Three-Dimensional Human Cell Culture Models to Study the Pathophysiology of the Anterior Eye
Abstract
:1. Introduction
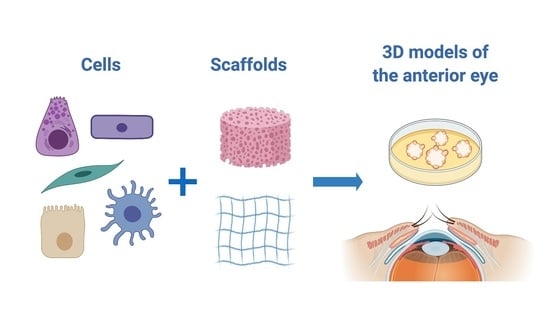
1.1. Increasing Complexity of In Vitro Models
1.2. Cell Types Used in In Vitro Models
1.3. In Vitro Models in Ophthalmic Research
2. Three-Dimensional In Vitro Models of Anterior Eye Tissues
2.1. Tear Film and Its Production Tissues
2.1.1. Lacrimal Gland
2.1.2. Meibomian Glands
2.2. Cornea
2.2.1. Corneal Epithelium 3D Models
2.2.2. Corneal Stroma 3D Models
2.2.3. Corneal Endothelium 3D Models
2.2.4. Multilayer or Whole Cornea Models (Corneal Equivalents)
2.3. Limbus
2.4. Conjunctiva
2.5. Conjunctiva and Uvea in Ocular Cancer
2.6. Trabecular Meshwork
2.7. Lens
3. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Abbott, R.D.; Kaplan, D.L. Strategies for improving the physiological relevance of human engineered tissues. Trends Biotechnol. 2015, 33, 401–407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jedrzejczak-Silicka, M. History of Cell Culture. New Insights into Cell Culture Technology; IntechOpen: London, UK, 2017. [Google Scholar] [CrossRef] [Green Version]
- Harrison, R.G. Observations on the living developing nerve fiber. Proc. Soc. Exp. Biol. Med. 1907. [Google Scholar] [CrossRef] [Green Version]
- Carrel, A.; Burrows, M.T. Cultivation of tissues in vitro and its technique. J. Exp. Med. 1911. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.W.; Taylor, M.W. A History of Cell Culture. In Viruses and Man: A History of Interactions; Springer: Cham, Switzerland, 2014. [Google Scholar] [CrossRef]
- Anton, D.; Burckel, H.; Josset, E.; Noel, G. Three-dimensional cell culture: A breakthrough in vivo. Int. J. Mol. Sci. 2015, 16, 5517–5527. [Google Scholar] [CrossRef]
- Ryan, S.L.; Baird, A.M.; Vaz, G.; Urquhart, A.J.; Senge, M.; Richard, D.J.; O’Byrne, K.J.; Davies, A.M. Drug Discovery Approaches Utilizing Three-Dimensional Cell Culture. Assay Drug Dev. Technol. 2016, 14, 19–28. [Google Scholar] [CrossRef]
- Breslin, S.; O’Driscoll, L. Three-dimensional cell culture: The missing link in drug discovery. Drug Discov. Today 2013, 18, 240–249. [Google Scholar] [CrossRef]
- Langhans, S.A. Three-dimensional in vitro cell culture models in drug discovery and drug repositioning. Front. Pharmacol. 2018, 9. [Google Scholar] [CrossRef]
- Eglen, R.M.; Randle, D.H. Drug Discovery Goes Three-Dimensional: Goodbye to Flat High-Throughput Screening? Assay Drug Dev. Technol. 2015, 13, 262–265. [Google Scholar] [CrossRef]
- Edmondson, R.; Broglie, J.J.; Adcock, A.F.; Yang, L. Three-dimensional cell culture systems and their applications in drug discovery and cell-based biosensors. Assay Drug Dev. Technol. 2014, 12, 207–218. [Google Scholar] [CrossRef] [Green Version]
- Ravi, M.; Paramesh, V.; Kaviya, S.R.; Anuradha, E.; Paul Solomon, F.D. 3D cell culture systems: Advantages and applications. J. Cell. Physiol. 2015. [Google Scholar] [CrossRef]
- Fitzgerald, K.A.; Malhotra, M.; Curtin, C.M.; O’Brien, F.J.; O’Driscoll, C.M. Life in 3D is never flat: 3D models to optimise drug delivery. J. Control. Release 2015, 215, 39–54. [Google Scholar] [CrossRef] [PubMed]
- Laschke, M.W.; Menger, M.D. Life is 3D: Boosting Spheroid Function for Tissue Engineering. Trends Biotechnol. 2017, 35, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.V.; Atala, A. 3D bioprinting of tissues and organs. Nat. Biotechnol. 2014, 32, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Ronaldson-Bouchard, K.; Vunjak-Novakovic, G. Organs-on-a-Chip: A Fast Track for Engineered Human Tissues in Drug Development. Cell Stem Cell 2018, 22, 310–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simian, M.; Bissell, M.J. Organoids: A historical perspective of thinking in three dimensions. J. Cell Biol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Badyal, D.K.; Desai, C. Animal use in pharmacology education and research: The changing scenario. Indian J. Pharmacol. 2014, 46, 257–265. [Google Scholar] [CrossRef]
- Kaur, G.; Dufour, J.M. Cell lines: Valuable tools or useless artifacts. Spermatogenesis 2012. [Google Scholar] [CrossRef] [Green Version]
- Carter, M.; Shieh, J. Cell Culture Techniques BT-Guide to Research Techniques in Neuroscience (Second Edition). In Guide to Research Techniques in Neuroscience, 2nd ed.; Academic Press; Elsevier: Waltham, MA, USA, 2015; ISBN 978-0-12-800511-8. [Google Scholar]
- MacLeod, R.A.; Drexler, H.G. Cell banks detect false cell lines: Journals must act too. Lancet Oncol. 2001, 2, 467–468. [Google Scholar] [CrossRef]
- Capes-Davis, A.; Theodosopoulos, G.; Atkin, I.; Drexler, H.G.; Kohara, A.; MacLeod, R.A.F.; Masters, J.R.; Nakamura, Y.; Reid, Y.A.; Reddel, R.R.; et al. Check your cultures! A list of cross-contaminated or misidentified cell lines. Int. J. Cancer 2010, 127, 1–8. [Google Scholar] [CrossRef]
- Horbach, S.P.J.M.; Halffman, W. The ghosts of HeLa: How cell line misidentification contaminates the scientific literature. PLoS ONE 2017. [Google Scholar] [CrossRef]
- Clark, A.; Tamm, E.R.; Al-Ubaidi, M.R.; Hollyfield, J.G. On the use of immortalized ocular cell lines in vision research: The unfortunate story of RGC-5. Exp. Eye Res. 2013, 116, 433. [Google Scholar] [CrossRef] [PubMed]
- Hughes, P.; Marshall, D.; Reid, Y.; Parkes, H.; Gelber, C. The costs of using unauthenticated, over-passaged cell lines: How much more data do we need? Biotechniques 2007, 43, 577–578. [Google Scholar] [CrossRef] [PubMed]
- Ben-David, U.; Siranosian, B.; Ha, G.; Tang, H.; Oren, Y.; Hinohara, K.; Strathdee, C.A.; Dempster, J.; Lyons, N.J.; Burns, R.; et al. Genetic and transcriptional evolution alters cancer cell line drug response. Nature 2018. [Google Scholar] [CrossRef] [PubMed]
- Lorsch, J.R.; Collins, F.S.; Lippincott-Schwartz, J. Fixing problems with cell lines. Science 2014, 346, 1452–1453. [Google Scholar] [CrossRef] [Green Version]
- Estlack, Z.; Bennet, D.; Reid, T.; Kim, J. Microengineered biomimetic ocular models for ophthalmological drug development. Lab Chip 2017, 17, 1539–1551. [Google Scholar] [CrossRef]
- Shafaie, S.; Hutter, V.; Cook, M.T.; Brown, M.B.; Chau, D.Y.S. In Vitro Cell Models for Ophthalmic Drug Development Applications. Biores. Open Access 2016, 5, 94–108. [Google Scholar] [CrossRef] [Green Version]
- Barar, J.; Asadi, M.; Mortazavi-Tabatabaei, S.A.; Omidi, Y. Ocular drug delivery; Impact of in vitro cell culture models. J. Ophthalmic Vis. Res. 2014, 4, 238–252. [Google Scholar]
- Tiffany, J. The normal tear film. Dev. Ophthalmol. 2008. [Google Scholar] [CrossRef]
- Dartt, D.A. Neural regulation of lacrimal gland secretory processes: Relevance in dry eye diseases. Prog. Retin. Eye Res. 2009, 28, 155–177. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.Y.; Hirayama, M.; Ali, M.; Shah, D.; Aakalu, V.K. Strategies for Regenerating the Lacrimal Gland. Curr. Ophthalmol. Rep. 2017, 5, 193–198. [Google Scholar] [CrossRef]
- Tiwari, S.; Ali, M.J.; Balla, M.M.S.; Naik, M.N.; Honavar, S.G.; Reddy, V.A.P.; Vemuganti, G.K. Establishing human lacrimal gland cultures with secretory function. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [Green Version]
- Yoshino, K. Establishment of a human lacrimal gland epithelial culture system with in vivo mimicry and its substrate modulation. Cornea 2000, 19, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Ueda, Y.; Karasawa, Y.; Satoh, Y.; Nishikawa, S.; Imaki, J.; Ito, M. Purification and characterization of mouse lacrimal gland epithelial cells and reconstruction of an acinarlike structure in three-dimensional culture. Investig. Ophthalmol. Vis. Sci. 2009. [Google Scholar] [CrossRef] [PubMed]
- Gromova, A.; Voronov, D.A.; Yoshida, M.; Thotakura, S.; Meech, R.; Dartt, D.A.; Makarenkova, H.P. Lacrimal Gland Repair Using Progenitor Cells. Stem Cells Transl. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Liu, Y.; He, H.; Botsford, B.; Yiu, S. Lacrimal Gland Repair after Short-term Obstruction of Excretory Duct in Rabbits. Sci. Rep. 2017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tiwari, S.; Nair, R.M.; Vamadevan, P.; Ali, M.J.; Naik, M.N.; Honavar, S.G.; Vemuganti, G.K. Establishing and characterizing lacrispheres from human lacrimal gland for potential clinical application. Graefe’s Arch. Clin. Exp. Ophthalmol. 2018, 256. [Google Scholar] [CrossRef]
- Knop, E.; Knop, N.; Millar, T.; Obata, H.; Sullivan, D.A. The international workshop on meibomian gland dysfunction: Report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland. Investig. Ophthalmol. Vis. Sci. 2011. [Google Scholar] [CrossRef] [Green Version]
- Wise, R.J.; Sobel, R.K.; Allen, R.C. Meibography: A review of techniques and technologies. Saudi J. Ophthalmol. 2012. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Hatton, M.P.; Khandelwal, P.; Sullivan, D.A. Culture, immortalization, and characterization of human meibomian gland epithelial cells. Investig. Ophthalmol. Vis. Sci. 2010. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, D.A.; Liu, Y.; Kam, W.R.; Ding, J.; Green, K.M.; Shaffer, S.A.; Hatton, M.P.; Liu, S. Serum-induced differentiation of human meibomian gland epithelial cells. Investig. Ophthalmol. Vis. Sci. 2014. [Google Scholar] [CrossRef] [Green Version]
- Hampel, U.; Garreis, F. The human meibomian gland epithelial cell line as a model to study meibomian gland dysfunction. Exp. Eye Res. 2017, 163, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Davis, R.M.; Aita, M.; Burns, K.A.; Clapp, P.W.; Gilmore, R.C.; Chua, M.; O’Neal, W.K.; Schlegel, R.; Randell, S.H.; et al. Characterization of rat meibomian gland ion and fluid transport. Investig. Ophthalmol. Vis. Sci. 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asano, N.; Hampel, U.; Garreis, F.; Schröder, A.; Schicht, M.; Hammer, C.M.; Paulsen, F. Differentiation patterns of immortalized human meibomian gland epithelial cells in three-dimensional culture. Investig. Ophthalmol. Vis. Sci. 2018. [Google Scholar] [CrossRef] [PubMed]
- Rötzer, V.; Melega, F.; Garreis, F.; Paulsen, F.; Waschke, J. E-Cadherin Is Important for Meibomian Gland Function as Revealed by a New Human ex Vivo Slice Culture Model. Am. J. Pathol. 2019. [Google Scholar] [CrossRef] [Green Version]
- Xu, K.K.; Huang, Y.K.; Liu, X.; Zhang, M.C.; Xie, H.T. Organotypic culture of mouse meibomian gland: A novel model to study meibomian gland dysfunction in vitro. Investig. Ophthalmol. Vis. Sci. 2020. [Google Scholar] [CrossRef]
- Hornof, M.; Toropainen, E.; Urtti, A. Cell culture models of the ocular barriers. Eur. J. Pharm. Biopharm. 2005, 60, 207–225. [Google Scholar] [CrossRef]
- DelMonte, D.W.; Kim, T. Anatomy and physiology of the cornea. J. Cataract Refract. Surg. 2011. [Google Scholar] [CrossRef]
- Eghrari, A.O.; Riazuddin, S.A.; Gottsch, J.D. Overview of the Cornea: Structure, Function, and Development. In Proceedings of the Progress in Molecular Biology and Translational Science; Academic Press; Elsevier: Waltham, MA, USA, 2015. [Google Scholar] [CrossRef]
- Sridhar, M.S. Anatomy of cornea and ocular surface. Indian J. Ophthalmol. 2018, 66, 190–194. [Google Scholar] [CrossRef]
- OECD. OECD Test No. 492: Reconstructed human Cornea-like Epithelium (RhCE) test method for identifying chemicals not requiring classification and labelling for eye irritation or serious eye damage. Guidel. Test. Chem. In OECD Guidelines for the Testing of Chemicals; OECD Publishing: Paris, France, 2019. [Google Scholar] [CrossRef] [Green Version]
- Stern, M.; Klausner, M.; Alvarado, R.; Renskers, K.; Dickens, M. Evaluation of the EpiOcular(TM) tissue model as an alternative to the draize eye irritation test. Toxicol. Vitr. 1998. [Google Scholar] [CrossRef]
- Kaluzhny, Y.; Kandárová, H.; D’argembeau-Thornton, L.; Kearney, P.; Klausner, M. Eye irritation test (EIT) for hazard identification of eye irritating chemicals using reconstructed human cornea-like epithelial (RhCE) tissue model. J. Vis. Exp. 2015. [Google Scholar] [CrossRef] [Green Version]
- Kaluzhny, Y.; Kandárová, H.; Hayden, P.; Kubilus, J.; D’Argembeau-Thornton, L.; Klausner, M. Development of the epiocularTM eye irritation test for hazard identification and labelling of eye irritating chemicals in response to the requirements of the EU cosmetics directive and REACH legislation. ATLA Altern. Lab. Anim. 2011. [Google Scholar] [CrossRef] [PubMed]
- Pfannenbecker, U.; Bessou-Touya, S.; Faller, C.; Harbell, J.; Jacob, T.; Raabe, H.; Tailhardat, M.; Alépée, N.; De Smedt, A.; De Wever, B.; et al. Cosmetics Europe multi-laboratory pre-validation of the EpiOcularTM reconstituted human tissue test method for the prediction of eye irritation. Toxicol. Vitr. 2013. [Google Scholar] [CrossRef]
- Kaluzhny, Y.; Kandárová, H.; Handa, Y.; DeLuca, J.; Truong, T.; Hunter, A.; Kearney, P.; D’Argembeau-Thornton, L.; Klausner, M. The epiocular eye irritation test (EIT) for hazard identification and labelling of eye irritating chemicals: Protocol optimisation for solid materials and the results after extended shipment. ATLA Altern. Lab. Anim. 2015. [Google Scholar] [CrossRef]
- Kolle, S.N.; Moreno, M.C.R.; Mayer, W.; Van Cott, A.; Van Ravenzwaay, B.; Landsiedel, R. The EpiOcularTM eye irritation test is the method of choice for the in vitro eye irritation testing of agrochemical formulations: Correlation analysis of epiocular eye irritation test and BCOP test data according to the un GHS, US EPA and Brazil ANVISA cla. ATLA Altern. Lab. Anim. 2015. [Google Scholar] [CrossRef] [PubMed]
- Alépée, N.; Bessou-Touya, S.; Cotovio, J.; de Smedt, A.; de Wever, B.; Faller, C.; Jones, P.; Le Varlet, B.; Marrec-Fairley, M.; Pfannenbecker, U.; et al. Cosmetics Europe multi-laboratory pre-validation of the SkinEthicTM reconstituted human corneal epithelium test method for the prediction of eye irritation. Toxicol. Vitr. 2013. [Google Scholar] [CrossRef] [PubMed]
- Van Rompay, A.R.; Alépée, N.; Nardelli, L.; Hollanders, K.; Leblanc, V.; Drzewiecka, A.; Gruszka, K.; Guest, R.; Kandarova, H.; Willoughby, J.A.; et al. CON4EI: SkinEthicTM Human Corneal Epithelium Eye Irritation Test (SkinEthicTM HCE EIT) for hazard identification and labelling of eye irritating chemicals. Toxicol. Vitr. 2018. [Google Scholar] [CrossRef]
- Alépée, N.; Leblanc, V.; Adriaens, E.; Grandidier, M.H.; Lelièvre, D.; Meloni, M.; Nardelli, L.; Roper, C.S.; Santirocco, E.; Toner, F.; et al. Multi-laboratory validation of SkinEthic HCE test method for testing serious eye damage/eye irritation using liquid chemicals. Toxicol. Vitr. 2016. [Google Scholar] [CrossRef]
- Cotovio, J.; Grandidier, M.H.; Lelièvre, D.; Bremond, C.; Amsellem, C.; Maloug, S.; Ovigne, J.M.; Loisel-Joubert, S.; Lee, A.V.D.; Minondo, A.M.; et al. In vitro assessment of eye irritancy using the Reconstructed Human Corneal Epithelial SkinEthicTM HCE model: Application to 435 substances from consumer products industry. Toxicol. Vitr. 2010. [Google Scholar] [CrossRef]
- Jung, K.M.; Lee, S.H.; Ryu, Y.H.; Jang, W.H.; Jung, H.S.; Han, J.H.; Seok, S.H.; Park, J.H.; Son, Y.; Park, Y.H.; et al. A new 3D reconstituted human corneal epithelium model as an alternative method for the eye irritation test. Toxicol. Vitr. 2011. [Google Scholar] [CrossRef]
- Katoh, M.; Hamajima, F.; Ogasawara, T.; Hata, K. ichiro Establishment of a new in vitro test method for evaluation of eye irritancy using a reconstructed human corneal epithelial model, LabCyte CORNEA-MODEL. Toxicol. Vitr. 2013. [Google Scholar] [CrossRef]
- Katoh, M.; Uemura, N.; Hamajima, F.; Ogasawara, T.; Hata, K. ichiro Morphological Characterization of a Reconstructed Human Corneal Epithelial Model (LabCyte CORNEA-MODEL) as an Alternative to the Draize Eye Test for the Assessment of Eye Irritation. Altern. Anim. Test. Exp. 2012, 17, 2–8. [Google Scholar] [CrossRef]
- Nakahara, S.; Kojima, H.; Omori, T.; Yamashita, A.; Endo, M.; Satake, M.; Nishiura, H.; Shinoda, S.; Hagiwara, S.; Kasahara, T.; et al. A Validation Study of a New In Vitro Eye Irritation Test using the Reconstructed Human Corneal Epithelial Tissue, LabCyte CORNEA-MODEL24. Altern. Anim. Test. Exp. 2019, 24, 11–23. [Google Scholar] [CrossRef]
- Han, B.; Schwab, I.R.; Madsen, T.K.; Isseroff, R.R. A fibrin-based bioengineered ocular surface with human corneal epithelial stem cells. Cornea 2002. [Google Scholar] [CrossRef] [PubMed]
- Kaluzhny, Y.; Kinuthia, M.W.; Truong, T.; Lapointe, A.M.; Hayden, P.; Klausner, M. New human organotypic corneal tissue model for ophthalmic drug delivery studies. Investig. Ophthalmol. Vis. Sci. 2018. [Google Scholar] [CrossRef] [Green Version]
- Kaluzhny, Y.; Kinuthia, M.W.; Lapointe, A.M.; Truong, T.; Klausner, M.; Hayden, P. Oxidative stress in corneal injuries of different origin: Utilization of 3D human corneal epithelial tissue model. Exp. Eye Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chacón, M.; Vázquez, N.; Berisa, S.; Persinal, M.; Sánchez, M.; Baamonde, B.; Alfonso, J.F.; Fernández-Vega Cueto, L.; Merayo-Lloves, J.; Meana, Á. QobuR–A new in vitro human corneal epithelial model for preclinical drug screening. Eur. J. Pharm. Biopharm. 2019. [Google Scholar] [CrossRef]
- Postnikoff, C.K.; Pintwala, R.; Williams, S.; Wright, A.M.; Hileeto, D.; Gorbet, M.B. Development of a curved, stratified, in vitro model to assess ocular biocompatibility. PLoS ONE 2014. [Google Scholar] [CrossRef]
- Agarwal, P.; Rupenthal, I.D. In vitro and ex vivo corneal penetration and absorption models. Drug Deliv. Transl. Res. 2016, 6, 634–647. [Google Scholar] [CrossRef] [PubMed]
- Rönkkö, S.; Vellonen, K.S.; Järvinen, K.; Toropainen, E.; Urtti, A. Human corneal cell culture models for drug toxicity studies. Drug Deliv. Transl. Res. 2016, 6, 660–675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reichl, S.; Kölln, C.; Hahne, M.; Verstraelen, J. In vitro cell culture models to study the corneal drug absorption. Expert Opin. Drug Metab. Toxicol. 2011, 7, 559–578. [Google Scholar] [CrossRef]
- Reichl, S.; Becker, U. Cell Culture Models of the Corneal Epithelium and Reconstructed Cornea Equivalents for In Vitro Drug Absorption Studies. In Drug Absorption Studies; Ehrhardt, C., Kim, K.J., Eds.; Springer: Boston, MA, USA, 2007; Biotechnology: Pharmaceutical Aspects; Volume VII. [Google Scholar] [CrossRef]
- Reichl, S. Cell culture models of the human cornea—A comparative evaluation of their usefulness to determine ocular drug absorption in-vitro. J. Pharm. Pharmacol. 2008. [Google Scholar] [CrossRef] [PubMed]
- Dey, S. Corneal cell culture models: A tool to study corneal drug absorption. Expert Opin. Drug Metab. Toxicol. 2011, 7, 529–532. [Google Scholar] [CrossRef] [PubMed]
- Toropainen, E.; Ranta, V.P.; Talvitte, A.; Suhonen, P.; Urtti, A. Culture model of human corneal epithelium for prediction of ocular drug absorption. Investig. Ophthalmol. Vis. Sci. 2001, 42, 2942–2948. [Google Scholar]
- Wilson, S.E. Bowman’s layer in the cornea– structure and function and regeneration. Exp. Eye Res. 2020. [Google Scholar] [CrossRef]
- Guo, X.; Hutcheon, A.E.K.; Melotti, S.A.; Zieske, J.D.; Trinkaus-Randall, V.; Ruberti, J.W. Morphologic characterization of organized extracellular matrix deposition by ascorbic acid-stimulated human corneal fibroblasts. Investig. Ophthalmol. Vis. Sci. 2007. [Google Scholar] [CrossRef]
- Ren, R.; Hutcheon, A.E.K.; Guo, X.Q.; Saeidi, N.; Melotti, S.A.; Ruberti, J.W.; Zieske, J.D.; Trinkaus-Randall, V. Human primary corneal fibroblasts synthesize and deposit proteoglycans in long-term 3-D cultures. Dev. Dyn. 2008. [Google Scholar] [CrossRef] [Green Version]
- Saika, S. Ultrastructural effect of L-ascorbic acid 2-phosphate on cultured keratocytes. Cornea 1992, 11. [Google Scholar] [CrossRef]
- Karamichos, D.; Guo, X.Q.; Hutcheon, A.E.K.; Zieske, J.D. Human corneal fibrosis: An in vitro model. Investig. Ophthalmol. Vis. Sci. 2010. [Google Scholar] [CrossRef] [Green Version]
- Karamichos, D.; Zareian, R.; Guo, X.; Hutcheon, A.; Ruberti, J.; Zieske, J. Novel in Vitro Model for Keratoconus Disease. J. Funct. Biomater. 2012. [Google Scholar] [CrossRef] [Green Version]
- Priyadarsini, S.; Sarker-Nag, A.; Rowsey, T.G.; Ma, J.X.; Karamichos, D. Establishment of a 3D In vitro model to accelerate the development of human therapies against corneal diabetes. PLoS ONE 2016. [Google Scholar] [CrossRef]
- Sharif, R.; Priyadarsini, S.; Rowsey, T.G.; Ma, J.X.; Karamichos, D. Corneal tissue engineering: An in vitro model of the stromal-nerve interactions of the human cornea. J. Vis. Exp. 2018, 2018. [Google Scholar] [CrossRef]
- Isaacson, A.; Swioklo, S.; Connon, C.J. 3D bioprinting of a corneal stroma equivalent. Exp. Eye Res. 2018. [Google Scholar] [CrossRef] [PubMed]
- Joyce, N.C. Proliferative capacity of the corneal endothelium. Prog. Retin. Eye Res. 2003, 95, 16–23. [Google Scholar] [CrossRef]
- Joyce, N.C. Proliferative capacity of corneal endothelial cells. Exp. Eye Res. 2012. [Google Scholar] [CrossRef] [Green Version]
- Hutcheon, A.E.K.; Zieske, J.D.; Guo, X. 3D in vitro model for human corneal endothelial cell maturation. Exp. Eye Res. 2019. [Google Scholar] [CrossRef]
- Arnalich-Montiel, F.; Moratilla, A.; Fuentes-Julián, S.; Aparicio, V.; Martin, M.C.; Peh, G.; Mehta, J.S.; Adnan, K.; Porrua, L.; Pérez-Sarriegui, A.; et al. Treatment of corneal endothelial damage in a rabbit model with a bioengineered graft using human decellularized corneal lamina and cultured human corneal endothelium. PLoS ONE 2019, 14. [Google Scholar] [CrossRef]
- Griffith, M.; Osborne, R.; Hunger, R.; Xiong, X.; Doillon, C.J.; Laycock, N.L.C.; Hakim, M.; Song, Y.; Watsky, M.A. Functional human corneal equivalents constructed from cell lines. Science 1999. [Google Scholar] [CrossRef]
- Proulx, S.; Uwamaliya, J.D.A.; Carrier, P.; Deschambeault, A.; Audet, C.; Giasson, C.J.; Guérin, S.L.; Auger, F.A.; Germain, L. Reconstruction of a human cornea by the self-assembly approach of tissue engineering using the three native cell types. Mol. Vis. 2010, 16, 2192–2201. [Google Scholar]
- Garzón, I.; Martín-Piedra, M.A.; Alfonso-Rodríguez, C.; Gonźalez-Andrades, M.; Carriel, V.; Martínez-Gómez, C.; Campos, A.; Alaminos, M. Generation of a biomimetic human artificial cornea model using wharton’s jelly mesenchymal stem cells. Investig. Ophthalmol. Vis. Sci. 2014. [Google Scholar] [CrossRef] [Green Version]
- González-Andrades, M.; Garzón, I.; Gascón, M.I.; Muñoz-Ávila, J.I.; Sánchez-Quevedo, M.C.; Campos, A.; Alaminos, M. Sequential development of intercellular junctions in bioengineered human corneas. J. Tissue Eng. Regen. Med. 2009. [Google Scholar] [CrossRef]
- De La Cruz Cardona, J.; Ionescu, A.M.; Gómez-Sotomayor, R.; González-Andrades, M.; Campos, A.; Alaminos, M.; Pérez, M.D.M. Transparency in a fibrin and fibrin-agarose corneal stroma substitute generated by tissue engineering. Cornea 2011. [Google Scholar] [CrossRef]
- Rico-Sánchez, L.; Garzón, I.; González-Andrades, M.; Ruíz-García, A.; Punzano, M.; Lizana-Moreno, A.; Muñoz-Ávila, J.I.; Sánchez-Quevedo, M.d.C.; Martínez-Atienza, J.; Lopez-Navas, L.; et al. Successful development and clinical translation of a novel anterior lamellar artificial cornea. J. Tissue Eng. Regen. Med. 2019. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Ghezzi, C.E.; Gomes, R.; Pollard, R.E.; Funderburgh, J.L.; Kaplan, D.L. In vitro 3D corneal tissue model with epithelium, stroma, and innervation. Biomaterials 2017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siran, W.; Ghezzi, C.E.; Cairns, D.M.; Pollard, R.E.; Chen, Y.; Gomes, R.; McKay, T.B.; Pouli, D.; Jamali, A.; Georgakoudi, I.; et al. Human Corneal Tissue Model for Nociceptive Assessments. Adv. Healthc. Mater. 2018. [Google Scholar] [CrossRef]
- Deardorff, P.M.; McKay, T.B.; Wang, S.; Ghezzi, C.E.; Cairns, D.M.; Abbott, R.D.; Funderburgh, J.L.; Kenyon, K.R.; Kaplan, D.L. Modeling Diabetic Corneal Neuropathy in a 3D In Vitro Cornea System. Sci. Rep. 2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKay, T.B.; Ford, A.; Wang, S.; Cairns, D.M.; Parker, R.N.; Deardorff, P.M.; Ghezzi, C.E.; Kaplan, D.L. Assembly and Application of a Three-Dimensional Human Corneal Tissue Model. Curr. Protoc. Toxicol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Scott, L.; Eskes, C.; Hoffmann, S.; Adriaens, E.; Alepée, N.; Bufo, M.; Clothier, R.; Facchini, D.; Faller, C.; Guest, R.; et al. A proposed eye irritation testing strategy to reduce and replace in vivo studies using Bottom-Up and Top-Down approaches. Toxicol. Vitr. 2010, 24, 1–9. [Google Scholar] [CrossRef]
- Beiβner, N.; Mattern, K.; Dietzel, A.; Reichl, S. DynaMiTES—A dynamic cell culture platform for in vitro drug testing PART 2—Ocular DynaMiTES for drug absorption studies of the anterior eye. Eur. J. Pharm. Biopharm. 2018. [Google Scholar] [CrossRef] [Green Version]
- Reichl, S.; Döhring, S.; Bednarz, J.; Müller-Goymann, C.C. Human cornea construct HCC-An alternative for in vitro permeation studies? A comparison with human donor corneas. Eur. J. Pharm. Biopharm. 2005, 60, 305–308. [Google Scholar] [CrossRef]
- Hahne, M.; Zorn-Kruppa, M.; Guzman, G.; Brandner, J.M.; Haltner-Ukomado, E.; Wätzig, H.; Reichl, S. Prevalidation of a human cornea construct as an alternative to animal corneas for in vitro drug absorption studies. J. Pharm. Sci. 2012. [Google Scholar] [CrossRef]
- Hahne, M.; Reichl, S. Development of a serum-free human cornea construct for in vitro drug absorption studies: The influence of varying cultivation parameters on barrier characteristics. Int. J. Pharm. 2011. [Google Scholar] [CrossRef] [PubMed]
- Araki-Sasaki, K.; Ohashi, Y.; Sasabe, T.; Hayashi, K.; Watanabe, H.; Tano, Y.; Handa, H. An SV40-immortalized human corneal epithelial cell line and its characterization. Investig. Ophthalmol. Vis. Sci. 1995, 36, 614–621. [Google Scholar]
- Zorn-Kruppa, M.; Tykhonova, S.; Beige, G.; Bednarz, J.; Diehl, H.A.; Engelke, M. A human corneal equivalent constructed from SV40-immortalised corneal cell lines. ATLA Altern. Lab. Anim. 2005. [Google Scholar] [CrossRef] [PubMed]
- Stepp, M.A.; Zieske, J.D.; Trinkaus-Randall, V.; Kyne, B.M.; Pal-Ghosh, S.; Tadvalkar, G.; Pajoohesh-Ganji, A. Wounding the cornea to learn how it heals. Exp. Eye Res. 2014, 121, 178–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, C.C.; Park, A.Y.; Guan, J.L. In vitro scratch assay: A convenient and inexpensive method for analysis of cell migration in vitro. Nat. Protoc. 2007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalez-Andrades, M.; Alonso-Pastor, L.; Mauris, J.; Cruzat, A.; Dohlman, C.H.; Argüeso, P. Establishment of a novel in vitro model of stratified epithelial wound healing with barrier function. Sci. Rep. 2016. [Google Scholar] [CrossRef] [Green Version]
- McKay, T.B.; Karamichos, D.; Zieske, J.D.; Hutcheon, A.E.K.; Guo, X. Corneal epithelial–stromal fibroblast constructs to study cell–cell communication in vitro. Bioengineering 2019. [Google Scholar] [CrossRef] [Green Version]
- Sorkio, A.; Koch, L.; Koivusalo, L.; Deiwick, A.; Miettinen, S.; Chichkov, B.; Skottman, H. Human stem cell based corneal tissue mimicking structures using laser-assisted 3D bioprinting and functional bioinks. Biomaterials 2018. [Google Scholar] [CrossRef]
- Engelke, M.; Zorn-Kruppa, M.; Gabel, D.; Reisinger, K.; Rusche, B.; Mewes, K.R. A human hemi-cornea model for eye irritation testing: Quality control of production, reliability and predictive capacity. Toxicol. Vitro 2013. [Google Scholar] [CrossRef]
- Yamaguchi, H.; Takezawa, T. Fabrication of a corneal model composed of corneal epithelial and endothelial cells via a collagen vitrigel membrane functioned as an acellular stroma and its application to the corneal permeability test of chemicals. Drug Metab. Dispos. 2018. [Google Scholar] [CrossRef] [Green Version]
- Levis, H.J.; Brown, R.A.; Daniels, J.T. Plastic compressed collagen as a biomimetic substrate for human limbal epithelial cell culture. Biomaterials 2010. [Google Scholar] [CrossRef] [PubMed]
- Massie, I.; Dale, S.B.; Daniels, J.T. Limbal Fibroblasts Maintain Normal Phenotype in 3D RAFT Tissue Equivalents Suggesting Potential for Safe Clinical Use in Treatment of Ocular Surface Failure. Tissue Eng. Part C Methods 2015, 21, 576–584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massie, I.; Levis, H.J.; Daniels, J.T. Response of human limbal epithelial cells to wounding on 3D RAFT tissue equivalents: Effect of airlifting and human limbal fibroblasts. Exp. Eye Res. 2014. [Google Scholar] [CrossRef] [PubMed]
- Levis, H.J.; Massie, I.; Dziasko, M.A.; Kaasi, A.; Daniels, J.T. Rapid tissue engineering of biomimetic human corneal limbal crypts with 3D niche architecture. Biomaterials 2013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steuhl, K.P. Ultrastructure of the conjunctival epithelium. Dev. Ophthalmol. 1989, 19, 1–104. [Google Scholar] [PubMed]
- Dartt, D.A. Regulation of mucin and fluid secretion by conjunctival epithelial cells. Prog. Retin. Eye Res. 2002, 21, 555–576. [Google Scholar] [CrossRef]
- Inatomi, T.; Spurr-Michaud, S.; Tisdale, A.S.; Zhan, Q.; Feldman, S.T.; Gipson, I.K. Expression of secretory mucin genes by human conjunctival epithelia. Investig. Ophthalmol. Vis. Sci. 1996, 37, 1684–1692. [Google Scholar]
- Diebold, Y.; Calonge, M. Characterization of epithelial primary cultures from human conjunctiva. Graefe’s Arch. Clin. Exp. Ophthalmol. 1997. [Google Scholar] [CrossRef] [PubMed]
- Diebold, Y.; Calonge, M.; Callejo, S.; Lázaro, M.C.; Bringas, R.; Herreras, J.M. Ultrastructural evidence of mucus in human conjunctival epithelial cultures. Curr. Eye Res. 1999. [Google Scholar] [CrossRef] [PubMed]
- Risse Marsh, B.C.; Massaro-Giordano, M.; Marshall, C.M.; Lavker, R.M.; Jensen, P.J. Initiation and characterization of keratinocyte cultures from biopsies of normal human conjunctiva. Exp. Eye Res. 2002. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Osorio, H.; Calonge, M.; Corell, A.; Reinoso, R.; López, A.; Fernández, I.; San José, E.G.; Diebold, Y. Characterization and short-term culture of cells recovered from human conjunctival epithelium by minimally invasive means. Mol. Vis. 2009, 15, 2185–2195. [Google Scholar]
- Shatos, M.A.; Ríos, J.D.; Horikawa, Y.; Hodges, R.R.; Chang, E.L.; Bernardino, C.R.; Rubin, P.A.D.; Dartt, D.A. Isolation and characterization of cultured human conjunctival goblet cells. Investig. Ophthalmol. Vis. Sci. 2003. [Google Scholar] [CrossRef] [Green Version]
- Li, D.; Hodges, R.R.; Jiao, J.; Carozza, R.B.; Shatos, M.A.; Chiang, N.; Serhan, C.N.; Dartt, D.A. Resolvin D1 and aspirin-triggered resolvin D1 regulate histamine-stimulated conjunctival goblet cell secretion. Mucosal Immunol. 2013. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Posadas, L.; Hodges, R.R.; Li, D.; Shatos, M.A.; Storr-Paulsen, T.; Diebold, Y.; Dartt, D.A. Interaction of IFN-[gamma] with cholinergic agonists to modulate rat and human goblet cell function. Mucosal Immunol. 2016, 9, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Dartt, D.A.; Hodges, R.R.; Li, D.; Shatos, M.A.; Lashkari, K.; Serhan, C.N. Conjunctival Goblet Cell Secretion Stimulated by Leukotrienes Is Reduced by Resolvins D1 and E1 To Promote Resolution of Inflammation. J. Immunol. 2011. [Google Scholar] [CrossRef] [Green Version]
- García-Posadas, L.; Arranz-Valsero, I.; López-García, A.; Soriano-Romaní, L.; Diebold, Y. A new human primary epithelial cell culture model to study conjunctival inflammation. Investig. Ophthalmol. Vis. Sci. 2013, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soriano-Romaní, L.; Contreras-Ruiz, L.; García-Posadas, L.; López-García, A.; Masli, S.; Diebold, Y. Inflammatory Cytokine-Mediated Regulation of Thrombospondin-1 and CD36 in Conjunctival Cells. J. Ocul. Pharmacol. Ther. 2015, 31, 419–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soriano-Romaní, L.; Álvarez-Trabado, J.; López-García, A.; Molina-Martínez, I.; Herrero-Vanrell, R.; Diebold, Y. Improved in vitro corneal delivery of a thrombospondin-1-derived peptide using a liposomal formulation. Exp. Eye Res. 2018. [Google Scholar] [CrossRef] [PubMed]
- Eidet, J.; Dartt, D.; Utheim, T. Concise Review: Comparison of Culture Membranes Used for Tissue Engineered Conjunctival Epithelial Equivalents. J. Funct. Biomater. 2015, 6, 1064–1084. [Google Scholar] [CrossRef]
- Ang, L.P.K.; Tanioka, H.; Kawasaki, S.; Ang, L.P.S.; Yamasaki, K.; Do, T.P.; Thein, Z.M.; Koizumi, N.; Nakamura, T.; Yokoi, N.; et al. Cultivated human conjunctival epithelial transplantation for total limbal stem cell deficiency. Investig. Ophthalmol. Vis. Sci. 2010, 51, 758–764. [Google Scholar] [CrossRef]
- Ang, L.P.K.; Tan, D.T.H.; Beuerman, R.W.; Lavker, R.M. Development of a conjunctival epithelial equivalent with improved proliferative properties using a multistep serum-free culture system. Investig. Ophthalmol. Vis. Sci. 2004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niiya, A.; Matsumoto, Y.; Ishibashi, T.; Matsumoto, K.; Kinoshita, S. Collagen gel-embedding culture of conjunctival epithelial cells. Graefe’s Arch. Clin. Exp. Ophthalmol. 1997, 235, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Drechsler, C.C.; Kunze, A.; Kureshi, A.; Grobe, G.; Reichl, S.; Geerling, G.; Daniels, J.T.; Schrader, S. Development of a conjunctival tissue substitute on the basis of plastic compressed collagen. J. Tissue Eng. Regen. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Witt, J.; Borrelli, M.; Mertsch, S.; Geerling, G.; Spaniol, K.; Schrader, S. Evaluation of Plastic-Compressed Collagen for Conjunctival Repair in a Rabbit Model. Tissue Eng. Part A 2019. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Lu, Q.; Guo, Q.; Chae, J.; Fan, X.; Elisseeff, J.H.; Grant, M.P. Vitrified collagen-based conjunctival equivalent for ocular surface reconstruction. Biomaterials 2014, 35, 7398–7406. [Google Scholar] [CrossRef] [PubMed]
- Yao, Q.; Zhang, W.; Hu, Y.; Chen, J.; Shao, C.; Fan, X.; Fu, Y. Electrospun collagen/poly (L-lactic acid-co-ε-caprolactone) scaffolds for conjunctival tissue engineering. Exp. Ther. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Bertolin, M.; Breda, C.; Ferrari, S.; Van Acker, S.I.; Zakaria, N.; Di Iorio, E.; Migliorati, A.; Ponzin, D.; Ferrari, B.; Lužnik, Z.; et al. Optimized protocol for regeneration of the conjunctival epithelium using the cell suspension technique. Cornea 2019. [Google Scholar] [CrossRef]
- Yao, Q.; Hu, Y.; Yu, F.; Zhang, W.; Fu, Y. A novel application of electrospun silk fibroin/poly(l-lactic acid-: Co-ϵ-caprolactone) scaffolds for conjunctiva reconstruction. RSC Adv. 2018. [Google Scholar] [CrossRef] [Green Version]
- Zhu, X.; Beuerman, R.W.; Chan-Park, M.B.E.; Cheng, Z.; Ang, L.P.K.; Tan, D.T.H. Enhancement of the mechanical and biological properties of a biomembrane for tissue engineering the ocular surface. Ann. Acad. Med. Singap. 2006, 35, 210–214. [Google Scholar]
- Yoshizawa, M.; Feinberg, S.E.; Marcelo, C.L.; Elner, V.M. Ex vivo produced human conjunctiva and oral mucosa equivalents grown in a serum-free culture system. J. Oral. Maxillofac. Surg. 2004, 62, 980–988. [Google Scholar] [CrossRef]
- Schrader, S.; Notara, M.; Beaconsfield, M.; Tuft, S.J.; Daniels, J.T.; Geerling, G. Tissue engineering for conjunctival reconstruction: Established methods and future outlooks. Curr. Eye Res. 2009, 34, 913–924. [Google Scholar] [CrossRef] [PubMed]
- Saha, P.; Kim, K.J.; Lee, V.H.L. A primary culture model of rabbit conjunctival epithelial cells exhibiting tight barrier properties. Curr. Eye Res. 1996. [Google Scholar] [CrossRef] [PubMed]
- Saha, P.; Uchiyama, T.; Kim, K.-J.; Lee, V.H.L. Permeability characteristics of primary cultured rabbit conjunctival epithelial cells to low molecular weight drugs. Curr. Eye Res. 1996, 15, 1170–1174. [Google Scholar] [CrossRef] [PubMed]
- Civiale, C.; Paladino, G.; Marino, C.; Trombetta, F.; Pulvirenti, T.; Enea, V. Multilayer primary epithelial cell culture from bovine conjunctiva as a model for in vitro toxicity tests. Ophthalmic Res. 2003. [Google Scholar] [CrossRef]
- Chung, S.H.; Lee, J.H.; Yoon, J.H.; Lee, H.K.; Seo, K.Y. Multi-layered culture of primary human conjunctival epithelial cells producing MUC5AC. Exp. Eye Res. 2007, 85, 226–233. [Google Scholar] [CrossRef]
- Rosellini, A.; Papini, S.; Giannarini, C.; Nardi, M.; Revoltella, R.P. Human conjunctival epithelial precursor cells and their progeny in 3D organotypic culture. Int. J. Dev. Biol. 2007, 51, 739–743. [Google Scholar] [CrossRef] [Green Version]
- Papini, S.; Rosellini, A.; Nardi, M.; Giannarini, C.; Revoltella, R.P. Selective growth and expansion of human corneal epithelial basal stem cells in a three-dimensional-organ culture. Differentiation 2005. [Google Scholar] [CrossRef]
- Gipson, I.K.; Spurr-Michaud, S.; Argüeso, P.; Tisdale, A.; Ng, T.F.; Russo, C.L. Mucin gene expression in immortalized human corneal-limbal and conjunctival epithelial cell lines. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2496–2506. [Google Scholar] [CrossRef]
- Zorn-Kruppa, M.; Houdek, P.; Wladykowski, E.; Engelke, M.; Bartok, M.; Mewes, K.R.; Moll, I.; Brner, J.M. Determining the depth of injury in bioengineered tissue models of cornea and conjunctiva for the prediction of all three ocular GHS categories. PLoS ONE 2014. [Google Scholar] [CrossRef] [Green Version]
- Fiorentzis, M.; Katopodis, P.; Kalirai, H.; Seitz, B.; Viestenz, A.; Coupland, S.E. Conjunctival melanoma and electrochemotherapy: Preliminary results using 2D and 3D cell culture models in vitro. Acta Ophthalmol. 2019. [Google Scholar] [CrossRef] [Green Version]
- García-Posadas, L.; Soriano-Romaní, L.; López-Garcí, A.; Diebold, Y. An engineered human conjunctival-like tissue to study ocular surface inflammatory diseases. PLoS ONE 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Tsai, R.J.F.; Ho, Y.S.; Chen, J.K. The effects of fibroblasts on the growth and differentiation of human bulbar conjunctival epithelial cells in an in vitro conjunctival equivalent. Investig. Ophthalmol. Vis. Sci. 1994, 35, 2865–2875. [Google Scholar]
- Mitani, A.; Kobayashi, T.; Hayashi, Y.; Matsushita, N.; Matsushita, S.; Nakao, S.; Takahira, N.; Shiraishi, A.; Ohashi, Y. Characterization of doxycycline-dependent inducible Simian Virus 40 large T antigen immortalized human conjunctival epithelial cell line. PLoS ONE 2019. [Google Scholar] [CrossRef] [PubMed]
- Damato, B.; Coupland, S.E. Management of conjunctival melanoma. Expert Rev. Anticancer Ther. 2009, 9, 1227–1239. [Google Scholar] [CrossRef] [PubMed]
- Norregaard, J.C.; Gerner, N.; Jensen, O.A.; Prause, J.U. Malignant melanoma of the conjunctiva: Occurrence and survival following surgery and radiotherapy in a Danish population. Graefe’s Arch. Clin. Exp. Ophthalmol. 1996. [Google Scholar] [CrossRef]
- Refaian, N.; Schlereth, S.L.; Koch, K.R.; Notara, M.; Hos, D.; Mescher, M.; Iden, S.; Bosch, J.J.; Jager, M.J.; Cursiefen, C.; et al. Comparing the hem- and lymphangiogenic profile of conjunctival and uveal melanoma cell lines. Investig. Ophthalmol. Vis. Sci. 2015. [Google Scholar] [CrossRef] [Green Version]
- Angi, M.; Versluis, M.; Kalirai, H. Culturing Uveal Melanoma Cells. Ocul. Oncol. Pathol. 2015. [Google Scholar] [CrossRef] [Green Version]
- Valyi-Nagy, K.; Dosa, S.; Kovacs, S.K.; Bacsa, S.; Voros, A.; Shukla, D.; Folberg, R.; Valyi-Nagy, T. Identification of virus resistant tumor cell subpopulations in three-dimensional uveal melanoma cultures. Cancer Gene Ther. 2010. [Google Scholar] [CrossRef] [Green Version]
- Fiorentzis, M.; Viestenz, A.; Siebolts, U.; Seitz, B.; Coupland, S.E.; Heinzelmann, J. The potential use of electrochemotherapy in the treatment of uveal melanoma: In vitro results in 3D tumor cultures and in vivo results in a chick embryo model. Cancers 2019. [Google Scholar] [CrossRef] [Green Version]
- Fiorentzis, M.; Katopodis, P.; Kalirai, H.; Seitz, B.; Viestenz, A.; Coupland, S.E. Image Analysis of 3D Conjunctival Melanoma Cell Cultures Following Electrochemotherapy. Biomedicines 2020. [Google Scholar] [CrossRef]
- Polansky, J.R.; Wood, I.S.; Maglio, M.T.; Alvarado, J.A. Trabecular Meshwork Cell Culture in Glaucoma Research: Evaluation of Biological Activity and Structural Properties of Human Trabecular Cells In Vitro. Ophthalmology 1984. [Google Scholar] [CrossRef]
- Pang, I.H.; Shade, D.L.; Clark, A.F.; Steely, H.T.; Desantis, L. Preliminary characterization of a transformed cell strain derived from human trabecular meshwork. Curr. Eye Res. 1994. [Google Scholar] [CrossRef] [PubMed]
- Torrejon, K.Y.; Pu, D.; Bergkvist, M.; Danias, J.; Sharfstein, S.T.; Xie, Y. Recreating a human trabecular meshwork outflow system on microfabricated porous structures. Biotechnol. Bioeng. 2013. [Google Scholar] [CrossRef] [PubMed]
- Torrejon, K.Y.; Papke, E.L.; Halman, J.R.; Stolwijk, J.; Dautriche, C.N.; Bergkvist, M.; Danias, J.; Sharfstein, S.T.; Xie, Y. Bioengineered glaucomatous 3D human trabecular meshwork as an in vitro disease model. Biotechnol. Bioeng. 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouchemi, M.; Roubeix, C.; Kessal, K.; Riancho, L.; Raveu, A.L.; Soualmia, H.; Baudouin, C.; Brignole-Baudouin, F. Effect of benzalkonium chloride on trabecular meshwork cells in a new in vitro 3D trabecular meshwork model for glaucoma. Toxicol. Vitr. 2017. [Google Scholar] [CrossRef] [PubMed]
- Vernazza, S.; Tirendi, S.; Scarfi, S.; Passalacqua, M.; Oddone, F.; Traverso, C.E.; Rizzato, I.; Bassi, A.M.; Sacca, S.C. 2D-A nd 3D-cultures of human trabecular meshwork cells: A preliminary assessment of an in vitro model for glaucoma study. PLoS ONE 2019. [Google Scholar] [CrossRef] [PubMed]
- Saccà, S.C.; Izzotti, A. Focus on molecular events in the anterior chamber leading to glaucoma. Cell. Mol. Life Sci. 2014, 71, 2197–2280. [Google Scholar] [CrossRef]
- Waduthanthri, K.D.; He, Y.; Montemagno, C.; Cetinel, S. An injectable peptide hydrogel for reconstruction of the human trabecular meshwork. Acta Biomater. 2019. [Google Scholar] [CrossRef]
- Yemanyi, F.; Vranka, J.; Raghunathan, V.K. Generating cell-derived matrices from human trabecular meshwork cell cultures for mechanistic studies. Methods Cell Biol. 2020, 156, 271–307. [Google Scholar] [CrossRef]
- Braunger, B.M.; Ademoglu, B.; Koschade, S.E.; Fuchshofer, R.; Gabelt, B.T.; Kiland, J.A.; Hennes-Beann, E.A.; Brunner, K.G.; Kaufman, P.L.; Tamm, E.R. Identification of adult stem cells in Schwalbe’s line region of the primate eye. Invest. Ophthalmol. Vis. Sci. 2014. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Cai, S.; Tseng, S.C.G.; Zhu, Y.T. Isolation and Expansion of Multipotent Progenitors from Human Trabecular Meshwork. Sci. Rep. 2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarrin, M.; Young, L.; Wu, W.; Girkin, J.M.; Quinlan, R.A. In vivo, Ex Vivo, and in Vitro Approaches to Study Intermediate Filaments in the Eye Lens. Methods Enzymol. 2016, 568, 581–611. [Google Scholar] [CrossRef] [PubMed]
- Eguchi, G. “Transdifferentiation” of vertebrate cells in cell culture. CIBA Found. Symp. 1976, 40, 241–258. [Google Scholar] [CrossRef]
- Tsonis, P.A.; Jang, W.; Del Rio-Tsonis, K.; Eguchi, G. A unique aged human retinal pigmented epithelial cell line useful for studying lens differentiation in vitro. Int. J. Dev. Biol. 2001. [Google Scholar] [CrossRef]
- Eguchi, G. Chapter 9 Lens transdifferentiation in the vertebrate retinal pigmented epithelial cell. Prog. Retin. Res. 1993, 12, 205–230. [Google Scholar] [CrossRef]
- De Vries, A.C.J.; Vermeer, M.A.; Hendriks, A.L.A.M.; Bloemendal, H.; Cohen, L.H. Biosynthetic capacity of the human lens upon aging. Exp. Eye Res. 1991. [Google Scholar] [CrossRef]
- Wormstone, I.M.; Liu, C.S.C.; Rakic, J.M.; Marcantonio, J.M.; Vrensen, G.F.J.M.; Duncan, G. Human lens epithelial cell proliferation in a protein-free medium. Investig. Ophthalmol. Vis. Sci. 1997, 38, 396–404. [Google Scholar]
- Liu, C.S.C.; Wormstone, I.M.; Duncan, G.; Marcantonio, J.M.; Webb, S.F.; Davies, P.D. A study of human lens cell growth in vitro: A model for posterior capsule opacification. Investig. Ophthalmol. Vis. Sci. 1996, 37, 906–914. [Google Scholar]
- Marcantonio, J.M.; Rakic, J.M.; Vrensen, G.F.J.M.; Duncan, G. Lens cell populations studied in human donor capsular bags with implanted intraocular lenses. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1130–1141. [Google Scholar]
- Collison, D.J.; Wang, L.; Wormstone, I.M.; Duncan, G. Spatial Characteristics of Receptor-Induced Calcium Signaling in Human Lens Capsular Bags. Investig. Ophthalmol. Vis. Sci. 2004. [Google Scholar] [CrossRef] [Green Version]
- James, C.; Collison, D.J.; Duncan, G. Characterization and functional activity of thrombin receptors in the human lens. Investig. Ophthalmol. Vis. Sci. 2005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Augusteyn, R.C.; Rosen, A.M.; Borja, D.; Ziebarth, N.M.; Parel, J.M. Biometry of primate lenses during immersion in preservation media. Mol. Vis. 2006, 12, 740–747. [Google Scholar] [PubMed]
- Andjelic, S.; Lumi, X.; Veréb, Z.; Josifovska, N.; Facskó, A.; Hawlina, M.; Petrovski, G. A Simple Method for Establishing Adherent Ex Vivo Explant Cultures from Human Eye Pathologies for Use in Subsequent Calcium Imaging and Inflammatory Studies. J. Immunol. Res. 2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galal, A.; Perez-Santonja, J.J.; Rodriguez-Prats, J.L.; Abad, M.; Alio, J. Human anterior lens capsule as a biologic substrate for the ex vivo expansion of limbal stem cells in ocular surface reconstruction. Cornea 2007. [Google Scholar] [CrossRef] [PubMed]
- Albert, R.; Veréb, Z.; Csomós, K.; Moe, M.C.; Johnsen, E.O.; Olstad, O.K.; Nicolaissen, B.; Rajnavölgyi, É.; Fésüs, L.; Berta, A.; et al. Cultivation and Characterization of Cornea Limbal Epithelial Stem Cells on Lens Capsule in Animal Material-Free Medium. PLoS ONE 2012. [Google Scholar] [CrossRef] [Green Version]
- Yoeruek, E.; Saygili, O.; Spitzer, M.S.; Tatar, O.; Bartz-Schmidt, K.U. Human anterior lens capsule as carrier matrix for cultivated human corneal endothelial cells. Cornea 2009. [Google Scholar] [CrossRef]
- Andjelic, S.; Drašlar, K.; Lumi, X.; Yan, X.; Graw, J.; Facskõ, A.; Hawlina, M.; Petrovski, G. Morphological and proliferative studies on ex vivo cultured human anterior lens epithelial cells-Relevance to capsular opacification. Acta Ophthalmol. 2015. [Google Scholar] [CrossRef] [Green Version]
- Luft, N.; Kreutzer, T.C.; Dirisamer, M.; Priglinger, C.S.; Burger, J.; Findl, O.; Priglinger, S.G. Evaluation of laser capsule polishing for prevention of posterior capsule opacification in a human ex vivo model. J. Cataract Refract. Surg. 2015. [Google Scholar] [CrossRef]
- Wertheimer, C.; Kassumeh, S.; Piravej, N.P.; Nilmayer, O.; Braun, C.; Priglinger, C.; Luft, N.; Wolf, A.; Mayer, W.J.; Priglinger, S.G.; et al. The intraocular lens as a drug delivery device: In vitro screening of pharmacologic substances for the prophylaxis of posterior capsule opacification. Investig. Ophthalmol. Vis. Sci. 2017. [Google Scholar] [CrossRef] [Green Version]
- Recek, N.; Andjelić, S.; Hojnik, N.; Filipič, G.; Lazović, S.; Vesel, A.; Primc, G.; Mozetič, M.; Hawlina, M.; Petrovski, G.; et al. Microplasma induced cell morphological changes and apoptosis of Ex vivo cultured human anterior lens epithelial cells relevance to capsular opacification. PLoS ONE 2016. [Google Scholar] [CrossRef] [Green Version]
- Yang, C.; Yang, Y.; Brennan, L.; Bouhassira, E.E.; Kantorow, M.; Cvekl, A. Efficient generation of lens progenitor cells and lentoid bodies from human embryonic stem cells in chemically defined conditions. FASEB J. 2010. [Google Scholar] [CrossRef] [Green Version]
- Nagineni, C.N.; Bhat, S.P. Lens fiber cell differentiation and expression of crystallins in Co-cultures of human fetal lens epithelial cells and fibroblasts. Exp. Eye Res. 1992. [Google Scholar] [CrossRef]
- Fu, Q.; Qin, Z.; Jin, X.; Zhang, L.; Chen, Z.; He, J.; Ji, J.; Yao, K. Generation of functional lentoid bodies from human induced pluripotent stem cells derived from urinary cells. Investig. Ophthalmol. Vis. Sci. 2017. [Google Scholar] [CrossRef] [Green Version]
- Qin, Z.; Zhang, L.; Lyu, D.; Li, J.; Tang, Q.; Yin, H.; Chen, Z.; Yao, K.; Fu, Q. Opacification of lentoid bodies derived from human induced pluripotent stem cells is accelerated by hydrogen peroxide and involves protein aggregation. J. Cell. Physiol. 2019. [Google Scholar] [CrossRef]
- Lu, Q.; Yin, H.; Grant, M.P.; Elisseeff, J.H. An in Vitro Model for the Ocular Surface and Tear Film System. Sci. Rep. 2017. [Google Scholar] [CrossRef]





| Layer | Milestones | References |
|---|---|---|
| Epithelium | Validation of reconstructed human cornea-like epithelium (RhCE) models for eye irritation tests | [53,54,55,56,57,58,59,60,61,62,63,64,65,66,67] |
| Representation of corneal curvature | [72] | |
| Stroma | Development of models with fibroblasts that produce their own extracellular matrix | [81,82,83,84,85,86] |
| Use of 3D bioprinting to develop corneal equivalents | [88] | |
| Endothelium | Combination of a stromal model with endothelial cells and the presence of Descemet’s membrane | [91] |
| Fabrication of tissue-engineered endothelial grafts using decellularized corneal stroma as scaffolds | [92] | |
| Corneal equivalents | Development of the first 3D model of the whole human cornea | [93] |
| 3D corneal model using human primary cells and the “self-assembly approach” (no use of exogenous material) | [94] | |
| 3D corneal model with epithelium, stroma, and innervation | [99,100,101,102] | |
| Application of dynamic systems to a corneal 3D model | [104] | |
| 3D models of human corneal wound healing | [112,113] | |
| Application of bioprinting to create corneal constructs | [114] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Posadas, L.; Diebold, Y. Three-Dimensional Human Cell Culture Models to Study the Pathophysiology of the Anterior Eye. Pharmaceutics 2020, 12, 1215. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12121215
García-Posadas L, Diebold Y. Three-Dimensional Human Cell Culture Models to Study the Pathophysiology of the Anterior Eye. Pharmaceutics. 2020; 12(12):1215. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12121215
Chicago/Turabian StyleGarcía-Posadas, Laura, and Yolanda Diebold. 2020. "Three-Dimensional Human Cell Culture Models to Study the Pathophysiology of the Anterior Eye" Pharmaceutics 12, no. 12: 1215. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12121215