |
| Kids | 16 | 6.1 |
| Mother | 13 | 4.9 |
| Other | 8 | 3.0 |
| Agreed that smoking is harmful | 261 | 99.2 |
| Aware of the harms of Cigarettes | 258 | 98.1 |
| Want to encourage family members to stop smoking | 245 | 93.2 |
| Tobacco Control Efforts | n (263) | % |
|---|---|---|
| Increase in cigarette price | ||
| Agreed | 228 | 86.7 |
| Disagreed | 35 | 13.3 |
| Fatwa that prohibits smoking in Islamic view | ||
| Agreed | 172 | 65.8 |
| Disagreed | 90 | 34.2 |
| Pictorial Health Warnings | ||
| Current PHWs are not effective | 133 | 50.6 |
| Current PHWs can convince people to quite smoking | 32 | 12.2 |
| Current PHWs have potential to raise awareness | 98 | 37.3 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nurhasana, R.; Ratih, S.P.; Djaja, K.; Hartono, R.K.; Dartanto, T. Passive Smokers’ Support for Stronger Tobacco Control in Indonesia. Int. J. Environ. Res. Public Health 2020, 17, 1942. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17061942
Nurhasana R, Ratih SP, Djaja K, Hartono RK, Dartanto T. Passive Smokers’ Support for Stronger Tobacco Control in Indonesia. International Journal of Environmental Research and Public Health. 2020; 17(6):1942. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17061942
Chicago/Turabian StyleNurhasana, Renny, Suci Puspita Ratih, Komara Djaja, Risky Kusuma Hartono, and Teguh Dartanto. 2020. "Passive Smokers’ Support for Stronger Tobacco Control in Indonesia" International Journal of Environmental Research and Public Health 17, no. 6: 1942. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17061942