Dangerous Liaisons: Gammaherpesvirus Subversion of the Immunoglobulin Repertoire
Abstract
:1. Introduction
2. B Lymphocytes: A Major Reservoir of Gammaherpesvirus Latency and Lymphoproliferations
2.1. Epstein–Barr Virus, Prototype Member of the Lymphocryptovirus Subfamily of the Gammaherpesviruses
2.2. Kaposi Sarcoma Herpesvirus, Prototype Member of the Rhadinovirus Subfamily of the Gammaherpesviruses
2.3. Murine Gammaherpesvirus 68 Infection of Mice, an Animal Pathogen System
3. Germinal Center Processes That Shape B Cell Evolution and Gammaherpesvirus Latency
3.1. Dynamic Molecular Events as the B Cell Traverses Compartments of the Germinal Center
3.1.1. Overview
3.1.2. Immunoglobulin Assembly and Somatic Hypermutation
3.1.3. Isotype Class Switching
3.1.4. Genome Instability
3.1.5. Receptor Editing
3.2. B Cell Differentiation and Selection Processes in the Context of GHV Infection
3.2.1. Epstein–Barr Virus
3.2.2. Kaposi Sarcoma Herpesvirus
3.2.3. Animal Models to Investigate the Interplay of GHVs with B Cell Biology
4. Immunoglobulin Bias in Gammaherpesvirus Infection
4.1. Epstein–Barr Virus
4.2. Kaposi Sarcoma Herpesvirus
4.3. Murine Gammaherpesvirus 68
5. Conclusions and Future Directions in the Field
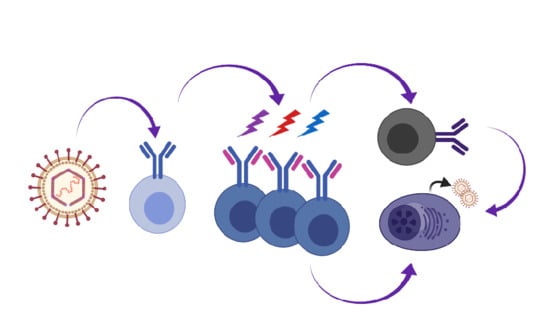
5.1. GHV GC Model
- The Ig repertoire of MHV68-infected cells is distinct from uninfected cells, indicating that infection of B cells in GC is not a stochastic event [88,89]. There is very little clonal overlap between the uninfected and infected cells [88]. This suggests that the virus enters the GC via a B cell with a distinct repertoire, and that entrant then expands in the GC.
- B cells infected with KSHV and MHV68 exhibit a bias towards Ig lambda light chain expression. The high depth analysis of Zelazowska et al. [88] captured clones in the process of Igκ to Igλ switching, and is supported by observations of a skew in lambda light chains of GC B cells by Collins et al. [89]. This complements observations of dual Igκ+ Igλ+ tonsillar cells upon new KSHV infection with concomitant induction of the expression of RAG1/2 recombinase [87]. We propose that rhadinoviruses drive receptor editing in the periphery.
- The Ig of MHV68-infected cells demonstrates SHM [88], consistent with SHM observed for GHV+ PEL and EBV+ B cells in the periphery.
- MHV68+ B cells undergo isotype class switching in the GC [88].
- The differentiation of a memory B cell to PC leads to infectious particle production. BCR cross-linking of surface Ig mimics a memory B cell that encounters its cognate antigen to cue terminal differentiation to a plasma cell. Cross-linking the BCR drives the reactivation of EBV, KSHV, and MHV68 in cell culture [159,160,161,164]. Loss of factors that drive plasma cell differentiation reduces MHV68 reactivation from the splenic reservoir in vivo [162,163,166].
5.2. Implications of Ig Repertoire Bias
5.2.1. The Impact of Bias on Chronic Infection
5.2.2. BCR and Autoimmunity and Other Distractions
5.2.3. Cancer
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Li, H.; Cunha, C.W.; Taus, N.S.; Knowles, D.P. Malignant catarrhal fever: Inching toward understanding. Annu. Rev. Anim. Biosci. 2014, 2, 209–233. [Google Scholar] [CrossRef]
- Mistrikova, J.; Briestenska, K. Murid herpesvirus 4 (MuHV-4, prototype strain MHV-68) as an important model in global research of human oncogenic gammaherpesviruses. Acta Virol. 2020, 64, 167–176. [Google Scholar] [CrossRef] [Green Version]
- Mühe, J.; Wang, F. Non-human Primate Lymphocryptoviruses: Past, Present, and Future. In Epstein Barr Virus Volume 2: One Herpes Virus: Many Diseases; Münz, C., Ed.; Springer International Publishing: Cham, Switzerland, 2015; pp. 385–405. [Google Scholar] [CrossRef]
- Fleckenstein, B.; Ensser, A. Gammaherpesviruses of New World primates. In Human Herpesviruses: Biology, Therapy, and Immunoprophylaxis; Arvin, A., Campadelli-Fiume, G., Mocarski, E., Eds.; Cambridge University Press: Cambridge, UK, 2007. [Google Scholar]
- Rosenwirth, B.; Kondova, I.; Niphuis, H.; Greenwood, E.J.; Schmidt, F.; Verschoor, E.J.; Wittmann, S.; Heeney, J.L.; Bogers, W.M.; Fickenscher, H.; et al. Herpesvirus saimiri infection of rhesus macaques: A model for acute rhadinovirus-induced t-cell transformation and oncogenesis. J. Med. Virol. 2011, 83, 1938–1950. [Google Scholar] [CrossRef]
- Burkitt, D.; Wright, D.H. A Lymphoma Syndrome in Tropical Africa with a Note on Histology, Cytology, and Histochemistry. Int. Rev. Exp. Pathol. 1963, 2, 67–138. [Google Scholar]
- Burkitt, D.P. Etiology of Burkitt’s lymphoma--an alternative hypothesis to a vectored virus. J. Natl. Cancer Inst. 1969, 42, 19–28. [Google Scholar] [PubMed]
- Epstein, A. Why and How Epstein-Barr Virus Was Discovered 50 Years Ago. Curr. Top. Microbiol. Immunol. 2015, 390, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Henle, W.; Henle, G. Epidemiologic aspects of Epstein-Barr virus (EBV)-associated diseases. Ann. N. Y. Acad. Sci. 1980, 354, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Thorley-Lawson, D.A. EBV Persistence--Introducing the Virus. Curr. Top. Microbiol. Immunol. 2015, 390, 151–209. [Google Scholar] [CrossRef] [Green Version]
- Shannon-Lowe, C.; Rickinson, A.B.; Bell, A.I. Epstein-Barr virus-associated lymphomas. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2017, 372, 20160271. [Google Scholar] [CrossRef]
- Centers for Disease, C. Kaposi’s sarcoma and Pneumocystis pneumonia among homosexual men--New York City and California. Morb. Mortal. Wkly. Rep. 1981, 30, 305–308. [Google Scholar]
- Chang, Y.; Cesarman, E.; Pessin, M.S.; Lee, F.; Culpepper, J.; Knowles, D.M.; Moore, P.S. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi’s sarcoma. Science 1994, 266, 1865–1869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cesarman, E.; Chang, Y.; Moore, P.S.; Said, J.W.; Knowles, D.M. Kaposi’s sarcoma-associated herpesvirus-like DNA sequences in AIDS-related body-cavity-based lymphomas. N. Engl. J. Med. 1995, 332, 1186–1191. [Google Scholar] [CrossRef] [PubMed]
- Cesarman, E. Gammaherpesviruses and lymphoproliferative disorders. Annu. Rev. Pathol. 2014, 9, 349–372. [Google Scholar] [CrossRef]
- Cesarman, E.; Damania, B.; Krown, S.E.; Martin, J.; Bower, M.; Whitby, D. Kaposi sarcoma. Nat. Rev. Dis. Primers 2019, 5, 9. [Google Scholar] [CrossRef] [PubMed]
- Minhas, V.; Wood, C. Epidemiology and transmission of Kaposi’s sarcoma-associated herpesvirus. Viruses 2014, 6, 4178–4194. [Google Scholar] [CrossRef] [Green Version]
- Chagas, C.A.; Endo, L.H.; Sakano, E.; Pinto, G.A.; Brousset, P.; Vassallo, J. Detection of herpesvirus type 8 (HHV8) in children’s tonsils and adenoids by immunohistochemistry and in situ hybridization. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 65–72. [Google Scholar] [CrossRef]
- Fatahzadeh, M.; Schwartz, R.A. Oral Kaposi’s sarcoma: A review and update. Int. J. Dermatol. 2013, 52, 666–672. [Google Scholar] [CrossRef]
- Uldrick, T.S.; Wang, V.; O’Mahony, D.; Aleman, K.; Wyvill, K.M.; Marshall, V.; Steinberg, S.M.; Pittaluga, S.; Maric, I.; Whitby, D.; et al. An interleukin-6-related systemic inflammatory syndrome in patients co-infected with Kaposi sarcoma-associated herpesvirus and HIV but without Multicentric Castleman disease. Clin. Infect. Dis. 2010, 51, 350–358. [Google Scholar] [CrossRef] [Green Version]
- Dupin, N.; Diss, T.L.; Kellam, P.; Tulliez, M.; Du, M.Q.; Sicard, D.; Weiss, R.A.; Isaacson, P.G.; Boshoff, C. HHV-8 is associated with a plasmablastic variant of Castleman disease that is linked to HHV-8-positive plasmablastic lymphoma. Blood 2000, 95, 1406–1412. [Google Scholar] [CrossRef]
- Du, M.Q.; Liu, H.; Diss, T.C.; Ye, H.; Hamoudi, R.A.; Dupin, N.; Meignin, V.; Oksenhendler, E.; Boshoff, C.; Isaacson, P.G. Kaposi sarcoma-associated herpesvirus infects monotypic (IgM lambda) but polyclonal naive B cells in Castleman disease and associated lymphoproliferative disorders. Blood 2001, 97, 2130–2136. [Google Scholar] [CrossRef]
- Chadburn, A.; Hyjek, E.M.; Tam, W.; Liu, Y.; Rengifo, T.; Cesarman, E.; Knowles, D.M. Immunophenotypic analysis of the Kaposi sarcoma herpesvirus (KSHV.; HHV-8)-infected B cells in HIV+ multicentric Castleman disease (MCD). Histopathology 2008, 53, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Fais, F.; Gaidano, G.; Capello, D.; Gloghini, A.; Ghiotto, F.; Roncella, S.; Carbone, A.; Chiorazzi, N.; Ferrarini, M. Immunoglobulin V region gene use and structure suggest antigen selection in AIDS-related primary effusion lymphomas. Leukemia 1999, 13, 1093–1099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matolcsy, A.; Nador, R.G.; Cesarman, E.; Knowles, D.M. Immunoglobulin VH gene mutational analysis suggests that primary effusion lymphomas derive from different stages of B cell maturation. Am. J. Pathol. 1998, 153, 1609–1614. [Google Scholar] [CrossRef] [Green Version]
- Sunil-Chandra, N.P.; Arno, J.; Fazakerley, J.; Nash, A.A. Lymphoproliferative disease in mice infected with murine gammaherpesvirus 68. Am. J. Pathol. 1994, 145, 818–826. [Google Scholar]
- Francois, S.; Vidick, S.; Sarlet, M.; Michaux, J.; Koteja, P.; Desmecht, D.; Stevenson, P.G.; Vanderplasschen, A.; Gillet, L. Comparative study of murid gammaherpesvirus 4 infection in mice and in a natural host, bank voles. J. Gen. Virol. 2010, 91, 2553–2563. [Google Scholar] [CrossRef]
- François, S.; Vidick, S.; Sarlet, M.; Desmecht, D.; Drion, P.; Stevenson, P.G.; Vanderplasschen, A.; Gillet, L. Illumination of Murine Gammaherpesvirus-68 Cycle Reveals a Sexual Transmission Route from Females to Males in Laboratory Mice. PLoS Pathog. 2013, 9, e1003292. [Google Scholar] [CrossRef]
- Gaspar, M.; May, J.S.; Sukla, S.; Frederico, B.; Gill, M.B.; Smith, C.M.; Belz, G.T.; Stevenson, P.G. Murid herpesvirus-4 exploits dendritic cells to infect B cells. PLoS Pathog. 2011, 7, e1002346. [Google Scholar] [CrossRef] [Green Version]
- Weck, K.E.; Barkon, M.L.; Yoo, L.I.; Speck, S.H.; Virgin Hw, I.V. Mature B cells are required for acute splenic infection, but not for establishment of latency, by murine gammaherpesvirus 68. J. Virol. 1996, 70, 6775–6780. [Google Scholar] [CrossRef] [Green Version]
- Marques, S.; Efstathiou, S.; Smith, K.G.; Haury, M.; Simas, J.P. Selective Gene Expression of Latent Murine Gammaherpesvirus 68 in B Lymphocytes. J. Virol. 2003, 77, 7308–7318. [Google Scholar] [CrossRef] [Green Version]
- Willer, D.O.; Speck, S.H. Long-term latent murine Gammaherpesvirus 68 infection is preferentially found within the surface immunoglobulin D-negative subset of splenic B cells in vivo. J. Virol. 2003, 77, 8310–8321. [Google Scholar] [CrossRef] [Green Version]
- Kim, I.J.; Flaño, E.; Woodland, D.L.; Lund, F.E.; Randall, T.D.; Blackman, M.A. Maintenance of long term gamma-herpesvirus B cell latency is dependent on CD40-mediated development of memory B cells. J. Immunol. 2003, 171, 886–892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nealy, M.S.; Coleman, C.B.; Li, H.; Tibbetts, S.A. Use of a virus-encoded enzymatic marker reveals that a stable fraction of memory B cells expresses latency-associated nuclear antigen throughout chronic gammaherpesvirus infection. J. Virol. 2010, 84, 7523–7534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coleman, C.B.; McGraw, J.E.; Feldman, E.R.; Roth, A.N.; Keyes, L.R.; Grau, K.R.; Cochran, S.L.; Waldschmidt, T.J.; Liang, C.; Forrest, J.C.; et al. A gammaherpesvirus Bcl-2 ortholog blocks B cell receptor-mediated apoptosis and promotes the survival of developing B cells in vivo. PLoS Pathog. 2014, 10, e1003916. [Google Scholar] [CrossRef] [PubMed]
- Frederico, B.; Chao, B.; May, J.S.; Belz, G.T.; Stevenson, P.G. A murid gamma-herpesviruses exploits normal splenic immune communication routes for systemic spread. Cell Host Microbe 2014, 15, 457–470. [Google Scholar] [CrossRef] [Green Version]
- Johnson, K.E.; Tarakanova, V.L. Gammaherpesviruses and B Cells: A Relationship That Lasts a Lifetime. Viral. Immunol. 2020, 33, 316–326. [Google Scholar] [CrossRef]
- Tarakanova, V.L.; Suarez, F.; Tibbetts, S.A.; Jacoby, M.A.; Weck, K.E.; Hess, J.L.; Speck, S.H.; Virgin, H.W.T. Murine gammaherpesvirus 68 infection is associated with lymphoproliferative disease and lymphoma in BALB beta2 microglobulin-deficient mice. J. Virol. 2005, 79, 14668–14679. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.S.; Groshong, S.D.; Cool, C.D.; Kleinschmidt-DeMasters, B.K.; van Dyk, L.F. Murine gammaherpesvirus 68 infection of IFNgamma unresponsive mice: A small animal model for gammaherpesvirus-associated B-cell lymphoproliferative disease. Cancer Res. 2009, 69, 5481–5489. [Google Scholar] [CrossRef] [Green Version]
- Liang, X.; Paden, C.R.; Morales, F.M.; Powers, R.P.; Jacob, J.; Speck, S.H. Murine gamma-herpesvirus immortalization of fetal liver-derived B cells requires both the viral cyclin D homolog and latency-associated nuclear antigen. PLoS Pathog. 2011, 7, e1002220. [Google Scholar] [CrossRef] [Green Version]
- Jung, D.; Giallourakis, C.; Mostoslavsky, R.; Alt, F.W. Mechanism and control of V(D)J recombination at the immunoglobulin heavy chain locus. Annu. Rev. Immunol. 2006, 24, 541–570. [Google Scholar] [CrossRef] [Green Version]
- Schatz, D.G.; Swanson, P.C. V(D)J recombination: Mechanisms of initiation. Annu. Rev. Genet. 2011, 45, 167–202. [Google Scholar] [CrossRef] [Green Version]
- Di Noia, J.M.; Neuberger, M.S. Molecular mechanisms of antibody somatic hypermutation. Annu. Rev. Biochem. 2007, 76, 1–22. [Google Scholar] [CrossRef] [PubMed]
- De Silva, N.S.; Klein, U. Dynamics of B cells in germinal centres. Nat. Rev. Immunol. 2015, 15, 137–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Victora, G.D.; Nussenzweig, M.C. Germinal centers. Annu. Rev. Immunol. 2012, 30, 429–457. [Google Scholar] [CrossRef] [PubMed]
- Mesin, L.; Ersching, J.; Victora, G.D. Germinal Center B Cell Dynamics. Immunity 2016, 45, 471–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shlomchik, M.J.; Weisel, F. Germinal center selection and the development of memory B and plasma cells. Immunol. Rev. 2012, 247, 52–63. [Google Scholar] [CrossRef]
- Methot, S.P.; Di Noia, J.M. Molecular Mechanisms of Somatic Hypermutation and Class Switch Recombination. Adv. Immunol. 2017, 133, 37–87. [Google Scholar] [CrossRef]
- Stavnezer, J.; Guikema, J.E.; Schrader, C.E. Mechanism and regulation of class switch recombination. Annu. Rev. Immunol. 2008, 26, 261–292. [Google Scholar] [CrossRef] [Green Version]
- Kuppers, R. Mechanisms of B-cell lymphoma pathogenesis. Nat. Rev. Cancer 2005, 5, 251–262. [Google Scholar] [CrossRef]
- Robbiani, D.F.; Nussenzweig, M.C. Chromosome translocation, B cell lymphoma, and activation-induced cytidine deaminase. Annu. Rev. Pathol. 2013, 8, 79–103. [Google Scholar] [CrossRef]
- Alt, F.W.; Zhang, Y.; Meng, F.L.; Guo, C.; Schwer, B. Mechanisms of programmed DNA lesions and genomic instability in the immune system. Cell 2013, 152, 417–429. [Google Scholar] [CrossRef] [Green Version]
- Ramiro, A.R.; Jankovic, M.; Eisenreich, T.; Difilippantonio, S.; Chen-Kiang, S.; Muramatsu, M.; Honjo, T.; Nussenzweig, A.; Nussenzweig, M.C. AID is required for c-myc/IgH chromosome translocations in vivo. Cell 2004, 118, 431–438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robbiani, D.F.; Bothmer, A.; Callen, E.; Reina-San-Martin, B.; Dorsett, Y.; Difilippantonio, S.; Bolland, D.J.; Chen, H.T.; Corcoran, A.E.; Nussenzweig, A.; et al. AID is required for the chromosomal breaks in c-myc that lead to c-myc/IgH translocations. Cell 2008, 135, 1028–1038. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.; Duke, J.L.; Richter, D.J.; Vinuesa, C.G.; Goodnow, C.C.; Kleinstein, S.H.; Schatz, D.G. Two levels of protection for the B cell genome during somatic hypermutation. Nature 2008, 451, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Klein, I.A.; Resch, W.; Jankovic, M.; Oliveira, T.; Yamane, A.; Nakahashi, H.; Di Virgilio, M.; Bothmer, A.; Nussenzweig, A.; Robbiani, D.F.; et al. Translocation-capture sequencing reveals the extent and nature of chromosomal rearrangements in B lymphocytes. Cell 2011, 147, 95–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiarle, R.; Zhang, Y.; Frock, R.L.; Lewis, S.M.; Molinie, B.; Ho, Y.J.; Myers, D.R.; Choi, V.W.; Compagno, M.; Malkin, D.J.; et al. Genome-wide Translocation Sequencing Reveals Mechanisms of Chromosome Breaks and Rearrangements in B Cells. Cell 2011, 147, 107–119. [Google Scholar] [CrossRef] [Green Version]
- Casellas, R.; Basu, U.; Yewdell, W.T.; Chaudhuri, J.; Robbiani, D.F.; Di Noia, J.M. Mutations, kataegis and translocations in B cells: Understanding AID promiscuous activity. Nat. Rev. Immunol. 2016, 16, 164–176. [Google Scholar] [CrossRef] [Green Version]
- Muto, T.; Okazaki, I.M.; Yamada, S.; Tanaka, Y.; Kinoshita, K.; Muramatsu, M.; Nagaoka, H.; Honjo, T. Negative regulation of activation-induced cytidine deaminase in B cells. Proc. Natl. Acad. Sci. USA 2006, 103, 2752–2757. [Google Scholar] [CrossRef] [Green Version]
- Dorsett, Y.; McBride, K.M.; Jankovic, M.; Gazumyan, A.; Thai, T.H.; Robbiani, D.F.; Di Virgilio, M.; Reina San-Martin, B.; Heidkamp, G.; Schwickert, T.A.; et al. MicroRNA-155 suppresses activation-induced cytidine deaminase-mediated Myc-Igh translocation. Immunity 2008, 28, 630–638. [Google Scholar] [CrossRef] [Green Version]
- Takizawa, M.; Tolarova, H.; Li, Z.; Dubois, W.; Lim, S.; Callen, E.; Franco, S.; Mosaico, M.; Feigenbaum, L.; Alt, F.W.; et al. AID expression levels determine the extent of cMyc oncogenic translocations and the incidence of B cell tumor development. J. Exp. Med. 2008, 205, 1949–1957. [Google Scholar] [CrossRef] [Green Version]
- Mu, Y.; Zelazowska, M.A.; McBride, K.M. Phosphorylation promotes activation-induced cytidine deaminase activity at the Myc oncogene. J. Exp. Med. 2017, 214, 3543–3552. [Google Scholar] [CrossRef]
- Gazumyan, A.; Timachova, K.; Yuen, G.; Siden, E.; Di Virgilio, M.; Woo, E.M.; Chait, B.T.; Reina San-Martin, B.; Nussenzweig, M.C.; McBride, K.M. Amino-terminal phosphorylation of activation-induced cytidine deaminase suppresses c-myc/IgH translocation. Mol. Cell. Biol. 2011, 31, 442–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luning Prak, E.T.; Monestier, M.; Eisenberg, R.A. B cell receptor editing in tolerance and autoimmunity. Ann. N. Y. Acad. Sci. 2011, 1217, 96–121. [Google Scholar] [CrossRef]
- Haughton, G.; Lanier, L.L.; Babcock, G.F. The murine kappa light chain shift. Nature 1978, 275, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Brauninger, A.; Goossens, T.; Rajewsky, K.; Kuppers, R. Regulation of immunoglobulin light chain gene rearrangements during early B cell development in the human. Eur. J. Immunol. 2001, 31, 3631–3637. [Google Scholar] [CrossRef]
- Yin, H.; Qu, J.; Peng, Q.; Gan, R. Molecular mechanisms of EBV-driven cell cycle progression and oncogenesis. Med. Microbiol. Immunol. 2019, 208, 573–583. [Google Scholar] [CrossRef] [Green Version]
- Cen, O.; Longnecker, R. Latent Membrane Protein 2 (LMP2). Curr. Top. Microbiol. Immunol. 2015, 391, 151–180. [Google Scholar] [CrossRef]
- Kieser, A.; Sterz, K.R. The Latent Membrane Protein 1 (LMP1). Curr. Top. Microbiol. Immunol. 2015, 391, 119–149. [Google Scholar] [CrossRef]
- Saha, A.; Robertson, E.S. Mechanisms of B-Cell Oncogenesis Induced by Epstein-Barr Virus. J. Virol. 2019, 93. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J.I. Herpesvirus latency. J. Clin. Investig. 2020, 130. [Google Scholar] [CrossRef]
- Allday, M.J.; Bazot, Q.; White, R.E. The EBNA3 Family: Two Oncoproteins and a Tumour Suppressor that Are Central to the Biology of EBV in B Cells. In Epstein Barr Virus Volume 2: One Herpes Virus: Many Diseases; Münz, C., Ed.; Springer International Publishing: Cham, Switzerland, 2015; pp. 61–117. [Google Scholar] [CrossRef]
- Pich, D.; Mrozek-Gorska, P.; Bouvet, M.; Sugimoto, A.; Akidil, E.; Grundhoff, A.; Hamperl, S.; Ling, P.D.; Hammerschmidt, W. First Days in the Life of Naive Human B Lymphocytes Infected with Epstein-Barr Virus. mBio 2019, 10. [Google Scholar] [CrossRef] [Green Version]
- Price, A.M.; Luftig, M.A. To be or not IIb: A multi-step process for Epstein-Barr virus latency establishment and consequences for B cell tumorigenesis. PLoS Pathog. 2015, 11, e1004656. [Google Scholar] [CrossRef] [PubMed]
- Mrozek-Gorska, P.; Buschle, A.; Pich, D.; Schwarzmayr, T.; Fechtner, R.; Scialdone, A.; Hammerschmidt, W. Epstein-Barr virus reprograms human B lymphocytes immediately in the prelatent phase of infection. Proc. Natl. Acad. Sci. USA 2019, 116, 16046–16055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.W.; Shen, H.; Nobre, L.; Ersing, I.; Paulo, J.A.; Trudeau, S.; Wang, Z.; Smith, N.A.; Ma, Y.; Reinstadler, B.; et al. Epstein-Barr-Virus-Induced One-Carbon Metabolism Drives B Cell Transformation. Cell Metab. 2019, 30, 539–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szymula, A.; Palermo, R.D.; Bayoumy, A.; Groves, I.J.; Ba Abdullah, M.; Holder, B.; White, R.E. Epstein-Barr virus nuclear antigen EBNA-LP is essential for transforming naive B cells, and facilitates recruitment of transcription factors to the viral genome. PLoS Pathog. 2018, 14, e1006890. [Google Scholar] [CrossRef] [Green Version]
- Siemer, D.; Kurth, J.; Lang, S.; Lehnerdt, G.; Stanelle, J.; Kuppers, R. EBV transformation overrides gene expression patterns of B cell differentiation stages. Mol. Immunol. 2008, 45, 3133–3141. [Google Scholar] [CrossRef]
- Heath, E.; Begue-Pastor, N.; Chaganti, S.; Croom-Carter, D.; Shannon-Lowe, C.; Kube, D.; Feederle, R.; Delecluse, H.J.; Rickinson, A.B.; Bell, A.I. Epstein-Barr virus infection of naive B cells in vitro frequently selects clones with mutated immunoglobulin genotypes: Implications for virus biology. PLoS Pathog. 2012, 8, e1002697. [Google Scholar] [CrossRef] [Green Version]
- Souza, T.A.; Stollar, B.D.; Sullivan, J.L.; Luzuriaga, K.; Thorley-Lawson, D.A. Peripheral B cells latently infected with Epstein-Barr virus display molecular hallmarks of classical antigen-selected memory B cells. Proc. Natl. Acad. Sci. USA 2005, 102, 18093–18098. [Google Scholar] [CrossRef] [Green Version]
- Souza, T.A.; Stollar, B.D.; Sullivan, J.L.; Luzuriaga, K.; Thorley-Lawson, D.A. Influence of EBV on the peripheral blood memory B cell compartment. J. Immunol. 2007, 179, 3153–3160. [Google Scholar] [CrossRef]
- Tracy, S.I.; Kakalacheva, K.; Lunemann, J.D.; Luzuriaga, K.; Middeldorp, J.; Thorley-Lawson, D.A. Persistence of Epstein-Barr virus in self-reactive memory B cells. J. Virol. 2012, 86, 12330–12340. [Google Scholar] [CrossRef] [Green Version]
- Mockridge, C.I.; Rahman, A.; Buchan, S.; Hamblin, T.; Isenberg, D.A.; Stevenson, F.K.; Potter, K.N. Common patterns of B cell perturbation and expanded V4-34 immunoglobulin gene usage in autoimmunity and infection. Autoimmunity 2004, 37, 9–15. [Google Scholar] [CrossRef]
- Bhat, N.M.; Bieber, M.M.; Yang, Y.C.; Leu, Y.S.; van Vollenhoven, R.F.; Teng, N.N. B cell lymphoproliferative disorders and VH4-34 gene encoded antibodies. Hum. Antibodies 2004, 13, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.; Wang, Q.; Lu, Y.; Xu, X.; Xia, Y.; Tu, M.; Liu, Y.; Zhang, Q.; Peng, Y.; Zheng, X. Signatures of B-cell receptor diversity in B lymphocytes following Epstein-Barr virus transformation. Physiol. Genom. 2019, 51, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Hassman, L.M.; Ellison, T.J.; Kedes, D.H. KSHV infects a subset of human tonsillar B cells, driving proliferation and plasmablast differentiation. J. Clin. Investig. 2011, 121, 752–768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Totonchy, J.; Osborn, J.M.; Chadburn, A.; Nabiee, R.; Argueta, L.; Mikita, G.; Cesarman, E. KSHV induces immunoglobulin rearrangements in mature B lymphocytes. PLoS Pathog. 2018, 14, e1006967. [Google Scholar] [CrossRef] [Green Version]
- Zelazowska, M.A.; Dong, Q.; Plummer, J.B.; Zhong, Y.; Liu, B.; Krug, L.T.; McBride, K.M. Gammaherpesvirus-infected germinal center cells express a distinct immunoglobulin repertoire. Life Sci. Alliance 2020, 3. [Google Scholar] [CrossRef]
- Collins, C.M.; Scharer, C.D.; Murphy, T.J.; Boss, J.M.; Speck, S.H. Murine gammaherpesvirus infection is skewed toward Iglambda+ B cells expressing a specific heavy chain V-segment. PLoS Pathog. 2020, 16, e1008438. [Google Scholar] [CrossRef]
- Roughan, J.E.; Thorley-Lawson, D.A. The intersection of Epstein-Barr virus with the germinal center. J. Virol. 2009, 83, 3968–3976. [Google Scholar] [CrossRef] [Green Version]
- Roughan, J.E.; Torgbor, C.; Thorley-Lawson, D.A. Germinal center B cells latently infected with Epstein-Barr virus proliferate extensively but do not increase in number. J. Virol. 2010, 84, 1158–1168. [Google Scholar] [CrossRef] [Green Version]
- Minamitani, T.; Ma, Y.; Zhou, H.; Kida, H.; Tsai, C.Y.; Obana, M.; Okuzaki, D.; Fujio, Y.; Kumanogoh, A.; Zhao, B.; et al. Mouse model of Epstein-Barr virus LMP1-and LMP2A-driven germinal center B-cell lymphoproliferative disease. Proc. Natl. Acad. Sci. USA 2017, 114, 4751–4756. [Google Scholar] [CrossRef] [Green Version]
- Kanzler, H.; Kuppers, R.; Hansmann, M.L.; Rajewsky, K. Hodgkin and Reed-Sternberg cells in Hodgkin’s disease represent the outgrowth of a dominant tumor clone derived from (crippled) germinal center B cells. J. Exp. Med. 1996, 184, 1495–1505. [Google Scholar] [CrossRef]
- Kalchschmidt, J.S.; Bashford-Rogers, R.; Paschos, K.; Gillman, A.C.; Styles, C.T.; Kellam, P.; Allday, M.J. Epstein-Barr virus nuclear protein EBNA3C directly induces expression of AID and somatic mutations in B cells. J. Exp. Med. 2016, 213, 921–928. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.H.; Kim, W.S.; Park, C. Epstein-Barr virus latent membrane protein 1 increases genomic instability through Egr-1-mediated up-regulation of activation-induced cytidine deaminase in B-cell lymphoma. Leuk. Lymphoma 2013, 54, 2035–2040. [Google Scholar] [CrossRef]
- Tobollik, S.; Meyer, L.; Buettner, M.; Klemmer, S.; Kempkes, B.; Kremmer, E.; Niedobitek, G.; Jungnickel, B. Epstein-Barr virus nuclear antigen 2 inhibits AID expression during EBV-driven B-cell growth. Blood 2006, 108, 3859–3864. [Google Scholar] [CrossRef] [PubMed]
- Wilmore, J.R.; Asito, A.S.; Wei, C.; Piriou, E.; Sumba, P.O.; Sanz, I.; Rochford, R. AID expression in peripheral blood of children living in a malaria holoendemic region is associated with changes in B cell subsets and Epstein-Barr virus. Int. J. Cancer 2015, 136, 1371–1380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorley-Lawson, D.; Deitsch, K.W.; Duca, K.A.; Torgbor, C. The Link between Plasmodium falciparum Malaria and Endemic Burkitt’s Lymphoma-New Insight into a 50-Year-Old Enigma. PLoS Pathog. 2016, 12, e1005331. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, J.R.; DeKosky, B.J.; Tanno, H.; Ellington, A.D.; Georgiou, G. Ultra-high-throughput sequencing of the immune receptor repertoire from millions of lymphocytes. Nat. Protoc. 2016, 11, 429–442. [Google Scholar] [CrossRef]
- Torgbor, C.; Awuah, P.; Deitsch, K.; Kalantari, P.; Duca, K.A.; Thorley-Lawson, D.A. A multifactorial role for P. falciparum malaria in endemic Burkitt’s lymphoma pathogenesis. PLoS Pathog. 2014, 10, e1004170. [Google Scholar] [CrossRef] [Green Version]
- Myoung, J.; Ganem, D. Infection of lymphoblastoid cell lines by Kaposi’s sarcoma-associated herpesvirus: Critical role of cell-associated virus. J. Virol. 2011, 85, 9767–9777. [Google Scholar] [CrossRef] [Green Version]
- Nicol, S.M.; Sabbah, S.; Brulois, K.F.; Jung, J.U.; Bell, A.I.; Hislop, A.D. Primary B Lymphocytes Infected with Kaposi’s Sarcoma-Associated Herpesvirus Can Be Expanded In Vitro and Are Recognized by LANA-Specific CD4+ T Cells. J. Virol. 2016, 90, 3849–3859. [Google Scholar] [CrossRef] [Green Version]
- Totonchy, J. Extrafollicular activities: Perspectives on HIV infection, germinal center-independent maturation pathways, and KSHV-mediated lymphoproliferation. Curr. Opin. Virol. 2017, 26, 69–73. [Google Scholar] [CrossRef]
- Ebert, A.; Hill, L.; Busslinger, M. Spatial Regulation of V-(D)J Recombination at Antigen Receptor Loci. Adv. Immunol. 2015, 128, 93–121. [Google Scholar] [CrossRef] [PubMed]
- Kumari, G.; Sen, R. Chromatin Interactions in the Control of Immunoglobulin Heavy Chain Gene Assembly. Adv. Immunol. 2015, 128, 41–92. [Google Scholar] [CrossRef]
- Jenner, R.G.; Maillard, K.; Cattini, N.; Weiss, R.A.; Boshoff, C.; Wooster, R.; Kellam, P. Kaposi’s sarcoma-associated herpesvirus-infected primary effusion lymphoma has a plasma cell gene expression profile. Proc. Natl. Acad. Sci. USA 2003, 100, 10399–10404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ascoli, V.; Signoretti, S.; Onetti-Muda, A.; Pescarmona, E.; Della-Rocca, C.; Nardi, F.; Mastroianni, C.M.; Gastaldi, R.; Pistilli, A.; Gaidano, G.; et al. Primary effusion lymphoma in HIV-infected patients with multicentric Castleman’s disease. J. Pathol. 2001, 193, 200–209. [Google Scholar] [CrossRef]
- Nador, R.G.; Cesarman, E.; Chadburn, A.; Dawson, D.B.; Ansari, M.Q.; Sald, J.; Knowles, D.M. Primary effusion lymphoma: A distinct clinicopathologic entity associated with the Kaposi’s sarcoma-associated herpes virus. Blood 1996, 88, 645–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McHugh, D.; Caduff, N.; Barros, M.H.M.; Ramer, P.C.; Raykova, A.; Murer, A.; Landtwing, V.; Quast, I.; Styles, C.T.; Spohn, M.; et al. Persistent KSHV Infection Increases EBV-Associated Tumor Formation In Vivo via Enhanced EBV Lytic Gene Expression. Cell Host Microbe 2017, 22, 61–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faure, A.; Hayes, M.; Sugden, B. How Kaposi’s sarcoma-associated herpesvirus stably transforms peripheral B cells towards lymphomagenesis. Proc. Natl. Acad. Sci. USA 2019, 116, 16519. [Google Scholar] [CrossRef] [Green Version]
- Bigi, R.; Landis, J.T.; An, H.; Caro-Vegas, C.; Raab-Traub, N.; Dittmer, D.P. Epstein-Barr virus enhances genome maintenance of Kaposi sarcoma-associated herpesvirus. Proc. Natl. Acad. Sci. USA 2018, 115, E11379–E11387. [Google Scholar] [CrossRef] [Green Version]
- Mack, A.A.; Sugden, B. EBV Is Necessary for Proliferation of Dually Infected Primary Effusion Lymphoma Cells. Cancer Res. 2008, 68, 6963. [Google Scholar] [CrossRef] [Green Version]
- Chandriani, S.; Ganem, D. Array-Based Transcript Profiling and Limiting-Dilution Reverse Transcription-PCR Analysis Identify Additional Latent Genes in Kaposi’s Sarcoma-Associated Herpesvirus. J. Virol. 2010, 84, 5565. [Google Scholar] [CrossRef] [Green Version]
- Arias, C.; Weisburd, B.; Stern-Ginossar, N.; Mercier, A.; Madrid, A.S.; Bellare, P.; Holdorf, M.; Weissman, J.S.; Ganem, D. KSHV 2.0: A Comprehensive Annotation of the Kaposi’s Sarcoma-Associated Herpesvirus Genome Using Next-Generation Sequencing Reveals Novel Genomic and Functional Features. PLoS Pathog. 2014, 10, e1003847. [Google Scholar] [CrossRef] [PubMed]
- Wen, K.W.; Damania, B. Kaposi sarcoma-associated herpesvirus (KSHV): Molecular biology and oncogenesis. Cancer Lett. 2010, 289, 140–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fakhari, F.D.; Dittmer, D.P. Charting latency transcripts in Kaposi’s sarcoma-associated herpesvirus by whole-genome real-time quantitative PCR. J. Virol. 2002, 76, 6213–6223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, L.; Majerciak, V.; Zheng, Z.-M.; Lan, K. Towards Better Understanding of KSHV Life Cycle: From Transcription and Posttranscriptional Regulations to Pathogenesis. Virol. Sin. 2019, 34, 135–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fakhari, F.D.; Jeong, J.H.; Kanan, Y.; Dittmer, D.P. The latency-associated nuclear antigen of Kaposi sarcoma-associated herpesvirus induces B cell hyperplasia and lymphoma. J. Clin. Investig. 2006, 116, 735–742. [Google Scholar] [CrossRef] [Green Version]
- Ellis, M.; Chew, Y.P.; Fallis, L.; Freddersdorf, S.; Boshoff, C.; Weiss, R.A.; Lu, X.; Mittnacht, S. Degradation of p27(Kip) cdk inhibitor triggered by Kaposi’s sarcoma virus cyclin-cdk6 complex. EMBO J. 1999, 18, 644–653. [Google Scholar] [CrossRef] [Green Version]
- McCormick, C.; Ganem, D. The kaposin B protein of KSHV activates the p38/MK2 pathway and stabilizes cytokine mRNAs. Science 2005, 307, 739–741. [Google Scholar] [CrossRef]
- Tomlinson, C.C.; Damania, B. Critical role for endocytosis in the regulation of signaling by the Kaposi’s sarcoma-associated herpesvirus K1 protein. J. Virol. 2008, 82, 6514–6523. [Google Scholar] [CrossRef] [Green Version]
- Aoki, Y.; Feldman, G.M.; Tosato, G. Inhibition of STAT3 signaling induces apoptosis and decreases survivin expression in primary effusion lymphoma. Blood 2003, 101, 1535–1542. [Google Scholar] [CrossRef]
- Coscoy, L.; Ganem, D. Kaposi’s sarcoma-associated herpesvirus encodes two proteins that block cell surface display of MHC class I chains by enhancing their endocytosis. Proc. Natl. Acad. Sci. USA 2000, 97, 8051–8056. [Google Scholar] [CrossRef] [Green Version]
- Sanchez, D.J.; Gumperz, J.E.; Ganem, D. Regulation of CD1d expression and function by a herpesvirus infection. J. Clin. Investig. 2005, 115, 1369–1378. [Google Scholar] [CrossRef] [Green Version]
- Bekerman, E.; Jeon, D.; Ardolino, M.; Coscoy, L. A role for host activation-induced cytidine deaminase in innate immune defense against KSHV. PLoS Pathog. 2013, 9, e1003748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sin, S.H.; Dittmer, D.P. Viral latency locus augments B-cell response in vivo to induce chronic marginal zone enlargement, plasma cell hyperplasia, and lymphoma. Blood 2013, 121, 2952–2963. [Google Scholar] [CrossRef] [Green Version]
- Boss, I.W.; Nadeau, P.E.; Abbott, J.R.; Yang, Y.; Mergia, A.; Renne, R. A Kaposi’s sarcoma-associated herpesvirus-encoded ortholog of microRNA miR-155 induces human splenic B-cell expansion in NOD/LtSz-scid IL2Rgammanull mice. J. Virol. 2011, 85, 9877–9886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dahlke, C.; Maul, K.; Christalla, T.; Walz, N.; Schult, P.; Stocking, C.; Grundhoff, A. A microRNA encoded by Kaposi sarcoma-associated herpesvirus promotes B-cell expansion in vivo. PLoS ONE 2012, 7, e49435. [Google Scholar] [CrossRef] [Green Version]
- Sin, S.H.; Kim, Y.B.; Dittmer, D.P. Latency locus complements MicroRNA 155 deficiency in vivo. J. Virol. 2013, 87, 11908–11911. [Google Scholar] [CrossRef] [Green Version]
- Dittmer, D.P.; Damania, B.; Sin, S.H. Animal models of tumorigenic herpesviruses—An update. Curr. Opin. Virol. 2015, 14, 145–150. [Google Scholar] [CrossRef] [Green Version]
- Bravo Cruz, A.G.; Damania, B. In Vivo Models of Oncoproteins Encoded by Kaposi’s Sarcoma-Associated Herpesvirus. J. Virol. 2019, 93. [Google Scholar] [CrossRef] [Green Version]
- Merchant, M.; Longnecker, R. LMP2A survival and developmental signals are transmitted through Btk-dependent and Btk-independent pathways. Virology 2001, 291, 46–54. [Google Scholar] [CrossRef] [Green Version]
- Sin, S.-H.; Kang, S.A.; Kim, Y.; Eason, A.; Tan, K.; An, H.; Dittmer, D.P. Kaposi’s Sarcoma-Associated Herpesvirus Latency Locus Compensates for Interleukin-6 in Initial B Cell Activation. J. Virol. 2016, 90, 2150. [Google Scholar] [CrossRef] [Green Version]
- Minamitani, T.; Yasui, T.; Ma, Y.; Zhou, H.; Okuzaki, D.; Tsai, C.-Y.; Sakakibara, S.; Gewurz, B.E.; Kieff, E.; Kikutani, H. Evasion of affinity-based selection in germinal centers by Epstein–Barr virus LMP2A. Proc. Natl. Acad. Sci. USA 2015, 112, 11612. [Google Scholar] [CrossRef] [Green Version]
- Vrazo, A.C.; Chauchard, M.; Raab-Traub, N.; Longnecker, R. Epstein-Barr Virus LMP2A Reduces Hyperactivation Induced by LMP1 to Restore Normal B Cell Phenotype in Transgenic Mice. PLoS Pathog. 2012, 8, e1002662. [Google Scholar] [CrossRef] [Green Version]
- Sin, S.H.; Eason, A.B.; Bigi, R.; Kim, Y.; Kang, S.; Tan, K.; Seltzer, T.A.; Venkataramanan, R.; An, H.; Dittmer, D.P. Kaposi’s Sarcoma-Associated Herpesvirus Latency Locus Renders B Cells Hyperresponsive to Secondary Infections. J. Virol. 2018, 92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ballon, G.; Chen, K.; Perez, R.; Tam, W.; Cesarman, E. Kaposi sarcoma herpesvirus (KSHV) vFLIP oncoprotein induces B cell transdifferentiation and tumorigenesis in mice. J. Clin. Investig. 2011, 121, 1141–1153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marshall, V.A.; Labo, N.; Hao, X.-P.; Holdridge, B.; Thompson, M.; Miley, W.; Brands, C.; Coalter, V.; Kiser, R.; Anver, M.; et al. Gammaherpesvirus infection and malignant disease in rhesus macaques experimentally infected with SIV or SHIV. PLoS Pathog. 2018, 14, e1007130. [Google Scholar] [CrossRef] [PubMed]
- Bielefeldt-Ohmann, H.; Bruce, A.G.; Howard, K.; Ikoma, M.; Thouless, M.E.; Rose, T.M. Macaque homologs of Kaposi’s sarcoma-associated herpesvirus (KSHV) infect germinal center lymphoid cells, epithelial cells in skin and gastrointestinal tract and gonadal germ cells in naturally infected macaques. Virology 2018, 519, 106–120. [Google Scholar] [CrossRef]
- Estep, R.D.; Wong, S.W. Rhesus macaque rhadinovirus-associated disease. Curr. Opin. Virol. 2013, 3, 245–250. [Google Scholar] [CrossRef] [Green Version]
- Fujiwara, S.; Nakamura, H. Animal Models for Gammaherpesvirus Infections: Recent Development in the Analysis of Virus-Induced Pathogenesis. Pathogens 2020, 9, 116. [Google Scholar] [CrossRef] [Green Version]
- Speck, S.H.; Ganem, D. Viral latency and its regulation: Lessons from the gamma-herpesviruses. Cell Host Microbe 2010, 8, 100–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barton, E.; Mandal, P.; Speck, S.H. Pathogenesis and host control of gammaherpesviruses: Lessons from the mouse. Annu. Rev. Immunol. 2011, 29, 351–397. [Google Scholar] [CrossRef]
- Siegel, A.M.; Herskowitz, J.H.; Speck, S.H. The MHV68 M2 protein drives IL-10 dependent B cell proliferation and differentiation. PLoS Pathog. 2008, 4, e1000039. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Zhu, L.; Lu, X.; Feldman, E.R.; Keyes, L.R.; Wang, Y.; Fan, H.; Feng, H.; Xia, Z.; Sun, J.; et al. Recombinant Murine Gamma Herpesvirus 68 Carrying KSHV G Protein-Coupled Receptor Induces Angiogenic Lesions in Mice. PLoS Pathog. 2015, 11, e1005001. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.S.; Suarez, A.L.; Claypool, D.J.; Armstrong, T.K.; Buckingham, E.M.; van Dyk, L.F. Viral Cyclins Mediate Separate Phases of Infection by Integrating Functions of Distinct Mammalian Cyclins. PLoS Pathog. 2012, 8, e1002496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffman, B.A.; Wang, Y.; Feldman, E.R.; Tibbetts, S.A. Epstein-Barr virus EBER1 and murine gammaherpesvirus TMER4 share conserved in vivo function to promote B cell egress and dissemination. Proc. Natl. Acad. Sci. USA 2019, 116, 25392–25394. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Oldenburg, D.G.; Salinas, E.; White, D.W.; Forrest, J.C. Murine Gammaherpesvirus 68 Expressing Kaposi Sarcoma-Associated Herpesvirus Latency-Associated Nuclear Antigen (LANA) Reveals both Functional Conservation and Divergence in LANA Homologs. J. Virol. 2017, 91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pires de Miranda, M.; Quendera, A.P.; McVey, C.E.; Kaye, K.M.; Simas, J.P. In Vivo Persistence of Chimeric Virus after Substitution of the Kaposi’s Sarcoma-Associated Herpesvirus LANA DNA Binding Domain with That of Murid Herpesvirus 4. J. Virol. 2018, 92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gujer, C.; Chatterjee, B.; Landtwing, V.; Raykova, A.; McHugh, D.; Munz, C. Animal models of Epstein Barr virus infection. Curr. Opin. Virol. 2015, 13, 6–10. [Google Scholar] [CrossRef]
- Munz, C. Humanized mouse models for Epstein Barr virus infection. Curr. Opin. Virol. 2017, 25, 113–118. [Google Scholar] [CrossRef] [Green Version]
- Milho, R.; Smith, C.M.; Marques, S.; Alenquer, M.; May, J.S.; Gillet, L.; Gaspar, M.; Efstathiou, S.; Simas, J.P.; Stevenson, P.G. In vivo imaging of murid herpesvirus-4 infection. J. Gen. Virol. 2009, 90, 21–32. [Google Scholar] [CrossRef]
- Hwang, S.; Wu, T.T.; Tong, L.M.; Kim, K.S.; Martinez-Guzman, D.; Colantonio, A.D.; Uittenbogaart, C.H.; Sun, R. Persistent gammaherpesvirus replication and dynamic interaction with the host in vivo. J. Virol. 2008, 82, 12498–12509. [Google Scholar] [CrossRef] [Green Version]
- Frederico, B.; Milho, R.; May, J.S.; Gillet, L.; Stevenson, P.G. Myeloid infection links epithelial and B cell tropisms of Murid Herpesvirus-4. PLoS Pathog. 2012, 8, e1002935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lawler, C.; de Miranda, M.P.; May, J.; Wyer, O.; Simas, J.P.; Stevenson, P.G. Gammaherpesvirus Colonization of the Spleen Requires Lytic Replication in B Cells. J. Virol. 2018, 92. [Google Scholar] [CrossRef] [Green Version]
- Collins, C.M.; Boss, J.M.; Speck, S.H. Identification of infected B-cell populations by using a recombinant murine gammaherpesvirus 68 expressing a fluorescent protein. J. Virol. 2009, 83, 6484–6493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowden, R.J.; Simas, J.P.; Davis, A.J.; Efstathiou, S. Murine gammaherpesvirus 68 encodes tRNA-like sequences which are expressed during latency. J. Gen. Virol. 1997, 78 Pt 7, 1675–1687. [Google Scholar] [CrossRef]
- Collins, C.M.; Speck, S.H. Tracking murine gammaherpesvirus 68 infection of germinal center B cells in vivo. PLoS ONE 2012, 7, e33230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kati, S.; Tsao, E.H.; Gunther, T.; Weidner-Glunde, M.; Rothamel, T.; Grundhoff, A.; Kellam, P.; Schulz, T.F. Activation of the B cell antigen receptor triggers reactivation of latent Kaposi’s sarcoma-associated herpesvirus in B cells. J. Virol. 2013, 87, 8004–8016. [Google Scholar] [CrossRef] [Green Version]
- Moser, J.M.; Upton, J.W.; Gray, K.S.; Speck, S.H. Ex vivo stimulation of B cells latently infected with gammaherpesvirus 68 triggers reactivation from latency. J. Virol. 2005, 79, 5227–5231. [Google Scholar] [CrossRef] [Green Version]
- Liang, X.; Collins, C.M.; Mendel, J.B.; Iwakoshi, N.N.; Speck, S.H. Gammaherpesvirus-driven plasma cell differentiation regulates virus reactivation from latently infected B lymphocytes. PLoS Pathog. 2009, 5, e1000677. [Google Scholar] [CrossRef] [Green Version]
- Siegel, A.M.; Rangaswamy, U.S.; Napier, R.J.; Speck, S.H. Blimp-1-dependent plasma cell differentiation is required for efficient maintenance of murine gammaherpesvirus latency and antiviral antibody responses. J. Virol. 2010, 84, 674–685. [Google Scholar] [CrossRef] [Green Version]
- Terrell, S.; Speck, S.H. Murine gammaherpesvirus M2 antigen modulates splenic B cell activation and terminal differentiation in vivo. PLoS Pathog. 2017, 13, e1006543. [Google Scholar] [CrossRef] [Green Version]
- Kenney, S.C.; Mertz, J.E. Regulation of the latent-lytic switch in Epstein-Barr virus. Semin. Cancer Biol. 2014, 26, 60–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, S.J.; Tsao, E.H.; Webb, B.L.; Ye, H.; Dalton-Griffin, L.; Tsantoulas, C.; Gale, C.V.; Du, M.Q.; Whitehouse, A.; Kellam, P. X box binding protein XBP-1s transactivates the Kaposi’s sarcoma-associated herpesvirus (KSHV) ORF50 promoter, linking plasma cell differentiation to KSHV reactivation from latency. J. Virol. 2007, 81, 13578–13586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matar, C.G.; Rangaswamy, U.S.; Wakeman, B.S.; Iwakoshi, N.; Speck, S.H. Murine gammaherpesvirus 68 reactivation from B cells requires IRF4 but not XBP-1. J. Virol. 2014, 88, 11600–11610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cieniewicz, B.; Santana, A.L.; Minkah, N.; Krug, L.T. Interplay of Murine Gammaherpesvirus 68 with NF-kappaB Signaling of the Host. Front. Microbiol. 2016, 7, 1202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reddy, S.S.; Foreman, H.C.; Sioux, T.O.; Park, G.H.; Poli, V.; Reich, N.C.; Krug, L.T. Ablation of STAT3 in the B Cell Compartment Restricts Gammaherpesvirus Latency In Vivo. mBio 2016, 7. [Google Scholar] [CrossRef] [Green Version]
- Moser, J.M.; Upton, J.W.; Allen, R.D., III; Wilson, C.B.; Speck, S.H. Role of B-cell proliferation in the establishment of gammaherpesvirus latency. J. Virol. 2005, 79, 9480–9491. [Google Scholar] [CrossRef] [Green Version]
- Collins, C.M.; Speck, S.H. Interleukin 21 signaling in B cells is required for efficient establishment of murine gammaherpesvirus latency. PLoS Pathog. 2015, 11, e1004831. [Google Scholar] [CrossRef]
- Collins, C.M.; Speck, S.H. Expansion of murine gammaherpesvirus latently infected B cells requires T follicular help. PLoS Pathog. 2014, 10, e1004106. [Google Scholar] [CrossRef] [Green Version]
- Jondle, C.N.; Johnson, K.E.; Uitenbroek, A.A.; Sylvester, P.A.; Nguyen, C.; Cui, W.; Tarakanova, V.L. B Cell-Intrinsic Expression of Interferon Regulatory Factor 1 Supports Chronic Murine Gammaherpesvirus 68 Infection. J. Virol. 2020, 94. [Google Scholar] [CrossRef]
- Johnson, K.E.; Lange, P.T.; Jondle, C.N.; Volberding, P.J.; Lorenz, U.M.; Cui, W.; Dittel, B.N.; Tarakanova, V.L. B Cell-Intrinsic SHP1 Expression Promotes the Gammaherpesvirus-Driven Germinal Center Response and the Establishment of Chronic Infection. J. Virol. 2019, 94. [Google Scholar] [CrossRef]
- Getahun, A.; Smith, M.J.; Kogut, I.; van Dyk, L.F.; Cambier, J.C. Retention of anergy and inhibition of antibody responses during acute gamma herpesvirus 68 infection. J. Immunol. 2012, 189, 2965–2974. [Google Scholar] [CrossRef] [Green Version]
- Sangster, M.Y.; Topham, D.J.; D’Costa, S.; Cardin, R.D.; Marion, T.N.; Myers, L.K.; Doherty, P.C. Analysis of the virus-specific and nonspecific B cell response to a persistent B-lymphotropic gammaherpesvirus. J. Immunol. 2000, 164, 1820–1828. [Google Scholar] [CrossRef] [Green Version]
- Freeman, M.L.; Burkum, C.E.; Lanzer, K.G.; Roberts, A.D.; Pinkevych, M.; Itakura, A.; Kummer, L.W.; Szaba, F.M.; Davenport, M.P.; McCarty, O.J.; et al. Gammaherpesvirus latency induces antibody-associated thrombocytopenia in mice. J. Autoimmun. 2013, 42, 71–79. [Google Scholar] [CrossRef] [Green Version]
- Darrah, E.J.; Jondle, C.N.; Johnson, K.E.; Xin, G.; Lange, P.T.; Cui, W.; Olteanu, H.; Tarakanova, V.L. Conserved Gammaherpesvirus Protein Kinase Selectively Promotes Irrelevant B Cell Responses. J. Virol. 2019, 93. [Google Scholar] [CrossRef] [Green Version]
- Virgin, H.W.T.; Presti, R.M.; Li, X.Y.; Liu, C.; Speck, S.H. Three distinct regions of the murine gammaherpesvirus 68 genome are transcriptionally active in latently infected mice. J. Virol. 1999, 73, 2321–2332. [Google Scholar] [CrossRef] [Green Version]
- Moorman, N.J.; Willer, D.O.; Speck, S.H. The gammaherpesvirus 68 latency-associated nuclear antigen homolog is critical for the establishment of splenic latency. J. Virol. 2003, 77, 10295–10303. [Google Scholar] [CrossRef] [Green Version]
- Sifford, J.M.; Stahl, J.A.; Salinas, E.; Forrest, J.C. Murine Gammaherpesvirus 68 LANA and SOX Homologs Counteract ATM-Driven p53 Activity during Lytic Viral Replication. J. Virol. 2015, 90, 2571–2585. [Google Scholar] [CrossRef] [Green Version]
- Cerqueira, S.A.; Tan, M.; Li, S.; Juillard, F.; McVey, C.E.; Kaye, K.M.; Simas, J.P. Latency-Associated Nuclear Antigen E3 Ubiquitin Ligase Activity Impacts Gammaherpesvirus-Driven Germinal Center B Cell Proliferation. J. Virol. 2016, 90, 7667. [Google Scholar] [CrossRef] [Green Version]
- Rangaswamy, U.S.; Speck, S.H. Murine gammaherpesvirus M2 protein induction of IRF4 via the NFAT pathway leads to IL-10 expression in B cells. PLoS Pathog. 2014, 10, e1003858. [Google Scholar] [CrossRef]
- Williams, L.M.; Niemeyer, B.F.; Franklin, D.S.; Clambey, E.T.; van Dyk, L.F. A Conserved Gammaherpesvirus Cyclin Specifically Bypasses Host p18(INK4c) To Promote Reactivation from Latency. J. Virol. 2015, 89, 10821–10831. [Google Scholar] [CrossRef] [Green Version]
- Niemeyer, B.F.; Oko, L.M.; Medina, E.M.; Oldenburg, D.G.; White, D.W.; Cool, C.D.; Clambey, E.T.; van Dyk, L.F. Host Tumor Suppressor p18(INK4c) Functions as a Potent Cell-Intrinsic Inhibitor of Murine Gammaherpesvirus 68 Reactivation and Pathogenesis. J. Virol. 2018, 92. [Google Scholar] [CrossRef] [Green Version]
- E, X.; Hwang, S.; Oh, S.; Lee, J.-S.; Jeong, J.H.; Gwack, Y.; Kowalik, T.F.; Sun, R.; Jung, J.U.; Liang, C. Viral Bcl-2-Mediated Evasion of Autophagy Aids Chronic Infection of γHerpesvirus 68. PLoS Pathog. 2009, 5, e1000609. [Google Scholar] [CrossRef] [Green Version]
- Feldman, E.R.; Kara, M.; Oko, L.M.; Grau, K.R.; Krueger, B.J.; Zhang, J.; Feng, P.; van Dyk, L.F.; Renne, R.; Tibbetts, S.A. A Gammaherpesvirus Noncoding RNA Is Essential for Hematogenous Dissemination and Establishment of Peripheral Latency. MSphere 2016, 1. [Google Scholar] [CrossRef] [Green Version]
- Usherwood, E.J.; Stewart, J.P.; Nash, A.A. Characterization of tumor cell lines derived from murine gammaherpesvirus-68-infected mice. J. Virol. 1996, 70, 6516–6518. [Google Scholar] [CrossRef] [Green Version]
- Ehlin-Henriksson, B.; Gordon, J.; Klein, G. B-lymphocyte subpopulations are equally susceptible to Epstein-Barr virus infection, irrespective of immunoglobulin isotype expression. Immunology 2003, 108, 427–430. [Google Scholar] [CrossRef]
- Hochberg, D.; Souza, T.; Catalina, M.; Sullivan, J.L.; Luzuriaga, K.; Thorley-Lawson, D.A. Acute infection with Epstein-Barr virus targets and overwhelms the peripheral memory B-cell compartment with resting, latently infected cells. J. Virol. 2004, 78, 5194–5204. [Google Scholar] [CrossRef] [Green Version]
- Kurth, J.; Hansmann, M.L.; Rajewsky, K.; Kuppers, R. Epstein-Barr virus-infected B cells expanding in germinal centers of infectious mononucleosis patients do not participate in the germinal center reaction. Proc. Natl. Acad. Sci. USA 2003, 100, 4730–4735. [Google Scholar] [CrossRef] [Green Version]
- Stevenson, F.K.; Smith, G.J.; North, J.; Hamblin, T.J.; Glennie, M.J. Identification of normal B-cell counterparts of neoplastic cells which secrete cold agglutinins of anti-I and anti-i specificity. Br. J. Haematol. 1989, 72, 9–15. [Google Scholar] [CrossRef]
- Kostareli, E.; Hadzidimitriou, A.; Stavroyianni, N.; Darzentas, N.; Athanasiadou, A.; Gounari, M.; Bikos, V.; Agathagelidis, A.; Touloumenidou, T.; Zorbas, I.; et al. Molecular evidence for EBV and CMV persistence in a subset of patients with chronic lymphocytic leukemia expressing stereotyped IGHV4-34 B-cell receptors. Leukemia 2009, 23, 919–924. [Google Scholar] [CrossRef]
- Pascual, V.; Capra, J.D. VH4-21, a human VH gene segment overrepresented in the autoimmune repertoire. Arthritis Rheumatol. 1992, 35, 11–18. [Google Scholar] [CrossRef]
- Ippolito, G.C.; Hoi, K.H.; Reddy, S.T.; Carroll, S.M.; Ge, X.; Rogosch, T.; Zemlin, M.; Shultz, L.D.; Ellington, A.D.; Vandenberg, C.L.; et al. Antibody repertoires in humanized NOD-scid-IL2Rgamma(null) mice and human B cells reveals human-like diversification and tolerance checkpoints in the mouse. PLoS ONE 2012, 7, e35497. [Google Scholar] [CrossRef]
- Mroczek, E.S.; Ippolito, G.C.; Rogosch, T.; Hoi, K.H.; Hwangpo, T.A.; Brand, M.G.; Zhuang, Y.; Liu, C.R.; Schneider, D.A.; Zemlin, M.; et al. Differences in the composition of the human antibody repertoire by B cell subsets in the blood. Front. Immunol. 2014, 5, 96. [Google Scholar] [CrossRef]
- Pugh-Bernard, A.E.; Silverman, G.J.; Cappione, A.J.; Villano, M.E.; Ryan, D.H.; Insel, R.A.; Sanz, I. Regulation of inherently autoreactive VH4-34 B cells in the maintenance of human B cell tolerance. J. Clin. Investig. 2001, 108, 1061–1070. [Google Scholar] [CrossRef]
- Isenberg, D.; Spellerberg, M.; Williams, W.; Griffiths, M.; Stevenson, F. Identification of the 9G4 idiotope in systemic lupus erythematosus. Br. J. Rheumatol. 1993, 32, 876–882. [Google Scholar] [CrossRef]
- Kobie, J.J.; Alcena, D.C.; Zheng, B.; Bryk, P.; Mattiacio, J.L.; Brewer, M.; Labranche, C.; Young, F.M.; Dewhurst, S.; Montefiori, D.C.; et al. 9G4 autoreactivity is increased in HIV-infected patients and correlates with HIV broadly neutralizing serum activity. PLoS ONE 2012, 7, e35356. [Google Scholar] [CrossRef] [Green Version]
- Grande, B.M.; Gerhard, D.S.; Jiang, A.; Griner, N.B.; Abramson, J.S.; Alexander, T.B.; Allen, H.; Ayers, L.W.; Bethony, J.M.; Bhatia, K.; et al. Genome-wide discovery of somatic coding and noncoding mutations in pediatric endemic and sporadic Burkitt lymphoma. Blood 2019, 133, 1313–1324. [Google Scholar] [CrossRef] [PubMed]
- Baptista, M.J.; Calpe, E.; Fernandez, E.; Colomo, L.; Cardesa-Salzmann, T.M.; Abrisqueta, P.; Bosch, F.; Crespo, M. Analysis of the IGHV region in Burkitt’s lymphomas supports a germinal center origin and a role for superantigens in lymphomagenesis. Leuk. Res. 2014, 38, 509–515. [Google Scholar] [CrossRef]
- Chapman, C.J.; Wright, D.; Stevenson, F.K. Insight into Burkitt’s lymphoma from immunoglobulin variable region gene analysis. Leuk. Lymphoma. 1998, 30, 257–267. [Google Scholar] [CrossRef]
- Amato, T.; Abate, F.; Piccaluga, P.; Iacono, M.; Fallerini, C.; Renieri, A.; De Falco, G.; Ambrosio, M.R.; Mourmouras, V.; Ogwang, M.; et al. Clonality Analysis of Immunoglobulin Gene Rearrangement by Next-Generation Sequencing in Endemic Burkitt Lymphoma Suggests Antigen Drive Activation of BCR as Opposed to Sporadic Burkitt Lymphoma. Am. J. Clin. Pathol. 2016, 145, 116–127. [Google Scholar] [CrossRef]
- Zhu, D.; Ottensmeier, C.H.; Du, M.Q.; McCarthy, H.; Stevenson, F.K. Incidence of potential glycosylation sites in immunoglobulin variable regions distinguishes between subsets of Burkitt’s lymphoma and mucosa-associated lymphoid tissue lymphoma. Br. J. Haematol. 2003, 120, 217–222. [Google Scholar] [CrossRef]
- Harris, R.S.; Croom-Carter, D.S.; Rickinson, A.B.; Neuberger, M.S. Epstein-Barr virus and the somatic hypermutation of immunoglobulin genes in Burkitt’s lymphoma cells. J. Virol. 2001, 75, 10488–10492. [Google Scholar] [CrossRef] [Green Version]
- Sale, J.E.; Neuberger, M.S. TdT-accessible breaks are scattered over the immunoglobulin V domain in a constitutively hypermutating B cell line. Immunity 1998, 9, 859–869. [Google Scholar] [CrossRef] [Green Version]
- Capello, D.; Cerri, M.; Muti, G.; Lucioni, M.; Oreste, P.; Gloghini, A.; Berra, E.; Deambrogi, C.; Franceschetti, S.; Rossi, D.; et al. Analysis of immunoglobulin heavy and light chain variable genes in post-transplant lymphoproliferative disorders. Hematol. Oncol. 2006, 24, 212–219. [Google Scholar] [CrossRef]
- Vletter, E.M.; Koning, M.T.; Scherer, H.U.; Veelken, H.; Toes, R.E.M. A Comparison of Immunoglobulin Variable Region N-Linked Glycosylation in Healthy Donors, Autoimmune Disease and Lymphoma. Front. Immunol. 2020, 11, 241. [Google Scholar] [CrossRef] [Green Version]
- Dollery, S.J.; Santiago-Crespo, R.J.; Kardava, L.; Moir, S.; Berger, E.A. Efficient infection of a human B cell line with cell-free Kaposi’s sarcoma-associated herpesvirus. J. Virol. 2014, 88, 1748–1757. [Google Scholar] [CrossRef] [Green Version]
- Rappocciolo, G.; Hensler, H.R.; Jais, M.; Reinhart, T.A.; Pegu, A.; Jenkins, F.J.; Rinaldo, C.R. Human herpesvirus 8 infects and replicates in primary cultures of activated B lymphocytes through DC-SIGN. J. Virol. 2008, 82, 4793–4806. [Google Scholar] [CrossRef] [Green Version]
- DeKosky, B.J.; Kojima, T.; Rodin, A.; Charab, W.; Ippolito, G.C.; Ellington, A.D.; Georgiou, G. In-depth determination and analysis of the human paired heavy- and light-chain antibody repertoire. Nat. Med. 2015, 21, 86–91. [Google Scholar] [CrossRef]
- DeKosky, B.J.; Ippolito, G.C.; Deschner, R.P.; Lavinder, J.J.; Wine, Y.; Rawlings, B.M.; Varadarajan, N.; Giesecke, C.; Dorner, T.; Andrews, S.F.; et al. High-throughput sequencing of the paired human immunoglobulin heavy and light chain repertoire. Nat. Biotechnol. 2013, 31, 166–169. [Google Scholar] [CrossRef] [Green Version]
- Prabakaran, P.; Chen, W.; Singarayan, M.G.; Stewart, C.C.; Streaker, E.; Feng, Y.; Dimitrov, D.S. Expressed antibody repertoires in human cord blood cells: 454 sequencing and IMGT/HighV-QUEST analysis of germline gene usage, junctional diversity, and somatic mutations. Immunogenetics 2012, 64, 337–350. [Google Scholar] [CrossRef] [PubMed]
- Decalf, J.; Godinho-Silva, C.; Fontinha, D.; Marques, S.; Simas, J.P. Establishment of murine gammaherpesvirus latency in B cells is not a stochastic event. PLoS Pathog. 2014, 10, e1004269. [Google Scholar] [CrossRef] [Green Version]
- Rekow, M.M.; Darrah, E.J.; Mboko, W.P.; Lange, P.T.; Tarakanova, V.L. Gammaherpesvirus targets peritoneal B-1 B cells for long-term latency. Virology 2016, 492, 140–144. [Google Scholar] [CrossRef]
- Phan, T.G.; Amesbury, M.; Gardam, S.; Crosbie, J.; Hasbold, J.; Hodgkin, P.D.; Basten, A.; Brink, R. B cell receptor-independent stimuli trigger immunoglobulin (Ig) class switch recombination and production of IgG autoantibodies by anergic self-reactive B cells. J. Exp. Med. 2003, 197, 845–860. [Google Scholar] [CrossRef] [PubMed]
- Prohaska, T.A.; Que, X.; Diehl, C.J.; Hendrikx, S.; Chang, M.W.; Jepsen, K.; Glass, C.K.; Benner, C.; Witztum, J.L. Massively Parallel Sequencing of Peritoneal and Splenic B Cell Repertoires Highlights Unique Properties of B-1 Cell Antibodies. J. Immunol. 2018, 200, 1702–1717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, H.; Cerny, J. Functional heterogeneity of marginal zone B cells revealed by their ability to generate both early antibody-forming cells and germinal centers with hypermutation and memory in response to a T-dependent antigen. J. Exp. Med. 2003, 198, 1923–1935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cerutti, A.; Cols, M.; Puga, I. Marginal zone B cells: Virtues of innate-like antibody-producing lymphocytes. Nat. Rev. Immunol. 2013, 13, 118–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maranhao, A.Q.; Costa, M.B.; Guedes, L.; Moraes-Vieira, P.M.; Raiol, T.; Brigido, M.M. A mouse variable gene fragment binds to DNA independently of the BCR context: A possible role for immature B-cell repertoire establishment. PLoS ONE 2013, 8, e72625. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brigido, M.M.; Polymenis, M.; Stollar, B.D. Role of mouse VH10 and VL gene segments in the specific binding of antibody to Z-DNA, analyzed with recombinant single chain Fv molecules. J. Immunol. 1993, 150, 469–479. [Google Scholar]
- Jang, Y.J.; Stollar, B.D. Anti-DNA antibodies: Aspects of structure and pathogenicity. Cell. Mol. Life Sci. 2003, 60, 309–320. [Google Scholar] [CrossRef]
- Brigido, M.M.; Stollar, B.D. Two induced anti-Z-DNA monoclonal antibodies use VH gene segments related to those of anti-DNA autoantibodies. J. Immunol. 1991, 146, 2005–2009. [Google Scholar]
- Rodkey, L.S.; Gololobov, G.; Rumbley, C.A.; Rumbley, J.; Schourov, D.V.; Makarevich, O.I.; Gabibov, A.G.; Voss, E.W., Jr. DNA hydrolysis by monoclonal autoantibody BV 04-01. Appl. Biochem. Biotechnol. 2000, 83, 95–103, discussion 103–105, 145–153. [Google Scholar] [CrossRef]
- Gong, S.; Crane, G.M.; McCall, C.M.; Xiao, W.; Ganapathi, K.A.; Cuka, N.; Davies-Hill, T.; Xi, L.; Raffeld, M.; Pittaluga, S.; et al. Expanding the Spectrum of EBV-positive Marginal Zone Lymphomas: A Lesion Associated With Diverse Immunodeficiency Settings. Am. J. Surg. Pathol. 2018, 42, 1306–1316. [Google Scholar] [CrossRef]
- Chaganti, S.; Bell, A.I.; Pastor, N.B.; Milner, A.E.; Drayson, M.; Gordon, J.; Rickinson, A.B. Epstein-Barr virus infection in vitro can rescue germinal center B cells with inactivated immunoglobulin genes. Blood 2005, 106, 4249–4252. [Google Scholar] [CrossRef] [PubMed]
- Jacoby, M.A.; Virgin, H.W.t.; Speck, S.H. Disruption of the M2 gene of murine gammaherpesvirus 68 alters splenic latency following intranasal, but not intraperitoneal, inoculation. J. Virol. 2002, 76, 1790–1801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, A.G.; Moorman, N.J.; Willer, D.O.; Speck, S.H. The M4 gene of gammaHV68 encodes a secreted glycoprotein and is required for the efficient establishment of splenic latency. Virology 2006, 344, 520–531. [Google Scholar] [CrossRef] [Green Version]
- Minkah, N.; Macaluso, M.; Oldenburg, D.G.; Paden, C.R.; White, D.W.; McBride, K.M.; Krug, L.T. Absence of the uracil DNA glycosylase of murine gammaherpesvirus 68 impairs replication and delays the establishment of latency in vivo. J. virol. 2015, 89, 3366–3379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Skike, N.D.; Minkah, N.K.; Hogan, C.H.; Wu, G.; Benziger, P.T.; Oldenburg, D.G.; Kara, M.; Kim-Holzapfel, D.M.; White, D.W.; Tibbetts, S.A.; et al. Viral FGARAT ORF75A promotes early events in lytic infection and gammaherpesvirus pathogenesis in mice. PLoS Pathog. 2018, 14, e1006843. [Google Scholar] [CrossRef] [Green Version]
- Tomayko, M.M.; Allman, D. What B cell memories are made of. Curr. Opin. Immunol. 2019, 57, 58–64. [Google Scholar] [CrossRef]
- Ascherio, A.; Munger, K.L. Epstein-barr virus infection and multiple sclerosis: A review. J. Neuroimmune Pharmacol. 2010, 5, 271–277. [Google Scholar] [CrossRef]
- Harley, J.B.; Harley, I.T.; Guthridge, J.M.; James, J.A. The curiously suspicious: A role for Epstein-Barr virus in lupus. Lupus 2006, 15, 768–777. [Google Scholar] [CrossRef]
- Zharkova, O.; Celhar, T.; Cravens, P.D.; Satterthwaite, A.B.; Fairhurst, A.M.; Davis, L.S. Pathways leading to an immunological disease: Systemic lupus erythematosus. Rheumatology 2017, 56, i55–i66. [Google Scholar] [CrossRef] [Green Version]
- Larson, J.D.; Thurman, J.M.; Rubtsov, A.V.; Claypool, D.; Marrack, P.; van Dyk, L.F.; Torres, R.M.; Pelanda, R. Murine gammaherpesvirus 68 infection protects lupus-prone mice from the development of autoimmunity. Proc. Natl. Acad. Sci. USA 2012, 109, E1092–E1100. [Google Scholar] [CrossRef] [Green Version]
- Gauld, S.B.; De Santis, J.L.; Kulinski, J.M.; McGraw, J.A.; Leonardo, S.M.; Ruder, E.A.; Maier, W.; Tarakanova, V.L. Modulation of B-cell tolerance by murine gammaherpesvirus 68 infection: Requirement for Orf73 viral gene expression and follicular helper T cells. Immunology 2013, 139, 197–204. [Google Scholar] [CrossRef]
- Sakakibara, S.; Yasui, T.; Jinzai, H.; O’Donnell, K.; Tsai, C.Y.; Minamitani, T.; Takeda, K.; Belz, G.T.; Tarlinton, D.M.; Kikutani, H. Self-reactive and polyreactive B cells are generated and selected in the germinal center during gamma-herpesvirus infection. Int. Immunol. 2020, 32, 27–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, K.A.; Efstathiou, S.; Cooke, A. Murine gammaherpesvirus-68 infection alters self-antigen presentation and type 1 diabetes onset in NOD mice. J. Immunol. 2007, 179, 7325–7333. [Google Scholar] [CrossRef] [PubMed]
- Peacock, J.W.; Elsawa, S.F.; Petty, C.C.; Hickey, W.F.; Bost, K.L. Exacerbation of experimental autoimmune encephalomyelitis in rodents infected with murine gammaherpesvirus-68. Eur. J. Immunol. 2003, 33, 1849–1858. [Google Scholar] [CrossRef] [PubMed]
- Yarilin, D.A.; Valiando, J.; Posnett, D.N. A mouse herpesvirus induces relapse of experimental autoimmune arthritis by infection of the inflammatory target tissue. J. Immunol. 2004, 173, 5238–5246. [Google Scholar] [CrossRef]
- Bhat, N.M.; Bieber, M.M.; Spellerberg, M.B.; Stevenson, F.K.; Teng, N.N. Recognition of auto- and exoantigens by V4-34 gene encoded antibodies. Scand. J. Immunol. 2000, 51, 134–140. [Google Scholar] [CrossRef]
- Afik, S.; Raulet, G.; Yosef, N. Reconstructing B-cell receptor sequences from short-read single-cell RNA sequencing with BRAPeS. Life Sci. Alliance 2019, 2. [Google Scholar] [CrossRef] [Green Version]
- Morrison, K.; Manzano, M.; Chung, K.; Schipma, M.J.; Bartom, E.T.; Gottwein, E. The Oncogenic Kaposi’s Sarcoma-Associated Herpesvirus Encodes a Mimic of the Tumor-Suppressive miR-15/16 miRNA Family. Cell Rep. 2019, 29, 2961–2969. [Google Scholar] [CrossRef] [Green Version]
- Forte, E.; Luftig, M.A. MDM2-dependent inhibition of p53 is required for Epstein-Barr virus B-cell growth transformation and infected-cell survival. J. Virol. 2009, 83, 2491–2499. [Google Scholar] [CrossRef] [Green Version]
- Epeldegui, M.; Hung, Y.P.; McQuay, A.; Ambinder, R.F.; Martinez-Maza, O. Infection of human B cells with Epstein-Barr virus results in the expression of somatic hypermutation-inducing molecules and in the accrual of oncogene mutations. Mol. Immunol. 2007, 44, 934–942. [Google Scholar] [CrossRef]
- Allday, M.J. How does Epstein-Barr virus (EBV) complement the activation of Myc in the pathogenesis of Burkitt’s lymphoma? Semin. Cancer Biol. 2009, 19, 366–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bechtel, D.; Kurth, J.; Unkel, C.; Kuppers, R. Transformation of BCR-deficient germinal-center B cells by EBV supports a major role of the virus in the pathogenesis of Hodgkin and posttransplantation lymphomas. Blood 2005, 106, 4345–4350. [Google Scholar] [CrossRef] [PubMed]
- Timms, J.M.; Bell, A.; Flavell, J.R.; Murray, P.G.; Rickinson, A.B.; Traverse-Glehen, A.; Berger, F.; Delecluse, H.J. Target cells of Epstein-Barr-virus (EBV)-positive post-transplant lymphoproliferative disease: Similarities to EBV-positive Hodgkin’s lymphoma. Lancet 2003, 361, 217–223. [Google Scholar] [CrossRef]
- Guillet, S.; Gerard, L.; Meignin, V.; Agbalika, F.; Cuccini, W.; Denis, B.; Katlama, C.; Galicier, L.; Oksenhendler, E. Classic and extracavitary primary effusion lymphoma in 51 HIV-infected patients from a single institution. Am. J. Hematol. 2016, 91, 233–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lurain, K.; Polizzotto, M.N.; Aleman, K.; Bhutani, M.; Wyvill, K.M.; Goncalves, P.H.; Ramaswami, R.; Marshall, V.A.; Miley, W.; Steinberg, S.M.; et al. Viral, immunologic, and clinical features of primary effusion lymphoma. Blood 2019, 133, 1753–1761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horns, F.; Dekker, C.L.; Quake, S.R. Memory B Cell Activation, Broad Anti-influenza Antibodies, and Bystander Activation Revealed by Single-Cell Transcriptomics. Cell Rep. 2020, 30, 905–913. [Google Scholar] [CrossRef] [Green Version]
- Sanborn, M.A.; Li, T.; Victor, K.; Siegfried, H.; Fung, C.; Rothman, A.L.; Srikiatkhachorn, A.; Fernandez, S.; Ellison, D.; Jarman, R.G.; et al. Analysis of cell-associated DENV RNA by oligo(dT) primed 5’ capture scRNAseq. Sci. Rep. 2020, 10, 9047. [Google Scholar] [CrossRef]
- Helmink, B.A.; Reddy, S.M.; Gao, J.; Zhang, S.; Basar, R.; Thakur, R.; Yizhak, K.; Sade-Feldman, M.; Blando, J.; Han, G.; et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature 2020, 577, 549–555. [Google Scholar] [CrossRef]
- Zhao, J.; Guo, C.; Xiong, F.; Yu, J.; Ge, J.; Wang, H.; Liao, Q.; Zhou, Y.; Gong, Q.; Xiang, B.; et al. Single cell RNA-seq reveals the landscape of tumor and infiltrating immune cells in nasopharyngeal carcinoma. Cancer Lett. 2020, 477, 131–143. [Google Scholar] [CrossRef]
- Tanno, H.; McDaniel, J.R.; Stevens, C.A.; Voss, W.N.; Li, J.; Durrett, R.; Lee, J.; Gollihar, J.; Tanno, Y.; Delidakis, G.; et al. A facile technology for the high-throughput sequencing of the paired VH:VL and TCRbeta:TCRalpha repertoires. Sci. Adv. 2020, 6, eaay9093. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Virus | Source | Tissue | #Cells | Bias | Ref. |
|---|---|---|---|---|---|
| EBV | IM patients | PB (CD20+, CD27+) | 32 | VH mutated evidence of antigen selection | [80] |
| IM patients | PB (CD20+, CD27+) | 100–300 | more SHM events in EBV+ EBV excluded from IgM+ | [81] | |
| IM patients | CD19+, IgD−, | 56 Abs a | no bias in IGHV usage, VH mutated evidence of antigen selection | [82] | |
| IM patients | sera | elevated level of IGHV4-34 expressing Abs b | [83] | ||
| IM patients | sera | elevated level of IGHV4-34 expressing Abs b | [84] | ||
| in vitro infection | healthy PBMCs, naïve (IgD+, CD27−) | 25 c | accumulation of SHM events with time, no CSR detected, clonal expansion | [79] | |
| in vitro infection | healthy PBMCs, non-switched memory (IgD+, CD27+) | 38 c | SHM pattern does not change with time, no CSR detected | [79] | |
| in vitro infection | healthy PBMCs, switched memory (IgD−, CD27+) | 55 c | SHM pattern does not change with time, no CSR detected | [79] | |
| in vitro infection | healthy PBMCs | bias in IGHV usage, lower BCR diversity, dominant consensus CDR3 motif | [85] | ||
| KSHV | in vitro infection | tonsillar B cells | infection restricted to IgMλ B cells | [86] | |
| in vitro infection | naïve B cells from tonsils (CD38lowIgD+CD27−) | 480 | induction of Igλ expression, bias in IGLV4 usage | [87] | |
| MHV68 | C57Bl/6 | MHV+ GC cells (CD19+GL7highCD95+) | >400 d | bias Ighv10 usage, bias in Igλ usage | [88] |
| C57Bl/6 | MHV+ GC cells (CDB220+GL7highCD95+) MHV+ PC (B220lo-neg, CD138+) | 100–200 d | bias Ighv10 usage, bias in Igλ usage | [89] |
| Virus | Cancer | Source | #Patients | Remarks | Ref. |
|---|---|---|---|---|---|
| EBV | eBL | EBV+ tumor samples | 11 tumor samples | IGHV1-69, IGHV3-23 and IGHV4-34 overrepresented in eBL | [202] |
| BL | EBV+ tumor samples | 71 tumor samples | IGHV4-34 and IGHV3-30 overrepresented | [199] | |
| NPC | sera | elevated level of IGHV4-34 expressing Abs a | [84] | ||
| CLL | PBMCs | 25 patients positive for either EBV or CMV | higher frequency of IGHV4-34 b | [192] | |
| CLL | PBMCs | 9 patients positive for both EBV and CMV | exclusive expression of IGHV4-34 b | [192] | |
| PTLD (P-PTLD, DLBCL, BL) | tissue sections | 26 patients | no IGHV bias detected, crippled BCR present | [206] | |
| KSHV | KSHV+ MCD | tissue sections | 13 patients | no bias in IGHV; λ light chain restriction; low SHM | [22] |
| PEL | cell samples of lymphomatous effusions | 4 patients | monoclonal Ig expressing IGHV3-23, IGHV3-73, IGHV4-39, and IGHV1-03, bias in λ usage | [24] | |
| PEL cell lines | cell line | 3 cell lines | monoclonal Ig expressing IGHV3-73 and IGHV5-51 | [24] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zelazowska, M.A.; McBride, K.; Krug, L.T. Dangerous Liaisons: Gammaherpesvirus Subversion of the Immunoglobulin Repertoire. Viruses 2020, 12, 788. https://0-doi-org.brum.beds.ac.uk/10.3390/v12080788
Zelazowska MA, McBride K, Krug LT. Dangerous Liaisons: Gammaherpesvirus Subversion of the Immunoglobulin Repertoire. Viruses. 2020; 12(8):788. https://0-doi-org.brum.beds.ac.uk/10.3390/v12080788
Chicago/Turabian StyleZelazowska, Monika A., Kevin McBride, and Laurie T. Krug. 2020. "Dangerous Liaisons: Gammaherpesvirus Subversion of the Immunoglobulin Repertoire" Viruses 12, no. 8: 788. https://0-doi-org.brum.beds.ac.uk/10.3390/v12080788