Gender Differences in Factors Affecting Life Satisfaction of the Elderly with Multimorbidity in Korea
Abstract
:1. Introduction
2. Methods
2.1. Aim and Design
2.2. Description of the Data Source, Procedure for Data Collection, and Sampling
2.3. Study Variables and Measurements
2.3.1. Sociodemographic Factors
2.3.2. Health Behavioral Factors
2.3.3. Health Status Factors
2.3.4. Life Satisfaction
2.4. Statistical Analyses
3. Results
3.1. Differences between Older Males and Females with Multimorbidity
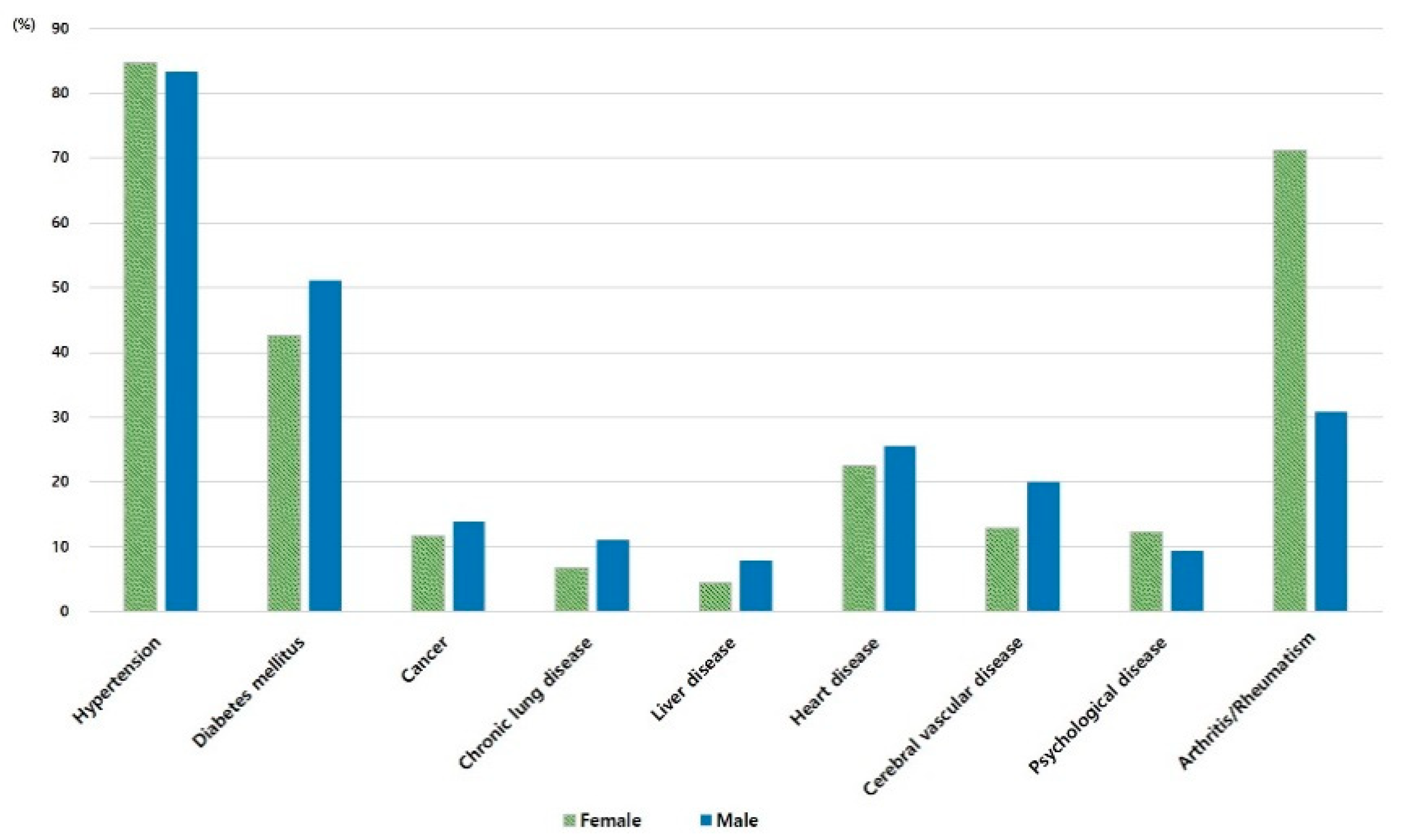
3.2. Differences in Multimorbidity by Gender
3.3. Predictors of Life Satisfaction in Older Females and Males with Multimorbidity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abad-Díez, J.M.; Calderón-Larrañaga, A.; Poncel-Falcó, A.; Poblador-Plou, B.; Calderón-Meza, J.; Sicras-Mainar, A.; Clerencia-Sierra, M.; Prados-Torres, A. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014, 14, 75. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health and Welfare & Korea Institute for Health and Social Affairs. 2017 Report on Elderly Survey. Sejong. Available online: http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=032901&page=1&CONT_SEQ=344953 (accessed on 28 November 2020).
- Quah, J.H.M.; Wang, P.; Ng, R.R.G.; Luo, N.; Tan, N.C. Health-related quality of life of older Asian patients with multimorbidity in primary care in a developed nation. Geriatr. Gerontol. Int. 2017, 17, 1429–1437. [Google Scholar] [CrossRef]
- Ward, B.W.; Black, L.I. State and regional prevalence of diagnosed multiple chronic conditions among adults aged ≥18 years—United States, 2014. MMWR Morb. Mortal Wkly Rep. 2016, 65, 735–738. [Google Scholar] [CrossRef]
- Statistics Korea. 2017. Population and Housing Census. Available online: https://www.korea.kr/news/pressReleaseView.do?newsId=156290510 (accessed on 18 January 2021).
- Statistics Korea. 2019 Population Status and Prospects of the World and Korea. Available online: http://kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&aSeq=377226 (accessed on 18 January 2021).
- Park, B.; Ock, M.; Lee, H.A.; Lee, S.; Han, H.; Jo, M.-W.; Park, H. Multimorbidity and health-related quality of life in Koreans aged 50 or older using KNHANES 2013-2014. Health Qual. Life Outcomes 2018, 16, 186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agur, K.; McLean, G.; Hunt, K.; Guthie, B.; Mercer, S.W. How does sex influence multimorbidity? Secondary analysis of a large nationally representative dataset. Int. J. Environ. Res. Public Health 2016, 13, 391. [Google Scholar] [CrossRef] [Green Version]
- King, D.E.; Xiang, J.; Pillkerton, C.S. Multimorbidity trends in United States adults, 1988-2014. J. Am. Board Fam. Med. 2018, 31, 503–513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, S.-S.; Cao, G.-Y.; Han, L.; Chen, Z.-S.; Huang, Z.-T.; Gong, P.; Hu, Y.; Xu, B. Prevalence and patterns of multimorbidity in a nationally representative sample of older Chinese: Results from the China Health and Retirement Longitudinal Study. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 1974–1980. [Google Scholar] [CrossRef]
- Violan, C.; Foguet-Boreu, Q.; Flores-Mateo, G.; Salisbury, C.; Blom, J.; Freitag, M.; Glynn, L.; Muth, C.; Valderas, J.M. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS ONE 2014, 9, e102149. [Google Scholar] [CrossRef] [PubMed]
- Rieckert, A.; Trampisch, U.S.; Klaaßen-Mielke, R.; Drewelow, E.; Esmail, A.; Johansson, T.; Keller, S.; Kunnamo, I.; Löffler, C.; Mäkinen, J.; et al. Polypharmacy in older patients with chronic diseases: A cross-sectional analysis of factors associated with excessive polypharmacy. BMC Fam. Pract. 2018, 19, 113. [Google Scholar] [CrossRef] [Green Version]
- Gu, J.; Chao, J.; Chen, W.; Xu, H.; Zhang, R.; He, T.; Deng, L. Multimorbidity and health-related quality of life among the community-dwelling elderly: A longitudinal study. Arch. Gerontol Geriatr. 2018, 74, 133–140. [Google Scholar] [CrossRef]
- Nunes, B.P.; Flores, T.R.; Mielke, G.I.; Thumé, E.; Facchini, L.A. Multimorbidity and mortality in older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2016, 67, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Chan, S.H.W.; Xu, Y.; Yeung, K.C. Determinants of life satisfaction and self-perception of ageing among elderly people in China: An exploratory study in comparison between physical and social functioning. Arch. Gerontol Geriatr. 2019, 84, 103910. [Google Scholar] [CrossRef] [PubMed]
- Organisation for Economic Co-operation and Development. “Life satisfaction”. In Society at a Glance 2019: OECD Social Indicators; OECD Publishing: Paris, French, 2019. [Google Scholar] [CrossRef]
- Bai, X.; Yang, S.; Knapp, M. Sources and directions of social support and life satisfaction among solitary Chinese older adults in Hong Kong: The mediating role of sense of loneliness. Clin. Interv. Aging 2018, 13, 63–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kimm, H.; Sull, J.W.; Gombojav, B.; Yi, S.-W.; Ohrr, H. Life satisfaction and mortality in elderly people: The Kangwha Cohort Study. BMC Public Health 2012, 12, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, D.-H. Effect of religion on the satisfaction of the elderly’s life. J. KoCon. A. 2020, 20, 212–221. [Google Scholar] [CrossRef]
- Kolosnitsyna, M.; Khorkina, N.; Dorzhiev, H. Determinants of life satisfaction in older Russians. Ageing Intl. 2017, 42, 354–373. [Google Scholar] [CrossRef]
- Tran, N.L.T.; Wassmer, R.W.; Lascher, E.L. The Health Insurance and Life Satisfaction Connection. J Happiness Stud. 2017, 18, 409–426. [Google Scholar] [CrossRef]
- Adams, T.R.; Rabin, L.A.; Da Silva, V.G.; Katz, M.J.; Fogel, J.; Lipton, R.B. Social support buffers the impact of depressive symptoms on life satisfaction in old age. Clin Gerontol. 2016, 39, 139–157. [Google Scholar] [CrossRef] [Green Version]
- Banjare, P.; Dwivedi, R.; Pradhan, J. Factors associated with the life satisfaction amongst the rural elderly in Odisha, India. Health Qual. Life Outcomes 2015, 13, 201. [Google Scholar] [CrossRef] [Green Version]
- Parra-Rizo, M.A.; Sanchis-Soler, G. Satisfaction with life, subjective well-being and functional skills in active older adults based on their level of physical activity practice. Int. J. Environ. Res. Public Health 2020, 17, 1299. [Google Scholar] [CrossRef] [Green Version]
- Tkatch, R.; Musich, S.; MacLeod, S.; Kraemer, S.; Hawkins, K.; Wicker, E.R.; Armstrong, D.G. A qualitative study to examine older adults’ perceptions of health: Keys to aging successfully. Geriatr. Nurs. 2017, 38, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Manandhar, M.; Hawkes, S.; Buse, K.; Nosrati, E.; Magar, V. Gender, health and the 2030 agenda for sustainable development. Bull World Health Organ. 2018, 96, 644–653. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.-K.; Kim, J.-E. Gender difference of community-residing elderly’s satisfaction with life and influential factors. J. KoCon. A. 2018, 18, 467–480. [Google Scholar] [CrossRef]
- Resnick, B.; Boltz, M.; Galik, E.; Holmes, S.; Fix, S.; Zhu, S. Gender differences in function, physical activity, falls medication use, and life satisfaction among residents in assisted living settings. Res. Gerontol. Nurs. 2020, 13, 31–39. [Google Scholar] [CrossRef]
- Meggiolaro, S.; Ongaro, F. Life satisfaction among older people in Italy in a gender approach. Ageing Soc. 2015, 35, 1481–1504. [Google Scholar] [CrossRef]
- Lee, S.-H.; Lee, J.; Choi, I. Life satisfaction in later life: The interplay of marital condition and income among elderly Koreans. Sustainability 2020, 12, 3483. [Google Scholar] [CrossRef] [Green Version]
- Joshanloo, M. Gender differences in the predictors of life satisfaction across 150 nations. Pers. Individ. Dif. 2018, 135, 312–315. [Google Scholar] [CrossRef]
- Lim, Y.M.; Lee, S.R.; Choi, E.J.; Jeong, K.; Chung, H.W. Urinary incontinence is strongly associated with depression in middle-aged and older Korean women: Data from the Korean longitudinal study of ageing. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 220, 69–73. [Google Scholar] [CrossRef]
- Yoo, J.I.; Choi, H.; Ha, Y.C. Mean hand grip strength and cut-off value for sarcopenia in Korean adults using KNHANES VI. J. Korean Med. Sci. 2017, 32, 868–872. [Google Scholar] [CrossRef]
- Korea Employment Information Service. 2018 User’s Guide of Korean Longitudinal Study of Ageing. Available online: https://survey.keis.or.kr/klosa/klosaguide/List.jsp (accessed on 15 October 2020).
- World Health Organization. Chronic Diseases and Health Promotion. Available online: https://www.who.int/chp/topics/rheumatic/en/ (accessed on 3 December 2020).
- Dieppe, P.A.; Lohmander, L.S. Pathogenesis and management of pain in osteoarthritis. Lancet 2005, 365, 965–973. [Google Scholar] [CrossRef]
- Hurley, B.F.; Hanson, E.D.; Sheaff, A.K. Strength training as a countermeasure to aging muscle and chronic disease. Sports Med. 2011, 41, 289–306. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.J.; Oh, H.; Lee, S.; Lee, K.; Kim, K. Effects of resistance exercise using the elastic band on the pain and function of patients with degenerative knee arthritis. J. Phys. Ther. Sci. 2020, 32, 52–54. [Google Scholar] [CrossRef] [PubMed]
- Statistics Korea. Life Expectancy and Life Expectancy excluding Disease Period. Available online: https://www.index.go.kr/potal/info/idxKoreaView.do?idx_cd=2758 (accessed on 19 January 2021).
- Lee, K.H.; Xu, H.; Wu, B. Gender differences in quality of life among community-dwelling older adults in low-and middle-income countries: Results from the Study on global AGEing and adult health (SAGE). BMC Public Health 2020, 20, 114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, H.G. The status of South Korea’s economy: A middle-income or a high-income country? East Asia Found. 2019, 126, 1–6. [Google Scholar]
- Organisation for Economic Co-operation and Development. “Old-age income poverty”. In Pensions at a Glance 2019: OECD and G20iIndicators; OECD Publishing: Paris, French, 2019. [Google Scholar] [CrossRef]
- Kang, E.N. Current state and challenges of senior employment programs. Health Welfare Forum 2017, 251, 28–39. [Google Scholar]
- Marques, A.; Peralta, M.; Gouveia, É.R.; Chávez, F.G.; Aleiro, M.G. Physical activity buffers the negative relationship between multimorbidity, self-rated health and life satisfaction. J. Public Health 2018, 40, e328–e335. [Google Scholar] [CrossRef]
- Boehmer, K.R.; Abu Dabrh, A.M.; Gionfriddo, M.R.; Erwin, P.; Montori, V.M. Does the chronic care model meet the emerging needs of people living with multimorbidity? A systematic review and thematic synthesis. PLoS ONE 2018, 13, e0190852. [Google Scholar] [CrossRef] [Green Version]
- Lei, X.; Hu, Y.; McArdle, J.J.; Smith, J.P.; Zhao, Y. Gender differences in cognition among older adults in China. J. Hum. Resour. 2012, 47, 951–971. [Google Scholar] [CrossRef] [Green Version]
- Ahrenfeldt, L.J.; Scheel-Hincke, L.L.; Kjærgaard, S.; Möller, S.; Christensen, K.; Lindahl-Jacobsen, R. Gender differences in cognitive function and grip strength: A cross-national comparison of four European regions. Eur. J. Public Health 2019, 29, 667–674. [Google Scholar] [CrossRef]
- Peitsch, L.; Tyas, S.L.; Menec, V.H.; St John, P.D. General life satisfaction predicts dementia in community living older adults: A prospective cohort study. Int. Psychogeriatr. 2016, 28, 1101–1109. [Google Scholar] [CrossRef]
- Onishi, C.; Yuasa, K.; Sei, M.; Ewis, A.A.; Nakano, T.; Munakata, H.; Nakahori, Y. Determinants of life satisfaction among Japanese elderly women attending health care and welfare service facilities. J. Med. Investig. 2010, 57, 69–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puvill, T.; Lindenberg, J.; de Craen, A.J.; Slaets, J.P.; Westendorp, R.G. Impact of physical and mental health on life satisfaction in old age: A population based observational study. BMC Geriatr. 2016, 16, 194. [Google Scholar] [CrossRef] [Green Version]
- Bohannon, R.W. Muscle strength: Clinical and prognostic value of hand-grip dynamometry. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 465–470. [Google Scholar] [CrossRef] [PubMed]
- McDowell, C.P.; Gordon, B.R.; Herring, M.P. Sex-related differences in the association between grip strength and depression: Results from the Irish Longitudinal Study on Ageing. Exp. Gerontol. 2018, 104, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Sternäng, O.; Reynolds, C.A.; Finkel, D.; Ernsth-Bravell, M.; Pedersen, N.L.; Dahl Aslan, A.K. Grip Strength and Cognitive Abilities: Associations in Old Age. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016, 71, 841–848. [Google Scholar] [CrossRef] [Green Version]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Institute for Futures Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Bronfenbrenner, U. Ecological systems theory. In Six Theories of Child Development: Revised Formulations and Current Issues; Vasta, R., Ed.; Jessica Kingsley Publishers: London, UK, 1992; pp. 187–249. [Google Scholar]
| Variables | Female (n = 1384) | Male (n = 756) | p | |
|---|---|---|---|---|
| Weighted %, Mean (SD) | ||||
| Age (year) | 76.22(7.22) | 74.17 (6.51) | <0.001 | |
| Education | Elementary school or less | 75.6 | 34.7 | <0.001 |
| Middle school or higher | 24.4 | 65.3 | ||
| Marital status | Married | 46.7 | 86.4 | <0.001 |
| Not married (widowed, etc.) | 53.3 | 13.6 | ||
| Religion | Yes | 51.0 | 36.4 | <0.001 |
| No | 49.0 | 63.6 | ||
| Current employment | Yes | 13.0 | 30.6 | <0.001 |
| No | 87.0 | 69.4 | ||
| Meeting with close friends | More than once a week | 67.7 | 54.8 | <0.001 |
| Less than once a week | 32.3 | 45.2 | ||
| Private health insurance | Yes | 14.2 | 19.9 | <0.001 |
| No | 85.8 | 80.1 | ||
| Cigarette smoking | Never smoked | 94.0 | 31.1 | <0.001 |
| smoker | 6.0 | 68.9 | ||
| Alcohol drinking | Never consumed | 74.7 | 18.8 | <0.001 |
| Has consumed | 25.3 | 81.2 | ||
| Regular exercise | Yes | 25.9 | 40.6 | <0.001 |
| No | 74.1 | 59.4 | ||
| Number of chronic diseases | 2.68 (0.87) | 2.52 (0.75) | <0.001 | |
| Cognition | 22.31 (6.20) | 24.98 (5.19) | <0.001 | |
| Depression | 3.84 (2.82) | 3.25 (2.93) | <0.001 | |
| Grip strength | 19.29 (5.26) | 28.24 (7.55) | <0.001 | |
| Satisfaction of life | Health | 47.99 (20.49) | 51.02 (20.17) | <0.001 |
| Overall quality of life | 56.22 (17.33) | 59.18 (17.21) | <0.001 | |
| Female | n (%) | Male | n (%) | |
|---|---|---|---|---|
| 1 | HTN, AR | 333 (24.0) | HTN, DM | 138 (18.2) |
| 2 | HTN, DM, AR | 168 (12.1) | HTN, AR | 68 (8.9) |
| 3 | HTN, DM | 118 (8.5) | HTN, HD | 49 (6.4) |
| 4 | HTN, HD, AR | 59 (4.2) | HTN, DM, HD | 40 (5.2) |
| 5 | DM, AR | 47 (3.4) | HTN, DM, AR | 35 (4.6) |
| 6 | HTN, HD | 45 (3.2) | HTN, CVD | 34 (4.5) |
| 7 | HTN, DM, HD, AR | 36 (2.6) | HTN, Cancer | 26 (3.4) |
| 8 | HTN, DM, HD | 27 (1.9) | HTN, DM, CVD | 19 (2.5) |
| 9 | HTN, CVD | 25 (1.8) | HTN, CLD | 16 (2.1) |
| 10 | HTN, CVD, AR | 24 (1.7) | HTN, DM, Cancer | 13 (1.7) |
| Variables | Female (n = 1384) | Male (n = 756) | ||||||
|---|---|---|---|---|---|---|---|---|
| B | S.E. | β | p | B | S.E. | β | p | |
| Depression | −2.286 | 0.182 | −0.316 | <0.001 | −1.967 | 0.236 | −0.286 | <0.001 |
| Cognition | 0.487 | 0.085 | 0.148 | <0.001 | 0.549 | 0.137 | 0.141 | <0.001 |
| Exercise (ref. No) | 5.790 | 1.158 | 0.124 | <0.001 | 5.530 | 1.325 | 0.135 | <0.001 |
| Number of chronic diseases | −2.868 | 0.557 | −0.122 | <0.001 | −3.565 | 0.839 | −0.133 | <0.001 |
| Current employment (ref. No) | 3.859 | 1.465 | 0.063 | 0.009 | 3.373 | 1.463 | 0.077 | 0.021 |
| Religion (ref. No) | 2.526 | 0.973 | 0.062 | 0.010 | ||||
| Education (ref. Elementary school or less) | 2.309 | 1.155 | 0.048 | 0.046 | ||||
| Grip strength | 0.309 | 0.094 | 0.116 | 0.001 | ||||
| Smoking (ref. No) | −2.998 | 1.346 | −0.069 | 0.026 | ||||
| Adjusted R2 = 0.249, F = 66.650 (p < 0.001) | Adjusted R2 = 0.290, F = 45.026 (p < 0.001) | |||||||
| Variables | Female (n = 1384) | Male (n = 756) | ||||||
|---|---|---|---|---|---|---|---|---|
| B | S.E. | β | p | B | S.E. | β | p | |
| Depression | −2.587 | 0.151 | −0.422 | <0.001 | −2.349 | 0.189 | −0.400 | <0.001 |
| Exercise (ref. No) | 4.052 | 0.960 | 0.102 | <0.001 | 5.811 | 1.092 | 0.166 | <0.001 |
| Number of chronic diseases | −1.878 | 0.468 | −0.094 | <0.001 | −2.253 | 0.709 | −0.099 | 0.002 |
| Religion (ref. No) | 2.108 | 0.814 | 0.061 | 0.010 | ||||
| Cognition | 0.165 | 0.069 | 0.059 | 0.017 | ||||
| Smoking (ref. No) | −3.888 | 1.689 | −0.053 | 0.021 | ||||
| Marriage (ref. No) | 6.678 | 1.563 | 0.133 | <0.001 | ||||
| Private health insurance (ref. No) | 4.594 | 1.333 | 0.107 | 0.001 | ||||
| Adjusted R2 = 0.261, F = 82.618 (p < 0.001) | Adjusted R2 = 0.294, F = 63.784 (p < 0.001) | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Lee, M.; Dan, H. Gender Differences in Factors Affecting Life Satisfaction of the Elderly with Multimorbidity in Korea. Nurs. Rep. 2021, 11, 54-63. https://0-doi-org.brum.beds.ac.uk/10.3390/nursrep11010006
Kim J, Lee M, Dan H. Gender Differences in Factors Affecting Life Satisfaction of the Elderly with Multimorbidity in Korea. Nursing Reports. 2021; 11(1):54-63. https://0-doi-org.brum.beds.ac.uk/10.3390/nursrep11010006
Chicago/Turabian StyleKim, Jeonghyun, Minkyung Lee, and Hyunju Dan. 2021. "Gender Differences in Factors Affecting Life Satisfaction of the Elderly with Multimorbidity in Korea" Nursing Reports 11, no. 1: 54-63. https://0-doi-org.brum.beds.ac.uk/10.3390/nursrep11010006






