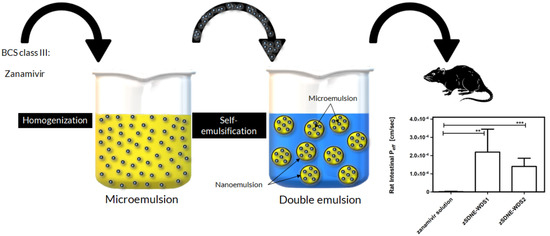
Towards Effective Antiviral Oral Therapy: Development of a Novel Self-Double Emulsifying Drug Delivery System for Improved Zanamivir Intestinal Permeability
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of SDNE-WDSs with or without Drug Cargo
2.2.2. Visualization by Electron Microscope
2.2.3. Confocal Laser Scanning Microscope (CLSM) Imaging
2.2.4. Analysis of Mean Droplet Size and Surface Charge
2.2.5. Small-Angle X-ray Scattering (SAXS)
2.2.6. Determination of Winsor Emulsion Type Using Conductivity Investigation
2.2.7. High-Pressure Liquid Chromatography (HPLC) Analysis of Zanamivir
2.2.8. Quantification of Encapsulation Efficiency
2.2.9. In Vitro Release Studies
2.2.10. Parallel Artificial Membrane Permeability Assay (PAMPA) for Assessing Passive Diffusion of Encapsulated Zanamivir
2.2.11. In Situ Single-Pass Intestinal Perfusion (SPIP) Studies
2.2.12. Data and Statistical Analysis
3. Results
3.1. Preparation and Characterization of Stable Zanamivir-Loaded SDNE-WDSs
3.2. In Vitro Release Studies
3.3. Parallel Artificial Membrane Permeability Assay
3.4. In Situ Single-Pass Intestinal Perfusion Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, R.; Wang, T.; Song, J.; Pu, D.; He, D.; Li, J.; Yang, J.; Li, K.; Zhong, C.; Zhang, J. Antiviral Drug Delivery System for Enhanced Bioactivity, Better Metabolism and Pharmacokinetic Characteristics. Int. J. Nanomed. 2021, 16, 4959–4984. [Google Scholar] [CrossRef]
- Dahan, A.; Miller, J.M.; Amidon, G.L. Prediction of solubility and permeability class membership: Provisional BCS classification of the world’s top oral drugs. AAPS J. 2009, 11, 740–746. [Google Scholar] [CrossRef]
- De Clercq, E.; Li, G. Approved Antiviral Drugs over the Past 50 Years. Clin. Microbiol. Rev. 2016, 29, 695–747. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. Available online: https://www.cdc.gov/flu/weekly/index.htm (accessed on 15 September 2023).
- Samson, M.; Pizzorno, A.; Abed, Y.; Boivin, G. Influenza virus resistance to neuraminidase inhibitors. Antivir. Res. 2013, 98, 174–185. [Google Scholar] [CrossRef]
- Holmes, E.H.; Devalapally, H.; Li, L.; Perdue, M.L.; Ostrander, G.K. Permeability enhancers dramatically increase zanamivir absolute bioavailability in rats: Implications for an orally bioavailable influenza treatment. PLoS ONE 2013, 8, e61853. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Escarpe, P.A.; Eisenberg, E.J.; Cundy, K.C.; Sweet, C.; Jakeman, K.J.; Merson, J.; Lew, W.; Williams, M.; Zhang, L.; et al. Identification of GS 4104 as an orally bioavailable prodrug of the influenza virus neuraminidase inhibitor GS 4071. Antimicrob. Agents Chemother. 1998, 42, 647–653. [Google Scholar] [CrossRef]
- Miller, J.M.; Dahan, A.; Gupta, D.; Varghese, S.; Amidon, G.L. Enabling the intestinal absorption of highly polar antiviral agents: Ion-pair facilitated membrane permeation of zanamivir heptyl ester and guanidino oseltamivir. Mol. Pharm. 2010, 7, 1223–1234. [Google Scholar] [CrossRef]
- Ploger, G.F.; Hofsass, M.A.; Dressman, J.B. Solubility Determination of Active Pharmaceutical Ingredients Which Have Been Recently Added to the List of Essential Medicines in the Context of the Biopharmaceutics Classification System-Biowaiver. J. Pharm. Sci. 2018, 107, 1478–1488. [Google Scholar] [CrossRef]
- Debotton, N.; Garsiani, S.; Cohen, Y.; Dahan, A. Enabling oral delivery of antiviral drugs: Double emulsion carriers to improve the intestinal absorption of zanamivir. Int. J. Pharm. 2022, 629, 122392. [Google Scholar] [CrossRef]
- Colman, P.M. Zanamivir: An influenza virus neuraminidase inhibitor. Expert. Rev. Anti Infect. Ther. 2005, 3, 191–199. [Google Scholar] [CrossRef]
- Food and Drug Administration. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2006/021036s008lbl.pdf#:~:text=Pharmacokinetics%3A%20Absorption%20and%20Bioavailability%3A%20Pharmacokinetic%20studies%20of%20orally,17%25%20of%20the%20inhaled%20dose%20is%20systemically%20absorbed (accessed on 19 September 2023).
- Food and Drug Administration. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/021036s030lbl.pdf (accessed on 19 September 2023).
- Palmer, R. Drugs: Lines of defence. Nature 2011, 480, S9–S10. [Google Scholar] [CrossRef]
- Babadi, D.; Dadashzadeh, S.; Osouli, M.; Daryabari, M.S.; Haeri, A. Nanoformulation strategies for improving intestinal permeability of drugs: A more precise look at permeability assessment methods and pharmacokinetic properties changes. J. Control. Release 2020, 321, 669–709. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Wang, J.; Wang, Y.; Gao, H.; Wei, G.; Huang, Y.; Yu, H.; Gan, Y.; Wang, Y.; Mei, L.; et al. Recent progress in drug delivery. Acta Pharm. Sin. B 2019, 9, 1145–1162. [Google Scholar] [CrossRef]
- Lembo, D.; Cavalli, R. Nanoparticulate delivery systems for antiviral drugs. Antivir. Chem. Chemother. 2010, 21, 53–70. [Google Scholar] [CrossRef] [PubMed]
- Nakano, M. Places of emulsions in drug delivery. Adv. Drug Deliv. Rev. 2000, 45, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, S.; Aqil, M.; Sultana, Y.; Kalam, M.A. Self-nanoemulsifying drug delivery system of nabumetone improved its oral bioavailability and anti-inflammatory effects in rat model. J. Drug Deliv. Sci. Technol. 2019, 51, 736–745. [Google Scholar] [CrossRef]
- Ritschel, W.A. Microemulsion technology in the reformulation of cyclosporine: The reason behind the pharmacokinetic properties of Neoral. Clin. Transplant. 1996, 10, 364–373. [Google Scholar]
- Shaikh, M.S.; Derle, N.D.; Bhamber, R. Permeability Enhancement Techniques for Poorly Permeable Drugs: A Review. J. Appl. Pharm. Sci. 2012, 2, 34–39. [Google Scholar] [CrossRef]
- Lv, L.Z.; Tong, C.Q.; Lv, Q.; Tang, X.J.; Li, L.M.; Fang, Q.X.; Yu, J.; Han, M.; Gao, J.Q. Enhanced absorption of hydroxysafflor yellow A using a self-double-emulsifying drug delivery system: In vitro and in vivo studies. Int. J. Nanomed. 2012, 7, 4099–4107. [Google Scholar]
- Padole, A.; Bodhankar, M. Self Double Emulsifying Drug Delivery System (Sdedds): A Review. J. Drug Deliv. Ther. 2012, 2, 124–127. [Google Scholar] [CrossRef]
- Qi, X.; Wang, L.; Zhu, J.; Hu, Z.; Zhang, J. Self-double-emulsifying drug delivery system (SDEDDS): A new way for oral delivery of drugs with high solubility and low permeability. Int. J. Pharm. 2011, 409, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, M.; Murray, B.S.; Afeisume, E.I.; Khew, S.H. Encapsulation of flavonoid in multiple emulsion using spinning disc reactor technology. Food Hydrocoll. 2014, 34, 62–67. [Google Scholar] [CrossRef]
- Garti, N.; Bisperink, C. Double emulsions: Progress and applications. Curr. Opin. Colloid. Interface Sci. 1998, 3, 657–667. [Google Scholar] [CrossRef]
- Sapei, L.; Naqvi, M.A.; Rousseau, D. Stability and release properties of double emulsions for food applications. Food Hydrocoll. 2012, 27, 316–323. [Google Scholar] [CrossRef]
- Hashim, A.A. Smart Nanoparticles Technology; InTech: Rijeka, Croatia, 2012; pp. 195–220. [Google Scholar]
- Li, Y.; Song, J.; Tian, N.; Cai, J.; Huang, M.; Xing, Q.; Wang, Y.; Wu, C.; Hu, H. Improving oral bioavailability of metformin hydrochloride using water-in-oil microemulsions and analysis of phase behavior after dilution. Int. J. Pharm. 2014, 473, 316–325. [Google Scholar] [CrossRef]
- Kumar, S.H.; Singh, V. Nanoemulsification-a novel targeted drug delivery tool. J. Drug Deliv. Ther. 2012, 2, 40–45. [Google Scholar] [CrossRef]
- Stauff, J. Solvent Properties of Amphiphilic Compounds, von P. A. Winsor. Butterworths Scientific Publ. Ltd.: London. 1954. 1. Aufl. IX, 270 S., gebd. 40 s. Angew. Chem. 1956, 68, 504. [Google Scholar] [CrossRef]
- Healy, R.N.; Reed, R.L.; Stenmark, D.G. Multiphase Microemulsion Systems. Soc. Pet. Eng. J. 1976, 16, 147–160. [Google Scholar] [CrossRef]
- Vasconcelos, T.; Marques, S.; Sarmento, B. Measuring the emulsification dynamics and stability of self-emulsifying drug delivery systems. Eur. J. Pharm. Biopharm. 2018, 123, 1–8. [Google Scholar] [CrossRef]
- Williams, H.D.; Sassene, P.; Kleberg, K.; Bakala-N’Goma, J.C.; Calderone, M.; Jannin, V.; Igonin, A.; Partheil, A.; Marchaud, D.; Jule, E.; et al. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 1: Method parameterization and comparison of in vitro digestion profiles across a range of representative formulations. J. Pharm. Sci. 2012, 101, 3360–3380. [Google Scholar] [CrossRef]
- Netanel Liberman, G.; Ochbaum, G.; Malis Arad, S.; Bitton, R. The sulfated polysaccharide from a marine red microalga as a platform for the incorporation of zinc ions. Carbohydr. Polym. 2016, 152, 658–664. [Google Scholar] [CrossRef] [PubMed]
- Tamhane, V.A.; Dhaware, D.G.; Khandelwal, N.; Giri, A.P.; Panchagnula, V. Enhanced permeation, leaf retention, and plant protease inhibitor activity with bicontinuous microemulsions. J. Colloid Interface Sci. 2012, 383, 177–183. [Google Scholar] [CrossRef]
- Cao, Q.; Wu, H.; Zhu, L.; Wu, D.; Zhu, Y.; Zhu, Z.; Cui, J. Preparation and evaluation of zanamivir-loaded solid lipid nanoparticles. J. Control. Release 2011, 152 (Suppl. S1), e2–e4. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.L.; Cao, Y.; Zhu, X.Y.; Cui, J.H.; Cao, Q.R. Optimization of process variables of zanamivir-loaded solid lipid nanoparticles and the prediction of their cellular transport in Caco-2 cell model. Int. J. Pharm. 2015, 478, 60–69. [Google Scholar] [CrossRef]
- Miller, J.M.; Beig, A.; Carr, R.A.; Spence, J.K.; Dahan, A. A win-win solution in oral delivery of lipophilic drugs: Supersaturation via amorphous solid dispersions increases apparent solubility without sacrifice of intestinal membrane permeability. Mol. Pharm. 2012, 9, 2009–2016. [Google Scholar] [CrossRef]
- Gupta, S.V.; Gupta, D.; Sun, J.; Dahan, A.; Tsume, Y.; Hilfinger, J.; Lee, K.D.; Amidon, G.L. Enhancing the intestinal membrane permeability of zanamivir: A carrier mediated prodrug approach. Mol. Pharm. 2011, 8, 2358–2367. [Google Scholar] [CrossRef] [PubMed]
- Hoppel, M.; Reznicek, G.; Kählig, H.; Kotisch, H.; Resch, G.P.; Valenta, C. Topical delivery of acetyl hexapeptide-8 from different emulsions: Influence of emulsion composition and internal structure. Eur. J. Pharm. Sci. 2015, 68, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Shimanouchi, T.; Hayashi, T.; Toramoto, K.; Fukuma, S.; Hayashi, K.; Yasuhara, K.; Kimura, Y. Microfluidic and hydrothermal preparation of vesicles using sorbitan monolaurate/polyoxyethylene (20) sorbitan monolaurate (Span 20/Tween 20). Colloids Surf. B Biointerfaces 2021, 205, 111836. [Google Scholar] [CrossRef]
- Dave, V.S.; Gupta, D.; Yu, M.; Nguyen, P.; Varghese Gupta, S. Current and evolving approaches for improving the oral permeability of BCS Class III or analogous molecules. Drug Dev. Ind. Pharm. 2017, 43, 177–189. [Google Scholar] [CrossRef]
- Spinks, C.B.; Zidan, A.S.; Khan, M.A.; Habib, M.J.; Faustino, P.J. Pharmaceutical characterization of novel tenofovir liposomal formulations for enhanced oral drug delivery: In vitro pharmaceutics and Caco-2 permeability investigations. Clin. Pharmacol. Adv. Appl. 2017, 9, 29–38. [Google Scholar] [CrossRef]
- Gupta, S.; Chavhan, S.; Sawant, K.K. Self-nanoemulsifying drug delivery system for adefovir dipivoxil: Design, characterization, in vitro and ex vivo evaluation. Colloids Surf. A Physicochem. Eng. Asp. 2011, 392, 145–155. [Google Scholar] [CrossRef]
- Koneva, A.; Safonova, E.; Kondrakhina, P.; Vovk, M.; Lezov, A.; Chernyshev, Y.S.; Smirnova, N. Effect of water content on structural and phase behavior of water-in-oil (n-decane) microemulsion system stabilized by mixed nonionic surfactants SPAN 80/TWEEN 80. Colloids Surf. A Physicochem. Eng. Asp. 2017, 518, 273–282. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://apps.who.int/iris/handle/10665/62169 (accessed on 15 September 2023).
- Komatsu, H.; Kitajima, A.; Okada, S. Pharmaceutical characterization of commercially available intravenous fat emulsions: Estimation of average particle size, size distribution and surface potential using photon correlation spectroscopy. Chem. Pharm. Bull. 1995, 43, 1412–1415. [Google Scholar] [CrossRef] [PubMed]
- Baloch, J.; Sohail, M.F.; Sarwar, H.S.; Kiani, M.H.; Khan, G.M.; Jahan, S.; Rafay, M.; Chaudhry, M.T.; Yasinzai, M.; Shahnaz, G. Self-nanoemulsifying drug delivery system (SNEDDS) for improved oral bioavailability of chlorpromazine: In vitro and in vivo evaluation. Medicina 2019, 55, 210. [Google Scholar] [CrossRef]
- Hu, C.; Zhao, G.; Xia, Q.; Sun, R. Development and characterization of a self-double-emulsifying drug delivery system containing both epigallocatechin-3-gallate and α-lipoic acid. J. Mater. Sci. 2015, 50, 6567–6577. [Google Scholar] [CrossRef]
- Boonyapiwat, B.; Sarisuta, N.; Kunastitchai, S. Characterization and in vitro evaluation of intestinal absorption of liposomes encapsulating zanamivir. Curr. Drug Deliv. 2011, 8, 392–397. [Google Scholar] [CrossRef]
- Beig, A.; Fine-Shamir, N.; Lindley, D.; Miller, J.M.; Dahan, A. Advantageous solubility-permeability interplay when using amorphous solid dispersion (ASD) formulation for the BCS class IV P-gp substrate rifaximin: Simultaneous increase of both the solubility and the permeability. AAPS J. 2017, 19, 806–813. [Google Scholar] [CrossRef]
- El-Kattan, A.; Varma, M. Oral absorption, intestinal metabolism and human oral bioavailability. Top. Drug Metab. 2012, 10, 31087. [Google Scholar]
- Yu, H.; Wang, Q.; Sun, Y.; Shen, M.; Li, H.; Duan, Y. A new PAMPA model proposed on the basis of a synthetic phospholipid membrane. PLoS ONE 2015, 10, e0116502. [Google Scholar] [CrossRef]
- Zur, M.; Cohen, N.; Agbaria, R.; Dahan, A. The biopharmaceutics of successful controlled release drug product: Segmental-dependent permeability of glipizide vs. metoprolol throughout the intestinal tract. Int. J. Pharm. 2015, 489, 304–310. [Google Scholar] [CrossRef]
- Guo, S.; Huang, L. Nanoparticles containing insoluble drug for cancer therapy. Biotechnol. Adv. 2014, 32, 778–788. [Google Scholar] [CrossRef] [PubMed]
- Hua, S. Lipid-based nano-delivery systems for skin delivery of drugs and bioactives. Front. Pharmacol. 2015, 6, 219. [Google Scholar] [CrossRef] [PubMed]










Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ifrah, S.; Dahan, A.; Debotton, N. Towards Effective Antiviral Oral Therapy: Development of a Novel Self-Double Emulsifying Drug Delivery System for Improved Zanamivir Intestinal Permeability. Pharmaceutics 2023, 15, 2518. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics15102518
Ifrah S, Dahan A, Debotton N. Towards Effective Antiviral Oral Therapy: Development of a Novel Self-Double Emulsifying Drug Delivery System for Improved Zanamivir Intestinal Permeability. Pharmaceutics. 2023; 15(10):2518. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics15102518
Chicago/Turabian StyleIfrah, Sapir, Arik Dahan, and Nir Debotton. 2023. "Towards Effective Antiviral Oral Therapy: Development of a Novel Self-Double Emulsifying Drug Delivery System for Improved Zanamivir Intestinal Permeability" Pharmaceutics 15, no. 10: 2518. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics15102518