A Biomechanical Study of Various Fixation Strategies for the Treatment of Clavicle Fractures Using Three-Dimensional Upper-Body Musculoskeletal Finite Element Models
Abstract
:1. Introduction
2. Materials and Methods
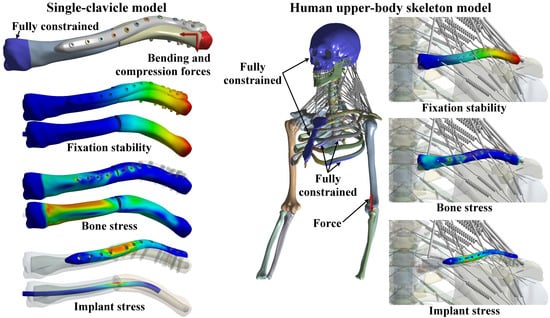
2.1. Single-Clavicle Model with Various Fixation Strategies
2.2. Human Upper-Body Skeleton Model with Various Surgical Strategies
2.3. Finite Element Analyses
2.4. Model Validation and Correlation Analyses
3. Results
3.1. Simplified Single-Clavicle Models
3.2. Complete Human Upper-Body Skeleton Models
3.3. Model Validation and Correlation Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sandstrom, C.K.; Kennedy, S.A.; Gross, J.A. Acute shoulder trauma: What the surgeon wants to know. RadioGraphics 2015, 35, 475–492. [Google Scholar] [CrossRef] [PubMed]
- Andersson, S.H.; Bahr, R.; Clarsen, B.; Myklebust, G. Preventing overuse shoulder injuries among throwing athletes: A cluster-randomised controlled trial in 660 elite handball players. Brit. J. Sport Med. 2016, 51, 1073–1080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kannus, P.; Niemi, S.; Sievänen, H.; Parkkari, J. Stabilized incidence in proximal humeral fractures of elderly women: Nationwide statistics from finland in 1970–2015. J. Gerontol. Ser. A 2017, 72, 1390–1393. [Google Scholar] [CrossRef] [Green Version]
- Gilde, A.K.; Hoffmann, M.F.; Sietsema, D.L.; Jones, C.B. Functional outcomes of operative fixation of clavicle fractures in patients with floating shoulder girdle injuries. J. Orthoped. Traumatol. 2015, 16, 221–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holder, J.; Kolla, S.; Lehto, S. Clavicle fractures: Allman and neer classification. J. Adv. Radiol. Med. Imag. 2017, 2, 102. [Google Scholar]
- Woltz, S.; Stegeman, S.A.; Krijnen, P.; van Dijkman, B.A.; van Thiel, T.P.H.; Schep, N.W.L.; de Rijcke, P.A.R.; Frolke, J.P.M.; Schipper, I.B. Plate fixation compared with nonoperative treatment for displaced midshaft clavicular fractures. J. Bone Jt. Surg. Am. 2017, 99, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Naimark, M.; Dufka, F.L.; Han, R.; Sing, D.C.; Toogood, P.; Ma, C.B.; Feeley, B.T. Plate fixation of midshaft clavicular fractures: Patient-reported outcomes and hardware-related complications. J. Shoulder Elb. Surg. 2016, 25, 739–746. [Google Scholar] [CrossRef]
- Asadollahi, S.; Hau, R.C.; Page, R.S.; Richardson, M.; Edwards, E.R. Complications associated with operative fixation of acute midshaft clavicle fractures. Injury 2016, 47, 1248. [Google Scholar] [CrossRef]
- Santolini, E.; Stella, M.; Sanguineti, F.; Felli, L.; Santolini, F. Treatment of distal clavicle nonunion with and without bone grafting. Injury 2018, 49, S34–S38. [Google Scholar] [CrossRef]
- Frima, H.; Hulsmans, M.H.J.; Houwert, R.M.; Ahmed Ali, U.; Verleisdonk, E.J.M.M.; Sommer, C.; van Heijl, M. End cap versus no end cap in intramedullary nailing for displaced midshaft clavicle fractures: Influence on implant-related irritation. Eur. J. Trauma Emerg. Surg. 2017, 44, 119–124. [Google Scholar] [CrossRef]
- Faust, K.C.; Lark, R.K.; Leversedge, F.J. Pediatric clavicle injuries. In Clavicle Injuries; Springer: Cham, Switzerland, 2018; pp. 205–214. [Google Scholar]
- Pulos, N.; Yoon, R.S.; Shetye, S.; Hast, M.W.; Liporace, F.; Donegan, D.J. Anteroinferior 2.7-mm versus 3.5-mm plating of the clavicle: A biomechanical study. Injury 2016, 47, 1642–1646. [Google Scholar] [CrossRef] [PubMed]
- Yagnik, G.P.; Brady, P.C.; Zimmerman, J.P.; Jordan, C.J.; Porter, D.A. A biomechanical comparison of new techniques for distal clavicular fracture repair versus locked plating. J. Shoulder Elb. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Van der Meijden, O.A.; Houwert, R.M.; Hulsmans, M.; Wijdicks, F.J.G.; Dijkgraaf, M.G.; Meylaerts, S.A.; Hammacher, E.R.; Verhofstad, M.H.J.; Verleisdonk, E.J.M.M. Operative treatment of dislocated midshaft clavicular fractures: Plate or intramedullary nail fixation? J. Bone Jt. Surg. Am. 2015, 97, 613–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ottomeyer, C.; Taylor, B.C.; Isaacson, M.; Martinez, L.; Ebaugh, P.; French, B.G. Midshaft clavicle fractures with associated ipsilateral acromioclavicular joint dislocations: Incidence and risk factors. Injury 2017, 48, 469–473. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Hsu, C.C.; Huang, P.Y. Biomechanical study of different fixation techniques for the treatment of sacroiliac joint injuries using finite element analyses and biomechanical tests. Comput. Biol. Med. 2017, 87, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Belli, S.; Eraslan, O.; Eskitaşcıoğlu, G. Effect of different treatment options on biomechanics of immature teeth: A finite element stress analysis study. J. Endodont. 2018, 44, 475–479. [Google Scholar] [CrossRef]
- Mirulla, A.I.; Bragonzoni, L.; Zaffagnini, S.; Bontempi, M.; Nigrelli, V.; Ingrassia, T. Virtual simulation of an osseointegrated trans-humeral prosthesis: A falling scenario. Injury 2018, 49, 784–791. [Google Scholar] [CrossRef]
- Fletcher, J.W.A.; Windolf, M.; Richards, R.G.; Gueorguiev, B.; Varga, P. Screw configuration in proximal humerus plating has a significant impact on fixation failure risk predicted by finite element models. J. Shoulder Elb. Surg. 2019, 28, 1816–1823. [Google Scholar] [CrossRef]
- Ingrassia, T.; Nalbone, L.; Nigrelli, V.; Ricotta, V.; Pisciotta, D. Biomechanical analysis of the humeral tray positioning in reverse shoulder arthroplasty design. Int. J. Interact. Des. Manuf. 2017, 12, 651–661. [Google Scholar] [CrossRef]
- Favre, P.; Kloen, P.; Helfet, D.L.; Werner, C.M.L. Superior versus anteroinferior plating of the clavicle: A finite element study. J. Orthop. Trauma 2011, 25, 661–665. [Google Scholar] [CrossRef]
- Pendergast, M.; Rusovici, R. A finite element parametric study of clavicle fixation plates. Int. J. Numer. Meth. Biomed. Eng. 2015, 31, e02710. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.L.; Chen, W.C.; Lin, K.J.; Tsai, C.L.; Lin, K.P.; Wei, H.W. Conceptual finite element study for comparison among superior, anterior, and spiral clavicle plate fixations for midshaft clavicle fracture. Med. Eng. Phys. 2016, 38, 1070–1075. [Google Scholar] [CrossRef]
- Sarrafpour, B.; Rungsiyakull, C.; Swain, M.; Li, Q.; Zoellner, H. Finite element analysis suggests functional bone strain accounts for continuous post-eruptive emergence of teeth. Arch. Oral. Biol. 2012, 57, 1070–1078. [Google Scholar] [CrossRef] [PubMed]
- Bassett, R.W.; Browne, A.O.; Morrey, B.F.; An, K.N. Glenohumeral muscle force and moment mechanics in a position of shoulder instability. J. Biomech. 1990, 23, 405–415. [Google Scholar] [CrossRef]
- Faizan, A.; Goel, V.K.; Biyani, A.; Garfin, S.R.; Bono, C.M. Adjacent level effects of bi level disc replacement, bi level fusion and disc replacement plus fusion in cervical spine- a finite element based study. Clin. Biomech. 2012, 27, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.K. Finite element modeling of multi-level cervical spinal segments (c3–c6) and biomechanical analysis of an elastomer-type prosthetic disc. Med. Eng. Phys. 2006, 28, 534–541. [Google Scholar] [CrossRef]
- Shih, K.S.; Truong, T.A.; Hsu, C.C.; Hou, S.M. Biomechanical investigation of different surgical strategies for the treatment of rib fractures using a three-dimensional human respiratory model. Biomed. Eng./Biomed. Tech. 2019, 64, 93–102. [Google Scholar] [CrossRef]
- Zeng, L.; Wei, H.; Liu, Y.; Zhang, W.; Pan, Y.; Zhang, W.; Zhang, C.; Zeng, B.; Chen, Y. Titanium elastic nail (ten) versus reconstruction plate repair of midshaft clavicular fractures: A finite element study. PLoS ONE 2015, 10, e0126131. [Google Scholar] [CrossRef]
- Ye, Y.; Hao, J.; Mauffrey, C.; Hammerberg, E.M.; Stahel, P.F.; Hak, D.J. Optimizing stability in femoral neck fracture fixation. Orthopedics 2015, 38, 625–630. [Google Scholar]
- Wehner, T.; Claes, L.; Niemeyer, F.; Nolte, D.; Simon, U. Influence of the fixation stability on the healing time—A numerical study of a patient-specific fracture healing process. Clin. Biomech. 2010, 25, 606–612. [Google Scholar] [CrossRef]
- Erdle, B.; Izadpanah, K.; Jaeger, M.; Jensen, P.; Konstantinidis, L.; Zwingmann, J.; Südkamp, N.P.; Maier, D. Comparative analysis of locking plate versus hook plate osteosynthesis of neer type iib lateral clavicle fractures. Arch. Orthop. Traum Surg. 2017, 137, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Shih, C.M.; Huang, K.C.; Chen, K.H.; Hung, L.K.; Su, K.C. Biomechanical analysis of implanted clavicle hook plates with different implant depths and materials in the acromioclavicular joint: A finite element analysis study. Artif. Organs 2016, 40, 1062–1070. [Google Scholar] [CrossRef] [PubMed]
- Ni, M.; Niu, W.; Wong, D.W.C.; Zeng, W.; Mei, J.; Zhang, M. Finite element analysis of locking plate and two types of intramedullary nails for treating mid-shaft clavicle fractures. Injury 2016, 47, 1618–1623. [Google Scholar] [CrossRef] [PubMed]
- Meeuwis, M.A.; Pull ter Gunne, A.F.; Verhofstad, M.H.J.; van der Heijden, F.H.W.M. Construct failure after open reduction and plate fixation of displaced midshaft clavicular fractures. Injury 2017, 48, 715–719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Switaj, P.J.; Fuchs, D.; Alshouli, M.; Patwardhan, A.G.; Voronov, L.I.; Muriuki, M.; Havey, R.M.; Kadakia, A.R. A biomechanical comparison study of a modern fibular nail and distal fibular locking plate in ao/ota 44c2 ankle fractures. J. Orthop. Surg. Res. 2016, 11, 100. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.N.; Chang, C.W.; Lin, C.W.; Wang, C.W.; Peng, Y.T.; Chang, C.H.; Li, C.T. Numerical investigation of fracture impaction in proximal humeral fracture fixation with locking plate and intramedullary nail. Int. Orthop. 2017, 41, 1471–1480. [Google Scholar] [CrossRef]
- Zhang, Y.K.; Wei, H.W.; Lin, K.P.; Chen, W.C.; Tsai, C.L.; Lin, K.J. Biomechanical effect of the configuration of screw hole style on locking plate fixation in proximal humerus fracture with a simulated gap: A finite element analysis. Injury 2016, 47, 1191–1195. [Google Scholar] [CrossRef]







| Materials | Young’s Modulus (MPa) | Poisson’s Ratio | Area (mm2) |
|---|---|---|---|
| Skeleton | |||
| Skull | 10,000 | 0.29 | - |
| Teeth | 18,600 | 0.31 | - |
| Clavicle (Cortical bone) | 10,000 | 0.29 | - |
| Clavicle (Cancellous bone) | 100 | 0.29 | - |
| Scapular | 16,000 | 0.3 | - |
| Rib | 4520 | 0.375 | - |
| Sternum | 9680 | 0.3 | - |
| Costal cartilages | 24.5 | 0.4 | - |
| Spine column (Cortical bone) | 10,000 | 0.25 | - |
| Spine column (Cancellous bone) | 450 | 0.25 | - |
| Spine column (Posterior elements) | 3500 | 0.3 | - |
| Spine column (Annulus fibrosus) | 4.2 | 0.45 | - |
| Spine column (Nucleus pulposus) | 1 | 0.499 | - |
| Implants | |||
| Plates/Nail/Screws (Titanium alloy) | 114,000 | 0.3 | - |
| Muscles | |||
| Sternocleidomastoid muscle | 0.5 | - | 246 |
| Trapezius muscle | 0.5 | - | 126 |
| Deltoid muscle | 0.5 | - | 1817 |
| Levator scapulae muscle | 0.5 | - | 126 |
| Supraspinatus muscle | 0.5 | - | 572 |
| Infraspinatus muscle | 0.5 | - | 1374 |
| Pectoralis major muscle | 0.5 | - | 1334 |
| Subscapularis muscle | 0.5 | - | 1630 |
| Ligaments | Stiffness (N/mm) | ||
| Anterior sternoclavicular ligament | 50 | - | - |
| Posterior sternoclavicular ligament | 50 | - | - |
| Interclavicular ligament | 50 | - | - |
| Costoclavicular ligament | 50 | - | - |
| Superior acromioclavicular ligament | 30 | - | - |
| Inferior acromioclavicular ligament | 30 | - | - |
| Coracoclavicular ligament | 30 | - | - |
| Coracoacromial ligament | 30 | - | - |
| Superior transverse scapular ligament | 30 | - | - |
| Superior glenohumeral ligament | 30 | - | - |
| Middle glenohumeral ligaments | 30 | - | - |
| Inferior glenohumeral ligaments | 30 | - | - |
| Coracohumeral ligament | 30 | - | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shih, K.-S.; Hsu, C.-C.; Shih, B.-Y. A Biomechanical Study of Various Fixation Strategies for the Treatment of Clavicle Fractures Using Three-Dimensional Upper-Body Musculoskeletal Finite Element Models. Appl. Sci. 2020, 10, 5651. https://0-doi-org.brum.beds.ac.uk/10.3390/app10165651
Shih K-S, Hsu C-C, Shih B-Y. A Biomechanical Study of Various Fixation Strategies for the Treatment of Clavicle Fractures Using Three-Dimensional Upper-Body Musculoskeletal Finite Element Models. Applied Sciences. 2020; 10(16):5651. https://0-doi-org.brum.beds.ac.uk/10.3390/app10165651
Chicago/Turabian StyleShih, Kao-Shang, Ching-Chi Hsu, and Bo-Yu Shih. 2020. "A Biomechanical Study of Various Fixation Strategies for the Treatment of Clavicle Fractures Using Three-Dimensional Upper-Body Musculoskeletal Finite Element Models" Applied Sciences 10, no. 16: 5651. https://0-doi-org.brum.beds.ac.uk/10.3390/app10165651