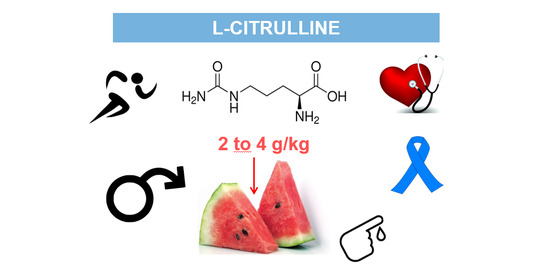
L-Citrulline: A Non-Essential Amino Acid with Important Roles in Human Health
Abstract
:1. Introduction
2. L-Citrulline Biochemistry
2.1. Endogenous Synthesis of L-Citrulline
2.2. L-Citrulline Metabolism
2.2.1. Arginine
Arginine Biosynthesis
Arginine Catabolism
2.2.2. Nitric Oxide Biosynthesis
2.2.3. Urea Cycle
3. L-Citrulline in Muscles
4. Pharmacokinetics and Pharmacodynamics of L-Citrulline
5. Ergogenic Effect of L-Citrulline Supplements
5.1. Ergogenic Effect of NO from L-Citrulline Supplements
5.2. Ergogenic Effect of Urea Cycle from L-Citrulline Supplements
6. Studies with Citrulline Malate (CM)
7. Other Positive Effects of L-Citrulline
7.1. L-Citrulline and Cardiovascular Diseases
7.2. L-Citrulline and Diabetes
7.3. L-Citrulline and Erectile Dysfunction
7.4. L-Citrulline and Cancer
8. Studies with Citrulline from Natural Sources: Watermelon
9. Conclusion, Perspectives and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bescós, R.; Sureda, A.; Tur, J.A.; Pons, A. The Effect of Nitric-Oxide-Related Supplements on Human Performance. Sports Med. 2012, 42, 99–117. [Google Scholar] [CrossRef]
- Mandel, H.; Levy, N.; Izkovitch, S.; Korman, S.H. Elevated plasma citrulline and arginine due to consumption of Citrullus vulgaris (watermelon). J. Inherit. Metab. Dis. 2005, 28, 467–472. [Google Scholar] [CrossRef]
- Windmueller, H.G.; Spaeth, A.E. Source and fate of circulating citrulline. Am. J. Physiol. Endocrinol. Metab. 1981, 241, E473–E480. [Google Scholar] [CrossRef] [PubMed]
- Rimando, A.M.; Perkins-Veazie, P.M. Determination of citrulline in watermelon rind. J. Chromatogr. A 2005, 1078, 196–200. [Google Scholar] [CrossRef]
- Tarazona-Díaz, M.P.; Viegas, J.; Moldao Martins, M.; Aguayo, E. Bio-active compounds of different cultivars from flesh and by-product of fresh-cut watermelons. J. Sci. Food Agric. 2011, 91, 805–812. [Google Scholar] [CrossRef]
- Joshi, V.; Joshi, M.; Silwal, D.; Noonan, K.; Rodriguez, S.; Penalosa, A. Systematized biosynthesis and catabolism regulate citrulline accumulation in watermelon. Phytochemistry 2019, 162, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Aguayo, E.; Tarazona-Díaz, M.P. National Patent: Procedimiento Para la Obtención de un Extracto de L-Citrulina a Partir de Plantas Cucurbitáceas. ES2394250 A1. Available online: http://www.oepm.es/pdf/ES/0000/000/02/39/42/ES-2394250_A1.pdf. (accessed on 12 November 2020).
- FAOSTAT Agriculture Data. 2021. Available online: http://www.fao.org/faostat/en/#data/QC/visualize (accessed on 12 November 2020).
- FAO. Fruit and Vegetables–Your Dietary Essentials. The International Year of Fruits and Vegetables, 2021, Background Paper. Rome. 2020. Available online: http://www.fao.org/documents/card/en/c/cb2395en (accessed on 15 November 2020).
- Crenn, P.; Messing, B.; Cynober, L. Citrulline as a biomarker of intestinal failure due to enterocyte mass reduction. Clin. Nutr. 2008, 27, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Morris, S.M., Jr. Arginine metabolism: Nitric oxide and beyond. Biochem. J. 1998, 336, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Breuillard, C.; Cynober, L.; Moinard, C.; Crenn, P.; Curis, E.; Chaumeil, J.C.; Cynober, L.; Sfar, S. Citrulline and nitrogen homeostasis: An overview. Amino Acids 2015, 47, 685–691. [Google Scholar] [CrossRef]
- Bahri, S.; Zerrouk, N.; Aussel, C.; Moinard, C.; Crenn, P.; Curis, E.; Chaumeil, J.C.; Cynober, L.; Sfar, S. Citrulline: From metabolism to therapeutic use. Nutrition 2013, 29, 479–484. [Google Scholar] [CrossRef] [Green Version]
- Marini, J.C.; Didelija, I.C.; Castillo, L.; Lee, B. Plasma Arginine and Ornithine Are the Main Citrulline Precursors in Mice Infused with Arginine-Free Diets. J. Nutr. 2010, 140, 1432–1437. [Google Scholar] [CrossRef] [Green Version]
- Tomlinson, C.; Rafii, M.; Ball, R.O.; Pencharz, P.B. Arginine Can Be Synthesized from Enteral Proline in Healthy Adult Humans. J. Nutr. 2011, 141, 1432–1436. [Google Scholar] [CrossRef] [PubMed]
- Wu, G. Intestinal Mucosal Amino Acid Catabolism. J. Nutr. 1998, 128, 1249–1252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barzał, J.A.; Szczylik, C.; Rzepecki, P.; Jaworska, M.; Anuszewska, E. Plasma citrulline level as a biomarker for cancer therapy-induced small bowel mucosal damage. Acta Biochim. Pol. 2014, 61, 615–631. [Google Scholar] [CrossRef] [Green Version]
- Curis, E.; Nicolis, I.; Moinard, C.; Osowska, S.; Zerrouk, N.; Bénazeth, S.; Cynober, L. Almost all about citrulline in mammals. Amino Acids 2005, 29, 177–205. [Google Scholar] [CrossRef]
- Luiking, Y.C.; Ten Have, G.A.M.; Wolfe, R.R.; Deutz, N.E.P. Arginine de novo and nitric oxide production in disease states. Am. J. Physiol.-Endocrinol. Metab. 2012, 303, E1177–E1189. [Google Scholar] [CrossRef] [Green Version]
- Morris, S.M. Regulation of arginine availability and its impact on NO synthesis. In Nitric Oxide: Biology and Pathobiology; Academic Press: Cambridge, MA, USA, 2020; pp. 187–197. [Google Scholar]
- Van De Poll, M.C.G.; Soeters, P.B.; Deutz, N.E.P.; Fearon, K.C.H.; DeJong, C.H.C. Renal metabolism of amino acids: Its role in interorgan amino acid exchange. Am. J. Clin. Nutr. 2004, 79, 185–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mori, M.; Gotoh, T. Arginine Metabolic Enzymes, Nitric Oxide and Infection. J. Nutr. 2004, 134, 2820S–2825S; discussion 2853S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durante, W.; Johnson, F.K.; Johnson, R.A. Arginase: A Critical Regulator of Nitric Oxide Synthesis and Vascular Function. Clin. Exp. Pharmacol. Physiol. 2007, 34, 906–911. [Google Scholar] [CrossRef] [Green Version]
- Pernow, J.; Jung, C. Arginase as a potential target in the treatment of cardiovascular disease: Reversal of arginine steal? Cardiovasc. Res. 2013, 98, 334–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vanhoutte, P.M.; Shimokawa, H.; Feletou, M.; Tang, E.H.C. Endothelial dysfunction and vascular disease-A 30th anniversary update. Acta Physiol. 2017, 219, 22–96. [Google Scholar] [CrossRef]
- Bode-Böger, S.M.; Böger, R.H.; Galland, A.; Tsikas, D.; Frölich, J.C. L-arginine-induced vasodilation in healthy humans: Pharmacokinetic-pharmacodynamic relationship. Br. J. Clin. Pharmacol. 1998, 46, 489–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Husson, A.; Brasse-Lagnel, C.; Fairand, A.; Renouf, S.; Lavoinne, A. Argininosuccinate synthetase from the urea cycle to the citrulline-NO cycle. Eur. J. Biochem.. 2003, 270, 1887–1899. [Google Scholar] [CrossRef] [PubMed]
- Foörstermann, U.; Sessa, W.C. Nitric oxide synthases: Regulation and function. Eur. Heart J. 2012, 33, 829–837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suzuki, T.; Morita, M.; Kobayashi, Y.; Kamimura, A. Oral L-citrulline supplementation enhances cycling time trial performance in healthy trained men: Double-blind randomized placebo-controlled 2-way crossover study. J. Int. Soc. Sports Nutr. 2016, 13, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morita, M.; Hayashi, T.; Ochiai, M.; Maeda, M.; Yamaguchi, T.; Ina, K.; Kuzuya, M. Oral supplementation with a combination of L-citrulline and L-arginine rapidly increases plasma L-arginine concentration and enhances NO bioavailability. Biochem. Biophys. Res. Commun. 2014, 454, 53–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luiking, Y.C.; Engelen, M.P.; Deutz, N.E. Regulation of nitric oxide production in health and disease. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 97–104. [Google Scholar] [CrossRef] [Green Version]
- Böger, R.H.; Sullivan, L.M.; Schwedhelm, E.; Wang, T.J.; Maas, R.; Benjamin, E.J.; Schulze, F.; Xanthakis, V.; Benndorf, R.A.; Vasan, R.S. Plasma Asymmetric Dimethylarginine and Incidence of Cardiovascular Disease and Death in the Community. Circulation 2009, 119, 1592–1600. [Google Scholar] [CrossRef]
- Kaore, S.N.; Amane, H.S.; Kaore, N.M. Citrulline: Pharmacological perspectives and its role as an emerging biomarker in future. Fundam. Clin. Pharmacol. 2013, 27, 35–50. [Google Scholar] [CrossRef]
- Cynober, L.; de Bandt, J.P.; Moinard, C. Leucine and citrulline: Two major regulators of protein turnover. In Nutrition in Intensive Care Medicine: Beyond Physiology; Singer, P., Ed.; Karger Medical and Scientific Publishers: Basel, Switzerland, 2012; Volume 105, pp. 97–105. [Google Scholar]
- Le Plénier, S.; Walrand, S.; Noirt, R.; Cynober, L.; Moinard, C. Effects of leucine and citrulline versus non-essential amino acids on muscle protein synthesis in fasted rat: A common activation pathway? Amino Acids 2012, 43, 1171–1178. [Google Scholar] [CrossRef]
- Faure, C.; Raynaud-Simon, A.; Ferry, A.; Daugé, V.; Cynober, L.; Aussel, C.; Moinard, C. Leucine and citrulline modulate muscle function in malnourished aged rats. Amino Acids 2011, 42, 1425–1433. [Google Scholar] [CrossRef]
- Jourdan, M.; Nair, K.S.; Carter, R.E.; Schimke, J.; Ford, G.C.; Marc, J.; Aussel, C.; Cynober, L. Citrulline stimulates muscle protein synthesis in the post-absorptive state in healthy people fed a low-protein diet–A pilot study. Clin. Nutr. 2015, 34, 449–456. [Google Scholar] [CrossRef] [Green Version]
- Goron, A.; Lamarche, F.; Cunin, V.; Dubouchaud, H.; Hourdé, C.; Noirez, P.; Corne, C.; Couturier, K.; Sève, M.; Fontaine, E.; et al. Synergistic effects of citrulline supplementation and exercise on performance in male rats: Evidence for implication of protein and energy metabolisms. Clin. Sci. 2017, 131, 775–790. [Google Scholar] [CrossRef]
- Ventura, G.; Noirez, P.; Breuillé, D.; Godin, J.P.; Pinaud, S.; Cleroux, M.; Choisy, C.; Le Plénier, S.; Bastic, V.; Neveux, N.; et al. Effect of citrulline on muscle functions during moderate dietary restriction in healthy adult rats. Amino Acids 2013, 45, 1123–1131. [Google Scholar] [CrossRef]
- Moinard, C.; Nicolis, I.; Neveux, N.; Darquy, S.; Benazeth, S.; Cynober, L. Dose-ranging effects of citrulline administration on plasma amino acids and hormonal patterns in healthy subjects: The Citrudose pharmacokinetic study. Br. J. Nutr. 2008, 99, 855–862. [Google Scholar] [CrossRef]
- Romero, M.J.; Platt, D.H.; Caldwell, R.W. Therapeutic Use of Citrulline in Cardiovascular Disease. Cardiovasc. Drug Rev. 2006, 24, 275–290. [Google Scholar]
- Rougé, C.; Des Robert, C.; Robins, A.; Le Bacquer, O.; Volteau, C.; De La Cochetière, M.F.; Darmaun, D. Manipulation of citrulline availability in humans. Am. J. Physiol. Gastrointest. Liver Physiol. 2007, 293, 1061–1067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwedhelm, E.; Maas, R.; Freese, R.; Jung, D.; Lukacs, Z.; Jambrecina, A.; Spickler, W.; Schulze, F.; Böger, R.H. Pharmacokinetic and pharmacodynamic properties of oral L-citrulline and L-arginine: Impact on nitric oxide metabolism. Br. J. Clin. Pharmacol. 2008, 65, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Moinard, C.; Maccario, J.; Walrand, S.; Lasserre, V.; Marc, J.; Boirie, Y.; Cynober, L. Arginine behaviour after arginine or citrulline administration in older subjects. Br. J. Nutr. 2016, 115, 399–404. [Google Scholar] [CrossRef] [Green Version]
- Closs, E.I.; Simon, A.; Vékony, N.; Rotmann, A. Plasma Membrane Transporters for Arginine. J. Nutr. 2004, 134, 2752S–2759S. [Google Scholar] [CrossRef]
- Vadgama, J.V.; Evered, D.F. Characteristics of L-Citrulline Transport across Rat Small Intestine In Vitro. Pediatr. Res. 1992, 32, 472–478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allerton, T.D.; Proctor, D.N.; Stephens, J.M.; Dugas, T.R.; Spielmann, G.; Irving, B.A. L-Citrulline Supplementation: Impact on Cardiometabolic Health. Nutrients 2018, 10, 921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grimble, G.K. Adverse Gastrointestinal Effects of Arginine and Related Amino Acids. J. Nutr. 2007, 137, 1693S–1701S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collins, J.K.; Wu, G.; Perkins-Veazie, P.; Spears, K.; Claypool, P.L.; Baker, R.A.; Clevidence, B.A. Watermelon consumption increases plasma arginine concentrations in adults. Nutrients 2007, 23, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Thibault, R.; Flet, L.; Vavasseur, F.; Lemerle, M.; Ferchaud-Roucher, V.; Picot, D.; Darmaun, D. Oral citrulline does not affect whole body protein metabolism in healthy human volunteers: Results of a prospective, randomized, double-blind, cross-over study. Clin. Nutr. 2011, 30, 807–811. [Google Scholar] [CrossRef] [PubMed]
- Cutrufello, P.T.; Gadomski, S.J.; Zavorsky, G.S. The effect of L-citrulline and watermelon juice supplementation on anaerobic and aerobic exercise performance. J. Sports Sci. 2015, 33, 1459–1466. [Google Scholar] [CrossRef] [PubMed]
- Bailey, S.J.; Blackwell, J.R.; Lord, T.; Vanhatalo, A.; Winyard, P.G.; Jones, A.M. l-Citrulline supplementation improves O2 uptake kinetics and high-intensity exercise performance in humans. J. Appl. Physiol. 2015, 119, 385–395. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Sánchez, A.; Alacid, F.; Rubio-Arias, J.A.; Fernández-Lobato, B.; Ramos-Campo, D.J.; Aguayo, E. Consumption of Watermelon Juice Enriched in l -Citrulline and Pomegranate Ellagitannins Enhanced Metabolism during Physical Exercise. J. Agric. Food Chem. 2017, 65, 4395–4404. [Google Scholar] [CrossRef]
- Martínez-Sánchez, A.; Ramos-Campo, D.J.; Fernández-Lobato, B.; Rubio-Arias, J.A.; Alacid, F.; Aguayo, E. Biochemical, physiological, and performance response of a functional watermelon juice enriched in L-citrulline during a half-marathon race. Food Nutr. Res. 2017, 61, 1330098. [Google Scholar] [CrossRef] [Green Version]
- Buckinx, F.; Gouspillou, G.; Carvalho, L.P.; Marcangeli, V.; Boutros, G.E.H.; Dulac, M.; Noirez, P.; Morais, J.A.; Gaudreau, P.; Aubertin-Leheudre, M. Effect of High-Intensity Interval Training Combined with L-Citrulline Supplementation on Functional Capacities and Muscle Function in Dynapenic-Obese Older Adults. J. Clin. Med. 2018, 7, 561. [Google Scholar] [CrossRef] [Green Version]
- Stanelle, S.T.; McLaughlin, K.L.; Crouse, S.F. One Week of L-Citrulline Supplementation Improves Performance in Trained Cyclists. J. Strength Cond. Res. 2020, 34, 647–652. [Google Scholar] [CrossRef] [PubMed]
- Ashley, J.; Kim, Y.; Gonzales, J.U. Impact of l-citrulline supplementation on oxygen uptake kinetics during walking. Appl. Physiol. Nutr. Metab. 2018, 43, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Romero, M.J.; Platt, D.H.; Tawfik, H.E.; Labazi, M.; El-Remessy, A.B.; Bartoli, M.; Caldwell, R.B.; Caldwell, R.W. Diabetes-induced Coronary Vascular Dysfunction Involves Increased Arginase Activity. Circ. Res. 2008, 102, 95–102. [Google Scholar] [CrossRef]
- McKinley-Barnard, S.; Andre, T.; Morita, M.; Willoughby, D.S. Combined L-citrulline and glutathione supplementation increases the concentration of markers indicative of nitric oxide synthesis. J. Int. Soc. Sports Nutr. 2015, 12, 27. [Google Scholar] [CrossRef] [Green Version]
- Sureda, A.; Córdova, A.; Ferrer, M.D.; Pérez, G.; Tur, J.A.; Pons, A. l-Citrulline-malate influence over branched chain amino acid utilization during exercise. Eur. J. Appl. Physiol. 2010, 110, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Takeda, K.; Machida, M.; Kohara, A.; Omi, N.; Takemasa, T. Effects of citrulline supplementation on fatigue and exercise performance in mice. J. Nutr. Sci. Vitaminol. 2011, 57, 246–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzales, J.U.; Raymond, A.; Ashley, J.; Kim, Y. Doesl-citrulline supplementation improve exercise blood flow in older adults? Exp. Physiol. 2017, 102, 1661–1671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meneguello, M.O.; Mendonça, J.R.; Lancha, A.H.; Costa Rosa, L.F.B.P. Effect of arginine, omithine and citrulline supplementation upon performance and metabolism of trained rats. Cell Biochem. Funct. 2013, 21, 85–91. [Google Scholar] [CrossRef]
- Gandevia, S.C. Spinal and Supraspinal Factors in Human Muscle Fatigue. Physiol. Rev. 2001, 81, 1725–1789. [Google Scholar] [CrossRef] [PubMed]
- Newsholme, E.A.; Blomstrand, E. Branched-Chain Amino Acids and Central Fatigue. J. Nutr. 2006, 136, 274S–276S. [Google Scholar] [CrossRef]
- Fernstrom, J.D. Branched-Chain Amino Acids and Brain Function. J. Nutr. 2005, 135, 1539S–1546S. [Google Scholar] [CrossRef]
- MacLean, D.A.; Graham, T.E.; Saltin, B. Stimulation of muscle ammonia production during exercise following branched-chain amino acid supplementation in humans. J. Physiol. 1996, 493 Pt 3, 909–922. [Google Scholar] [CrossRef] [Green Version]
- Nybo, L.; Dalsgaard, M.K.; Steensberg, A.; Møller, K.; Secher, N.H. Cerebral ammonia uptake and accumulation during prolonged exercise in humans. J. Physiol. 2005, 563, 285–290. [Google Scholar] [CrossRef]
- Wilkinson, D.J.; Smeeton, N.J.; Watt, P.W. Ammonia metabolism, the brain and fatigue; revisiting the link. Prog. Neurobiol. 2010, 91, 200–219. [Google Scholar] [CrossRef]
- Chang, C.-K.; Chien, K.-M.C.; Chang, J.-H.; Huang, M.-H.; Liang, Y.-C.; Liu, T.-H. Branched-Chain Amino Acids and Arginine Improve Performance in Two Consecutive Days of Simulated Handball Games in Male and Female Athletes: A Randomized Trial. PLoS ONE 2015, 10, e0121866. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.-F.; Wu, H.-J.; Chen, C.-Y.; Chou, K.-M.; Chang, C.-K. Branched-chain amino acids, arginine, citrulline alleviate central fatigue after 3 simulated matches in taekwondo athletes: A randomized controlled trial. J. Int. Soc. Sports Nutr. 2016, 13, 28. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Guisado, J.; Jakeman, P.M. Citrulline Malate Enhances Athletic Anaerobic Performance and Relieves Muscle Soreness. J. Strength Cond. Res. 2010, 24, 1215–1222. [Google Scholar] [CrossRef] [PubMed]
- Bendahan, D.; Mattei, J.P.; Ghattas, B.; Confort-Gouny, S.; Le Guern, M.E.; Cozzone, P.J. Citrulline/malate promotes aerobic energy production in human exercising muscle. Br. J. Sports Med. 2002, 36, 282–289. [Google Scholar] [CrossRef] [Green Version]
- Figueroa, A.; Wong, A.; Jaime, S.J.; Gonzales, J.U. Influence of L-citrulline and watermelon supplementation on vascular function and exercise performance. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 92–98. [Google Scholar] [CrossRef]
- Glenn, J.M.; Gray, M.; Wethington, L.N.; Stone, M.S.; Stewart, R.W.; Moyen, N.E. Acute citrulline malate supplementation improves upper- and lower-body submaximal weightlifting exercise performance in resistance-trained females. Eur. J. Nutr. 2015, 56, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Kiyici, F.; Eroglu, H.; Kishali, N.F.; Burmaoglu, G. The Effect of Citrulline/Malate on Blood Lactate Levels in Intensive Exercise. Biochem. Genet. 2017, 55, 387–394. [Google Scholar] [CrossRef]
- López-Cabral, J.A.; Rivera-Cisneros, A.; Rodríguez-Camacho, H.; Sánchez-González, J.M.; Serna-Sánchez, I.; Trejo-Trejo, M. Modification of fatigue indicators using citrulline malate for high performance endurance athletes. Rev. Mex. Patol. Clin. Med. Lab. 2012, 59, 194–201. [Google Scholar]
- Giannesini, B.; Le Fur, Y.; Cozzone, P.J.; Verleye, M.; Le Guern, M.E.; Bendahan, D. Citrulline malate supplementation increases muscle efficiency in rat skeletal muscle. Eur. J. Pharmacol. 2011, 667, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Wax, B.; Kavazis, A.N.; Weldon, K.; Sperlak, J. Effects of Supplemental Citrulline Malate Ingestion During Repeated Bouts of Lower-Body Exercise in Advanced Weightlifters. J. Strength Cond. Res. 2015, 29, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Cunniffe, B.; Papageorgiou, M.; O’Brien, B.; Davies, N.A.; Grimble, G.K.; Cardinale, M. Acute Citrulline-Malate Supplementation and High-Intensity Cycling Performance. J. Strength Cond. Res. 2016, 30, 2638–2647. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, D.K.; Jacinto, J.L.; de Andrade, W.B.; Roveratti, M.C.; Estoche, J.M.; Balvedi, M.C.W.; de Oliveira, D.B.; da Silva, R.A.; Aguiar, A.F. Citrulline malate does not improve muscle recovery after resistance exercise in untrained young adult men. Nutrients 2017, 9, 1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casonatto, J.; Cavalaria, J.V.; Goessler, K.F.; Christofaro, D.G.D.; Polito, M.D.; Enokida, D.M.; Grandolfi, K. Citrulline malate supplementation might potentiate post-exercise hypotension in hypertensives: A 24-hour analysis. Sci. Sports 2019, 34, 261.1–261.9. [Google Scholar] [CrossRef]
- Versari, D.; Daghini, E.; Virdis, A.; Ghiadoni, L.; Taddei, S. Endothelial Dysfunction as a Target for Prevention of Cardiovascular Disease. Diabetes Care 2009, 32, S314–S321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharifi-Rad, J.; Rodrigues, C.F.; Sharopov, F.; Docea, A.O.; Can Karaca, A.; Sharifi-Rad, M.; Kahveci Karıncaoglu, D.; Gülseren, G.; Şenol, E.; Demircan, E.; et al. Diet, Lifestyle and Cardiovascular Diseases: Linking Pathophysiology to Cardioprotective Effects of Natural Bioactive Compounds. Int. J. Environ. Res. Public Health 2020, 17, 2326. [Google Scholar] [CrossRef] [Green Version]
- Le Roux-Mallouf, T.; Pelen, F.; Vallejo, A.; Halimaoui, I.; Doutreleau, S.; Verges, S. Effect of chronic nitrate and citrulline supplementation on vascular function and exercise performance in older individuals. Aging 2019, 11, 3315–3332. [Google Scholar] [CrossRef]
- Khalaf, D.; Krüger, M.; Wehland, M.; Infanger, M.; Grimm, D. The Effects of Oral l-Arginine and l-Citrulline Supplementation on Blood Pressure. Nutrients 2019, 11, 1679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayashi, T.; Juliet, P.A.R.; Matsui-Hirai, H.; Miyazaki, A.; Fukatsu, A.; Funami, J.; Iguchi, A.; Ignarro, L.J. L-citrulline and L-arginine supplementation retards the progression of high-cholesterol-diet-induced atherosclerosis in rabbits. Proc. Natl. Acad. Sci. USA 2005, 102, 13681–13686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morita, M.; Sakurada, M.; Watanabe, F.; Yamasaki, T.; Doi, H.; Ezaki, H.; Morishita, K.; Miyake, T. Effects of Oral L-Citrulline Supplementation on Lipoprotein Oxidation and Endothelial Dysfunction in Humans with Vasospastic Angina. Immunol. Endocr. Metab. Agents Med. Chem. 2013, 13, 214–220. [Google Scholar] [CrossRef] [Green Version]
- Kim, I.-Y.; Schutzler, S.E.; Schrader, A.; Spencer, H.J.; Azhar, G.; Deutz, N.E.P.; Wolfe, R.R. Acute ingestion of citrulline stimulates nitric oxide synthesis but does not increase blood flow in healthy young and older adults with heart failure. Am. J. Physiol. Metab. 2015, 309, E915–E924. [Google Scholar] [CrossRef] [Green Version]
- Wong, A.; Chernykh, O.; Figueroa, A. Chronic l-citrulline supplementation improves cardiac sympathovagal balance in obese postmenopausal women: A preliminary report. Auton. Neurosci. 2016, 198, 50–53. [Google Scholar] [CrossRef]
- El-Bassossy, H.M.; El-Fawal, R.; Fahmy, A. Arginase inhibition alleviates hypertension associated with diabetes: Effect on endothelial dependent relaxation and NO production. Vasc. Pharmacol. 2012, 57, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, T.; Maeda, M.; Hayashi, T. Administration of L-arginine plus L-citrulline or L-citrulline alone successfully retarded endothelial senescence. PLoS ONE 2018, 13, e0192252. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Collins, J.K.; Perkins-Veazie, P.; Siddiq, M.; Dolan, K.D.; Kelly, K.A.; Heaps, C.L.; Meininger, C.J. Dietary supplementation with watermelon pomace juice enhances arginine availability and ameliorates the metabolic syndrome in Zucker diabetic fatty rats. J. Nutr. 2007, 137, 2680–2685. [Google Scholar] [CrossRef]
- Kövamees, O.; Shemyakin, A.; Checa, A.; Wheelock, C.E.; Lundberg, J.O.; Östenson, C.-G.; Pernow, J. Arginase inhibition improves microvascular endothelial function in patients with type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 2016, 101, 3952–3958. [Google Scholar] [CrossRef] [PubMed]
- El-Bassossy, H.M.; El-Fawal, R.; Fahmy, A.; Watson, M.L. Arginase inhibition alleviates hypertension in the metabolic syndrome. Br. J. Pharmacol. 2013, 169, 693–703. [Google Scholar] [CrossRef] [Green Version]
- Wijnands, K.A.; Meesters, D.M.; Van Barneveld, K.W.Y.; Visschers, R.G.J.; Briedé, J.J.; VandenDriessche, B.; Van Eijk, H.M.H.; Bessems, B.A.F.M.; Hoven, N.V.D.; Von Wintersdorff, C.J.H.; et al. Citrulline Supplementation Improves Organ Perfusion and Arginine Availability under Conditions with Enhanced Arginase Activity. Nutrients 2015, 7, 5217–5238. [Google Scholar] [CrossRef] [Green Version]
- You, H.; Gao, T.; Cooper, T.K.; Morris, S.M.; Awad, A.S. Diabetic nephropathy is resistant to oral l-arginine or l-citrulline supplementation. Am. J. Physiol. Renal Physiol. 2014, 307, F1292–F1301. [Google Scholar] [CrossRef]
- Azizi, S.; Mahdavi, R.; Vaghef-Mehrabany, E.; Maleki, V.; Karamzad, N.; Ebrahimi-Mameghani, M. Potential roles of Citrulline and watermelon extract on metabolic and inflammatory variables in diabetes mellitus, current evidence and future directions: A systematic review. Clin. Exp. Pharmacol. Physiol. 2019, 47, 187–198. [Google Scholar] [CrossRef]
- Cormio, L.; De Siati, M.; Lorusso, F.; Selvaggio, O.; Mirabella, L.; Sanguedolce, F.; Carrieri, G. Oral L-Citrulline Supplementation Improves Erection Hardness in Men With Mild Erectile Dysfunction. Urology 2011, 77, 119–122. [Google Scholar] [CrossRef]
- Barassi, A.; Romanelli, M.M.C.; Pezzilli, R.; Damele, C.A.L.; Vaccalluzzo, L.; Goi, G.; Papini, N.; Colpi, G.M.; Massaccesi, L.; D’Eril, G.V.M. Levels of l -arginine and l -citrulline in patients with erectile dysfunction of different etiology. Andrology 2017, 5, 256–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lacchini, R.; Tanus-Santos, J.E. Pharmacogenetics of erectile dysfunction: Navigating into uncharted waters. Pharmacogenomics 2014, 15, 1519–1538. [Google Scholar] [CrossRef]
- Shiota, A.; Hotta, Y.; Kataoka, T.; Morita, M.; Maeda, Y.; Kimura, K. Oral l-Citrulline Supplementation Improves Erectile Function in Rats with Acute Arteriogenic Erectile Dysfunction. J. Sex. Med. 2013, 10, 2423–2429. [Google Scholar] [CrossRef]
- Shirai, M.; Hiramatsu, I.; Aoki, Y.; Shimoyama, H.; Mizuno, T.; Nozaki, T.; Fukuhara, S.; Iwasa, A.; Kageyama, S.; Tsujimura, A. Oral L-citrulline and Transresveratrol Supplementation Improves Erectile Function in Men With Phosphodiesterase 5 Inhibitors: A Randomized, Double-Blind, Placebo-Controlled Crossover Pilot Study. Sex. Med. 2018, 6, 291–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salehi, B.; Azzini, E.; Zucca, P.; Varoni, E.M.; Kumar, N.V.A.; Dini, L.; Panzarini, E.; Rajkovic, J.; Fokou, P.V.T.; Peluso, I.; et al. Plant-Derived Bioactives and Oxidative Stress-Related Disorders: A Key Trend towards Healthy Aging and Longevity Promotion. Appl. Sci. 2020, 10, 947. [Google Scholar] [CrossRef] [Green Version]
- Burke, A.J.; Sullivan, F.J.; Giles, F.J.; Glynn, S.A. The yin and yang of nitric oxide in cancer progression. Carcinogenesis 2013, 34, 503–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fahey, J.M.; Girotti, A.W. Accelerated migration and invasion of prostate cancer cells after a photodynamic therapy-like challenge: Role of nitric oxide. Nitric Oxide-Biol. Chem. 2015, 49, 47–55. [Google Scholar] [CrossRef] [Green Version]
- Carpenter, A.W.; Schoenfisch, M.H. Nitric oxide release: Part II. Therapeutic applications. Chem. Soc. Rev. 2012, 41, 3742–3752. [Google Scholar] [CrossRef]
- Seabra, A.B. Nitric Oxide Donors: Novel Biomedical Applications and Perspective, 1st ed.; Elsevier Inc.: London, UK, 2017. [Google Scholar]
- Timosenko, E.; Hadjinicolaou, A.V.; Cerundolo, V. Modulation of cancer-specific immune responses by amino acid degrading enzymes. Immunotherapy 2017, 9, 83–97. [Google Scholar] [CrossRef] [Green Version]
- Bronte, V.; Zanovello, P. Regulation of immune responses by L-arginine metabolism. Nat. Rev. Immunol. 2005, 5, 641–654. [Google Scholar] [CrossRef]
- Munder, M. Arginase: An emerging key player in the mammalian immune system: REVIEW. Br. J. Pharmacol. 2009, 158, 638–651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pham, T.-N.; Liagre, B.; Girard-Thernier, C.; Demougeot, C. Research of novel anticancer agents targeting arginase inhibition. Drug Discov. Today 2018, 23, 871–878. [Google Scholar] [CrossRef]
- Ambe, K.; Watanabe, H.; Takahashi, S.; Nakagawa, T.; Sasaki, J. Production and physiological role of NO in the oral cavity. Jpn. Dent. Sci. Rev. 2016, 52, 14–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajendran, R.; Varkey, S. Inducible nitric oxide synthase expression is upregulated in oral submucous fibrosis. Indian J. Dent. Res. 2007, 18, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Saito, H.; Oro, S.; Tatebe, S.; Ikeguchi, M.; Tsujitani, S. Expression of Inducible Nitric Oxide Synthase Is Significantly Correlated with Expression of Vascular Endothelial Growth Factor and Dendritic Cell Infiltration in Patients with Advanced Gastric Carcinoma. Oncology 2005, 68, 471–478. [Google Scholar] [CrossRef] [Green Version]
- Mumenthaler, S.M.; Rozengurt, N.; Livesay, J.C.; Sabaghian, A.; Cederbaum, S.D.; Grody, W.W. Disruption of arginase II alters prostate tumor formation in TRAMP mice. Prostate 2008, 68, 1561–1569. [Google Scholar] [CrossRef]
- Yin, D.; Wang, X.; Konda, B.M.; Ong, J.M.; Hu, J.; Sacapano, M.R.; Ko, M.K.; Espinoza, A.J.; Irvin, D.K.; Shu, Y.; et al. Increase in Brain Tumor Permeability in Glioma-Bearing Rats with Nitric Oxide Donors. Clin. Cancer Res. 2008, 14, 4002–4009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Onoue, H.; Katusic, Z.S. Role of potassium channels in relaxations of canine middle cerebral arteries induced by nitric oxide donors. Stroke 1997, 28, 1264–1271. [Google Scholar] [CrossRef]
- Ningaraj, N.S.; Rao, M.; Hashizume, K.; Asotra, K.; Black, K.L. Regulation of Blood-Brain Tumor Barrier Permeability by Calcium-Activated Potassium Channels. J. Pharmacol. Exp. Ther. 2002, 301, 838–851. [Google Scholar] [CrossRef] [Green Version]
- Statista. Global Sports Nutrition Market 2018–2023. Available online: https://0-www-statista-com.brum.beds.ac.uk/study/37001/sports-drinks-statista-dossier (accessed on 8 January 2021).
- Fields, S.K.; Macdonald, J.; Joseph, A.M.; Wold, L.E.; Collins, C.L.; Comstock, R.D. Consumption of Sports and Energy Drinks by High School Athletes in the United States: A Pilot Study. Beverages 2015, 1, 218–224. [Google Scholar] [CrossRef] [Green Version]
- Cordrey, K.; Keim, S.A.; Milanaik, R.; Adesman, A. Adolescent Consumption of Sports Drinks. Pediatrics 2018, 141, e20172784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cruz-Muñoz, V.; Urquizu-Rovira, M.; Valls-Ibañez, V.; Manresa-Domínguez, J.M.; Ruiz-Blanco, G.; Urquizu-Rovira, M.; Toran, P. Consumo de bebidas refrescantes, deportivas y energéticas en adolescentes. Estudio BEENIS. In Anales de Pediatría; Elsevier Doyma: Amsterdam, The Netherlands, 2020; Volume 93, pp. 242–250. [Google Scholar]
- Malik, V.S.; Pan, A.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 1084–1102. [Google Scholar] [CrossRef] [Green Version]
- Maoto, M.M.; Beswa, D.; Jideani, A.I.O. Watermelon as a potential fruit snack. Int. J. Food Prop. 2019, 22, 355–370. [Google Scholar] [CrossRef] [Green Version]
- Hartman, J.L.; Wehner, T.C.; Ma, G.; Perkins-Veazie, P. Citrulline and Arginine Content of Taxa of Cucurbitaceae. Horticulturae 2019, 5, 22. [Google Scholar] [CrossRef] [Green Version]
- Akashi, K.; Miyake, C.; Yokota, A. Citrulline, a novel compatible solute in drought-tolerant wild watermelon leaves, is an efficient hydroxyl radical scavenger. FEBS Lett. 2001, 508, 438–442. [Google Scholar] [CrossRef] [Green Version]
- Hdider, C.; Tlili, I.; Ilahy, R. Chapter 32–Watermelon. Nutritional Composition and Antioxidant Properties of Fruits and Vegetables; Jaiswal, A.K., Ed.; Academic Press: Cambridge, MA, USA, 2020; pp. 515–531. ISBN 9780128127803. [Google Scholar]
- Naz, A.; Butt, M.S.; Pasha, I.; Nawaz, H. Antioxidant Indices of Watermelon Juice and Lycopene Extract. Pak. J. Nutr. 2013, 12, 255–260. [Google Scholar] [CrossRef] [Green Version]
- Candir, E.; Yetisir, H.; Karaca, F.; Ustun, D. Phytochemical characteristics of grafted watermelon on different bottle gourds (Lagenaria siceraria) collected from Mediterranean region of Turkey. Turk. J. Agric.-Food Sci. Technol. 2013, 37, 443–456. [Google Scholar]
- USDA. USDA National Nutrient Database for Standard Reference Release 23; Department of Agriculture, Agricultural Research Service: Washington, DC, USA, 2020.
- Tlili, I.; Hdider, C.; Lenucci, M.S.; Ilahy, R.; Jebari, H.; Dalessandro, G. Bioactive compounds and antioxidant activities during fruit ripening of watermelon cultivars. J. Food Compos. Anal. 2011, 24, 923–928. [Google Scholar] [CrossRef]
- Kim, C.-H.; Park, M.-K.; Kim, S.-K.; Cho, Y.-H. Antioxidant capacity and anti-inflammatory activity of lycopene in watermelon. Int. J. Food Sci. Technol. 2014, 49, 2083–2091. [Google Scholar] [CrossRef]
- Saini, R.K.; Rengasamy, K.R.; Mahomoodally, F.M.; Keum, Y.-S. Protective effects of lycopene in cancer, cardiovascular, and neurodegenerative diseases: An update on epidemiological and mechanistic perspectives. Pharmacol. Res. 2020, 155, 104730. [Google Scholar] [CrossRef] [PubMed]
- Perkins-Veazie, P.; Collins, J.K.; Davis, A.R.; Roberts, W. Carotenoid Content of 50 Watermelon Cultivars. J. Agric. Food Chem. 2006, 54, 2593–2597. [Google Scholar] [CrossRef]
- Edwards, A.J.; Vinyard, B.T.; Wiley, E.R.; Brown, E.D.; Collins, J.K.; Perkins-Veazie, P.; Baker, R.A.; Clevidence, B.A. Consumption of watermelon juice increases plasma concentrations of lycopene and beta-carotene in humans. J. Nutr. 2003, 133, 1043–1050. [Google Scholar] [CrossRef]
- Naderi, A.; Rezaei, S.; Moussa, A.; Levers, K.; Earnest, C.P. Fruit for sport. Trends Food Sci. Technol. 2018, 74, 85–98. [Google Scholar] [CrossRef]
- Tarazona-Díaz, M.P.; Alacid, F.; Carrasco, M.; Martínez, I.; Aguayo, E. Watermelon Juice: Potential Functional Drink for Sore Muscle Relief in Athletes. J. Agric. Food Chem. 2013, 61, 7522–7528. [Google Scholar] [CrossRef]
- Blohm, K.; Beidler, J.; Rosen, P.; Kressler, J.; Hong, M.Y. Effect of acute watermelon juice supplementation on post-submaximal exercise heart rate recovery, blood lactate, blood pressure, blood glucose and muscle soreness in healthy non-athletic men and women. Int. J. Food Sci. Nutr. 2019, 71, 482–489. [Google Scholar] [CrossRef]
- Bailey, S.J.; Blackwell, J.R.; Williams, E.; Vanhatalo, A.; Wylie, L.J.; Winyard, P.G.; Jones, A.M. Two weeks of watermelon juice supplementation improves nitric oxide bioavailability but not endurance exercise performance in humans. Nitric Oxide 2016, 59, 10–20. [Google Scholar] [CrossRef] [Green Version]
- Shanely, R.A.; Nieman, D.C.; Perkins-Veazie, P.; Henson, D.A.; Meaney, M.P.; Knab, A.M.; Cialdell-Kam, L. Comparison of Watermelon and Carbohydrate Beverage on Exercise-Induced Alterations in Systemic Inflammation, Immune Dysfunction, and Plasma Antioxidant Capacity. Nutrients 2016, 8, 518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhim, H.C.; Kim, S.J.; Park, J.; Jang, K.-M. Effect of citrulline on post-exercise rating of perceived exertion, muscle soreness, and blood lactate levels: A systematic review and meta-analysis. J. Sport Heal. Sci. 2020, 9, 553–561. [Google Scholar] [CrossRef]
- Massa, N.M.L.; Silva, A.S.; de Oliveira, C.V.C.; Costa, M.J.C.; Persuhn, D.C.; Barbosa, C.V.S.; Goncalves, M.C.R. Supplementation with Watermelon Extract Reduces Total Cholesterol and LDL Cholesterol in Adults with Dyslipidaemia under the Influence of the MTHFR C677T Polymorphism. J. Am. Coll. Nutr. 2016, 35, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, A.; Wong, A.; Hooshmand, S.; Sanchez-Gonzalez, M.A. Effects of watermelon supplementation on arterial stiffness and wave reflection amplitude in postmenopausal women. Menopause 2013, 20, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, A.; Wong, A.; Kalfon, R. Effects of Watermelon Supplementation on Aortic Hemodynamic Responses to the Cold Pressor Test in Obese Hypertensive Adults. Am. J. Hypertens. 2014, 27, 899–906. [Google Scholar] [CrossRef] [Green Version]
- Figueroa, A.; Sanchez-Gonzalez, M.A.; Wong, A.; Arjmandi, B.H. Watermelon extract supplementation reduces ankle blood pressure and carotid augmentation index in obese adults with prehypertension or hypertension. Am. J. Hypertens. 2012, 25, 640–643. [Google Scholar] [CrossRef] [Green Version]
- Shanely, R.A.; Zwetsloot, J.J.; Jurrissen, T.J.; Hannan, L.C.; Zwetsloot, K.A.; Needle, A.R.; Bishop, A.E.; Wu, G.; Perkins-Veazie, P. Daily watermelon consumption decreases plasma sVCAM-1 levels in overweight and obese postmenopausal women. Nutr. Res. 2020, 76, 9–19. [Google Scholar] [CrossRef]
- Lum, T.; Connolly, M.; Marx, A.; Beidler, J.; Hooshmand, S.; Kern, M.; Liu, C.; Hong, M.Y. Effects of Fresh Watermelon Consumption on the Acute Satiety Response and Cardiometabolic Risk Factors in Overweight and Obese Adults. Nutrients 2019, 11, 595. [Google Scholar] [CrossRef] [Green Version]
- Hong, M.Y.; Hartig, N.; Kaufman, K.; Hooshmand, S.; Figueroa, A.; Kern, M. Watermelon consumption improves inflammation and antioxidant capacity in rats fed an atherogenic diet. Nutr. Res. 2015, 35, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Hong, M.Y.; Beidler, J.; Hooshmand, S.; Figueroa, A.; Kern, M. Watermelon and l-arginine consumption improve serum lipid profile and reduce inflammation and oxidative stress by altering gene expression in rats fed an atherogenic diet. Nutr. Res. 2018, 58, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Hong, M.Y.; Tseng, Y.-T.; Kalaba, M.; Beidler, J. Effects of watermelon powder supplementation on colitis in high-fat diet-fed and dextran sodium sulfate-treated rats. J. Funct. Foods 2019, 54, 520–528. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguayo, E.; Martínez-Sánchez, A.; Fernández-Lobato, B.; Alacid, F. L-Citrulline: A Non-Essential Amino Acid with Important Roles in Human Health. Appl. Sci. 2021, 11, 3293. https://0-doi-org.brum.beds.ac.uk/10.3390/app11073293
Aguayo E, Martínez-Sánchez A, Fernández-Lobato B, Alacid F. L-Citrulline: A Non-Essential Amino Acid with Important Roles in Human Health. Applied Sciences. 2021; 11(7):3293. https://0-doi-org.brum.beds.ac.uk/10.3390/app11073293
Chicago/Turabian StyleAguayo, Encarna, Ascensión Martínez-Sánchez, Bárbara Fernández-Lobato, and Fernando Alacid. 2021. "L-Citrulline: A Non-Essential Amino Acid with Important Roles in Human Health" Applied Sciences 11, no. 7: 3293. https://0-doi-org.brum.beds.ac.uk/10.3390/app11073293