Economic Burden of Not Complying with Canadian Food Recommendations in 2018
Abstract
:1. Introduction
2. Materials and Methods
2.1. Food Selection
2.2. Food Consumption Data Analysis
2.3. Population Attributable Fraction Calculations
2.4. Estimation of Direct Health Care and Indirect Costs
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Statistics Canada. Leading Causes of Death, Total Population, by Age Group. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039401 (accessed on 28 June 2019).
- Public Health Agency of Canada. Economic Burden of Illness in Canada, 2005–2008. Government of Canada: Ottawa, ON, Canada, 2014; pp. 1–111. Available online: http://www.phac-aspc.gc.ca/publicat/ebic-femc98/pdf/ebic1998.pdf (accessed on 10 May 2018).
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Hassen Abate, K.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392. Available online: www.thelancet.com (accessed on 17 May 2019).
- IHME. Country Profile: Canada. Top 10 Risks Contributing to DALYS in 2016 and Percent Change, 2005–2016, All Ages. Available online: http://www.healthdata.org/canada (accessed on 5 July 2019).
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. Available online: https://0-linkinghub-elsevier-com.brum.beds.ac.uk/retrieve/pii/S0140673619300418 (accessed on 20 April 2019). [CrossRef]
- Ekwaru, J.P.; Ohinmaa, A.; Loehr, S.; Setayeshgar, S.; Thanh, N.X.; Veugelers, P.J. The economic burden of inadequate consumption of vegetables and fruit in Canada. Public Health Nutr. 2016, 20, 1–9. Available online: https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pmc/articles/PMC5426323/ (accessed on 15 May 2018). [CrossRef] [PubMed]
- Krueger, H.; Koot, J.; Andres, E. The economic benefits of fruit and vegetable consumption in Canada. Can. J. Public Health 2017, 108, e152–e161. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/28621651 (accessed on 5 July 2019). [CrossRef] [Green Version]
- Doidge, J.C.; Segal, L.; Gospodarevskaya, E. Attributable Risk Analysis Reveals Potential Healthcare Savings from Increased Consumption of Dairy Products. J. Nutr. 2012, 142, 1772–1780. Available online: https://0-academic-oup-com.brum.beds.ac.uk/jn/article/142/9/1772/4630973 (accessed on 5 July 2019). [CrossRef] [Green Version]
- McCarron, D.; Heaney, R.P. Estimated healthcare savings associated with adequate dairy food intake. Am. J. Hypertens. 2004, 17, 88–97. Available online: https://0-academic-oup-com.brum.beds.ac.uk/ajh/article-lookup/doi/10.1016/j.amjhyper.2003.08.008 (accessed on 5 July 2019). [CrossRef] [Green Version]
- Barnard, N.D.; Nicholson, A.; Howard, J.L. The Medical Costs Attributable to Meat Consumption. Prev. Med. 1995, 24, 646–655. Available online: https://0-www-sciencedirect-com.brum.beds.ac.uk/science/article/pii/S0091743585711000?via%3Dihub (accessed on 5 July 2019). [CrossRef]
- Abdullah, M.M.H.; Gyles, C.L.; Marinangeli, C.P.F.; Carlberg, J.G.; Jones, P.J.H. Cost-of-illness analysis reveals potential healthcare savings with reductions in type 2 diabetes and cardiovascular disease following recommended intakes of dietary fiber in Canada. Front. Pharmacol. 2015, 6, 167. Available online: http://journal.frontiersin.org/Article/10.3389/fphar.2015.00167/abstract (accessed on 5 July 2019). [CrossRef] [Green Version]
- Meier, T.; Deumelandt, P.; Christen, O.; Stangl, G.I.; Riedel, K.; Langer, M. Global Burden of Sugar-Related Dental Diseases in 168 Countries and Corresponding Health Care Costs. J. Dent. Res. 2017, 96, 845–854. Available online: http://0-journals-sagepub-com.brum.beds.ac.uk/doi/10.1177/0022034517708315 (accessed on 5 July 2019). [CrossRef]
- Jones, A.C.; Veerman, J.L.; Hammond, D. The Health and Economic Impact of a Tax on Sugary Drinks in Canada; University Waterloo: Waterloo, ON, Canada, 2017; pp. 1–77. Available online: https://www.diabetes.ca/getattachment/Newsroom/Latest-News/Will-a-sugary-drinks-levy-benefit-Canadians/The-Health-and-Economic-Impact-of-a-Sugary-Drinks-Tax.pdf.aspx (accessed on 15 May 2018).
- Candari, C.J.; World Health Organization; Cylus, J.; Nolte, E.; European Observatory on Health Systems and Policies. Assessing the Economic Costs of Unhealthy Diets and Low Physical Activity an Evidence Review and Proposed Framework; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Scarborough, P.; Bhatnagar, P.; Wickramasinghe, K.K.; Allender, S.; Foster, C.; Rayner, M. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: An update to 2006-07 NHS costs. J. Public Health (Bangk.) 2011, 33, 527–535. Available online: https://0-academic-oup-com.brum.beds.ac.uk/jpubhealth/article-lookup/doi/10.1093/pubmed/fdr033 (accessed on 5 July 2019). [CrossRef]
- Frazao, E. High Costs of Poor Eating Patterns in the United States. Agric. Inf. Bull. 1999, 494. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.467.3556&rep=rep1&type=pdf (accessed on 8 July 2019).
- Health Canada. Food and Nutrition Surveillance in Canada: An Environmental Scan. 2000. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/food-nutrition-surveillance-canada-environmental-scan-health-canada-2000.html (accessed on 16 October 2019).
- Nshimyumukiza, L.; Lieffers, J.R.L.; Ekwaru, J.P.; Ohinmaa, A.; Veugelers, P.J. Temporal changes in diet quality and the associated economic burden in Canada. PLoS ONE 2018, 13, e0206877. Available online: https://0-doi-org.brum.beds.ac.uk/10.1371/journal.pone.0206877 (accessed on 22 November 2018). [CrossRef] [PubMed]
- Renzella, J.; Townsend, N.; Jewell, J.; Breda, J.; Roberts, N.; Rayner, M.; Wickramasinghe, K. What National and Subnational Interventions and Policies Based on Mediterranean and Nordic Diets are Recommended or Implemented in the WHO European Region, and Is There Evidence of Effectiveness in Reducing Noncommunicable Diseases? Health Evidence Network Synthesis Report; WHO Regional Office for Europe: Copenhagen, Danmark, 2018. [Google Scholar]
- Garriguet, D. Canadians’ eating habits. Health Rep. 2007, 18, 17–32. [Google Scholar] [PubMed]
- Lieffers, J.R.L.; Ekwaru, J.P.; Ohinmaa, A.; Veugelers, P.J. The economic burden of not meeting food recommendations in Canada: The cost of doing nothing. PLoS ONE 2018, 13, e0196333. Available online: https://0-doi-org.brum.beds.ac.uk/10.1371/journal.pone.0196333 (accessed on 28 August 2018). [CrossRef]
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. Available online: https://0-www-sciencedirect-com.brum.beds.ac.uk/science/article/pii/S0140673616316798?via%3Dihub (accessed on 5 July 2019). [CrossRef]
- Health Canada. Reference Guide to Understanding and Using the Data 2015 Canadian Community Health Survey-Nutrition. 2017. Available online: https://www.canada.ca/content/dam/hc-sc/documents/services/food-nutrition/food-nutrition-surveillance/ReferenceGuide2015CCHS-Nutr_Eng_Final_06192017.pdf (accessed on 9 July 2019).
- Health Canada. Eating Well with Canada’s Food Guide. 2007. Available online: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/hpfb-dgpsa/pdf/food-guide-aliment/print_eatwell_bienmang-eng.pdf (accessed on 6 June 2019).
- Elvidge Munene, L.A.; Dumais, L.; Esslinger, K.; Jones-Mclean, E.; Mansfield, E.; Verreault, M.-F.; Villeneuve, M.; Miller, D. A surveillance tool to assess diets according to Eating Well with Canada’s Food Guide. Health Rep. 2015, 26, 12–20. Available online: http://0-ovidsp-ovid-com.brum.beds.ac.uk/ovidweb.cgi?T=JS&PAGE=reference&D=emed16&NEWS=N&AN=611137297 (accessed on 15 May 2018).
- Health Canada. The Development and Use of a Surveillance Tool: The Classification of Foods in the Canadian Nutrient File according to Eating Well with Canada’s Food Guide. p. 25. Available online: http://publications.gc.ca/site/eng/9.698720/publication.html (accessed on 16 July 2019).
- Micha, R.; Kalantarian, S.; Wirojratana, P.; Byers, T.; Danaei, G.; Elmadfa, I.; Ding, E.; Giovannucci, E.; Powles, J.; Smith-Warner, S.; et al. Estimating the global and regional burden of suboptimal nutrition on chronic disease: Methods and inputs to the analysis. Eur. J. Clin. Nutr. 2012, 66, 119–129. Available online: http://0-www-nature-com.brum.beds.ac.uk/articles/ejcn2011147 (accessed on 26 September 2019). [CrossRef]
- International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Available online: https://monographs.iarc.fr/ (accessed on 16 July 2019).
- Canadian Cancer Society. Red and Processed Meat. Available online: http://www.cancer.ca/en/prevention- and-screening/live-well/nutrition-and-fitness/eating-well/red-and-processed-meat/?region=on (accessed on 2 May 2019).
- Anderson, T.J.; Grégoire, J.; Pearson, G.J.; Barry, A.R.; Couture, P.; Dawes, M.; Francis, G.A.; Genest, J.; Grover, S.; Gupta, M.; et al. 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can. J. Cardiol. 2016, 32, 1263–1282. Available online: https://0-www-sciencedirect-com.brum.beds.ac.uk/science/article/pii/S0828282×16307322?via%3Dihub (accessed on 16 July 2019). [CrossRef]
- Tooze, J.A.; Midthune, D.; Dodd, K.W.; Freedman, L.S.; Krebs-Smith, S.M.; Subar, A.F.; Guenther, P.M.; Carroll, R.J.; Kipnis, V. A New Statistical Method for Estimating the Usual Intake of Episodically Consumed Foods with Application to Their Distribution. J. Am. Diet. Assoc. 2006, 106, 1575–1587. Available online: https://0-www-sciencedirect-com.brum.beds.ac.uk/science/article/pii/S0002822306016907?via%3Dihub (accessed on 16 July 2019). [CrossRef] [Green Version]
- Kirkpatrick, S.I.; Dodd, K.W.; Parsons, R.; Ng, C.; Garriguet, D.; Tarasuk, V. Household Food Insecurity Is a Stronger Marker of Adequacy of Nutrient Intakes among Canadian Compared to American Youth and Adults. J. Nutr. 2015, 145, 1596–1603. Available online: https://0-academic-oup-com.brum.beds.ac.uk/jn/article/145/7/1596/4589978 (accessed on 16 July 2019). [CrossRef] [Green Version]
- Kirkpatrick, S.I.; Dodd, K.W.; Reedy, J.; Krebs-Smith, S.M. Income and Race/Ethnicity Are Associated with Adherence to Food-Based Dietary Guidance among US Adults and Children. J. Acad. Nutr. Diet. 2012, 112, 624–635.e6. Available online: https://0-www-sciencedirect-com.brum.beds.ac.uk/science/article/pii/S2212267211019435?via%3Dihub (accessed on 16 July 2019). [CrossRef] [PubMed] [Green Version]
- Krebs-Smith, S.M.; Guenther, P.M.; Subar, A.F.; Kirkpatrick, S.I.; Dodd, K.W. Americans Do Not Meet Federal Dietary Recommendations. J. Nutr. 2010, 140, 1832–1838. Available online: https://0-academic-oup-com.brum.beds.ac.uk/jn/article/140/10/1832/4600316 (accessed on 16 July 2019). [CrossRef] [PubMed]
- Krueger, H.; Williams, D.; Ready, E.; Trenaman, L.; Turner, D. Improved estimation of the health and economic burden of chronic disease risk factors in Manitoba. Chronic Dis. Inj. Can. 2013, 33, 236–246. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/23987220 (accessed on 10 May 2018). [PubMed]
- Whiteman, D.C.; Webb, P.M.; Green, A.C.; Neale, R.E.; Fritschi, L.; Bain, C.J.; Parkin, D.M.; Wilson, L.F.; Olsen, C.M.; Nagle, C.M.; et al. Cancers in Australia in 2010 attributable to modifiable factors: Introduction and overview. Aust. N. Z. J. Public Health 2015, 39, 403–407. Available online: http://0-doi-wiley-com.brum.beds.ac.uk/10.1111/1753-6405.12468 (accessed on 9 July 2019). [CrossRef]
- Azevedo ESilva, G.; de Moura, L.; Curado, M.P.; Gomes Fda, S.; Otero, U.; Rezende, L.F.; de Daumas, R.P.; Guimarães, R.M.; Meira, K.C.; Leite Ida, C.; et al. The Fraction of Cancer Attributable to Ways of Life, Infections, Occupation, and Environmental Agents in Brazil in 2020. PLoS ONE 2016, 11, e0148761. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/26863517 (accessed on 9 July 2019). [CrossRef]
- Canadian Institute for Health Information. National Health Expenditure Trends, 1975 to 2018. Available online: https://www.cihi.ca/en/health-spending/2018/national-health-expenditure-trends (accessed on 16 July 2019).
- Health Canada. Economic Burden of Illness in Canada, 1998. 2002. Available online: http://publications.gc.ca/collections/Collection/H21-136-1998E.pdf (accessed on 16 July 2019).
- Krueger, H.; Andres, E.N.; Koot, J.M.; Reilly, B.D. The economic burden of cancers attributable to tobacco smoking, excess weight, alcohol use, and physical inactivity in Canada. Curr. Oncol. 2016, 23, 241–249. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/27536174 (accessed on 26 September 2018). [CrossRef]
- Krueger, H.; Turner, D.; Krueger, J.; Ready, A.E. The economic benefits of risk factor reduction in Canada: Tobacco smoking, excess weight and physical inactivity. Can. J. Public Health 2014, 105, e69–e78. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/24735700 (accessed on 8 July 2019). [CrossRef]
- Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; Cohen, A.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/26364544 (accessed on 9 July 2019). [CrossRef]
- Statistics Canada. Table 2 Population by Age Group and Sex, Canada. 2014. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501 (accessed on 10 April 2019).
- Garriguet, D. Accounting for misreporting when comparing energy intake across time in Canada. Health Rep. 2018, 29, 3–12. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/29852052 (accessed on 12 April 2019).
- Fedorak, R.N.; Switzer, C.M.; Bridges, R.J. Canadian Digestive Health Foundation Public Impact Series 4: Celiac disease in Canada. Incidence, prevalence, and direct and indirect economic impact. Can. J. Gastroenterol. 2012, 26, 350–352. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/22720277 (accessed on 17 July 2019). [CrossRef]
- Topper, A. Non-Celiacs Drive Gluten-Free Market Growth. 2014. Available online: https://0-www-mintel-com.brum.beds.ac.uk/blog/food-market-news/gluten-free-consumption-trends (accessed on 18 July 2019).
- Canadian Celiac Association. Non-Celiac Gluten Sensitivity: How to Diagnose and Differentiate It from Celiac Disease. Available online: https://www.celiac.ca/gluten-related-disorders/non-celiac-gluten-sensitivity/ (accessed on 17 July 2019).
- Rubio-Tapia, A.; Ludvigsson, J.F.; Brantner, T.L.; Murray, J.A.; Everhart, J.E. The Prevalence of Celiac Disease in the United States. Am. J. Gastroenterol. 2012, 107, 1538–1544. Available online: http://0-insights-ovid-com.brum.beds.ac.uk/crossref?an=00000434-201210000-00017 (accessed on 18 July 2019). [CrossRef] [PubMed]
- Rizvi, S.; Pagnutti, C.; Fraser, E.; Bauch, C.T.; Anand, M. Global land use implications of dietary trends. PLoS ONE 2018, 13, e0200781. [Google Scholar]
- Krueger, H.; Krueger, J.; Koot, J. Variation across Canada in the economic burden attributable to excess weight, tobacco smoking and physical inactivity. Can. J. Public Health 2015, 106, 171–177. Available online: http://journal.cpha.ca/index.php/cjph/article/view/4994/3123 (accessed on 26 September 2018). [CrossRef] [PubMed]

| Food | Chronic Disease | Food Recommendation | Serving Size | CNF/CFG Group Subgroup and Tiers Included for Analysis |
|---|---|---|---|---|
| Fruit | Cancer: Mouth; Larynx; Esophagus; Trachea, Lung, and Bronchus Cardiovascular Disease: Ischemic Heart Disease; Ischemic Stroke; Hemorrhagic Stroke Diabetes | Female and Male † ≤14 years: 2 servings/day 15+ years: 3 servings/day | 80 g | Vegetables and Fruit
|
| Vegetables | Cardiovascular Disease: Ischemic Heart Disease; Ischemic Stroke; Hemorrhagic Stroke | Female † ≤14 years: 3 servings/day 15+ years: 4 servings/day Male † ≤14 years: 3 servings/day15–54 years: 5 servings/day 55+ years: 4 servings/day | 80 g | Vegetables and Fruit (note all corn and potatoes were removed from relevant categories):
|
| Whole Grains | Cardiovascular Disease: Ischemic Heart Disease; Ischemic Stroke; Hemorrhagic Stroke Diabetes | Female †† ≤14 years: 2.5 servings/day 15+ years: 3 servings/day Male †† ≤14 years: 2.5 servings/day 15–54 years: 4 servings/day 55+ years: 3.5 servings/day | 35 g | Grain Products
|
| Nuts and Seeds | Cardiovascular Disease: Ischemic Heart Disease Diabetes | 30 g (~1 Canada Food Guide serving)/d* | 30 g | Meat and Alternatives
|
| Milk | Cancer: Colorectal | 2 cups/day †† | 1 cup (~257.8 g) | Milk and Alternatives (all soy beverages removed)
|
| Red Meat | Cancer: Colorectal Diabetes | No more than 3 × 85 g servings/week (rounded this to <0.5 servings/day) ** | 75 g | Meat and Alternatives (all offal and meat not meeting the International Agency for Research on Cancer criteria for red meat were excluded):
|
| Processed Meat | Cancer: Colorectal Cardiovascular Disease: Ischemic Heart Disease Diabetes | Only for special occasions (assumed 0.05 servings/day servings/day) ** Assumed those who usually consumed <0.25 servings/day had no elevated risk of disease | 75 g | Meat and Alternatives
|
| Sugar-Sweetened Beverages | Cancer: Esophagus; Thyroid; Liver; Pancreas; Colorectal; Breast (post-menopausal); Ovary, Uterus; Kidney; Leukemia Cardiovascular Disease: Ischemic Heart Disease; Ischemic Stroke; Hemorrhagic Stroke Diabetes Chronic Kidney Disease | 5 g g/day *** Assumed those who usually consumed <56.7 g/day had no elevated risk of disease. | 226.8 g | Beverages sweetened with sugar with ≥50 kcal/226.8 g were included from the following categories
|
| Canadian Population in 2018 (‘000) † | Healthful Foods (% Consuming at or Above Recommendation) | Harmful Foods (% Consuming at or Below Recommendation) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nuts and Seeds | Whole Grains | Fruit | Vegetables | Milk | Processed Meat †† | Sugar-Sweetened Beverages * | Red Meat | ||
| Females | |||||||||
| ≤14 years | 2780.6 | 1.1 | 4.8 | 19.0 | 15.9 | 27.6 | 49.3 | 15.8 | 70.1 |
| 15–34 years | 4703.0 | 1.5 | 1.6 | 5.8 | 5.8 | 9.7 | 67.0 | 24.6 | 59.2 |
| 35–54 years | 4989.7 | 3.1 | 1.6 | 8.7 | 13.4 | 6.0 | 70.6 | 48.7 | 44.2 |
| 55–64 years | 2378.0 | 4.3 | 2.4 | 8.9 | 15.7 | 4.7 | 78.4 | 57.7 | 42.0 |
| 65–74 years | 1629.2 | 1.9 | 1.5 | 9.0 | 13.1 | 5.5 | 73.2 | 61.7 | 48.0 |
| 75+ years | 1434.6 | 1.5 | 2.2 | 8.1 | 6.7 | 6.9 | 84.0 | 66.7 | 49.8 |
| Males | |||||||||
| ≤14 years | 2928.0 | 0.8 | 9.1 | 15.7 | 12.2 | 37.8 | 34.4 | 12.5 | 54.8 |
| 15–34 years | 4825.4 | 2.5 | 1.3 | 5.2 | 7.0 | 16.8 | 22.4 | 9.9 | 22.4 |
| 35–54 years | 5002.8 | 3.5 | 1.8 | 9.9 | 9.4 | 6.7 | 28.3 | 29.3 | 17.1 |
| 55–64 years | 2347.5 | 3.5 | 3.5 | 12.6 | 26.1 | 5.8 | 26.2 | 42.5 | 22.1 |
| 65–74 years | 1516.3 | 3.0 | 3.1 | 11.6 | 21.3 | 7.1 | 38.1 | 54.4 | 27.9 |
| 75+ years | 1005.1 | 2.8 | 2.8 | 9.4 | 17.4 | 11.8 | 51.2 | 68.9 | 36.3 |
| Females | Males | Foods Included in Calculations | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤14 years | 15–34 years | 35–54 years | 55–64 years | 65–74 years | 75+ years | ≤14 years | 15–34 years | 35–54 years | 55–64 years | 65–74 years | 75+ years | ||
| Cancer | |||||||||||||
| Mouth | 2.3 | 5.8 | 5.5 | 5.2 | 5.3 | 5.4 | 2.4 | 6.1 | 5.7 | 5.5 | 5.6 | 5.6 | F |
| Larynx | 2.3 | 5.8 | 5.5 | 5.2 | 5.3 | 5.4 | 2.4 | 6.1 | 5.7 | 5.5 | 5.6 | 5.6 | F |
| Thyroid | 0.3 | 0.3 | 0.2 | 0.2 | 0.1 | 0.1 | 0.5 | 0.5 | 0.5 | 0.4 | 0.3 | 0.2 | SSB |
| Trachea, Lung, and Bronchus | 4.2 | 10.1 | 9.6 | 9.1 | 9.3 | 9.5 | 4.3 | 10.6 | 10.0 | 9.6 | 9.7 | 9.9 | F |
| Esophagus | 8.5 | 19.3 | 18.3 | 17.5 | 17.8 | 17.9 | 8.9 | 20.5 | 19.3 | 18.5 | 18.6 | 18.7 | F, SSB |
| Liver | 0.3 | 0.4 | 0.2 | 0.2 | 0.2 | 0.1 | 0.7 | 0.8 | 0.5 | 0.5 | 0.4 | 0.3 | SSB |
| Pancreas | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 | 0.2 | 0.2 | 0.1 | 0.1 | 0.1 | SSB |
| Colorectal | 15.4 | 18.5 | 19.4 | 19.8 | 19.0 | 18.5 | 16.9 | 23.5 | 23.9 | 24.9 | 23.2 | 22.6 | M, RM, PM, SSB |
| Kidney | 0.5 | 0.6 | 0.4 | 0.3 | 0.3 | 0.2 | 0.6 | 0.7 | 0.5 | 0.4 | 0.3 | 0.2 | SSB |
| Leukemia | 0.3 | 0.3 | 0.2 | 0.2 | 0.1 | 0.1 | 0.2 | 0.2 | 0.2 | 0.2 | 0.1 | 0.1 | SSB |
| Post-Menopausal Breast | 0.1 | 0.1 | 0.1 | SSB | |||||||||
| Ovary | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | SSB | ||||||
| Uterus | 1.0 | 1.0 | 0.7 | 0.6 | 0.5 | 0.3 | SSB | ||||||
| Cardiovascular Diseases | |||||||||||||
| Ischemic Heart Disease | 86.2 | 86.8 | 64.1 | 54.1 | 47.2 | 41.7 | 88.3 | 93.0 | 73.9 | 60.5 | 53.1 | 46.6 | F, V, WG, NS, PM, SSB |
| Ischemic Stroke | 76.4 | 89.9 | 61.9 | 47.3 | 34.0 | 14.5 | 76.5 | 94.4 | 70.5 | 50.5 | 36.2 | 15.5 | F, V, WG, SSB |
| Hemorrhagic Stroke | 62.9 | 79.5 | 56.4 | 46.8 | 37.0 | 17.1 | 63.2 | 86.3 | 64.8 | 49.9 | 39.3 | 18.3 | F, V, WG, SSB |
| Diabetes | 64.1 | 70.4 | 54.8 | 45.9 | 37.3 | 23.6 | 71.5 | 83.2 | 68.4 | 57.9 | 47.5 | 30.6 | F, WG, NS, RM, PM, SSB |
| Chronic Kidney Disease | 1.2 | 1.2 | 0.8 | 0.7 | 0.5 | 0.2 | 1.4 | 1.6 | 1.1 | 1.0 | 0.7 | 0.3 | SSB |
| 2018 Costs ($CAN) | |||||||
|---|---|---|---|---|---|---|---|
| Females | Males | Females and Males | |||||
| Direct Costs | Indirect Costs | Direct Costs | Indirect Costs | Direct Costs | Indirect Costs | Total Direct Health and Indirect Costs | |
| Whole Grains | 479,696,161 | 732,962,516 | 1,013,846,354 | 1,592,873,190 | 1,493,542,514 | 2,325,835,706 | 3,819,378,221 |
| Ischemic Heart Disease | 231,644,786 | 404,966,223 | 608,802,593 | 1,064,321,328 | 840,447,379 | 1,469,287,550 | 2,309,734,929 |
| Ischemic Stroke | 28,258,369 | 49,401,867 | 41,805,494 | 73,085,232 | 70,063,862 | 122,487,098 | 192,550,961 |
| Hemorrhagic Stroke | 22,328,761 | 39,035,604 | 27,651,485 | 48,340,901 | 49,980,247 | 87,376,505 | 137,356,752 |
| Diabetes | 197,464,245 | 239,558,823 | 335,586,782 | 407,125,730 | 533,051,027 | 646,684,553 | 1,179,735,579 |
| Nuts and Seeds | 498,432,254 | 782,751,451 | 954,697,875 | 1,546,309,433 | 1,453,130,129 | 2,329,060,883 | 3,782,191,012 |
| Ischemic Heart Disease | 332,804,780 | 581,816,223 | 725,346,710 | 1,268,066,174 | 1,058,151,490 | 1,849,882,397 | 2,908,033,887 |
| Diabetes | 165,627,474 | 200,935,227 | 229,351,164 | 278,243,259 | 394,978,638 | 479,178,486 | 874,157,125 |
| Fruit | 326,305,644 | 596,430,274 | 576,656,369 | 1,049,843,530 | 902,962,012 | 1,646,273,804 | 2,549,235,816 |
| Mouth Cancer | 1,728,793 | 8,442,531 | 3,812,495 | 18,618,252 | 5,541,288 | 27,060,783 | 32,602,071 |
| Laryngeal Cancer | 476,108 | 2,325,065 | 2,075,830 | 10,137,280 | 2,551,938 | 12,462,345 | 15,014,283 |
| Esophageal Cancer | 2,936,399 | 14,339,852 | 9,816,589 | 47,939,145 | 12,752,988 | 62,278,997 | 75,031,985 |
| Tracheal, Bronchial and Lung Cancer | 21,104,161 | 103,061,806 | 23,602,668 | 115,263,226 | 44,706,829 | 218,325,032 | 263,031,861 |
| Ischemic Heart Disease | 137,370,373 | 240,153,738 | 317,238,513 | 554,602,952 | 454,608,886 | 794,756,690 | 1,249,365,576 |
| Ischemic Stroke | 32,067,357 | 56,060,819 | 40,893,335 | 71,490,577 | 72,960,692 | 127,551,396 | 200,512,088 |
| Hemorrhagic Stroke | 25,378,191 | 44,366,681 | 26,858,418 | 46,954,444 | 52,236,609 | 91,321,125 | 143,557,734 |
| Diabetes | 105,244,262 | 127,679,781 | 152,358,521 | 184,837,656 | 257,602,783 | 312,517,437 | 570,120,219 |
| Processed Meat | 146,720,962 | 240,898,174 | 693,784,426 | 1,158,558,074 | 840,505,388 | 1,399,456,248 | 2,239,961,636 |
| Colon and Rectal Cancer | 7,435,911 | 36,313,146 | 27,537,031 | 134,476,619 | 34,972,943 | 170,789,766 | 205,762,708 |
| Ischemic Heart Disease | 66,551,012 | 116,345,861 | 403,342,304 | 705,131,386 | 469,893,316 | 821,477,247 | 1,291,370,563 |
| Diabetes | 72,734,038 | 88,239,168 | 262,905,091 | 318,950,068 | 335,639,129 | 407,189,236 | 742,828,365 |
| Vegetables | 190,257,302 | 332,611,764 | 436,385,955 | 762,898,984 | 626,643,257 | 1,095,510,748 | 1,722,154,005 |
| Ischemic Heart Disease | 166,710,242 | 291,446,305 | 405,516,582 | 708,932,505 | 572,226,824 | 1,000,378,809 | 1,572,605,633 |
| Ischemic Stroke | 13,301,355 | 23,253,704 | 17,991,402 | 31,452,942 | 31,292,757 | 54,706,647 | 85,999,403 |
| Hemorrhagic Stroke | 10,245,706 | 17,911,755 | 12,877,971 | 22,513,537 | 23,123,677 | 40,425,292 | 63,548,969 |
| Sugar-Sweetened Beverages | 109,485,809 | 140,609,158 | 255,443,721 | 324,647,983 | 364,929,531 | 465,257,142 | 830,186,672 |
| Esophageal Cancer | 49,594 | 242,189 | 270,047 | 1,318,772 | 319,641 | 1,560,961 | 1,880,602 |
| Thyroid Cancer | 76,400 | 373,097 | 54,084 | 264,117 | 130,484 | 637,214 | 767,698 |
| Liver Cancer | 9898 | 48,336 | 80,200 | 391,655 | 90,098 | 439,991 | 530,089 |
| Pancreatic Cancer | 43,910 | 214,434 | 59,525 | 290,688 | 103,435 | 505,122 | 608,556 |
| Colorectal Cancer | 170,942 | 834,793 | 1,018,775 | 4,975,168 | 1,189,717 | 5,809,961 | 6,999,677 |
| Breast Cancer | 347,638 | 1,697,684 | 347,638 | 1,697,684 | 2,045,322 | ||
| Ovarian Cancer | 25,635 | 125,189 | 25,635 | 125,189 | 150,824 | ||
| Uterine Cancer | 380,325 | 1,857,312 | 380,325 | 1,857,312 | 2,237,637 | ||
| Kidney Cancer | 290,291 | 1,417,629 | 192,135 | 938,286 | 482,425 | 2,355,915 | 2,838,340 |
| Leukemia | 196,821 | 961,173 | 179,011 | 874,199 | 375,833 | 1,835,372 | 2,211,205 |
| Ischemic Heart Disease | 4,228,109 | 7,391,669 | 15,693,878 | 27,436,363 | 19,921,987 | 34,828,032 | 54,750,019 |
| Ischemic Stroke | 463,246 | 809,857 | 966,438 | 1,689,547 | 1,429,684 | 2,499,404 | 3,929,088 |
| Hemorrhagic Stroke | 697,652 | 1,219,649 | 1,089,408 | 1,904,525 | 1,787,059 | 3,124,174 | 4,911,233 |
| Diabetes | 101,401,444 | 123,017,768 | 234,020,470 | 283,907,948 | 335,421,915 | 406,925,716 | 742,347,631 |
| Chronic Kidney Disease | 1,103,904 | 398,379 | 1,819,751 | 656,715 | 2,923,655 | 1,055,094 | 3,978,750 |
| Milk | 50,108,728 | 244,705,113 | 63,055,698 | 307,931,418 | 113,164,426 | 552,636,531 | 665,800,957 |
| Colon and Rectal Cancer | 50,108,728 | 244,705,113 | 63,055,698 | 307,931,418 | 113,164,426 | 552,636,531 | 665,800,957 |
| Red Meat | 17,465,576 | 32,182,526 | 63,406,702 | 117,840,630 | 80,872,278 | 150,023,157 | 230,895,435 |
| Colon and Rectal Cancer | 2,995,312 | 14,627,554 | 11,148,157 | 54,441,833 | 14,143,469 | 69,069,386 | 83,212,855 |
| Diabetes | 14,470,264 | 17,554,973 | 52,258,546 | 63,398,798 | 66,728,810 | 80,953,770 | 147,682,580 |
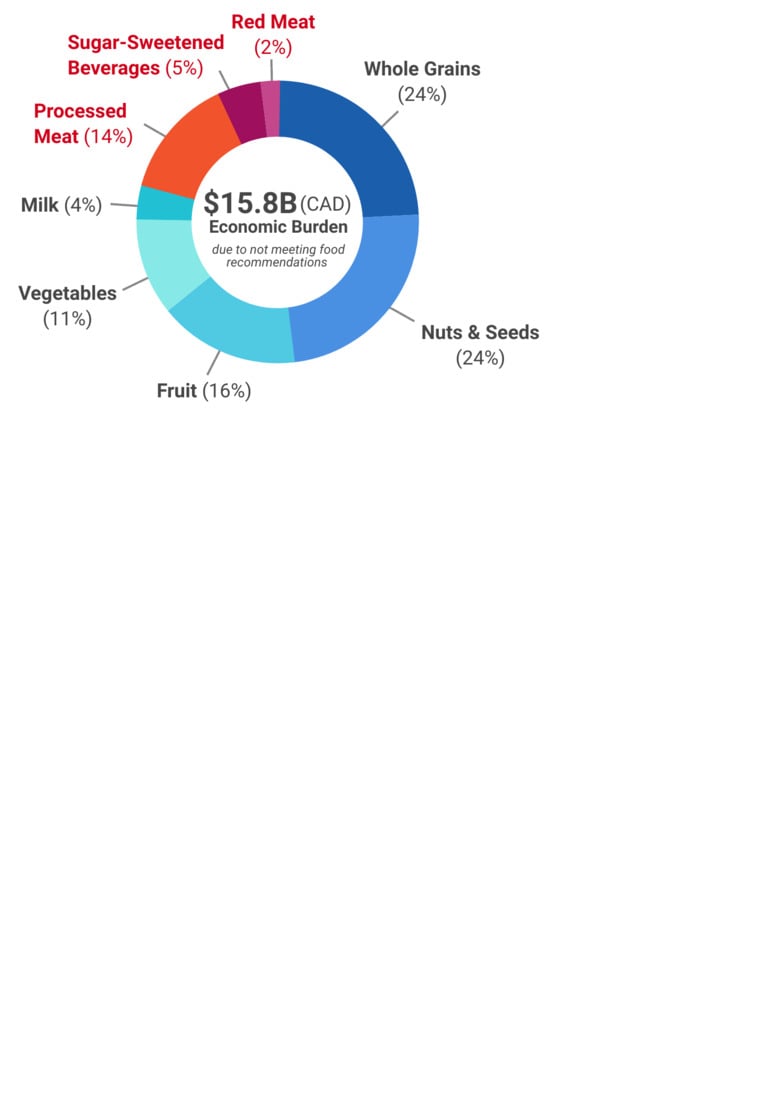
| TOTAL COSTS | 1,818,472,435 | 3,103,150,976 | 4,057,277,100 | 6,860,903,243 | 5,875,749,535 | 9,964,054,219 | 15,839,803,754 |
| 2018 Costs ($CAN) | Percent of Costs | ||||
|---|---|---|---|---|---|
| Direct Costs | Indirect Costs | Total Direct and Indirect Costs | Costs within Sex Group | Total Costs | |
| Females | 1,936,570,565 | 3,302,166,717 | 5,238,737,282 | 100.0% | 33.1% |
| ≤14 years | 12,040,403 | 15,666,224 | 27,706,627 | 0.5% | 0.2% |
| 15–34 years | 76,513,918 | 100,906,919 | 177,420,837 | 3.4% | 1.1% |
| 35–54 years | 386,859,501 | 595,385,456 | 982,244,957 | 18.7% | 6.2% |
| 55–64 years | 440,519,124 | 728,965,831 | 1,169,484,955 | 22.3% | 7.4% |
| 65–74 years | 480,354,720 | 840,813,557 | 1,321,168,277 | 25.2% | 8.3% |
| 75+ years | 540,282,899 | 1,020,428,729 | 1,560,711,628 | 29.8% | 9.9% |
| Males | 3,939,178,970 | 6,661,887,503 | 10,601,066,473 | 100.0% | 66.9% |
| ≤14 years | 24,667,689.36 | 31,113,645.39 | 55,781,335 | 0.5% | 0.4% |
| 15–34 years | 87,878,603 | 118,808,699 | 206,687,302 | 1.9% | 1.3% |
| 35–54 years | 1,076,934,563 | 1,651,501,848 | 2,728,436,411 | 25.7% | 17.2% |
| 55–64 years | 1,074,108,771 | 1,808,010,348 | 2,882,119,119 | 27.2% | 18.2% |
| 65–74 years | 972,731,815 | 1,717,252,172 | 2,689,983,987 | 25.4% | 17.0% |
| 75+ years | 702,857,528 | 1,335,200,790 | 2,038,058,318 | 19.2% | 12.9% |
| All years | 3,939,178,970 | 6,661,887,503 | 10,601,066,473 | 100.0% | 66.9% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loewen, O.K.; Ekwaru, J.P.; Ohinmmaa, A.; Veugelers, P.J. Economic Burden of Not Complying with Canadian Food Recommendations in 2018. Nutrients 2019, 11, 2529. https://0-doi-org.brum.beds.ac.uk/10.3390/nu11102529
Loewen OK, Ekwaru JP, Ohinmmaa A, Veugelers PJ. Economic Burden of Not Complying with Canadian Food Recommendations in 2018. Nutrients. 2019; 11(10):2529. https://0-doi-org.brum.beds.ac.uk/10.3390/nu11102529
Chicago/Turabian StyleLoewen, Olivia K., John P. Ekwaru, Arto Ohinmmaa, and Paul J. Veugelers. 2019. "Economic Burden of Not Complying with Canadian Food Recommendations in 2018" Nutrients 11, no. 10: 2529. https://0-doi-org.brum.beds.ac.uk/10.3390/nu11102529