Recent Developments in Blood-Compatible Superhydrophobic Surfaces
Abstract
:1. Background
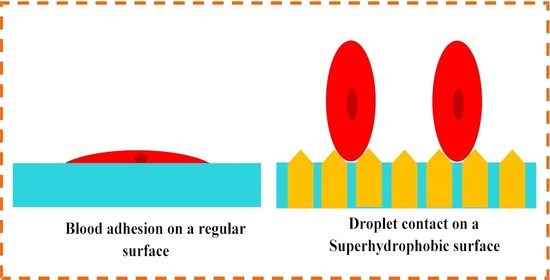
2. Characterization of Superhydrophobicity
3. Biomedical Applications of Superhydrophobicity
4. Materials for Superhydrophobicity
4.1. Substrates and Base Materials
4.2. Coating and Layered Materials

5. Methods
5.1. Testing and Characterizations
5.2. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alexander, P.; Visagan, S.; Issa, R.; Gorantla, V.R.; Thomas, S.E. Current Trends in the Duration of Anticoagulant Therapy for Venous Thromboembolism: A Systematic Review. Cureus 2021, 13, e18992. [Google Scholar] [CrossRef] [PubMed]
- Ashorobi, D.; Ameer, M.A.; Fernandez, R. Thrombosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Konarik, M.; Netuka, I.; Ivak, P.; Riha, H.; Tucanova, Z.; Wohlfahrt, P.; Maly, J.; Szarszoi, O. Association of thrombophilia prospective detection with hemocompatibility related outcomes in left ventricular assist device patients. Int. J. Artif. Organs 2021, 44, 838–845. [Google Scholar] [CrossRef] [PubMed]
- Tatsuoka, J.; Igarashi, T.; Kajimoto, R.; Kobayashi, M.; Moro, N.; Suma, T.; Oshima, H.; Yoshino, A. High-dose-infliximab-associated Cerebral Venous Sinus Thrombosis: A Case Report and Review of the Literature. Intern. Med. 2021, 60, 2677–2681. [Google Scholar] [CrossRef] [PubMed]
- Montgomerie, Z.; Popat, K.C. Improved hemocompatibility and reduced bacterial adhesion on superhydrophobic titania nanoflower surfaces. Mater. Sci. Eng. C 2020, 119, 111503. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Neuberger, T.; Manning, K.B. In vitro real-time magnetic resonance imaging for quantification of thrombosis. Magn. Reson. Mater. Phys. Biol. Med. 2020, 34, 285–295. [Google Scholar] [CrossRef]
- Panahi, L.; Udeani, G.; Horseman, M.; Weston, J.; Samuel, N.; Joseph, M.; Mora, A.; Bazan, D.; Patel, P. Anticoagulants in the Management of Pulmonary Embolism. In Pulmonary Embolism; IntechOpen: London, UK, 2021. [Google Scholar] [CrossRef]
- Chu, T.L.; Tripathi, G.; Bae, S.H.; Lee, B.-T. In-vitro and in-vivo hemostat evaluation of decellularized liver extra cellular matrix loaded chitosan/gelatin spongy scaffolds for liver injury. Int. J. Biol. Macromol. 2021, 193, 638–646. [Google Scholar] [CrossRef]
- Butler, A.; Tait, R. Management of oral anticoagulant-induced intracranial haemorrhage. Blood Rev. 1998, 12, 35–44. [Google Scholar] [CrossRef]
- Onundarson, P.T.; Palsson, R.; Witt, D.M.; Gudmundsdottir, B.R. Replacement of traditional prothrombin time monitoring with the new Fiix prothrombin time increases the efficacy of warfarin without increasing bleeding. A review article. Thromb. J. 2021, 19, 72. [Google Scholar] [CrossRef]
- Wang, S.; Liu, K.; Yao, X.; Jiang, L. Bioinspired Surfaces with Superwettability: New Insight on Theory, Design, and Applications. Chem. Rev. 2015, 115, 8230–8293. [Google Scholar] [CrossRef]
- Khanmohammadi Chenab, K.; Sohrabi, B.; Rahmanzadeh, A. Superhydrophobicity: Advanced biological and biomedical applications. Biomater. Sci. 2019, 7, 3110–3137. [Google Scholar] [CrossRef]
- Jeevahan, J.; Chandrasekaran, M.; Joseph, G.B.; Raj, R.B.D.; Mageshwaran, G. Superhydrophobic surfaces: A review on fundamentals, applications, and challenges. J. Coat. Technol. Res. 2018, 15, 231–250. [Google Scholar] [CrossRef]
- Parvate, S.; Dixit, P.; Chattopadhyay, S. Superhydrophobic Surfaces: Insights from Theory and Experiment. J. Phys. Chem. B 2020, 124, 1323–1360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verplanck, N.; Coffinier, Y.; Thomy, V.; Boukherroub, R. Wettability Switching Techniques on Superhydrophobic Surfaces. Nanoscale Res. Lett. 2007, 2, 577–596. [Google Scholar] [CrossRef] [Green Version]
- Marmur, A. Wetting on Hydrophobic Rough Surfaces: To Be Heterogeneous or Not To Be? Langmuir 2003, 19, 8343–8348. [Google Scholar] [CrossRef]
- Deeksha, P.; Kavitha Sri, A.; Nishanthini, K.; Hikku, G.S.; Antinate Shilpa, S.; Jeyasubramanian, K.; Murugesan, R. Super-hydrophobicity: Mechanism, fabrication and its application in medical implants to prevent biomaterial associated infections. J. Ind. Eng. Chem. 2020, 92, 1–17. [Google Scholar] [CrossRef]
- Gao, L.; McCarthy, T.J. Contact Angle Hysteresis Explained. Langmuir 2006, 22, 6234–6237. [Google Scholar] [CrossRef]
- Falde, E.J.; Yohe, S.T.; Colson, Y.L.; Grinstaff, M.W. Superhydrophobic materials for biomedical applications. Biomaterials 2016, 104, 87–103. [Google Scholar] [CrossRef] [Green Version]
- Lv, J.; Gong, Z.; He, Z.; Yang, J.; Chen, Y.; Tang, C.; Liu, Y.; Fan, M.; Lau, W.-M. 3D printing of a mechanically durable superhydrophobic porous membrane for oil–water separation. J. Mater. Chem. A 2017, 5, 12435–12444. [Google Scholar] [CrossRef]
- Zhao, Y.; Tang, Y.; Wang, X.; Lin, T. Superhydrophobic cotton fabric fabricated by electrostatic assembly of silica nanoparticles and its remarkable buoyancy. Appl. Surf. Sci. 2010, 256, 6736–6742. [Google Scholar] [CrossRef]
- Lu, C.; Xie, Y.; Yang, Y.; Cheng, M.M.C.; Koh, C.-G.; Bai, Y.; Lee, L.J. New Valve and Bonding Designs for Microfluidic Biochips Containing Proteins. Anal. Chem. 2006, 79, 994–1001. [Google Scholar] [CrossRef] [PubMed]
- Van Buren, T.; Smits, A.J. Substantial drag reduction in turbulent flow using liquid-infused surfaces. J. Fluid Mech. 2017, 827, 448–456. [Google Scholar] [CrossRef] [Green Version]
- Hedayati, M.; Neufeldb, M.J.; Reynoldscde, M.M.; Kipper, M.J. The quest for blood-compatible materials: Recent advances and future technologies. Mater. Sci. Eng. R Rep. 2019, 138, 118–152. [Google Scholar] [CrossRef]
- Vilaseca, P.; Dawson, K.A.; Franzese, G. Understanding and modulating the competitive surface-adsorption of proteins through coarse-grained molecular dynamics simulations. Soft Matter 2013, 9, 6978–6985. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Yang, R.; Yu, M.; Bai, F.; Li, C.; Wang, Z.L. Cellular Level Biocompatibility and Biosafety of ZnO Nanowires. J. Phys. Chem. C 2008, 112, 20114–20117. [Google Scholar] [CrossRef] [Green Version]
- De Mel, A.; Cousins, B.G.; Seifalian, A. Surface Modification of Biomaterials: A Quest for Blood Compatibility. Int. J. Biomater. 2012, 2012, 707863. [Google Scholar] [CrossRef] [PubMed]
- Tu, Q.; Shen, X.; Liu, Y.; Zhang, Q.; Zhao, X.; Maitz, M.F.; Liu, T.; Qiu, H.; Wang, J.; Huang, N.; et al. A facile metal–phenolic–amine strategy for dual-functionalization of blood-contacting devices with antibacterial and anticoagulant properties. Mater. Chem. Front. 2018, 3, 265–275. [Google Scholar] [CrossRef]
- Bender, M.; Plachetka, U.; Ran, J.; Fuchs, A.; Vratzov, B.; Kurz, H. High resolution lithography with PDMS molds. J. Vac. Sci. Technol. B 2004, 22, 3229–3232. [Google Scholar] [CrossRef]
- Nathanael, A.J.; Oh, T.H. Biopolymer Coatings for Biomedical Applications. Polymers 2020, 12, 3061. [Google Scholar] [CrossRef]
- Halldorsson, S.; Lucumi, E.; Gómez-Sjöberg, R.; Fleming, R.M. Advantages and Challenges of Microfluidic Cell Culture in Polydimethylsiloxane Devices. Biosens. Bioelectron. 2015, 63, 218–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qin, D.; Xia, Y.; Whitesides, G.M. Soft lithography for micro- and nanoscale patterning. Nat. Protoc. 2010, 5, 491–502. [Google Scholar] [CrossRef] [Green Version]
- Eduok, U.; Faye, O.; Szpunar, J. Recent developments and applications of protective silicone coatings: A review of PDMS functional materials. Prog. Org. Coat. 2017, 111, 124–163. [Google Scholar] [CrossRef]
- Seethapathy, S.; Górecki, T. Applications of polydimethylsiloxane in analytical chemistry: A review. Anal. Chim. Acta 2012, 750, 48–62. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, Y.; Zhang, D.; Li, L.; Wang, T.; Duan, S. Preparation of superhydrophobic flexible tubes with water and blood repellency based on template method. Colloids Surf. A Physicochem. Eng. Asp. 2019, 587, 124331. [Google Scholar] [CrossRef]
- Kim, S.; Cho, H.; Hwang, W. Simple fabrication method of flexible and translucent high-aspect ratio superhydrophobic polymer tube using a repeatable replication and nondestructive detachment process. Chem. Eng. J. 2018, 361, 975–981. [Google Scholar] [CrossRef]
- Brancato, L.; Decrop, D.; Lammertyn, J.; Puers, R. Surface Nanostructuring of Parylene-C Coatings for Blood Contacting Implants. Materials 2018, 11, 1109. [Google Scholar] [CrossRef] [Green Version]
- Hoshian, S.; Kankuri, E.; Ras, R.H.A.; Franssila, S.; Jokinen, V. Water and Blood Repellent Flexible Tubes. Sci. Rep. 2017, 7, 16019. [Google Scholar] [CrossRef] [Green Version]
- Iqbal, R.; Majhy, B.; Sen, A.K. Facile Fabrication and Characterization of a PDMS-Derived Candle Soot Coated Stable Biocompatible Superhydrophobic and Superhemophobic Surface. ACS Appl. Mater. Interfaces 2017, 9, 31170–31180. [Google Scholar] [CrossRef]
- Da Câmara, P.C.F.; Madruga, L.Y.C.; Sabino, R.M.; Vlcek, J.; Balaban, R.C.; Popat, K.C.; Martins, A.F.; Kipper, M.J. Polyelectrolyte multilayers containing a tannin derivative polyphenol improve blood compatibility through interactions with platelets and serum proteins. Mater. Sci. Eng. C 2020, 112, 110919. [Google Scholar] [CrossRef]
- Kang, Z.; Zhang, J.; Niu, L. A one-step hydrothermal process to fabricate superhydrophobic hydroxyapatite coatings and determination of their properties. Surf. Coat. Technol. 2018, 334, 84–89. [Google Scholar] [CrossRef]
- Xie, J.; Hu, J.; Fang, L.; Liao, X.; Du, R.; Wu, F.; Wu, L. Facile fabrication and biological properties of super-hydrophobic coating on magnesium alloy used as potential implant materials. Surf. Coat. Technol. 2019, 384, 125223. [Google Scholar] [CrossRef]
- Sabino, R.M.; Kauk, K.; Movafaghi, S.; Kota, A.; Popat, K.C. Interaction of blood plasma proteins with superhemophobic titania nanotube surfaces. Nanomed. Nanotechnol. Biol. Med. 2019, 21, 102046. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.G.S.; Bertolini, M.M.; Costa, R.C.; Cordeiro, J.M.; Nagay, B.E.; De Almeida, A.B.; Retamal-Valdes, B.; Nociti, F.H.; Feres, M.; Rangel, E.C.; et al. Targeting Pathogenic Biofilms: Newly Developed Superhydrophobic Coating Favors a Host-Compatible Microbial Profile on the Titanium Surface. ACS Appl. Mater. Interfaces 2020, 12, 10118–10129. [Google Scholar] [CrossRef]
- Antonowicz, M.; Kurpanik, R.; Walke, W.; Basiaga, M.; Sondor, J.; Paszenda, Z. Selected Physicochemical Properties of Diamond Like Carbon (DLC) Coating on Ti-13Nb-13Zr Alloy Used for Blood Contacting Implants. Materials 2020, 13, 5077. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Lai, Y.; Zhang, Q.; Wu, K.; Zhang, L.; Lin, C.; Tang, P. A novel electrochemical strategy for improving blood compatibility of titanium-based biomaterials. Colloids Surf. B Biointerfaces 2010, 79, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Feng, H.; Ye, X.; Lu, L.; Xu, S.; Yang, X.; Fan, Z.; Yang, C.; Zhu, J. Preparation of Microstructured Surface of Pyrolytic Carbon by Laser and Its Blood Compatibility Application. J. Laser Micro Nanoeng. 2021, 16, 53–61. [Google Scholar]
- Ozkan, E.; Mondal, A.; Singha, P.; Douglass, M.; Hopkins, S.P.; Devine, R.; Garren, M.; Manuel, J.; Warnock, J.; Handa, H. Fabrication of Bacteria- and Blood-Repellent Superhydrophobic Polyurethane Sponge Materials. ACS Appl. Mater. Interfaces 2020, 12, 51160–51173. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.-R.; Lin, C.-W.; Chou, C.-M.; Chung, C.-J.; He, J.-L. Surface modification of blood-contacting biomaterials by plasma-polymerized superhydrophobic films using hexamethyldisiloxane and tetrafluoromethane as precursors. Appl. Surf. Sci. 2015, 346, 50–56. [Google Scholar] [CrossRef]
- Seyfi, J.; Goodarzi, V.; Wurm, F.R.; Shojaei, S.; Jafari-Nodoushan, M.; Najmoddin, N.; Khonakdar, H.A.; Baghersad, M.H.; Uzun, L. Developing antibacterial superhydrophobic coatings based on polydimethylsiloxane/silver phosphate nanocomposites: Assessment of surface morphology, roughness and chemistry. Prog. Org. Coat. 2020, 149, 105944. [Google Scholar] [CrossRef]
- Manabe, K.; Nara, H. Construction of stable biological albumin/heparin multilayers for elastic coatings on hydrophobic antithrombogenic artificial blood vessels. Tribol. Int. 2020, 156, 106843. [Google Scholar] [CrossRef]
- Vijayan, V.M.; Tucker, B.S.; Baker, P.A.; Vohra, Y.K.; Thomas, V. Non-equilibrium hybrid organic plasma processing for superhydrophobic PTFE surface towards potential bio-interface applications. Colloids Surf. B Biointerfaces 2019, 183, 110463. [Google Scholar] [CrossRef]
- PJ, J.F.; Arun, K.J.; Navas, A.A.; Joseph, I. Biomedical applications of polymers—An overview. Macromolecules 2018, 28, 939–944. [Google Scholar]
- Santos, G. The importance of metallic materials as biomaterials. Adv. Tissue Eng. Regen. Med. Open Access 2017, 3, 300–302. [Google Scholar] [CrossRef] [Green Version]
- Logeeswaran, V.; Chan, M.-L.; Bayam, Y.; Islam, M.S.; Horsley, D.; Li, X.; Wu, W.; Wang, S.-Y.; Williams, R. Ultra-smooth metal surfaces generated by pressure-induced surface deformation of thin metal films. Appl. Phys. A 2007, 87, 187–192. [Google Scholar] [CrossRef]
- Singh, A.; Singh, S. ZnO nanowire-coated hydrophobic surfaces for various biomedical applications. Bull. Mater. Sci. 2018, 41, 94. [Google Scholar] [CrossRef] [Green Version]
- Park, S.; Jung, S.; Heo, J.; Hong, J. Facile synthesis of polysilsesquioxane toward durable superhydrophilic/superhydrophobic coatings for medical devices. J. Ind. Eng. Chem. 2019, 77, 97–104. [Google Scholar] [CrossRef]
- Shaban, M.; Mohamed, F.; Abdallah, S. Production and Characterization of Superhydrophobic and Antibacterial Coated Fabrics Utilizing ZnO Nanocatalyst. Sci. Rep. 2018, 8, 3925. [Google Scholar] [CrossRef]
- Mendoza, A.I.; Moriana, R.; Hillborg, H.; Strömberg, E. Super-hydrophobic zinc oxide/silicone rubber nanocomposite surfaces. Surf. Interfaces 2019, 14, 146–157. [Google Scholar] [CrossRef]
- Wu, J.; Chen, J.; Xia, J.; Lei, W.; Wang, B.-P. A Brief Review on Bioinspired ZnO Superhydrophobic Surfaces: Theory, Synthesis, and Applications. Adv. Mater. Sci. Eng. 2013, 2013, 232681. [Google Scholar] [CrossRef] [Green Version]
- Boticas, I.; Dias, D.; Ferreira, D.; Magalhães, P.; Silva, R.; Fangueiro, R. Superhydrophobic cotton fabrics based on ZnO nanoparticles functionalization. SN Appl. Sci. 2019, 1, 1376. [Google Scholar] [CrossRef] [Green Version]
- Fischer, A. Dietary supplements as additional sources of zinc in the human organism. Farmacia 2021, 69, 325–331. [Google Scholar] [CrossRef]
- Sirelkhatim, A.; Mahmud, S.; Seeni, A.; Kaus, N.H.M.; Ann, L.C.; Bakhori, S.K.M.; Hasan, H.; Mohamad, D. Review on Zinc Oxide Nanoparticles: Antibacterial Activity and Toxicity Mechanism. Nano-Micro Lett. 2015, 7, 219–242. [Google Scholar] [CrossRef] [Green Version]
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Fedora, G.; Paola, T. Titanium Dioxide Nanoparticles: A Risk for Human Health? Mini-Rev. Med. Chem. 2016, 16, 762–769. [Google Scholar]
- Peng, S.; Meng, W.; Guo, J.; Wang, B.; Wang, Z.; Xu, N.; Li, X.; Wang, J.; Xu, J. Photocatalytically Stable Superhydrophobic and Translucent Coatings Generated from PDMS-Grafted-SiO2/TiO2@PDMS with Multiple Applications. Langmuir 2019, 35, 2760–2771. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, Z.; Gurney, R.S.; Liu, D. Superhydrophobic and photocatalytic PDMS/TiO2 coatings with environmental stability and multifunctionality. Colloids Surf. A Physicochem. Eng. Asp. 2019, 561, 101–108. [Google Scholar] [CrossRef]
- Li, C.; Cao, Z.; Xie, C.; Li, Z.; Fang, X.; Ou, J.; Xue, M.; Wang, F.; Lei, S.; Li, W. Facile preparation of TiO2/acrylic resin superhydrophobic surface with excellent wear resistance. J. Appl. Polym. Sci. 2019, 136, 47762. [Google Scholar] [CrossRef]
- Smith, B.S.; Yoriya, S.; Grissom, L.; Grimes, C.A.; Popat, K.C. Hemocompatibility of titania nanotube arrays. J. Biomed. Mater. Res.Part A 2010, 95A, 350–360. [Google Scholar] [CrossRef]
- Jiang, J.; Xu, J.; Liu, Z.; Deng, L.; Sun, B.; Liu, S.; Wang, L.; Liu, H. Preparation, corrosion resistance and hemocompatibility of the superhydrophobic TiO2 coatings on biomedical Ti-6Al-4V alloys. Appl. Surf. Sci. 2015, 347, 591–595. [Google Scholar] [CrossRef]
- Lazauskas, A.; Jucius, D.; Puodžiukynas, L.; Guobienė, A.; Grigaliūnas, V. SiO2-Based Nanostructured Superhydrophobic Film with High Optical Transmittance. Coatings 2020, 10, 934. [Google Scholar] [CrossRef]
- Xue, C.-H.; Tian, Q.-Q.; Jia, S.-T.; Zhao, L.-L.; Ding, Y.-R.; Li, H.-G.; An, Q.-F. The fabrication of mechanically durable and stretchable superhydrophobic PDMS/SiO2 composite film. RSC Adv. 2020, 10, 19466–19473. [Google Scholar] [CrossRef]
- Guo, J.; Wang, C.; Yu, H.; Li, X. Preparation of a wear-resistant, superhydrophobic SiO2/silicone-modified polyurethane composite coating through a two-step spraying method. Prog. Org. Coat. 2020, 146, 105710. [Google Scholar] [CrossRef]
- Zhang, J.; Li, G.; Li, D.; Zhang, X.; Li, Q.; Liu, Z.; Fang, Y.; Zhang, S.; Man, J. In Vivo Blood-Repellent Performance of a Controllable Facile-Generated Superhydrophobic Surface. ACS Appl. Mater. Interfaces 2021, 13, 29021–29033. [Google Scholar] [CrossRef]
- Li, Z.; Nguyen, B.L.; Cheng, Y.C.; Xue, J.; MacLaren, G.; Yap, C.H. Durable, flexible, superhydrophobic and blood-repelling surfaces for use in medical blood pumps. J. Mater. Chem. B 2018, 6, 6225–6233. [Google Scholar] [CrossRef]
- Shadanbaz, S.; Dias, G.J. Calcium phosphate coatings on magnesium alloys for biomedical applications: A review. Acta Biomater. 2012, 8, 20–30. [Google Scholar] [CrossRef]
- Esmeryan, K.D.; Castano, C.E.; Chaushev, T.A.; Mohammadi, R.; Vladkova, T.G. Silver-doped superhydrophobic carbon soot coatings with enhanced wear resistance and anti-microbial performance. Colloids Surf. A Physicochem. Eng. Asp. 2019, 582, 123880. [Google Scholar] [CrossRef]
- Wu, A.; Tian, C.; Chang, W.; Hong, Y.; Zhang, Q.; Qu, Y.; Fu, H. Morphology-controlled synthesis of Ag3PO4 nano/microcrystals and their antibacterial properties. Mater. Res. Bull. 2013, 48, 3043–3048. [Google Scholar] [CrossRef]
- Chu, K.T.; Oshida, Y.; Hancock, E.B.; Kowolik, M.J.; Barco, T.; Zunt, S.L. Hydroxyapatite/PMMA composites as bone cements. Bio-Med. Mater. Eng. 2004, 14, 87–105. [Google Scholar]
- Frazer, R.Q.; Byron, R.T.; Osborne, P.B.; West, K.P. PMMA: An Essential Material in Medicine and Dentistry. J. Long-Term Eff. Med. Implant. 2005, 15, 629–639. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.J.; Choi, B.; Kim, K.S.; Bae, W.J.; Hong, S.H.; Lee, J.Y.; Hwang, T.K.; Kim, S.W. The Potential Role of Polymethyl Methacrylate as a New Packaging Material for the Implantable Medical Device in the Bladder. BioMed Res. Int. 2015, 2015, 852456. [Google Scholar] [CrossRef]
- Thielen, T.; Maas, S.; Zuerbes, A.; Waldmann, D.; Kelm, J. Mechanical Material Properties of Polymethylmethacrylate (PMMA) for Medical Applications. Mater. Test. 2009, 51, 203–209. [Google Scholar] [CrossRef]
- Huh, J.; Joo, M.-K.; Jang, D.; Lee, J.-H.; Kim, G.T. Reduced charge fluctuations in individual SnO2 nanowires by suppressed surface reactions. J. Mater. Chem. 2012, 22, 24012–24016. [Google Scholar] [CrossRef]
- Liu, J.; Ye, L.; Sun, Y.; Hu, M.; Chen, F.; Wegner, S.; Mailänder, V.; Steffen, W.; Kappl, M.; Butt, H. Elastic Superhydrophobic and Photocatalytic Active Films Used as Blood Repellent Dressing. Adv. Mater. 2020, 32, e1908008. [Google Scholar] [CrossRef]
- Shi, Y.; Jiang, Z.; Cao, J.; Ehmann, K.F. Texturing of metallic surfaces for superhydrophobicity by water jet guided laser micro-machining. Appl. Surf. Sci. 2020, 500, 144286. [Google Scholar] [CrossRef]
- Zhang, G.; Wang, D.; Gu, A.Z.-Z.; Möhwald†, H. Fabrication of Superhydrophobic Surfaces from Binary Colloidal Assembly. Langmuir 2005, 21, 9143–9148. [Google Scholar] [CrossRef]
- Yang, Y.; He, H.; Li, Y.; Qiu, J. Using Nanoimprint Lithography to Create Robust, Buoyant, Superhydrophobic PVB/SiO2 Coatings on wood Surfaces Inspired by Red roses petal. Sci. Rep. 2019, 9, 9961. [Google Scholar] [CrossRef]
- Pozzato, A.; Zilio, S.D.; Fois, G.; Vendramin, D.; Mistura, G.; Belotti, M.; Chen, Y.; Natali, M. Superhydrophobic surfaces fabricated by nanoimprint lithography. Microelectron. Eng. 2006, 83, 884–888. [Google Scholar] [CrossRef]
- Hardman, S.J.; Muhamad-Sarih, N.; Riggs, H.J.; Thompson, R.; Rigby, J.; Bergius, W.; Hutchings, L. Electrospinning Superhydrophobic Fibers Using Surface Segregating End-Functionalized Polymer Additives. Macromolecules 2011, 44, 6461–6470. [Google Scholar] [CrossRef] [Green Version]
- Jiang, S.; Meng, X.; Chen, B.; Wang, N.; Chen, G. Electrospinning superhydrophobic–superoleophilic PVDF-SiO2 nanofibers membrane for oil–water separation. J. Appl. Polymer Sci. 2020, 137, 49546. [Google Scholar] [CrossRef]
- Zhou, M.; Yang, J.H.; Ye, X.; Zheng, A.R.; Li, G.; Yang, P.F.; Zhu, Y.; Cai, L. Blood Platelet’s Behavior on Nanostructured Superhydrophobic Surface. J. Nano Res. 2008, 2, 129–136. [Google Scholar] [CrossRef] [Green Version]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Z.; Paul, S.; Stein, L.H.; Salemi, A.; Mitra, S. Recent Developments in Blood-Compatible Superhydrophobic Surfaces. Polymers 2022, 14, 1075. https://0-doi-org.brum.beds.ac.uk/10.3390/polym14061075
Wang Z, Paul S, Stein LH, Salemi A, Mitra S. Recent Developments in Blood-Compatible Superhydrophobic Surfaces. Polymers. 2022; 14(6):1075. https://0-doi-org.brum.beds.ac.uk/10.3390/polym14061075
Chicago/Turabian StyleWang, Zhiqian, Sumona Paul, Louis H. Stein, Arash Salemi, and Somenath Mitra. 2022. "Recent Developments in Blood-Compatible Superhydrophobic Surfaces" Polymers 14, no. 6: 1075. https://0-doi-org.brum.beds.ac.uk/10.3390/polym14061075