The Impact of IT-Based Healthcare Communication on Mammography Screening Utilization among Women in the United States: National Health Interview Survey (2011–2018)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Resource
2.2. Study Population and Sample Data
2.3. Variables
2.3.1. Outcomes
2.3.2. Exposures
2.3.3. Confounding Variables
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
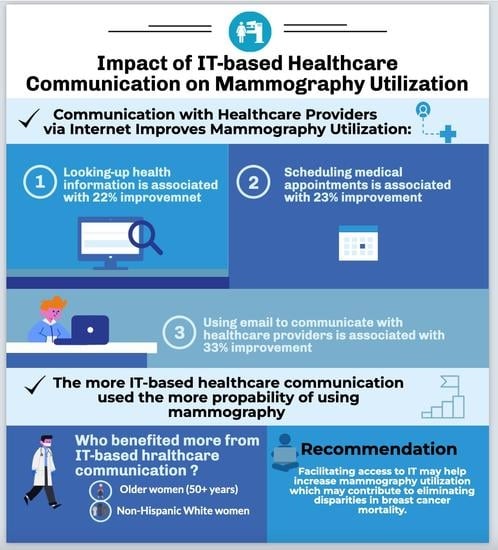
3.2. Associations between IT-Based Healthcare Communication Strategies and Mammography Screening Utilization
3.3. Associations between IT-Based Healthcare Communication Strategies and Mammography Screening Utilization after Adjusting for Mammography Recommendation
3.4. The Predicted Probability of Mammography Screening Utilization by the Number of IT-Based Healthcare Communication Strategies
3.5. Effect Modification by Race/Ethnicity on the Association between IT-Based Healthcare Communication and Mammography Utilization
3.6. Effect Modification by Age on the Association between IT-Based Healthcare Communication and Mammography Utilization
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cokkinides, V.; Albano, J.; Samuels, A.; Ward, M.; Thum, J. American Cancer Society: Cancer Facts and Figures; American Cancer Society: Atlanta, GA, USA, 2005. [Google Scholar]
- US Department of Health and Human Services Office of Disease Prevention and Health Promotion. Available online: https://www.healthypeople.gov/2020/data-search/Search-the-Data?nid=4055 (accessed on 27 June 2021).
- American Cancer Society. Cancer Facts & Figures. 2019. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf?utm_medium=email&utm_source=transaction (accessed on 12 October 2020).
- Ha, J.F.; Longnecker, N. Doctor-Patient Communication: A Review. Ochsner J. 2010, 10, 38. [Google Scholar] [CrossRef] [PubMed]
- Peterson, E.B.; Ostroff, J.S.; DuHamel, K.N.; D’Agostino, T.A.; Hernandez, M.; Canzona, M.R.; Bylund, C.L. Impact of provider-patient communication on cancer screening adherence: A systematic review. Prev. Med. 2016, 93, 96–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meguerditchian, A.N.; Dauphinee, D.; Girard, N.; Eguale, T.; Riedel, K.; Jacques, A.; Tamblyn, R. Do physician communication skills influence screening mammography utilization? BMC Health Serv. Res. 2012, 12, 219. [Google Scholar] [CrossRef] [Green Version]
- Roman, L.; Meghea, C.; Ford, S.; Penner, L.; Hamade, H.; Estes, T.; Williams, K.P. Individual, provider, and system risk factors for breast and cervical cancer screening among underserved Black, Latina, and Arab women. J. Women’s Health 2014, 23, 57–64. [Google Scholar] [CrossRef] [Green Version]
- Kindratt, T.B.; Dallo, F.J.; Allicock, M.; Atem, F.; Balasubramanian, B.A. The influence of patient-provider communication on cancer screenings differs among racial and ethnic groups. Prev. Med. Rep. 2020, 18, 101086. [Google Scholar] [CrossRef] [PubMed]
- Spring, L.M.; Marshall, M.R.; Warner, E.T. Mammography decision making: Trends and predictors of provider communication in the Health Information National Trends Survey, 2011 to 2014. Cancer 2016, 123, 401–409. [Google Scholar] [CrossRef] [Green Version]
- U.S. Department of Health and Human Services. Healthy People 2030. Available online: https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-it/increase-proportion-adults-who-use-it-track-health-care-data-or-communicate-providers-hchit-07 (accessed on 12 November 2021).
- Calton, B.; Abedini, N.; Fratkin, M. Telemedicine in the Time of Coronavirus. J. Pain Symptom Manag. 2020, 60, e12–e14. [Google Scholar] [CrossRef]
- Tan, S.S.-L.; Goonawardene, N. Internet Health Information Seeking and the Patient-Physician Relationship: A Systematic Review. J. Med. Internet Res. 2017, 19, e9. [Google Scholar] [CrossRef]
- Liu, P.L.; Yeo, T.E.D. How Online Patient-Provider Communication Impacts Quality of Life: Examining the Role of Patient-Centered Care and Health Competence. Health Commun. 2021, 1–6. [Google Scholar] [CrossRef]
- Lee, J. The impact of health information technology on disparity of process of care. Int. J. Equity Health 2015, 14, 34. [Google Scholar] [CrossRef]
- Zhang, X.; Hailu, B.; Tabor, D.C.; Gold, R.; Sayre, M.H.; Sim, I.; Jean-Francois, B.; Casnoff, C.A.; Cullen, T.; Thomas, V.A.; et al. Role of Health Information Technology in Addressing Health Disparities: Patient, Clinician, and System Perspectives. Med. Care 2019, 57, S115–S120. [Google Scholar] [CrossRef] [PubMed]
- Elkin, E.B.; Pocus, V.H.; Mushlin, A.I.; Cigler, T.; Atoria, C.L.; Polaneczky, M.M. Facilitating informed decisions about breast cancer screening: Development and evaluation of a web-based decision aid for women in their 40s. BMC Med. Inform. Decis. Mak. 2017, 17, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eden, K.B.; Scariati, P.; Klein, K.; Watson, L.; Remiker, M.; Hribar, M.; Forro, V.; Michaels, L.; Nelson, H.D. Mammography Decision Aid Reduces Decisional Conflict for Women in Their Forties Considering Screening. J. Women’s Health 2015, 24, 1013–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerrison, R.S.; Shukla, H.; Cunningham, D.; Oyebode, O.; Friedman, E. Text-message reminders increase uptake of routine breast screening appointments: A randomised controlled trial in a hard-to-reach population. Br. J. Cancer 2015, 112, 1005–1010. [Google Scholar] [CrossRef] [Green Version]
- Wright, A.; Poon, E.G.; Wald, J.; Feblowitz, J.; Pang, J.E.; Schnipper, J.L.; Grant, R.W.; Gandhi, T.K.; Volk, L.A.; Bloom, A.; et al. Randomized Controlled Trial of Health Maintenance Reminders Provided Directly to Patients Through an Electronic PHR. J. Gen. Intern. Med. 2011, 27, 85–92. [Google Scholar] [CrossRef] [Green Version]
- National Center for Health Statistics. NHIS Data, Questionnaires and Related Documentation. Available online: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm (accessed on 25 January 2022).
- Centers for Disease Control and Prevention (CDC). Breast Cancer Screening Guidelines for Women. 2020. Available online: https://www.cdc.gov/cancer/breast/pdf/breast-cancer-screening-guidelines-508.pdf (accessed on 28 January 2021).
- Agresti, A. Categorical Data Analysis, 3rd ed.; Wiley: New York, NY, USA, 2013. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [Green Version]
- Shi, W.; Nagler, R.H.; Fowler, E.F.; Gollust, S.E. Predictors of Women’s Awareness of the Benefits and Harms of Mammography Screening and Associations with Confusion, Ambivalence, and Information Seeking. Health Commun. 2019, 36, 303–314. [Google Scholar] [CrossRef]
- Zhao, P.; Yoo, I.; Lavoie, J.; Lavoie, B.J.; Simoes, E. Web-Based Medical Appointment Systems: A Systematic Review. J. Med. Internet Res. 2017, 19, e134. [Google Scholar] [CrossRef] [Green Version]
- Kindratt, T.B.; Allicock, M.; Atem, F.; Dallo, F.J.; Balasubramanian, B.A. Email Patient-Provider Communication and Cancer Screenings among US Adults: Cross-sectional Study. JMIR Cancer 2021, 7, e23790. [Google Scholar] [CrossRef]
- Kindratt, T.B.; Atem, F.; Dallo, F.J.; Allicock, M.; Balasubramanian, B.A. The Influence of Patient–Provider Communication on Cancer Screening. J. Patient Exp. 2020, 7, 1648–1657. [Google Scholar] [CrossRef]
- Sims, T.; Reed, A.E.; Carr, D.C. Information and Communication Technology Use Is Related to Higher Well-Being among the Oldest-Old. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2016, 72, 761–770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 5, 1173–1182. [Google Scholar] [CrossRef]

| Variable | Frequency (N) | Percentage (%) | |
|---|---|---|---|
| Age group | 40–49 | 21,645 | 22.96 |
| 50+ | 72,645 | 77.04 | |
| Race/ethnicity | Hispanic | 11,548 | 12.25 |
| NH White a | 63,843 | 67.71 | |
| NH Black b | 13,287 | 14.09 | |
| NH Other c | 5612 | 5.95 | |
| Marital Status | Currently married | 40,382 | 42.83 |
| Otherwise | 53,908 | 57.17 | |
| Region | Northeast | 16,527 | 17.53 |
| Midwest | 20,246 | 21.47 | |
| South | 34,456 | 36.54 | |
| West | 23,061 | 24.46 | |
| Insurance Coverage | Private | 56,171 | 59.73 |
| Public | 25,374 | 26.98 | |
| Military | 3350 | 3.56 | |
| Other | 1325 | 1.41 | |
| Uninsured | 7814 | 8.31 | |
| Education | Less than high school | 16,769 | 17.88 |
| High school | 22,561 | 24.05 | |
| Some college | 28,120 | 29.98 | |
| Bachelor’s degree | 15,940 | 16.99 | |
| Graduate degree | 10,408 | 11.10 | |
| Ratio of Family Income to the Poverty Threshold | <100% | 12,863 | 15.23 |
| 100–199% | 17,511 | 20.73 | |
| 200–399% | 23,969 | 28.38 | |
| ≥400% | 30,113 | 35.66 | |
| Work Status | Yes | 46,519 | 49.36 |
| No | 47,718 | 50.64 | |
| Survey Year | Year 2011 | 11,574 | 12.27 |
| Year 2012 | 12,306 | 13.05 | |
| Year 2013 | 12,364 | 13.11 | |
| Year 2014 | 13,436 | 14.25 | |
| Year 2015 | 12,483 | 13.24 | |
| Year 2016 | 12,253 | 13.00 | |
| Year 2017 | 10,099 | 10.71 | |
| Year 2018 | 9775 | 10.37 | |
| Mammography Utilization by Time Period | Odds Ratio | S.E. | p | 95% Conf. Interval | |
|---|---|---|---|---|---|
| All years 2011–2018 (n = 94,290) b | |||||
| Q1 c | 1.22 | 0.02 | <0.001 | 1.18 | 1.27 |
| Q2 d | 1.23 | 0.04 | <0.001 | 1.16 | 1.30 |
| Q3 e | 1.33 | 0.03 | <0.001 | 1.26 | 1.40 |
| Q4 f | 1.27 | 0.02 | <0.001 | 1.23 | 1.32 |
| Year 2011 (n = 11,574) | |||||
| Q1 c | 1.20 | 0.06 | 0.001 | 1.08 | 1.34 |
| Q2 d | 1.43 | 0.18 | 0.004 | 1.12 | 1.83 |
| Q3 e | 1.26 | 0.13 | 0.029 | 1.02 | 1.56 |
| Q4 f | 1.24 | 0.07 | <0.001 | 1.12 | 1.38 |
| Year 2012 (n = 12,306) | |||||
| Q1 c | 1.14 | 0.06 | 0.010 | 1.03 | 1.26 |
| Q2 d | 1.40 | 0.17 | 0.005 | 1.10 | 1.77 |
| Q3 e | 1.25 | 0.13 | 0.031 | 1.02 | 1.53 |
| Q4 f | 1.16 | 0.06 | <0.001 | 1.05 | 1.29 |
| Year 2013 (n = 12,364) | |||||
| Q1 c | 1.15 | 0.06 | 0.004 | 1.05 | 1.27 |
| Q2 d | 1.24 | 0.12 | 0.020 | 1.03 | 1.50 |
| Q3 e | 1.32 | 0.11 | 0.001 | 1.12 | 1.56 |
| Q4 f | 1.16 | 0.06 | 0.001 | 1.05 | 1.28 |
| Year 2014 (n = 13,436) | |||||
| Q1 c | 1.29 | 0.06 | <0.001 | 1.18 | 1.41 |
| Q2 d | 1.35 | 0.13 | 0.002 | 1.12 | 1.63 |
| Q3 e | 1.41 | 0.12 | <0.001 | 1.20 | 1.65 |
| Q4 f | 1.33 | 0.06 | <0.001 | 1.22 | 1.46 |
| Year 2015 (n = 12,483) | |||||
| Q1 c | 1.23 | 0.06 | <0.001 | 1.21 | 1.35 |
| Q2 d | 1.32 | 0.10 | <0.001 | 1.13 | 1.53 |
| Q3 e | 1.25 | 0.09 | 0.002 | 1.09 | 1.43 |
| Q4 f | 1.27 | 0.06 | <0.001 | 1.16 | 1.40 |
| Year 2016 (n = 12,253) | |||||
| Q1 c | 1.28 | 0.06 | <0.001 | 1.17 | 1.41 |
| Q2 d | 1.29 | 0.09 | 0.001 | 1.12 | 1.49 |
| Q3 e | 1.48 | 0.10 | <0.001 | 1.30 | 1.69 |
| Q4 | 1.30 | 0.06 | <0.001 | 1.18 | 1.42 |
| Year 2017 (n = 10,099) | |||||
| Q1 c | 1.30 | 0.07 | <0.001 | 1.18 | 1.44 |
| Q2 d | 1.19 | 0.09 | 0.019 | 1.03 | 1.38 |
| Q3 e | 1.61 | 0.11 | <0.001 | 1.40 | 1.84 |
| Q4 f | 1.38 | 0.07 | <0.001 | 1.25 | 1.53 |
| Year 2018 (n = 9775) | |||||
| Q1 c | 1.36 | 0.07 | <0.001 | 1.23 | 1.50 |
| Q2 d | 1.21 | 0.08 | 0.005 | 1.06 | 1.39 |
| Q3 e | 1.34 | 0.09 | <0.001 | 1.18 | 1.52 |
| Q4 f | 1.43 | 0.08 | <0.001 | 1.28 | 1.59 |
| Mammography Utilization | Odds Ratio | S.E. | p | 95% Conf. Interval | |
|---|---|---|---|---|---|
| Q1 a | |||||
| Adjusted model 1 b | 1.23 | 0.06 | <0.001 | 1.12 | 1.35 |
| Adjusted model 2 c | 1.15 | 0.06 | 0.006 | 1.04 | 1.27 |
| Q2 d | |||||
| Adjusted model 1 b | 1.32 | 0.10 | <0.001 | 1.12 | 1.54 |
| Adjusted model 2 c | 1.34 | 0.12 | 0.001 | 1.13 | 1.59 |
| Q3 e | |||||
| Adjusted model 1 b | 1.25 | 0.09 | 0.002 | 1.08 | 1.43 |
| Adjusted model 2 c | 1.16 | 0.09 | 0.049 | 1.00 | 1.35 |
| Q4 f | |||||
| Adjusted model 1 b | 1.27 | 0.06 | <0.001 | 1.16 | 1.40 |
| Adjusted model 2 c | 1.18 | 0.06 | 0.001 | 1.07 | 1.31 |
| Mammography Utilization | Odds Ratio | S.E. | p | 95% Conf. Interval | |
|---|---|---|---|---|---|
| Q1 c | |||||
| Exposure effect | 1.23 | 0.02 | <0.001 | 1.18 | 1.27 |
| Baseline difference | |||||
| Hispanic | 1.55 | 0.04 | <0.001 | 1.46 | 1.64 |
| NH Black d | 1.54 | 0.04 | <0.001 | 1.46 | 1.63 |
| NH other e | 1.05 | 0.04 | 0.186 | 0.97 | 1.14 |
| Effect modification by race | |||||
| Hispanic vs. NH White a | 0.76 | 0.03 | <0.001 | 0.70 | 0.84 |
| NH Black d vs. NH White a | 0.84 | 0.04 | <0.001 | 0.77 | 0.92 |
| NH other e vs. NH White a | 0.93 | 0.06 | 0.275 | 0.83 | 1.05 |
| Q2 f | |||||
| Exposure effect | 1.14 | 0.03 | <0.001 | 1.08 | 1.21 |
| Baseline difference | |||||
| Hispanic | 1.38 | 0.03 | <0.001 | 1.32 | 1.45 |
| NH Black d | 1.41 | 0.03 | <0.001 | 1.35 | 1.48 |
| NH other e | 0.98 | 0.03 | 0.497 | 0.92 | 1.04 |
| Effect modification by race | |||||
| Hispanic vs. NH White a | 0.86 | 0.08 | 0.106 | 0.73 | 1.03 |
| NH Black d vs. NH White a | 1.02 | 0.08 | 0.768 | 0.87 | 1.20 |
| NH other e vs. NH White a | 1.18 | 0.12 | 0.102 | 0.97 | 1.43 |
| Q3 g | |||||
| Exposure effect | 1.28 | 0.03 | <0.001 | 1.22 | 1.35 |
| Baseline difference | |||||
| Hispanic | 1.41 | 0.03 | <0.001 | 1.34 | 1.48 |
| NH Black d | 1.43 | 0.03 | <0.001 | 1.36 | 1.49 |
| NH Other e | 1.01 | 0.03 | 0.835 | 0.94 | 1.07 |
| Effect modification by race | |||||
| Hispanic vs. NH White a | 0.72 | 0.06 | <0.001 | 0.60 | 0.86 |
| NH Black d vs. NH White a | 0.95 | 0.08 | 0.574 | 0.81 | 1.12 |
| NH other e vs. NH White a | 0.95 | 0.09 | 0.620 | 0.79 | 1.15 |
| Q4 h | |||||
| Exposure effect | 1.28 | 0.02 | <0.001 | 1.23 | 1.33 |
| Baseline difference | |||||
| Hispanic | 1.57 | 0.05 | <0.001 | 1.48 | 1.67 |
| NH Black d | 1.55 | 0.04 | <0.001 | 1.47 | 1.64 |
| NH other e | 1.07 | 0.04 | 0.105 | 0.98 | 1.16 |
| Effect modification by race | |||||
| Hispanic vs. NH White a | 0.75 | 0.03 | <0.001 | 0.69 | 0.83 |
| NH Black d vs. NH White a | 0.85 | 0.04 | <0.001 | 0.78 | 0.93 |
| NH other e vs. NH White a | 0.93 | 0.06 | 0.212 | 0.82 | 1.04 |
| Mammography Utilization | Odds Ratio | S.E. | p | 95% Conf. Interval | |
|---|---|---|---|---|---|
| Q1 b | |||||
| Exposure effect | 0.72 | 0.02 | <0.001 | 0.69 | 1.76 |
| Baseline difference | |||||
| 50+ | 2.71 | 0.06 | <0.001 | 2.58 | 0.76 |
| Effect modification by age | |||||
| 50+ vs. 40–49 | 1.85 | 0.05 | <0.001 | 1.74 | 1.96 |
| Q2 c | |||||
| Exposure effect | 1.06 | 0.03 | 0.016 | 1.01 | 1.12 |
| Baseline difference | |||||
| 50+ | 3.29 | 0.07 | <0.001 | 3.16 | 3.42 |
| Effect modification by age | |||||
| 50+ vs. 40–49 | 1.35 | 0.02 | <0.001 | 1.30 | 1.40 |
| Q3 d | |||||
| Exposure effect | 1.14 | 0.03 | <0.001 | 1.09 | 1.19 |
| Baseline difference | |||||
| 50+ | 3.31 | 0.07 | <0.001 | 3.18 | 3.44 |
| Effect modification by age | |||||
| 50+ vs. 40–49 | 1.34 | 0.02 | <0.001 | 1.29 | 1.39 |
| Q4 e | |||||
| Exposure effect | 0.80 | 0.02 | <0.001 | 0.76 | 0.84 |
| Baseline difference | |||||
| 50+ | 3.88 | 0.07 | <0.001 | 2.75 | 3.02 |
| Effect modification by age | |||||
| 50+ vs. 40–49 | 1.67 | 0.05 | <0.001 | 1.57 | 1.76 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alabdullatif, N.; Arrieta, A.; Dlugasch, L.; Hu, N. The Impact of IT-Based Healthcare Communication on Mammography Screening Utilization among Women in the United States: National Health Interview Survey (2011–2018). Int. J. Environ. Res. Public Health 2022, 19, 12737. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph191912737
Alabdullatif N, Arrieta A, Dlugasch L, Hu N. The Impact of IT-Based Healthcare Communication on Mammography Screening Utilization among Women in the United States: National Health Interview Survey (2011–2018). International Journal of Environmental Research and Public Health. 2022; 19(19):12737. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph191912737
Chicago/Turabian StyleAlabdullatif, Noof, Alejandro Arrieta, Lucie Dlugasch, and Nan Hu. 2022. "The Impact of IT-Based Healthcare Communication on Mammography Screening Utilization among Women in the United States: National Health Interview Survey (2011–2018)" International Journal of Environmental Research and Public Health 19, no. 19: 12737. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph191912737