Malnutrition in Hospitalized Old Patients: Screening and Diagnosis, Clinical Outcomes, and Management
Abstract
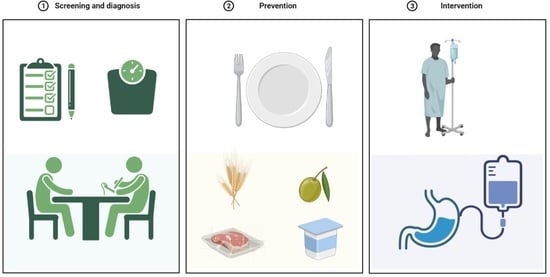
:1. Introduction
2. Definition of Malnutrition
3. Screening and Assessment of Malnutrition in the Acute Setting
4. Epidemiology of Hospital Malnutrition
4.1. Prevalence of Malnutrition in Hospital Setting
4.2. Risk of Malnutrition during Hospitalization
4.3. Risk Factors for Malnutrition in Hospitalized Patients
5. Clinical Outcomes of Malnutrition in Hospitalized Patients
5.1. Malnutrition and Length of Stay
5.2. Malnutrition, Falls, and Other Complications of Hospitalization
5.3. Malnutrition, Muscle and Functional Impairment, and Quality of Life
5.4. Malnutrition, Hospital Readmission, and Mortality
6. Management of Malnutrition in the Hospital
6.1. Diagnosis
6.2. Complementary Procedures
6.3. Nutritional Recommendations
6.4. Food Adaptation
6.5. Oral Supplements
6.6. Enteral and Parenteral Nutrition
6.7. Effect of Nutritional Interventions in Hospital
7. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Correia, M.I.T.D.; Perman, M.I.; Waitzberg, D.L. Hospital malnutrition in Latin America: A systematic review. Clin. Nutr. 2017, 36, 958–967. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellanti, F.; lo Buglio, A.; Quiete, S.; Pellegrino, G.; Dobrakowski, M.; Kasperczyk, A.; Kasperczyk, S.; Vendemiale, G. Comparison of three nutritional screening tools with the new glim criteria for malnutrition and association with sarcopenia in hospitalized older patients. J. Clin. Med. 2020, 9, 1898. [Google Scholar] [CrossRef] [PubMed]
- Guenter, P.; Abdelhadi, R.; Anthony, P.; Blackmer, A.; Malone, A.; Mirtallo, J.M.; Phillips, W.; Resnick, H.E. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States, 2018. Nutr. Clin. Pract. 2021, 36, 957–969. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, L.L.; Kashiwagi, D.T.; Brantley, S.; Scheurer, D.; Varkey, P. Nutrition in the hospitalized patient. J. Hosp. Med. 2013, 8, 52–58. [Google Scholar] [CrossRef]
- Inciong, J.F.B.; Chaudhary, A.; Hsu, H.S.; Joshi, R.; Seo, J.M.; Trung, L.V.; Ungpinitpong, W.; Usman, N. Hospital malnutrition in northeast and southeast Asia: A systematic literature review. Clin. Nutr. ESPEN 2020, 39, 30–45. [Google Scholar] [CrossRef]
- Schuetz, P.; Seres, D.; Lobo, D.N.; Gomes, F.; Kaegi-Braun, N.; Stanga, Z. Management of disease-related malnutrition for patients being treated in hospital. Lancet 2021, 398, 1927–1938. [Google Scholar] [CrossRef]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Prognostic impact of disease-related malnutrition. Clin. Nutr. 2008, 27, 5–15. [Google Scholar] [CrossRef]
- Power, L.; Mullally, D.; Gibney, E.R.; Clarke, M.; Visser, M.; Volkert, D.; Bardon, L.; de van der Schueren, M.A.E.; Corish, C.A. A review of the validity of malnutrition screening tools used in older adults in community and healthcare settings—A MaNuEL study. Clin. Nutr. ESPEN 2018, 24, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Galindo Martín, C.A.; Aportela Vázquez, V.A.; Becerril Hernández, F.; Aguilar Medina, C.R.; Ayala Carrillo, S.L.; Chávez Flores, A.; Gabriel Almanza, E.; Guizar Agredano, M.I.; Montoya Vilchis, J.D. The GLIM criteria for adult malnutrition and its relation with adverse outcomes, a prospective observational study. Clin. Nutr. ESPEN 2020, 38, 67–73. [Google Scholar] [CrossRef]
- Sánchez-Rodríguez, D.; Marco, E.; Ronquillo-Moreno, N.; Maciel-Bravo, L.; Gonzales-Carhuancho, A.; Duran, X.; Guillén-Solà, A.; Vázquez-Ibar, O.; Escalada, F.; Muniesa, J.M. ASPEN-AND-ESPEN: A postacute-care comparison of the basic definition of malnutrition from the American Society of Parenteral and Enteral Nutrition and Academy of Nutrition and Dietetics with the European Society for Clinical Nutrition and Metabolism definition. Clin. Nutr. 2019, 38, 297–302. [Google Scholar]
- Jensen, G.L.; Cederholm, T.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; de Baptista, G.A.; Barazzoni, R.; Blaauw, R.; Coats, A.J.S.; et al. GLIM Criteria for the Diagnosis of Malnutrition: A Consensus Report From the Global Clinical Nutrition Community. J. Parenter. Enter. Nutr. 2019, 43, 32–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teigen, L.M.; Kuchnia, A.J.; Nagel, E.M.; Price, K.L.; Hurt, R.T.; Earthman, C.P. Diagnosing clinical malnutrition: Perspectives from the past and implications for the future. Clin. Nutr. ESPEN 2018, 26, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Hoogendijk, E.O.; Visvanathan, R.; Wright, O.R.L. Malnutrition Screening and Assessment in Hospitalised Older People: A Review. J. Nutr. Health Aging 2019, 23, 431–441. [Google Scholar] [CrossRef]
- White, J.V.; Guenter, P.; Jensen, G.; Malone, A.; Schofield, M. Consensus Statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition. J. Parenter. Enter. Nutr. 2012, 36, 275–283. [Google Scholar] [CrossRef] [Green Version]
- Malnutrition. Available online: https://www.who.int/news-room/questions-and-answers/item/malnutrition (accessed on 22 January 2022).
- Roberts, S.; Collins, P.; Rattray, M. Identifying and Managing Malnutrition, Frailty and Sarcopenia in the Community: A Narrative Review. Nutrients 2021, 13, 2316. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Cederholm, T.; Bosaeus, I.; Barazzoni, R.; Bauer, J.; Van Gossum, A.; Klek, S.; Muscaritoli, M.; Nyulasi, I.; Ockenga, J.; Schneider, S.M.M.; et al. Diagnostic criteria for malnutrition—An ESPEN Consensus Statement. Clin. Nutr. 2015, 34, 335–340. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Kirkland, L.L.; Shaughnessy, E. Recognition and Prevention of Nosocomial Malnutrition: A Review and A Call to Action! Am. J. Med. 2017, 130, 1345–1350. [Google Scholar] [CrossRef] [Green Version]
- Elia, M. Defining, Recognizing, and Reporting Malnutrition. Int. J. Low. Extrem. Wounds 2017, 16, 230–237. [Google Scholar] [CrossRef]
- Skipper, A.; Ferguson, M.; Thompson, K.; Castellanos, V.H.; Porcari, J. Nutrition screening tools: An analysis of the evidence. JPEN J. Parenter. Enteral Nutr. 2012, 36, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Van Bokhorst-de van der Schueren, M.A.E.; Guaitoli, P.R.; Jansma, E.P.; de Vet, H.C.W. Nutrition screening tools: Does one size fit all? A systematic review of screening tools for the hospital setting. Clin. Nutr. 2014, 33, 39–58. [Google Scholar] [CrossRef] [PubMed]
- Reber, E.; Gomes, F.; Bally, L.; Schuetz, P.; Stanga, Z. Nutritional Management of Medical Inpatients. J. Clin. Med. 2019, 8, 1130. [Google Scholar] [CrossRef] [Green Version]
- Moreira, N.C.F.; Krausch-Hofmann, S.; Matthys, C.; Vereecken, C.; Vanhauwaert, E.; Declercq, A.; Bekkering, G.E.; Duyck, J. Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef] [PubMed]
- Cereda, E.; Pedrolli, C.; Klersy, C.; Bonardi, C.; Quarleri, L.; Cappello, S.; Turri, A.; Rondanelli, M.; Caccialanza, R. Nutritional status in older persons according to healthcare setting: A systematic review and meta-analysis of prevalence data using MNA®. Clin. Nutr. 2016, 35, 1282–1290. [Google Scholar] [CrossRef]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cereda, E.; Cruz-Jentoft, A.; Goisser, S.; dde Groot, L.; Großhauser, F.; Kiesswetter, E.; Norman, K.; et al. Management of malnutrition in older patients—current approaches, evidence and open questions. J. Clin. Med. 2019, 8, 974. [Google Scholar] [CrossRef] [Green Version]
- Orlandoni, P.; Venturini, C.; Jukic Peladic, N.; Costantini, A.; Di Rosa, M.; Cola, C.; Giorgini, N.; Basile, R.; Fagnani, D.; Sparvoli, D.; et al. Malnutrition upon Hospital Admission in Geriatric Patients: Why Assess It? Front. Nutr. 2017, 4, 50. [Google Scholar] [CrossRef] [Green Version]
- Leegaard Andersen, A.; Lundsgaard Nielsen, R.; Baltzer Houlind, M.; Tavenier, J.; Rasmussen, L.J.H.; Mørch Jørgensen, L.; Treldal, C.; Marie Beck, A.; Merete Pedersen, M.; Andersen, O.; et al. Risk of Malnutrition upon Admission and after Discharge in Acutely Admitted Older Medical Patients: A Prospective Observational Study. Nutrients 2021, 13, 2757. [Google Scholar] [CrossRef]
- Lueg, G.; Wirth, R.; Kwiatkowski, J.; Rösler, A.; Jäger, M.; Gehrke, I.; Volkert, D.; Pourhassan, M. Low Self-Perception of Malnutrition in Older Hospitalized Patients. Clin. Interv. Aging 2020, 15, 2219–2226. [Google Scholar] [CrossRef]
- Zadak, Z.; Hyspler, R.; Ticha, A.; Vlcek, J. Polypharmacy and malnutrition. Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 50–55. [Google Scholar] [CrossRef]
- Correia, M.I.T.D.; Hegazi, R.A.; Higashiguchi, T.; Michel, J.P.; Reddy, B.R.; Tappenden, K.A.; Uyar, M.; Muscaritoli, M. Evidence-based recommendations for addressing malnutrition in health care: An updated strategy from the feedM.E. Global Study Group. J. Am. Med. Dir. Assoc. 2014, 15, 544–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weijzen, M.E.G.; Kouw, I.W.K.; Geerlings, P.; Verdijk, L.B.; van Loon, L.J.C. During Hospitalization, Older Patients at Risk for Malnutrition Consume <0.65 Grams of Protein per Kilogram Body Weight per Day. Nutr. Clin. Pract. 2020, 35, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Witney-Cochrane, K.; Cunich, M.; Ferrie, S.; Carey, S. Defining and quantifying preventable and non-preventable hospital-acquired malnutrition—A cohort study. Nutr. Diet. 2019, 76, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Schneider, S.M.; Pirlich, M.; Lochs, H.; Hebuterne, X.; Pichard, C. Does nutritional risk, as assessed by Nutritional Risk Index, increase during hospital stay? A multinational population-based study. Clin. Nutr. 2005, 24, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Allard, J.P.; Keller, H.; Jeejeebhoy, K.N.; Laporte, M.; Duerksen, D.R.; Gramlich, L.; Payette, H.; Bernier, P.; Davidson, B.; Teterina, A.; et al. Decline in nutritional status is associated with prolonged length of stay in hospitalized patients admitted for 7 days or more: A prospective cohort study. Clin. Nutr. 2016, 35, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, A.J.; Buitrago, G.; Rodríguez, N.; Gómez, G.; Sulo, S.; Gómez, C.; Partridge, J.; Misas, J.; Dennis, R.; Alba, M.J.; et al. Clinical and economic outcomes associated with malnutrition in hospitalized patients. Clin. Nutr. 2019, 38, 1310–1316. [Google Scholar] [CrossRef] [Green Version]
- Woodward, T.; Josephson, C.; Ross, L.; Hill, J.; Hosking, B.; Naumann, F.; Stoney, R.; Palmer, M. A retrospective study of the incidence and characteristics of long-stay adult inpatients with hospital-acquired malnutrition across five Australian public hospitals. Eur. J. Clin. Nutr. 2020, 74, 1668–1676. [Google Scholar] [CrossRef]
- Kubrak, C.; Jensen, L. Malnutrition in acute care patients: A narrative review. Int. J. Nurs. Stud. 2007, 44, 1036–1054. [Google Scholar] [CrossRef]
- Sergi, G.; Bano, G.; Pizzato, S.; Veronese, N.; Manzato, E. Taste loss in the elderly: Possible implications for dietary habits. Crit. Rev. Food Sci. Nutr. 2017, 57, 3684–3689. [Google Scholar] [CrossRef]
- Amarya, S.; Singh, K.; Sabharwal, M. Changes during aging and their association with malnutrition. J. Clin. Gerontol. Geriatr. 2015, 6, 78–84. [Google Scholar] [CrossRef] [Green Version]
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in Older Adults—Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef] [PubMed]
- Rafaella, F.; Silva, M.; Gondim, M.; Aquino De Oliveira, O.; Sandro, A.; Souza, R.; Figueroa, J.N.; Santos, C.S. Factors associated with malnutrition in hospitalized cancer patients: A croos-sectional study. Nutr. J. 2015, 14, 123. [Google Scholar]
- Planas, M.; Álvarez-Hernández, J.; León-Sanz, M.; Celaya-Pérez, S.; Araujo, K.; García de Lorenzo, A. Prevalence of hospital malnutrition in cancer patients: A sub-analysis of the PREDyCES® study. Support. Care Cancer 2016, 24, 429–435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chien, S.C.; Lo, C.I.; Lin, C.F.; Sung, K.T.; Tsai, J.P.; Huang, W.H.; Yun, C.H.; Hung, T.C.; Lin, J.L.; Liu, C.Y.; et al. Malnutrition in acute heart failure with preserved ejection fraction: Clinical correlates and prognostic implications. ESC Hear. Fail. 2019, 6, 953–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Czapla, M.; Juárez-Vela, R.; Łokieć, K.; Karniej, P. The Association between Nutritional Status and In-Hospital Mortality among Patients with Heart Failure—A Result of the Retrospective Nutritional Status Heart Study 2 (NSHS2). Nutrients 2021, 13, 1669. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Choe, Y.; Mustad, V.A.; Chakraborty, S.; Goates, S.; Luo, M.; Mechanick, J.I. Impact of malnutrition on survival and healthcare utilization in Medicare beneficiaries with diabetes: A retrospective cohort analysis. BMJ Open Diabetes Res. Care 2018, 6, e000471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramos, F.D.; Fontanilla, J.A.; Lat, R.E. Association between Degrees of Malnutrition and Clinical Outcomes among Non-critically Ill Hospitalized Adult Patients with Type 2 Diabetes Mellitus. J. ASEAN Fed. Endocr. Soc. 2021, 36, 172–179. [Google Scholar] [CrossRef]
- Nakamura, T.; Itoh, T.; Yabe, A.; Imai, S.; Nakamura, Y.; Mizokami, Y.; Okouchi, Y.; Ikeshita, A.; Kominato, H. Polypharmacy is associated with malnutrition and activities of daily living disability among daycare facility users: A cross-sectional study. Medicine 2021, 100, e27073. [Google Scholar] [CrossRef]
- Bardon, L.A.; Corish, C.A.; Lane, M.; Bizzaro, M.G.; Loayza Villarroel, K.; Clarke, M.; Power, L.C.; Gibney, E.R.; Dominguez Castro, P. Ageing rate of older adults affects the factors associated with, and the determinants of malnutrition in the community: A systematic review and narrative synthesis. BMC Geriatr. 2021, 21, 1–39. [Google Scholar] [CrossRef]
- Katsas, K.; Mamalaki, E.; Kontogianni, M.D.; Anastasiou, C.A.; Kosmidis, M.H.; Varlamis, I.; Hadjigeorgiou, G.M.; Dardiotis, E.; Sakka, P.; Scarmeas, N.; et al. Malnutrition in older adults: Correlations with social, diet-related, and neuropsychological factors. Nutrition 2020, 71, 110640. [Google Scholar] [CrossRef]
- lo Buglio, A.; Bellanti, F.; Capurso, C.; Paglia, A.; Vendemiale, G. Adherence to Mediterranean Diet, Malnutrition, Length of Stay and Mortality in Elderly Patients Hospitalized in Internal Medicine Wards. Nutrients 2019, 11, 790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pirlich, M.; Schütz, T.; Kemps, M.; Luhman, N.; Minko, N.; Lübke, H.J.; Rossnagel, K.; Willich, S.N.; Lochs, H. Social risk factors for hospital malnutrition. Nutrients 2005, 21, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Westergren, A.; Lindholm, C.; Axelsson, C.; Ulander, K. Prevalence of eating difficulties and malnutrition among persons within hospital care and special accommodations. J. Nutr. Health Aging 2008, 12, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Krzymińska-Siemaszko, R.; Deskur-Śmielecka, E.; Kaluźniak-Szymanowska, A.; Kaczmarek, B.; Kujawska-Danecka, H.; Klich-Rączka, A.; Mossakowska, M.; Małgorzewicz, S.; Dworak, L.B.; Kostka, T.; et al. Socioeconomic Risk Factors of Poor Nutritional Status in Polish Elderly Population: The Results of PolSenior2 Study. Nutrients 2021, 13, 4388. [Google Scholar] [CrossRef] [PubMed]
- Delerue Matos, A.; Barbosa, F.; Cunha, C.; Voss, G.; Correia, F. Social isolation, physical inactivity and inadequate diet among European middle-aged and older adults. BMC Public Health 2021, 21, 1–12. [Google Scholar] [CrossRef]
- Amaral, T.F.; Matos, L.C.; Teixeira, M.A.; Tavares, M.M.; Álvares, L.; Antunes, A.; Hospital, D.; Hispano, P.; Matosinhos, U.; Regional De Saúde, S.; et al. Undernutrition and associated factors among hospitalized patients. Clin. Nutr. 2010, 29, 580–585. [Google Scholar] [CrossRef]
- Besora-Moreno, M.; Llauradó, E.; Tarro, L.; Solà, R. Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2020, 12, 737. [Google Scholar] [CrossRef] [Green Version]
- Ross, L.J.; Wilson, M.; Banks, M.; Rezannah, F.; Daglish, M. Prevalence of malnutrition and nutritional risk factors in patients undergoing alcohol and drug treatment. Nutrition 2012, 28, 738–743. [Google Scholar] [CrossRef]
- Teixeira, J.; Mota, T.; Fernandes, J.C. Nutritional evaluation of alcoholic inpatients admitted for alcohol detoxification. Alcohol Alcohol. 2011, 46, 558–560. [Google Scholar] [CrossRef] [Green Version]
- Kiss, N.; Hiesmayr, M.; Sulz, I.; Bauer, P.; Heinze, G.; Mouhieddine, M.; Schuh, C.; Tarantino, S.; Simon, J. Predicting Hospital Length of Stay at Admission Using Global and Country-Specific Competing Risk Analysis of Structural, Patient, and Nutrition-Related Data from nutritionDay 2007–2015. Nutrients 2021, 13, 4111. [Google Scholar] [CrossRef]
- Rojas-García, A.; Turner, S.; Pizzo, E.; Hudson, E.; Thomas, J.; Raine, R. Impact and experiences of delayed discharge: A mixed-studies systematic review. Health Expect. 2018, 21, 41–56. [Google Scholar] [CrossRef] [PubMed]
- Felder, S.; Lechtenboehmer, C.; Bally, M.; Fehr, R.; Deiss, M.; Faessler, L.; Kutz, A.; Steiner, D.; Rast, A.C.; Laukemann, S.; et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition 2015, 31, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- Lima, J.; Teixeira, P.P.; Eckert, I.D.C.; Burgel, C.F.; Silva, F.M. Decline of nutritional status in the first week of hospitalisation predicts longer length of stay and hospital readmission during 6-month follow-up. Br. J. Nutr. 2021, 125, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Eglseer, D.; Hoedl, M.; Schoberer, D. Malnutrition risk and hospital-acquired falls in older adults: A cross-sectional, multicenter study. Geriatr. Gerontol. Int. 2020, 20, 348–353. [Google Scholar] [CrossRef] [Green Version]
- Ishida, Y.; Maeda, K.; Nonogaki, T.; Shimizu, A.; Yamanaka, Y.; Matsuyama, R.; Kato, R.; Mori, N. Malnutrition at Admission Predicts In-Hospital Falls in Hospitalized Older Adults. Nutrients 2020, 12, 541. [Google Scholar] [CrossRef] [Green Version]
- Lackoff, A.S.; Hickling, D.; Collins, P.F.; Stevenson, K.J.; Nowicki, T.A.; Bell, J.J. The association of malnutrition with falls and harm from falls in hospital inpatients: Findings from a 5-year observational study. J. Clin. Nurs. 2020, 29, 429–436. [Google Scholar] [CrossRef]
- Abugroun, A.; Nayyar, A.; Abdel-Rahman, M.; Patel, P. Impact of Malnutrition on Hospitalization Outcomes for Older Adults Admitted for Sepsis. Am. J. Med. 2021, 134, 221–226.e1. [Google Scholar] [CrossRef]
- Paillaud, E.; Herbaud, S.; Caillet, P.; Lejonc, J.L.; Campillo, B.; Bories, P.N. Relations between undernutrition and nosocomial infections in elderly patients. Age Ageing 2005, 34, 619–625. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Wu, H.; Jiang, J.; Xu, K.; Gao, S.; Chen, L.; Wang, H.; Li, X. Nutritional risk screening score as an independent predictor of nonventilator hospital-acquired pneumonia: A cohort study of 67,280 patients. BMC Infect. Dis. 2021, 21, 1–10. [Google Scholar] [CrossRef]
- Rosted, E.; Prokofieva, T.; Sanders, S.; Schultz, M. Serious Consequences of Malnutrition and Delirium in Frail Older Patients. J. Nutr. Gerontol. Geriatr. 2018, 37, 105–116. [Google Scholar] [CrossRef]
- Pourhassan, M.; Rommersbach, N.; Lueg, G.; Klimek, C.; Schnatmann, M.; Liermann, D.; Janssen, G.; Wirth, R. The Impact of Malnutrition on Acute Muscle Wasting in Frail Older Hospitalized Patients. Nutrients 2020, 12, 1387. [Google Scholar] [CrossRef] [PubMed]
- lo Buglio, A.; Bellanti, F.; Serviddio, G.; Vendemiale, G. Impact of Nutritional Status on Muscle Architecture in Elderly Patients Hospitalized in Internal Medicine Wards. J. Nutr. Health Aging 2020, 24, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Esmayel, E.M.M.; Eldarawy, M.M.; Hassan, M.M.M.; Hassanin, H.M.; Reda Ashour, W.M.; Mahmoud, W. Nutritional and functional assessment of hospitalized elderly: Impact of sociodemographic variables. J. Aging Res. 2013, 2013, 101725. [Google Scholar] [CrossRef] [Green Version]
- Hettiarachchi, J.; Reijnierse, E.M.; Soh, C.H.; Agius, B.; Fetterplace, K.; Lim, W.K.; Maier, A.B. Malnutrition is associated with poor trajectories of activities of daily living in geriatric rehabilitation inpatients: RESORT. Mech. Ageing Dev. 2021, 197, 111500. [Google Scholar] [CrossRef] [PubMed]
- Lengfelder, L.; Mahlke, S.; Moore, L.; Zhang, X.; Williams, G.; Lee, J. Prevalence and impact of malnutrition on length of stay, readmission, and discharge destination. J. Parenter. Enter. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- Fitriana, I.; Setiati, S.; Rizal, E.W.; Istanti, R.; Rinaldi, I.; Kojima, T.; Akishita, M.; Azwar, M.K. Malnutrition and depression as predictors for 30-day unplanned readmission in older patient: A prospective cohort study to develop 7-point scoring system. BMC Geriatr. 2021, 21, 1–10. [Google Scholar] [CrossRef]
- Cruz, P.L.M.; de Soares, B.L.M.; da Silva, J.E.; Lima e Silva, R.R. de Clinical and nutritional predictors of hospital readmission within 30 days. Eur. J. Clin. Nutr. 2021, 2021, 1–7. [Google Scholar]
- Sharma, Y.; Miller, M.; Kaambwa, B.; Shahi, R.; Hakendorf, P.; Horwood, C.; Thompson, C. Malnutrition and its association with readmission and death within 7 days and 8–180 days postdischarge in older patients: A prospective observational study. BMJ Open 2017, 7, e018443. [Google Scholar]
- Snider, J.T.; Jena, A.B.; Linthicum, M.T.; Hegazi, R.A.; Partridge, J.S.; LaVallee, C.; Lakdawalla, D.N.; Wischmeyer, P.E. Effect of hospital use of oral nutritional supplementation on length of stay, hospital cost, and 30-day readmissions among Medicare patients with COPD. Chest 2015, 147, 1477–1484. [Google Scholar] [CrossRef] [Green Version]
- Yang, P.H.; Lin, M.C.; Liu, Y.Y.; Lee, C.L.; Chang, N.J. Effect of Nutritional Intervention Programs on Nutritional Status and Readmission Rate in Malnourished Older Adults with Pneumonia: A Randomized Control Trial. Int. J. Environ. Res. Public Health 2019, 16, 4758. [Google Scholar] [CrossRef] [Green Version]
- Lim, S.L.; Ong, K.C.B.; Chan, Y.H.; Loke, W.C.; Ferguson, M.; Daniels, L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin. Nutr. 2012, 31, 345–350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Correia, M.I.T.D.; Sulo, S.; Brunton, C.; Sulz, I.; Rodriguez, D.; Gomez, G.; Tarantino, S.; Hiesmayr, M. Prevalence of malnutrition risk and its association with mortality: NutritionDay Latin America survey results. Clin. Nutr. 2021, 40, 5114–5121. [Google Scholar] [CrossRef] [PubMed]
- Kaegi-Braun, N.; Mueller, M.; Schuetz, P.; Mueller, B.; Kutz, A. Evaluation of Nutritional Support and In-Hospital Mortality in Patients With Malnutrition. JAMA Netw. Open 2021, 4, e2033433. [Google Scholar] [CrossRef] [PubMed]
- Lew, C.C.H.; Wong, G.J.Y.; Cheung, K.P.; Chua, A.P.; Chong, M.F.F.; Miller, M. Association between Malnutrition and 28-Day Mortality and Intensive Care Length-of-Stay in the Critically ill: A Prospective Cohort Study. Nutrients 2017, 10, 10. [Google Scholar] [CrossRef] [Green Version]
- Lew, C.C.H.; Yandell, R.; Fraser, R.J.L.L.; Chua, A.P.; Chong, M.F.F.; Miller, M. Association Between Malnutrition and Clinical Outcomes in the Intensive Care Unit: A Systematic Review. J. Parenter. Enter. Nutr. 2017, 41, 744–758. [Google Scholar] [CrossRef]
- Bonetti, L.; Terzoni, S.; Lusignani, M.; Negri, M.; Froldi, M.; Destrebecq, A. Prevalence of malnutrition among older people in medical and surgical wards in hospital and quality of nutritional care: A multicenter, cross-sectional study. J. Clin. Nurs. 2017, 26, 5082–5092. [Google Scholar] [CrossRef]
- Swan, I.; Nyulasi, I.; Collins, K.; Weir-Phyland, J.; Bolster, D.; Burgell, R.; Fineberg, D.; Johnson, W.; King, S.; Leong, R.; et al. Identification and management of malnutrition in hospitalised patients: A survey of staff knowledge and attitudes. Clin. Nutr. Exp. 2020, 31, 8–18. [Google Scholar] [CrossRef]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin. Nutr. 2019, 38, 10–47. [Google Scholar] [CrossRef] [Green Version]
- Deer, R.R.; Volpi, E. Protein Requirements in Critically Ill Older Adults. Nutrients 2018, 10, 378. [Google Scholar] [CrossRef] [Green Version]
- Kruizenga, H.M.; Schager, M.; van Dronkelaar, C.; Naumann, E. Protein intake during hospital admission; Dutch national data on protein intake in 339,720 malnourished patients from 2009–2019. Clin. Nutr. Open Sci. 2022, 41, 74–81. [Google Scholar] [CrossRef]
- Schindler, K.; Themessl-Huber, M.; Hiesmayr, M.; Kosak, S.; Lainscak, M.; Laviano, A.; Ljungqvist, O.; Mouhieddine, M.; Schneider, S.; De Van Der Schueren, M.; et al. To eat or not to eat? Indicators for reduced food intake in 91,245 patients hospitalized on nutritionDays 2006–2014 in 56 countries worldwide: A descriptive analysis. Am. J. Clin. Nutr. 2016, 104, 1393–1402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonnefoy, M.; Gilbert, T.; Normand, S.; Jauffret, M.; Roy, P.; Morio, B.; Cornu, C.; Roche, S.; Laville, M. Energy Expenditure in Older People Hospitalized for an Acute Episode. Nutrients 2019, 11, 2946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berger, M.M.; Pantet, O.; Schneider, A.; Ben-Hamouda, N. Clinical Medicine Micronutrient Deficiencies in Medical and Surgical Inpatients. J. Clin. Med. 2019, 8, 931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blaauw, R.; Osland, E.; Sriram, K.; Ali, A.; Allard, J.P.; Ball, P.; Chan, L.N.; Jurewitsch, B.; Logan Coughlin, K.; Manzanares, W.; et al. Parenteral Provision of Micronutrients to Adult Patients: An Expert Consensus Paper. J. Parenter. Enter. Nutr. 2019, 43, S5–S23. [Google Scholar] [CrossRef] [Green Version]
- Gomes, F.; Schuetz, P.; Bounoure, L.; Austin, P.; Ballesteros-Pomar, M.; Cederholm, T.; Fletcher, J.; Laviano, A.; Norman, K.; Poulia, K.-A.; et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clin. Nutr. 2017, 37, 336–353. [Google Scholar] [CrossRef] [Green Version]
- Graeb, F.; Wolke, R. Malnutrition and Inadequate Eating Behaviour during Hospital Stay in Geriatrics—An Explorative Analyses of NutritionDay Data in Two Hospitals. Nurs. Rep. 2021, 11, 929–941. [Google Scholar] [CrossRef]
- Curtis, L.J.; Valaitis, R.; Laur, C.; McNicholl, T.; Nasser, R.; Keller, H. Low food intake in hospital: Patient, institutional, and clinical factors. Appl. Physiol. Nutr. Metab. 2018, 43, 1239–1246. [Google Scholar] [CrossRef]
- Osman, N.S.; Nor, N.M.; Sharif, M.S.M.; Hamid, S.B.A.; Rahamat, S. Hospital food service strategies to improve food intakes among inpatients: A systematic review. Nutrients 2021, 13, 3649. [Google Scholar] [CrossRef]
- Dijxhoorn, D.N.; IJmker-Hemink, V.E.; Wanten, G.J.A.; van den Berg, M.G.A. Strategies to increase protein intake at mealtimes through a novel high-frequency food service in hospitalized patients. Eur. J. Clin. Nutr. 2018, 73, 910–916. [Google Scholar] [CrossRef]
- Nieuwenhuizen, W.F.; Weenen, H.; Rigby, P.; Hetherington, M.M. Older adults and patients in need of nutritional support: Review of current treatment options and factors influencing nutritional intake. Clin. Nutr. 2010, 29, 160–169. [Google Scholar] [CrossRef]
- Campbell, W.W.; Crim, M.C.; Young, V.R.; Evans, W.J. Increased energy requirements and changes in body composition with resistance training in older adults. Am. J. Clin. Nutr. 1994, 60, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.H.; Cable, N.T.; Faulkner, G.; Hillsdon, M.; Narici, M.; Van der Bij, A.K. Physical activity and older adults: A review of health benefits and the effectiveness of interventions. J. Sports Sci. 2004, 22, 703–725. [Google Scholar] [CrossRef] [PubMed]
- Goodpaster, B.H.; Park, S.W.; Harris, T.B.; Kritchevsky, S.B.; Nevitt, M.; Schwartz, A.V.; Simonsick, E.M.; Tylavsky, F.A.; Visser, M.; Newman, A.B. The loss of skeletal muscle strength, mass, and quality in older adults: The Health, Aging and Body Composition Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2006, 61, 1059–1064. [Google Scholar] [CrossRef]
- Vasiloglou, M.F.; Fletcher, J.; Poulia, K.A. Challenges and Perspectives in Nutritional Counselling and Nursing: A Narrative Review. J. Clin. Med. 2019, 8, 1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papathanail, I.; Brühlmann, J.; Vasiloglou, M.F.; Stathopoulou, T.; Exadaktylos, A.K.; Stanga, Z.; Münzer, T.; Mougiakakou, S. Evaluation of a Novel Artificial Intelligence System to Monitor and Assess Energy and Macronutrient Intake in Hospitalised Older Patients. Nutrients 2021, 13, 4539. [Google Scholar] [CrossRef]
- Sharma, V.; Sharma, V.; Khan, A.; Wassmer, D.J.; Schoenholtz, M.D.; Hontecillas, R.; Bassaganya-Riera, J.; Zand, R.; Abedi, V. Malnutrition, Health and the Role of Machine Learning in Clinical Setting. Front. Nutr. 2020, 7, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raphaeli, O.; Singer, P. Towards personalized nutritional treatment for malnutrition using machine learning-based screening tools. Clin. Nutr. 2021, 40, 5249–5251. [Google Scholar] [CrossRef]
- Thibault, R.; Abbasoglu, O.; Ioannou, E.; Meija, L.; Ottens-Oussoren, K.; Pichard, C.; Rothenberg, E.; Rubin, D.; Siljamäki-Ojansuu, U.; Vaillant, M.F.; et al. ESPEN guideline on hospital nutrition. Clin. Nutr. 2021, 40, 5684–5709. [Google Scholar] [CrossRef]
- Mills, S.R.; Wilcox, C.R.; Ibrahim, K.; Roberts, H.C. Can fortified foods and snacks increase the energy and protein intake of hospitalised older patients? A systematic review. J. Hum. Nutr. Diet. 2018, 31, 379–389. [Google Scholar] [CrossRef] [Green Version]
- Morilla-Herrera, J.C.; Martín-Santos, F.J.; Caro-Bautista, J.; Saucedo-Figueredo, C.; García-Mayor, S.; Morales-Asencio, J.M. Effectiveness of food-based fortification in older people a systematic review and meta-analysis. J. Nutr. Health Aging 2015, 20, 178–184. [Google Scholar] [CrossRef]
- Malafarina, V.; Serra Rexach, J.A.; Masanés, F.; Cervera-Díaz, M.C.; Lample Lacasa, L.; Ollero Ortigas, A.; Cruz-Jentoft, A.J. Results of High-Protein, High-Calorie Oral Nutritional Supplementation in Malnourished Older People in Nursing Homes: An Observational, Multicenter, Prospective, Pragmatic Study (PROT-e-GER). J. Am. Med. Dir. Assoc. 2021, 22, 1919–1926.e5. [Google Scholar] [CrossRef] [PubMed]
- Kozeniecki, M.; Fritzshall, R. Enteral Nutrition for Adults in the Hospital Setting. Nutr. Clin. Pract. 2015, 30, 634–651. [Google Scholar] [CrossRef] [PubMed]
- Heighes, P.T.; Doig, G.S.; Simpson, F. Timing and Indications for Enteral Nutrition in the Critically III. In Nutrition Support for the Critically III, 1st ed.; Seres, D.S., Van Way, C.W., III, Eds.; Humana Press: Cham, Switzerland, 2016; pp. 55–62. [Google Scholar]
- McClave, S.A.; Dibaise, J.K.; Mullin, G.E.; Martindale, R.G. ACG clinical guideline: Nutrition therapy in the adult hospitalized patient. Am. J. Gastroenterol. 2016, 111, 315–334. [Google Scholar] [CrossRef] [PubMed]
- de Aguilar-Nascimento, J.E.; Bicudo-Salomao, A.; Portari-Filho, P.E. Optimal timing for the initiation of enteral and parenteral nutrition in critical medical and surgical conditions. Nutrition 2012, 28, 840–843. [Google Scholar] [CrossRef] [PubMed]
- Guenter, P.; Blackmer, A.; Malone, A.; Mirtallo, J.M.; Phillips, W.; Tyler, R.; Barrocas, A.; Resnick, H.E.; Anthony, P.; Abdelhadi, R. Update on use of enteral and parenteral nutrition in hospitalized patients with a diagnosis of malnutrition in the United States. Nutr. Clin. Pract. 2022, 37, 94–101. [Google Scholar] [CrossRef]
- Ying, I. Artificial nutrition and hydration in advanced dementia. Can. Fam. Physician 2015, 61, 245. [Google Scholar]
- McClave, S.A.; Martindale, R.G.; Vanek, V.W.; McCarthy, M.; Roberts, P.; Taylor, B.; Ochoa, J.B.; Napolitano, L.; Cresci, G. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient. J. Parenter. Enter. Nutr. 2009, 33, 277–316. [Google Scholar] [CrossRef]
- Pivi, G.A.K.; Bertolucci, P.H.F.; Schultz, R.R. Nutrition in severe dementia. Curr. Gerontol. Geriatr. Res. 2012, 2012, 983056. [Google Scholar] [CrossRef]
- Gomes, F.; Baumgartner, A.; Bounoure, L.; Bally, M.; Deutz, N.E.; Greenwald, J.L.; Stanga, Z.; Mueller, B.; Schuetz, P. Association of Nutritional Support With Clinical Outcomes Among Medical Inpatients Who Are Malnourished or at Nutritional Risk: An Updated Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e1915138. [Google Scholar] [CrossRef] [Green Version]
- Pratt, K.J.; Hernandez, B.; Blancato, R.; Blankenship, J.; Mitchell, K. Impact of an interdisciplinary malnutrition quality improvement project at a large metropolitan hospital. BMJ Open Qual. 2020, 9, e000735. [Google Scholar] [CrossRef] [Green Version]
- Bellanti, F.; Lo Buglio, A.; Di Stasio, E.; di Bello, G.; Tamborra, R.; Dobrakowski, M.; Kasperczyk, A.; Kasperczyk, S.; Vendemiale, G. An open-label, single-center pilot study to test the effects of an amino acid mixture in older patients admitted to internal medicine wards. Nutrition 2020, 69, 110588. [Google Scholar] [CrossRef] [PubMed]
- Kaegi-Braun, N.; Faessli, M.; Kilchoer, F.; Dragusha, S.; Tribolet, P.; Gomes, F.; Bretscher, C.; Germann, S.; Deutz, N.E.; Stanga, Z.; et al. Nutritional trials using high protein strategies and long duration of support show strongest clinical effects on mortality.: Results of an updated systematic review and meta-analysis. Clin. Nutr. ESPEN 2021, 45, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Munk, T.; Svendsen, J.A.; Knudsen, A.W.; Østergaard, T.B.; Thomsen, T.; Olesen, S.S.; Rasmussen, H.H.; Beck, A.M. A multimodal nutritional intervention after discharge improves quality of life and physical function in older patients—A randomized controlled trial. Clin. Nutr. 2021, 40, 5500–5510. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Kang, J.E.; Park, S.H.; Jin, H.K.; Jang, S.M.; Kim, S.A.; Rhie, S.J. Nutrition and Clinical Outcomes of Nutrition Support in Multidisciplinary Team for Critically Ill Patients. Nutr. Clin. Pract. 2018, 33, 633–639. [Google Scholar] [CrossRef]
- Lærum-Onsager, E.; Molin, M.; Olsen, C.F.; Bye, A.; Debesay, J.; Hestevik, C.H.; Bjerk, M.; Pripp, A.H. Effect of nutritional and physical exercise intervention on hospital readmission for patients aged 65 or older: A systematic review and meta-analysis of randomized controlled trials. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 62. [Google Scholar] [CrossRef]


| 1. Patients Classified as “at Risk” with Any Validated Risk Screening Tool | |
|---|---|
| 2a Either: | 2b Or: |
| BMI <18.5 kg/m2 | Unintentional weight loss >10% indefinite of time, or >5% over the last 3 months, |
combined with either
| |
| Presence of at Least Two of the Following | ||||
|---|---|---|---|---|
| Moderate | Severe | |||
| Insufficient energy intake | <75% of estimated energy requirements for >7 days | ≤50% of estimated energy requirements for ≥5 days | ||
| Weight loss (from baseline) | % | Time | % | Time |
| 1–2 5 7.5 | 1 week 1 month 3 months | >2 >5 >7.5 | 1 week 1 month 3 months | |
| Loss of muscle mass | Mild | Moderate | ||
| Loss of subcutaneous fat | Mild | Moderate | ||
| Fluid retention | Mild | Moderate to Severe | ||
| Handgrip strength | No reduction | Reduced | ||
| Two-Step Approach | |
|---|---|
| First step: identify at-risk patients using any validated screening tool | |
| Second step: at least one Phenotypic and one Etiologic criterion are necessary to diagnosis. | |
| Phenotypic Criteria: | Etiologic Criteria: |
|
|
| |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellanti, F.; lo Buglio, A.; Quiete, S.; Vendemiale, G. Malnutrition in Hospitalized Old Patients: Screening and Diagnosis, Clinical Outcomes, and Management. Nutrients 2022, 14, 910. https://0-doi-org.brum.beds.ac.uk/10.3390/nu14040910
Bellanti F, lo Buglio A, Quiete S, Vendemiale G. Malnutrition in Hospitalized Old Patients: Screening and Diagnosis, Clinical Outcomes, and Management. Nutrients. 2022; 14(4):910. https://0-doi-org.brum.beds.ac.uk/10.3390/nu14040910
Chicago/Turabian StyleBellanti, Francesco, Aurelio lo Buglio, Stefano Quiete, and Gianluigi Vendemiale. 2022. "Malnutrition in Hospitalized Old Patients: Screening and Diagnosis, Clinical Outcomes, and Management" Nutrients 14, no. 4: 910. https://0-doi-org.brum.beds.ac.uk/10.3390/nu14040910