Sitting Posture, Sagittal Spinal Curvatures and Back Pain in 8 to 12-Year-Old Children from the Region of Murcia (Spain): ISQUIOS Programme
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
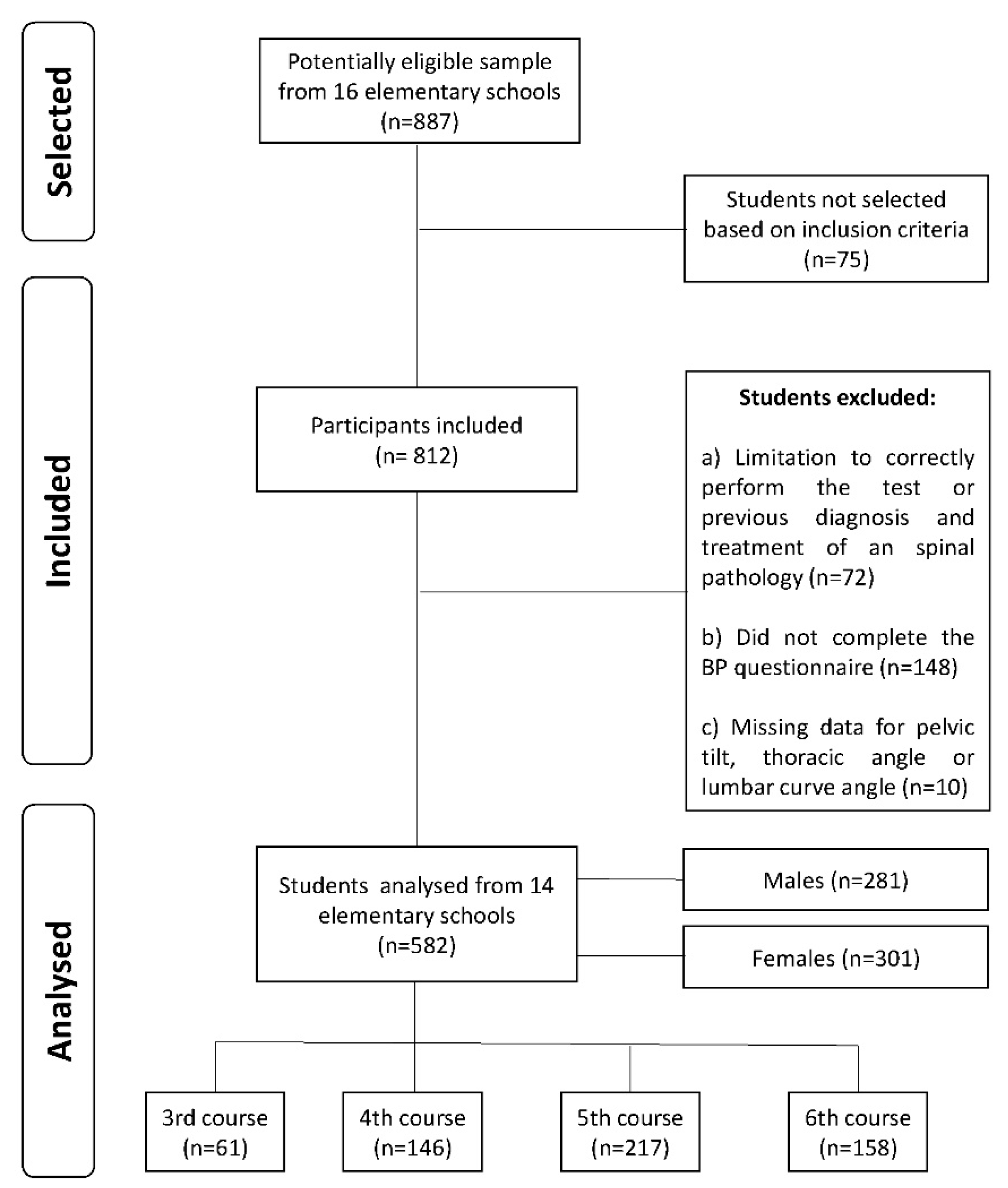
2.2. Participants
2.3. Procedures
2.3.1. Thoracic and Lumbar Sagittal Curves Assessment
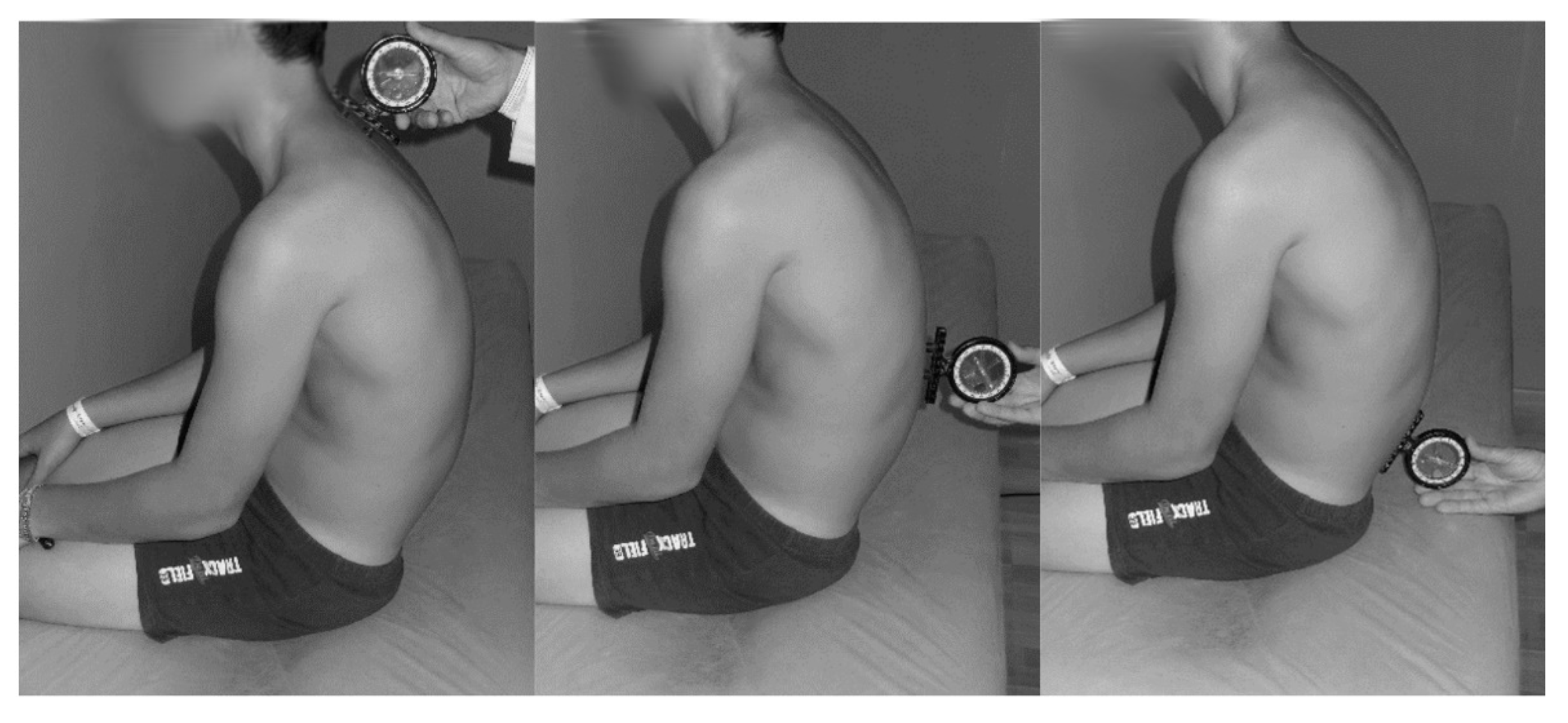
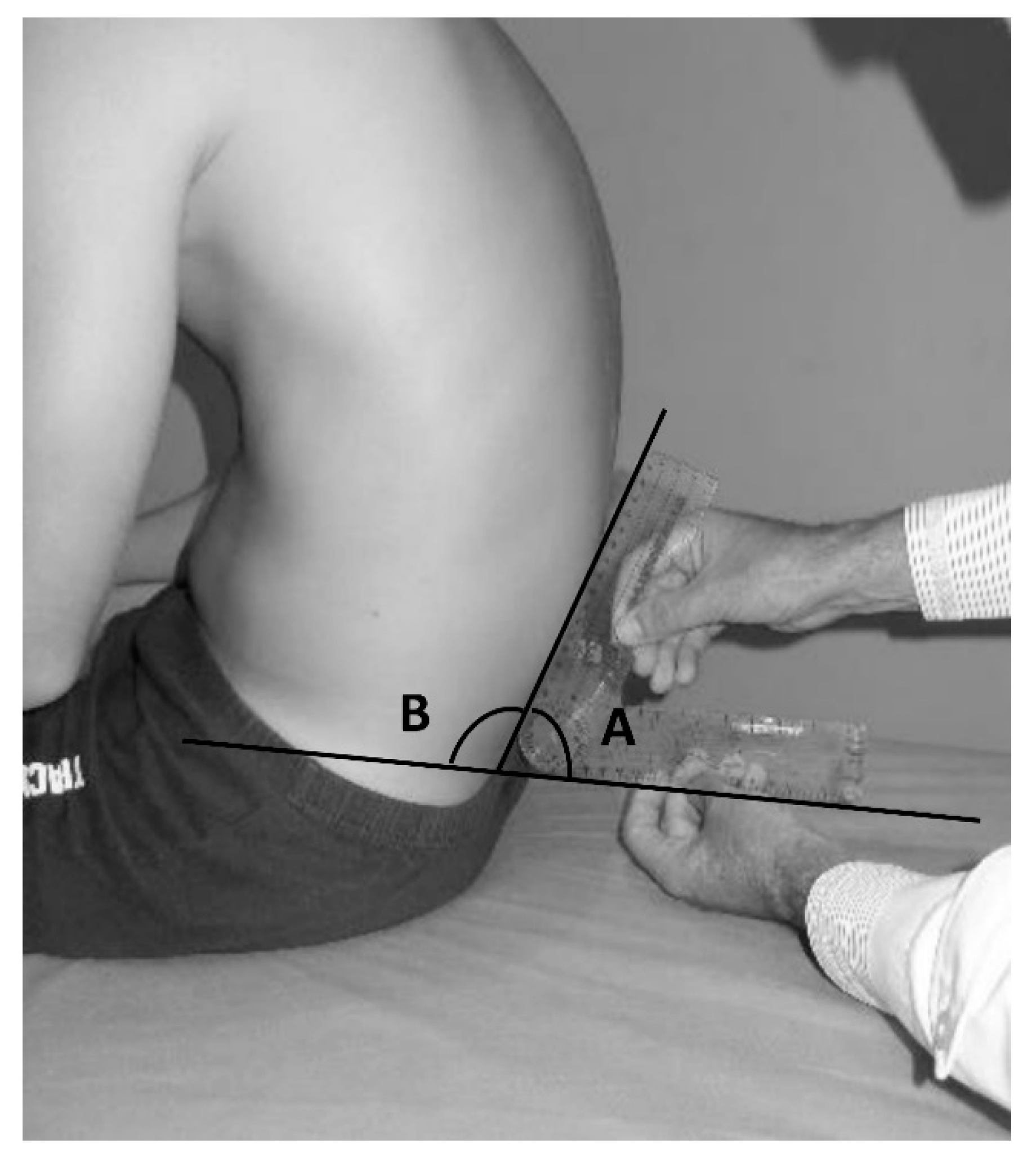
2.3.2. Pelvic Tilt Evaluation in a Slump Sitting Position
2.3.3. Back Pain Assessment
2.4. Statistical Analyses
3. Results
3.1. Sagittal Spinal Alignment and Pelvic Tilt in a Slump Sitting Position
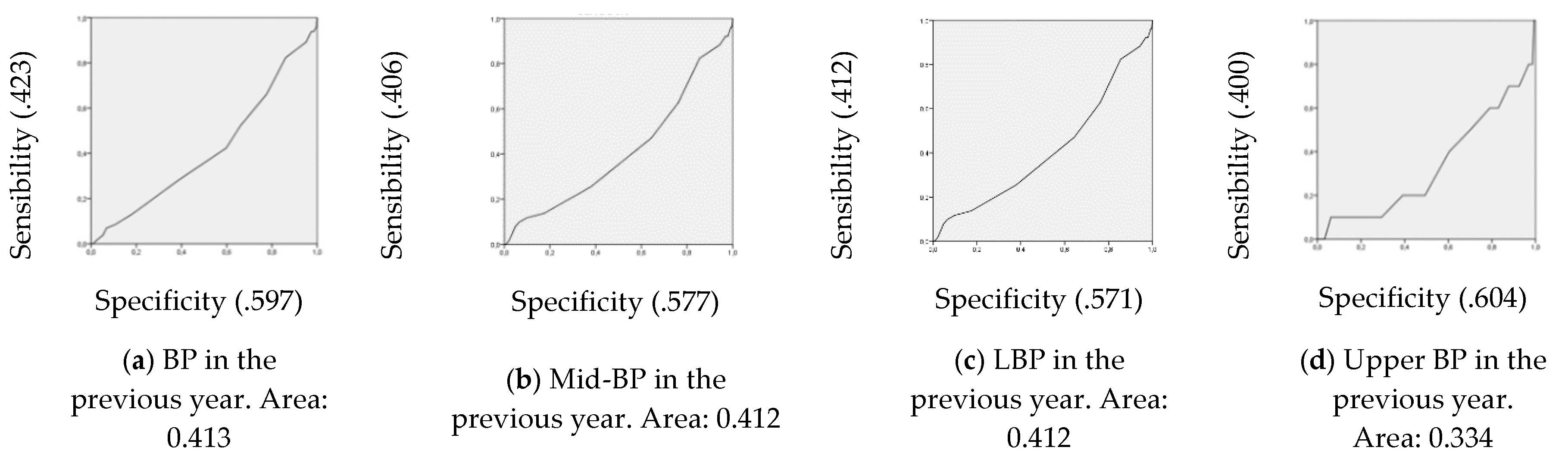
3.2. Sagittal Spinal Alignment in a Slump Sitting Position, Pelvic Tilt While Sitting and Back Pain
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Geldhof, E.; Cardon, G.; De Bourdeaudhuij, I.; Danneels, L.; Coorevits, P.; Vanderstraeten, G.; De Clercq, D. Effects of back posture education on elementary schoolchildren’s back function. Eur. Spine J. 2007, 16, 829–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minghelli, B.; Oliveira, R.; Nunes, C. Postural habits and weight of backpacks of Portuguese adolescents: Are they associated with scoliosis and low back pain? Work Read Mass. 2016, 54, 197–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, Q.; Jiang, C.; Zhou, Y.; Huang, Y.; Zhang, M. Relationship between spinal morphology and function and adolescent non-specific back pain: A cross-sectional study. J. Back Musculoskel. Rehabil. 2017, 30, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Panagiotopoulou, G.; Christoulas, K.; Papanckolaou, A.; Mandroukas, K. Classroom furniture dimensions and anthropometric measures in primary school. Appl. Ergon. 2004, 35, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Kamaci, S.; Yucekul, A.; Demirkiran, G.; Berktas, M.; Yazici, M. The Evolution of Sagittal Spinal Alignment in Sitting Position During Childhood. Spine 2015, 40, E787–E793. [Google Scholar] [CrossRef] [PubMed]
- Endo, K.; Suzuki, H.; Nishimura, H.; Tanaka, H.; Shishido, T.; Yamamoto, K. Sagittal lumbar and pelvic alignment in the standing and sitting positions. J. Orthop. Sci. 2012, 17, 682–686. [Google Scholar] [CrossRef] [PubMed]
- Philippot, R.; Wegrzyn, J.; Farizon, F.; Fessy, M.H. Pelvic balance in sagittal and Lewinnek reference planes in the standing, supine and sitting positions. Orthop. Traumatol. Surg. Res. 2009, 95, 70–76. [Google Scholar] [CrossRef]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Is ‘ideal’ sitting posture real? Measurement of spinal curves in four sitting postures. Man. Ther. 2009, 14, 404–408. [Google Scholar] [CrossRef]
- De Carvalho, D.E.; Soave, D.; Ross, K.; Callaghan, J.P. Lumbar spine and pelvic posture between standing and sitting: A radiologic investigation including reliability and repeatability of the lumbar lordosis measure. J Manipulative Physiol. Ther. 2010, 33, 48–55. [Google Scholar] [CrossRef]
- Drzał-Grabiec, J.; Snela, S.; Truszczyńska, A. The development of anterior-posterior spinal curvature in children aged 7–12 years. Biomed. Hum. Kinet. 2016, 8, 72–82. [Google Scholar] [CrossRef] [Green Version]
- Dunk, N.M.; Kedgley, A.E.; Jenkyn, T.R.; Callaghan, J.P. Evidence of a pelvis-driven flexion pattern: Are the joints of the lower lumbar spine fully flexed in seated postures? Clin. Biomech. 2009, 24, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Scannell, J.P.; McGill, S.M. Lumbar Posture—Should It, and Can It, Be Modified? A Study of Passive Tissue Stiffness and Lumbar Position During Activities of Daily Living. Phys. Ther. 2003, 83, 907–917. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, L.; Hancock, E.; Agouris, I.; Smith, F.W.; Macsween, A. The Response of the Nucleus Pulposus of the Lumbar Intervertebral Discs to Functionally Loaded Positions. Spine 2007, 32, 1508–1512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nazari, J.; Pope, M.H.; Graveling, R.A. Reality about migration of the nucleus pulposus within the intervertebral disc with changing postures. Clin. Biomech. 2012, 27, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Ledet, E.H.; Tymeson, M.P.; DiRisio, D.J.; Cohen, B.; Uhl, R.L. Direct real-time measurement of in vivo forces in the lumbar spine. Spine J. 2005, 5, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Castanharo, R.; Duarte, M.; McGill, S. Corrective sitting strategies: An examination of muscle activity and spine loading. J. Electromyogr. Kinesiol. 2014, 24, 114–119. [Google Scholar] [CrossRef]
- McGill, S. Ultimate Back Fitness and Performance, 6th ed.; Backfitpro Incorporated: Waterloo, ON, Canada, 2017. [Google Scholar]
- Arundell, L.; Salmon, J.; Koorts, H.; Ayala, A.M.C.; Timperio, A. Exploring when and how adolescents sit: Cross-sectional analysis of activPAL-measured patterns of daily sitting time, bouts and breaks. BMC Public Health 2019, 19, 653. [Google Scholar] [CrossRef] [Green Version]
- Sainz de Baranda, P.; Rodríguez, P.L.; Santonja, F.; Andújar, P. La Columna Vertebral del Escolar; Sevilla Wanceulen Editorial Deportiva: Sevilla, Spain, 2006; p. 205. [Google Scholar]
- O’Sullivan, P.; Grahamslaw, K.M.; Kendell, M.; Lapenskie, S.C.; Möller, N.E.; Richards, K.V. The Effect of Different Standing and Sitting Postures on Trunk Muscle Activity in a Pain-Free Population. Spine 2002, 27, 1238–1244. [Google Scholar] [CrossRef]
- Caneiro, J.P.; O’Sullivan, P.; Burnett, A.; Barach, A.; O’Neil, D.; Tveit, O.; Olafsdottir, K. The influence of different sitting postures on head/neck posture and muscle activity. Man. Ther. 2010, 15, 54–60. [Google Scholar] [CrossRef]
- Adams, M.A.; Bogduk, N.; Burton, K.; Dolan, P. The Biomechanics of Back Pain, 3rd ed.; Elsevier: Edinburgh, UK, 2012. [Google Scholar]
- Castellucci, H.; Arezes, P.; Viviani, C. Mismatch between classroom furniture and anthropometric measures in Chilean schools. Appl. Ergon. 2010, 41, 563–568. [Google Scholar] [CrossRef]
- Saarni, L.A.; Nygård, C.-H.; Kaukiainen, A.; Rimpelä, A. Are the desks and chairs at school appropriate? Ergonomics 2007, 50, 1561–1570. [Google Scholar] [CrossRef] [PubMed]
- Aparicio, E.Q.; Nogueras, A.M.; Sánchez, C.S.; López, I.R.; Sendín, N.L.; Arenillas, J.C. Estudio de la postura sedente en una población infantil. Fisioterapia 2004, 26, 153–163. [Google Scholar] [CrossRef]
- Kwon, Y.; Kim, J.-W.; Heo, J.-H.; Jeon, H.-M.; Choi, E.-B.; Eom, G.-M. The effect of sitting posture on the loads at cervico-thoracic and lumbosacral joints. Technol. Health Care 2018, 26, 409–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Womersley, L.; May, S. Sitting Posture of Subjects with Postural Backache. J. Manip. Physiol. Ther. 2006, 29, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Pynt, J.; Higgs, J.; Mackey, M. Seeking the optimal posture of the seated lumbar spine. Physiother. Theory Pr. 2001, 17, 5–21. [Google Scholar] [CrossRef]
- Adams, M.; Dolan, P.; Hutton, W.C. The Lumbar Spine in Backward Bending. Spine 1988, 13, 1019–1026. [Google Scholar] [CrossRef]
- Adams, M.; Hutton, W. The effect of posture on the role of the apophysial joints in resisting intervertebral compressive forces. J. Bone Jt. Surgery. Br. Vol. 1980, 62, 358–362. [Google Scholar] [CrossRef]
- Auvinen, J.; Tammelin, T.; Taimela, S.; Zitting, P.; Karppinen, J. Associations of physical activity and inactivity with low back pain in adolescents. Scand. J. Med. Sci. Sports 2007, 18, 188–194. [Google Scholar] [CrossRef]
- Dunk, N.M.; Callaghan, J.P. Lumbar spine movement patterns during prolonged sitting differentiate low back pain developers from matched asymptomatic controls. Work 2010, 35, 3–14. [Google Scholar] [CrossRef]
- Grimes, P.; Legg, S. Musculoskeletal Disorders (MSD) in School Students as a Risk Factor for Adult MSD: A Review of the Multiple Factors Affecting Posture, Comfort and Health in Classroom Environments. J. Hum.-Environ. Syst. 2004, 7, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Muñoz, I.C.; Kovacs, F.M.; Roqué, M.; Fernández, I.G.; Calvo, J.S. Risk Factors for Low Back Pain in Childhood and Adolescence. A Systematic Review. Clin. J. Pain 2017, 34, 468–484. [Google Scholar]
- Ginés-Díaz, A.; Martínez-Romero, M.T.; Cejudo, A.; Aparicio-Sarmiento, A.; Sainz de Baranda, P. Sagittal Spinal Morphotype Assessment in Dressage and Show Jumping Riders. J. Sport Rehabilit. 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Mengibar, J.M.; Sainz-De-Baranda, P.; Santonja-Medina, F. Training intensity and sagittal curvature of the spine in male and female artistic gymnasts. J. Sports Med. Phys. Fit. 2018, 58, 465–471. [Google Scholar]
- Saur, P.M.M.; Ensink, F.-B.M.; Frese, K.; Seeger, D.; Hildebrandt, J. Lumbar Range of Motion: Reliability and Validity of the Inclinometer Technique in the Clinical Measurement of Trunk Flexibility. Spine 1996, 21, 1332–1338. [Google Scholar] [CrossRef]
- Santonja, F. Las desviaciones sagitales del raquis y su relación con la práctica deportiva. In Escolar: Medicina y Deporte; Ferrer, V., Martínez, L., Santonja, F., Eds.; Diputación Provincial de Albacete: Albacete, Spain, 1996; pp. 251–268. [Google Scholar]
- Sainz de Baranda, P.; Rodríguez-García, P.L.; Santonja, F. Efectos sobre la disposición sagital del raquis de un programa de Educación Postural en Educación Física de Primaria. Apunts. Educ. Fís. Deporte 2010, 4, 16–21. [Google Scholar]
- Sainz de Baranda, P.; Santonja-Medina, F.; Rodríguez-Iniesta, M. Valoración de la disposición sagital del raquis en gimnastas especialistas en trampolín. (Assessment of the sagittal plane of the spine in trampoline gymnasts.). RICYDE Rev. Int. Cienc. Deport. 2009, 5, 21–33. [Google Scholar] [CrossRef]
- Sainz de Baranda, P.; Santonja, F.; Rodriguez-Iniesta, M. Tiempo de entrenamiento y plano sagital del raquis en gimnastas de trampolin. Rev. Int. Med. Cienc. Act. Fís. Deporte 2010, 10, 521–536. [Google Scholar]
- Santonja, F. Exploración Clínica y Radiográfica del Raquis Sagital. Sus Correlaciones; Universidad de Murcia: Murcia, Spain, 1993. [Google Scholar]
- Sainz de Baranda, P.; Rodríguez-Iniesta, M.; Ayala, F.; Santonja, F.; Cejudo, A. Determination of the Criterion-Related Validity of Hip Joint Angle Test for Estimating Hamstring Flexibility Using a Contemporary Statistical Approach. Clin. J. Sport Med. 2014, 24, 320–325. [Google Scholar] [CrossRef]
- Ayala, F.; Sainz de Baranda, P.; Cejudo, A.; Santonja, F. Pruebas angulares de estimación de la flexibilidad isquiosural: Descripción de los procedimientos exploratorios y valores de referencia. Rev. Andal. Med. Deport. 2013, 6, 120–128. [Google Scholar] [CrossRef] [Green Version]
- Ferrer, V. Repercusiones de la Cortedad Isquiosural Sobre la Pelvis y el Raquis Lumbar. Ph.D. Thesis, Universidad de Murcia, Murcia, Spain, 1998. [Google Scholar]
- Dionne, C.E.; Dunn, K.M.; Croft, P.; Nachemson, A.L.; Buchbinder, R.; Walker, B.; Wyatt, M.; Cassidy, J.D.; Rossignol, M.; Leboeuf-Yde, C.; et al. A Consensus Approach Toward the Standardization of Back Pain Definitions for Use in Prevalence Studies. Spine 2008, 33, 95–103. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Crespo, G.; Durán, M.R.-P.; López-Salguero, A.; Zarco-Periñán, M.; Ibáñez-Campos, T.; De Vargas, C.E.-R. Dolor de espalda en adolescentes: Prevalencia y factores asociados. Rehabilitación 2009, 43, 72–80. [Google Scholar] [CrossRef]
- Muñoz, I.C.; Conesa, A.G.; Sánchez-Meca, J. Prevalence of low back pain in children and adolescents: A meta-analysis. BMC Pediatr. 2013, 13, 14. [Google Scholar]
- Aparicio-Sarmiento, A.; Rodríguez-Ferrán, O.; Martínez-Romero, M.T.; Cejudo, A.; Santonja, F.; Sainz de Baranda, P. Back Pain and Knowledge of Back Care Related to Physical Activity in 12 to 17 Year Old Adolescents from the Region of Murcia (Spain): ISQUIOS Programme. Sustainability 2019, 11, 5249. [Google Scholar] [CrossRef] [Green Version]
- Coombes, E.; Jones, A.P.; Hillsdon, M. The relationship of physical activity and overweight to objectively measured green space accessibility and use. Soc. Sci. Med. 2010, 70, 816–822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cortes, C.; Mohri, M. AUC Optimization vs. Error Rate Minimization. In Proceedings of the Advances in Neural Information Processing Systems, Vancouver, CA, USA, 8–13 December 2003; pp. 313–320. [Google Scholar]
- Green, J.P.; Grenier, S.G.; McGill, S.M. Low-back stiffness is altered with warm-up and bench rest: Implications for athletes. Med. Sci. Sports Exerc. 2002, 34, 1076–1081. [Google Scholar] [CrossRef] [PubMed]
- Lengsfeld, M.; Frank, A.; Van Deursen, D.L.; Griss, P. Lumbar spine curvature during office chair sitting. Med Eng. Phys. 2000, 22, 665–669. [Google Scholar] [CrossRef]
- Bendix, T. Seated Trunk Posture at Various Seat Inclinations, Seat Heights, and Table Heights. Hum. Factors J. Hum. Factors Ergon. Soc. 1984, 26, 695–703. [Google Scholar] [CrossRef]
- Black, K.M.; McClure, P.; Polansky, M. The Influence of Different Sitting Positions on Cervical and Lumbar Posture. Spine 1996, 21, 65–70. [Google Scholar] [CrossRef]
- McGill, S.M. Distribution of tissue loads in the low back during a variety of daily and rehabilitation tasks. J. Rehabil. Res. Dev. 1997, 34, 448–458. [Google Scholar]
- Callaghan, J.P.; McGill, S.M. Intervertebral disc herniation: Studies on a porcine model exposed to highly repetitive flexion/extension motion with compressive force. Clin. Biomech. 2001, 16, 28–37. [Google Scholar] [CrossRef]
- Gunning, J.L.; Callaghan, J.P.; McGill, S.M. Spinal posture and prior loading history modulate compressive strength and type of failure in the spine: A biomechanical study using a porcine cervical spine model. Clin. Biomech. 2001, 16, 471–480. [Google Scholar] [CrossRef]
- McGill, S. Low Back Disorders. Evidence-Based Prevention and Rehabilitation; University of Human Kinetics: Waterloo, CA, USA, 2002; p. 424. [Google Scholar]
- O’Sullivan, P.; Smith, A.J.; Beales, D.J.; Straker, L. Association of Biopsychosocial Factors With Degree of Slump in Sitting Posture and Self-Report of Back Pain in Adolescents: A Cross-Sectional Study. Phys. Ther. 2011, 91, 470–483. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cil, A.; Yazici, M.; Uzumcugil, A.; Kandemir, U.; Alanay, A.; Alanay, Y.; Acaroglu, E.; Surat, A. The Evolution of Sagittal Segmental Alignment of the Spine During Childhood. Spine 2005, 30, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Mac-Thiong, J.-M.; Labelle, H.; Berthonnaud, E.; Betz, R.R.; Roussouly, P. Sagittal spinopelvic balance in normal children and adolescents. Eur. Spine J. 2005, 16, 227–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic Analysis of the Sagittal Alignment and Balance of the Spine in Asymptomatic Subjects. JBJS 2005, 87, 260. [Google Scholar] [CrossRef]
- Smith, A.; O’Sullivan, P.; Straker, L. Classification of Sagittal Thoraco-Lumbo-Pelvic Alignment of the Adolescent Spine in Standing and Its Relationship to Low Back Pain. Spine 2008, 33, 2101–2107. [Google Scholar] [CrossRef]
- Noll, M.; Candotti, C.T.; Da Rosa, B.N.; Sedrez, J.A.; Vieira, A.; Loss, J.F. Layout for Assessing Dynamic Posture. Pediatr. Phys. Ther. 2016, 28, 435–444. [Google Scholar] [CrossRef]
- Noll, M.; Silveira, E.A.; De Avelar, I.S. Evaluation of factors associated with severe and frequent back pain in high school athletes. PLoS ONE 2017, 12, e0171978. [Google Scholar] [CrossRef] [Green Version]
- Trompeter, K.; Fett, D.; Platen, P. Prevalence of Back Pain in Sports: A Systematic Review of the Literature. Sports Med. 2017, 47, 1183–1207. [Google Scholar] [CrossRef] [Green Version]
- Hakala, P.T.; Rimpelä, A.; Saarni, L.A.; Salminen, J.J. Frequent computer-related activities increase the risk of neck–shoulder and low back pain in adolescents. Eur. J. Public Health 2006, 16, 536–541. [Google Scholar] [CrossRef]
- Gupta, N.; Christiansen, C.S.; Hallman, D.M.; Korshøj, M.; Carneiro, I.G.; Holtermann, A. Is Objectively Measured Sitting Time Associated with Low Back Pain? A Cross-Sectional Investigation in the NOMAD study. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lis, A.M.; Black, K.M.; Korn, H.; Nordin, M. Association between sitting and occupational LBP. Eur. Spine J. 2006, 16, 283–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Troussier, B.; Salminen, J.J.; Balagué, F. Non-specific low back pain in children and adolescents: Risk factors. Eur. Spine J. 1999, 8, 429–438. [Google Scholar]
- Mohseni-Bandpei, M.A.; Bagheri-Nesami, M.; Shayesteh-Azar, M.; Bagheri-Nesami, M. Nonspecific Low Back Pain in 5000 Iranian School-age Children. J. Pediatr. Orthop. 2007, 27, 126–129. [Google Scholar] [CrossRef]
- Shehab, D.K.; Al-Jarallah, K.F. Nonspecific low-back pain in Kuwaiti children and adolescents: Associated factors. J. Adolesc. Health 2005, 36, 32–35. [Google Scholar] [CrossRef]
- Fernandes, J.A.A.; Genebra, C.V.D.S.; Maciel, N.M.; Fiorelli, A.; De Conti, M.H.S.; Vitta, F.C.F. Low Back Pain in Shoolchildren: A Cross-Sectional Study in a Western City of Sao Paulo State, Brazil. Acta Ortop. Bras. 2015, 23, 235–238. [Google Scholar] [CrossRef] [Green Version]
- Murphy, S.; Buckle, P.; Stubbs, D. A cross-sectional study of self-reported back and neck pain among English schoolchildren and associated physical and psychological risk factors. Appl. Ergon. 2007, 38, 797–804. [Google Scholar] [CrossRef]
- Filho, N.M.; Coutinho, E.S.; Silva, G.A.E. Association between home posture habits and low back pain in high school adolescents. Eur. Spine J. 2014, 24, 425–433. [Google Scholar] [CrossRef]
- Sainz de Baranda, P.; Cejudo, A.; Moreno-Alcaraz, V.J.; Martinez-Romero, M.T.; Aparicio-Sarmiento, A.; Santonja-Medina, F. Sagittal spinal morphotype assessment in 8 to 15 years old Inline Hockey players. Peer J. 2020, 8, e8229. [Google Scholar] [CrossRef] [Green Version]
- Wirth, B.; Knecht, C.; Humphreys, B.K. Spine day 2012: Spinal pain in Swiss school children– epidemiology and risk factors. BMC Pediatr. 2013, 13, 159. [Google Scholar] [CrossRef]
- Junge, T.; Wedderkopp, N.; Boyle, E.; Kjaer, P. The natural course of low back pain from childhood to young adulthood—A systematic review. Chiropr. Man. Ther. 2019, 27, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunn, K.M.; Hestbaek, L.; Cassidy, J.D. Low back pain across the life course. Best Pr. Res. Clin. Rheumatol. 2013, 27, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Chiwaridzo, M.; Naidoo, N. Are parents and adolescents in agreement on reporting of recurrent non-specific low back pain in adolescents? A cross-sectional descriptive study. BMC Pediatr. 2015, 15, 203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fogel, B.S.; Greenberg, D.B. Psychiatric Care of the Medical Patient Psychiatric. In Care of the Medical Patient; Oxford University Press: Oxford, UK, 2015. [Google Scholar]

| Variables | Age | Height | Weight | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Sex | Male (n = 281) | 10.41 | 1.16 | 141.88 | 8.90 | 39.93 | 10.54 |
| Female (n = 301) | 10.44 | 1.09 | 142.60 | 9.31 | 41.68 | 12.06 | |
| Age | 8 years (n = 62) | 8.44 | 0.29 | 129.70 | 5.21 | 30.82 | 6.01 |
| 9 years (n = 132) | 9.49 | 0.29 | 137.40 | 6.38 | 37.04 | 8.62 | |
| 10 years (n = 207) | 10.49 | 0.28 | 142.80 | 7.08 | 40.19 | 9.46 | |
| 11 years (n = 142) | 11.50 | 0.29 | 148.90 | 6.94 | 47.16 | 12.71 | |
| 12 years (n = 39) | 12.47 | 0.34 | 151.57 | 6.34 | 50.00 | 11.26 | |
| Total (n = 582) | 10.42 | 1.12 | 142.25 | 9.11 | 40.84 | 11.37 | |
| Variable | Thoracic Curve 1 | Lumbar Curve 1 | Pelvic Tilt (LSA) 1 | |
|---|---|---|---|---|
| Sex | Male (n = 281) | 43.86 ± 8.64 * | 25.90 ± 7.42 † | 107.99 ± 5.10 † |
| Female (n = 301) | 41.61 ± 9.83 | 22.79 ± 8.07 | 105.85 ± 5.79 | |
| Age | 8 years (n = 62) | 41.61 ± 7.83 | 25.81 ± 6.13 | 108.45 ± 4.63 † |
| 9 years (n = 132) | 42.09 ± 9.51 | 24.68 ± 7.09 | 107.50 ± 5.02 † | |
| 10 years (n = 207) | 44.13 ± 9.30 * | 25.05 ± 7.89 * | 107.53 ± 5.45 † | |
| 11 years (n = 142) | 40.72 ± 9.71 * | 22.62 ± 8.79 * | 104.92 ± 6.10 † | |
| 12 years (n = 39) | 46.10 ± 7.93 * | 22.62 ± 8.78 | 106.05 ± 5.55 | |
| Total (n = 582) | 42.70 ± 9.34 | 24.29 ± 7.91 | 106.88 ± 5.57 | |
| V | Thoracic Kyphosis 1 | Lumbar Kyphosis 1 | Pelvic Tilt (Retroversion) 1 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hypo | N | S Hyper | M Hyper | N | S Hyper | M Hyper | N | S | Sig. | |
| ♂ | 1 (16.67) | 112 (43.24) | 164 * (52.73) | 4 (66.67) | 22 (30.14) | 93 (41.33) | 166 † (58.45) | 28¥ (32.56) | 197 (49.62) | 56 (56.57) |
| ♀ | 5 (83.33) | 147 * (56.76) | 147 (47.27) | 2 (33.33) | 51† (69.86) | 132 † (58.67) | 118 (41.55) | 58 * (67.44) | 200 (50.38) | 43 (43.43) |
| 8y | 0 (0.00) | 32 (12.36) | 30 (9.65) | 0 (0.00) | 2¥ (2.74) | 25 (11.11) | 35 (12.32) | 5 (5.81) | 47 (11.84) | 10 (10.10) |
| 9y | 2 (33.33) | 59 (22.78) | 70 (22.51) | 1 (16.67) | 12 (16.44) | 56 (24.89) | 64 (22.54) | 13 (15.12) | 96 (24.18) | 23 (23.23) |
| 10y | 2 (33.33) | 74 (28.57) | 127 (40.84) | 4 (66.67) | 21 (28.77) | 77 (34.22) | 109 (38.38) | 24 (27.91) | 141 (35.52) | 42 (42.42) |
| 11y | 2 (33.33) | 79 (30.50) | 60 (19.29) | 1 (16.67) | 32 * (43.84) | 47 (20.89) | 63 (22.18) | 35 * (40.70) | 91 (22.92) | 16¥ (16.16) |
| 12y | 0 (0.00) | 15 (5.79) | 24 (7.72) | 0 (0.00) | 6 (8.22) | 20 (8.89) | 13 (4.58) | 9 (10.47) | 22 (5.54) | 8 (8.08) |
| T | 6 (1.03) | 259 (44.50) | 311 (53.44) | 6 (1.03) | 73 (12.54) | 225 (38.66) | 284 (48.80) | 86 (14.78) | 397 (68.21) | 99 (17.01) |
| H | 146.92 ± 11.21 | 142.36 ± 9.12 | 141.97 ± 9.06 | 147.98 ±8.25 | 146.44 ± 8.30 *,† | 142.49 * ± 8.71 | 140.99 † ± 9.31 | 146.67 † ± 9.03 | 141.72 † ± 8.79 | 140.57 † ± 9.38 |
| W | 46.37 ± 18.15 | 41.69 ± 12.05 | 40.01 ± 10.61 | 41.12 ±10.44 | 51.34† ± 13.95 | 42.10 † ± 10.43 | 37.13 † ± 9.30 | 52.84 † ± 13.85 | 39.41 †,* ± 9.43 | 36.14 † * ± 9.16 |
| Spinal Curves | LSA or Pelvic Tilt | |||
|---|---|---|---|---|
| Normal 1 | Slight Retroversion 1 | Significant Retroversion 1 | ||
| Thoracic kyphosis | Hypokyphosis | 3 (3.49) † | 3 (0.76) | 0 (0.00) |
| Normal | 50 (58.14) † | 186 (46.85) | 23 (23.23) † ¥ | |
| Slight hyperkyphosis | 33 (38.37) † ¥ | 203 (51.13) | 75 (75.76) † | |
| Moderate hyperkyphosis | 0 (0.00) | 5 (1.26) | 1 (1.01) | |
| Lumbar kyphosis | Normal | 40 (46.51) † | 32 (8.06) † ¥ | 1 (1.01) † ¥ |
| Slight hyperkyphosis | 33 (38.37) | 179 (45.09) † | 13 (13.13) † ¥ | |
| Moderate hyperkyphosis | 13 (15.12) † ¥ | 186 (46.85) | 85 (85.86) † | |
| BP by Recurrence in the Previous Year, Body Area and Prevalence Period | Thoracic Curve 1 | Lumbar Curve 1 | Pelvic Tilt (LSA) 1 | ||
|---|---|---|---|---|---|
| Previous year | BP | No (n = 452) | 42.81 ± 9.23 | 24.64 ± 7.84 * | 107.27 ± 5.38 * |
| Yes (n = 130) | 42.32 ± 9.73 | 23.08 ± 8.06 | 105.52 ± 6.00 | ||
| One-time event (n = 39) | 43,54 ± 12,76 | 23,95 ± 7,29 | 106,21 ± 6,00 | ||
| Recurrent BP (n = 91) | 41,80 ± 8,12 | 22,70 ± 8,38 | 105,23 ± 6,01 | ||
| Upper BP | No (n = 546) | 42.65 ± 9.22 | 24.34 ± 7.94 | 106.91 ± 5.62 | |
| Yes (n = 31) | 43.16 ± 11.70 | 22.90 ± 7.28 | 105.94 ± 4.77 | ||
| Mid-BP | No (n = 508) | 42.77 ± 9.60 | 24.45 ± 7.79 | 107.11 ± 5.39 * | |
| Yes (n = 69) | 41.97 ± 7.35 | 22.87 ± 8.68 | 105.04 ± 6.57 | ||
| LBP | No (n = 525) | 42.76 ± 9.28 | 24.44 ± 7.83 | 107.02 ± 5.45 * | |
| Yes (n = 51) | 41.80 ± 10.29 | 22.47 ± 8.56 | 105.37 ± 6.58 | ||
| Previous week | BP | No (n = 516) | 42.62 ± 9.59 | 24.42 ± 7.89 | 106.97 ± 5.59 |
| Yes (n = 62) | 43.48 ± 7.05 | 23.03 ± 8.14 | 106.29 ± 5.27 | ||
| Upper BP | No (n = 568) | 42.70 ± 9.39 | 24.36 ± 7.86 * | 106.93 ± 5.50 | |
| Yes (n = 10) | 43.60 ± 6.65 | 19.00 ± 10.08 | 105.20 ± 8.23 | ||
| Mid-BP | No (n = 533) | 42.66 ± 9.54 | 24.38 ± 7.87 | 106.93 ± 5.55 | |
| Yes (n = 45) | 43.33 ± 6.77 | 22.93 ± 8.50 | 106.53 ± 5.70 | ||
| LBP | No (n = 561) | 42.62 ± 9.38 | 24.35 ± 7.90 | 106.97 ± 5.54 | |
| Yes (n = 17) | 46.00 ± 7.87 | 21.41 ± 8.54 | 104.47 ± 5.50 | ||
| Variable | Categories | LSA | Lumbar Curve | OR * | SE | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|---|---|---|
| <107° | ≥107° | <23° | ≥23° | ||||||
| BP (year) | No (n = 516) | 39.2% | 60.8% | - | - | 1.059 (small) | 0.018 | 1.021 to 1.097 | 0.002 |
| Yes (n = 62) | 28.5% | 71.5% | - | - | |||||
| MB pain (year) | No (n = 508) | 62.2% | 37.8% | - | - | 1.069 (small) | 0.023 | 1.021 to 1.118 | 0.004 |
| Yes (n = 69) | 71.0% | 29.0% | - | - | |||||
| LBP (year) | No (n = 525) | 62.1% | 37.9% | - | - | 1.054 (small) | 0.026 | 1.001 to 1.109 | 0.045 |
| Yes (n = 51) | 74.5% | 25.5% | - | - | |||||
| UB pain (week) | No (n = 568) | - | - | 49.3% | 50.7% | 1.082 (small) | 0.026 | 1.005 to 1.116 | 0.036 |
| Yes (n = 10) | - | - | 20.0% | 80.0% | |||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sainz de Baranda, P.; Cejudo, A.; Martínez-Romero, M.T.; Aparicio-Sarmiento, A.; Rodríguez-Ferrán, O.; Collazo-Diéguez, M.; Hurtado-Avilés, J.; Andújar, P.; Santonja-Medina, F. Sitting Posture, Sagittal Spinal Curvatures and Back Pain in 8 to 12-Year-Old Children from the Region of Murcia (Spain): ISQUIOS Programme. Int. J. Environ. Res. Public Health 2020, 17, 2578. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072578
Sainz de Baranda P, Cejudo A, Martínez-Romero MT, Aparicio-Sarmiento A, Rodríguez-Ferrán O, Collazo-Diéguez M, Hurtado-Avilés J, Andújar P, Santonja-Medina F. Sitting Posture, Sagittal Spinal Curvatures and Back Pain in 8 to 12-Year-Old Children from the Region of Murcia (Spain): ISQUIOS Programme. International Journal of Environmental Research and Public Health. 2020; 17(7):2578. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072578
Chicago/Turabian StyleSainz de Baranda, Pilar, Antonio Cejudo, María Teresa Martínez-Romero, Alba Aparicio-Sarmiento, Olga Rodríguez-Ferrán, Mónica Collazo-Diéguez, José Hurtado-Avilés, Pilar Andújar, and Fernando Santonja-Medina. 2020. "Sitting Posture, Sagittal Spinal Curvatures and Back Pain in 8 to 12-Year-Old Children from the Region of Murcia (Spain): ISQUIOS Programme" International Journal of Environmental Research and Public Health 17, no. 7: 2578. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072578






