Is Early Oral Antimicrobial Switch Useful for Less Critically Ill Adults with Community-Onset Bacteraemia in Emergency Departments?
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Setting
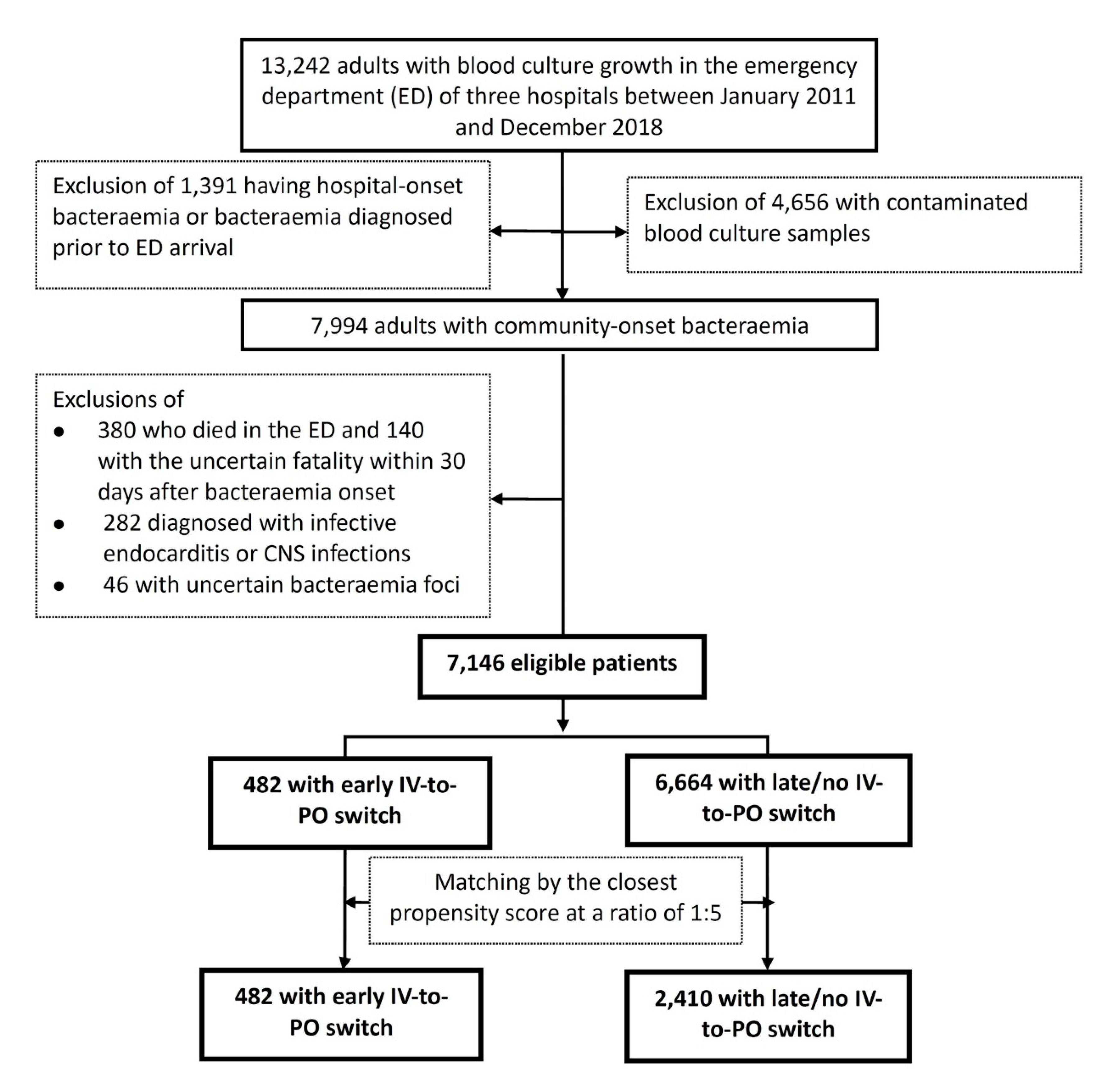
2.2. Selection of Participants
2.3. Methods of Measurement
2.4. Outcome Measures
2.5. Definitions
2.6. Microbiological Methods
2.7. Statistical Analyses
3. Results
3.1. Characteristics of Study Subjects
3.2. Baseline Characteristics and Outcomes between the Early and Late/No IV-to-PO Switch Groups
3.3. Predictors of 30-Day Crude Mortality
3.4. Clinical Characteristics and Outcomes of the PS-Matched Cohort
3.5. Predictors of Post-Switch 30-Day Crude Mortality in Early Switch Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Laupland, K.B.; Gregson, D.B.; Flemons, W.W.; Hawkins, D.; Ross, T.; Church, D.L. Burden of community-onset bloodstream infection: A population-based assessment. Epidemiol. Infect. 2007, 135, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.W.; Pruess, K.E.; Lee, T.H. How bad are bacteremia and sepsis? Outcomes in a cohort with suspected bacteremia. Arch. Intern. Med. 1995, 155, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.C.; Lee, C.H.; Hong, M.Y.; Tang, H.J.; Ko, W.C. Timing of appropriate empirical antimicrobial administration and outcome of adults with community-onset bacteremia. Crit. Care 2017, 21, 119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, C.C.; Lee, C.H.; Yang, C.Y.; Hsieh, C.C.; Tang, H.J.; Ko, W.C. Beneficial effects of early empirical administration of appropriate antimicrobials on survival and defervescence in adults with community-onset bacteremia. Crit. Care 2019, 23, 363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omidvari, K.; de Boisblanc, B.P.; Karam, G.; Nelson, S.; Haponik, E.; Summer, W. Early transition to oral antibiotic therapy for community-acquired pneumonia: Duration of therapy, clinical outcomes, and cost analysis. Respir. Med. 1998, 92, 1032–1039. [Google Scholar] [CrossRef] [Green Version]
- Gangji, D.; Jacobs, F.; de Jonckheer, J.; Coppens, L.; Serruys, E.; Hanotte, F.; Motte, S.; Thys, J.P. Randomized study of intravenous versus sequential intravenous/oral regimen of ciprofloxacin in the treatment of gram-negative septicemia. Am. J. Med. 1989, 87, 206S–208S. [Google Scholar] [CrossRef]
- Erickson, R.M.; Tritle, B.J.; Spivak, E.S.; Timbrook, T.T. Impact of an antimicrobial stewardship bundle for uncomplicated gram-negative bacteremia. Open Forum Infect. Dis. 2019, 6, ofz490. [Google Scholar] [CrossRef] [Green Version]
- Tamma, P.D.; Conley, A.T.; Cosgrove, S.E.; Harris, A.D.; Lautenbach, E.; Amoah, J.; Avdic, E.; Tolomeo, P.; Wise, J.; Subudhi, S.; et al. Association of 30-Day Mortality With Oral Step-Down vs Continued Intravenous Therapy in Patients Hospitalized With Enterobacteriaceae Bacteremia. JAMA Intern. Med. 2019, 179, 316–323. [Google Scholar] [CrossRef]
- Lee, C.C.; Hsieh, C.C.; Yang, C.Y.; Hong, M.Y.; Lee, C.H.; Tang, H.J.; Ko, W.C. Short versus long duration antimicrobial treatment for community-onset bacteraemia: A propensity score matching study. Int. J. Antimicrob. Agents 2019, 54, 176–183. [Google Scholar] [CrossRef]
- Amoah, J.; Stuart, E.A.; Cosgrove, S.E.; Harris, A.D.; Han, J.H.; Lautenbach, E.; Tamma, P.D. Comparing Propensity Score Methods versus Traditional Regression Analysis for the Evaluation of Observational Data: A Case Study Evaluating the Treatment of Gram-Negative Bloodstream Infections. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Gentry, L.O.; Koshdel, A. Intravenous/oral ciprofloxacin versus intravenous ceftazidime in the treatment of serious gram-negative infections of the skin and skin structure. Am. J. Med. 1989, 87, 132S–135S. [Google Scholar] [CrossRef]
- Sevinc, F.; Prins, J.M.; Koopmans, R.P.; Langendijk, P.N.; Bossuyt, P.M.; Dankert, J.; Speelman, P. Early switch from intravenous to oral antibiotics: Guidelines and implementation in a large teaching hospital. J. Antimicrob. Chemother. 1999, 43, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Ahkee, S.; Smith, S.; Newman, D.; Ritter, W.; Burke, J.; Ramirez, J.A. Early switch from intravenous to oral antibiotics in hospitalized patients with infections: A 6-month prospective study. Pharmacotherapy 1997, 17, 569–575. [Google Scholar] [PubMed]
- Mandell, L.A.; Bergeron, M.G.; Gribble, M.J.; Jewesson, P.J.; Low, D.E.; Marrie, T.J.; Nicolle, L.E. Sequential antibiotic therapy: Effective cost management and patient care. Can. J. Infect. Dis. 1995, 6, 306–315. [Google Scholar] [CrossRef] [Green Version]
- Hamilton-Miller, J.M. Switch therapy: The theory and practice of early change from parenteral to non-parenteral antibiotic administration. Clin. Microbiol. Infect. 1996, 2, 12–19. [Google Scholar] [CrossRef] [Green Version]
- Shih, F.Y.; Ma, M.H.; Chen, S.C.; Wang, H.P.; Fang, C.C.; Shyu, R.S.; Huang, G.T.; Wang, S.M. ED overcrowding in Taiwan: Facts and strategies. Am. J. Emerg. Med. 1999, 17, 198–202. [Google Scholar] [CrossRef]
- Trzeciak, S.; Rivers, E.P. Emergency department overcrowding in the United States: An emerging threat to patient safety and public health. Emerg. Med. J. 2003, 20, 402–405. [Google Scholar] [CrossRef] [Green Version]
- Cowan, R.M.; Trzeciak, S. Clinical review: Emergency department overcrowding and the potential impact on the critically ill. Crit. Care 2005, 9, 291–295. [Google Scholar] [CrossRef] [Green Version]
- Derlet, R.W. Overcrowding in emergency departments: Increased demand and decreased capacity. Ann. Emerg. Med. 2002, 39, 430–432. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Lee, C.C.; Lin, W.J.; Shih, H.I.; Wu, C.J.; Chen, P.L.; Lee, H.C.; Lee, N.Y.; Chang, C.M.; Wang, L.R.; Ko, W.C. Clinical significance of potential contaminants in blood cultures among patients in a medical center. J. Microbiol. Immunol. Infect. 2007, 40, 438–444. [Google Scholar] [PubMed]
- Gilbert, D.N.; Chambers, H.F.; Eliopoulos, G.M.; Saag, M.S.; Pavia, A.T. Antibacterial Durg Dosage/Side Effects. Sanford Guide Antimicrob. Ther. 2020, 106–124. [Google Scholar]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Approved Standard. 30th Informational Supplement; CLSI document M100-S30; CLSI: Wayne, PA, USA, 2020. [Google Scholar]
- Leibovici, L.; Shraga, I.; Drucker, M.; Konigsberger, H.; Samra, Z.; Pitlik, S.D. The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J. Intern. Med. 1998, 244, 379–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leligdowicz, A.; Dodek, P.M.; Norena, M.; Wong, H.; Kumar, A.; Kumar, A.; Co-operative Antimicrobial Therapy of Septic Shock Database Research Group. Association between source of infection and hospital mortality in patients who have septic shock. Am. J. Respir. Crit. Care Med. 2014, 189, 1204–1213. [Google Scholar] [CrossRef]
- Garner, J.S.; Jarvis, W.R.; Emori, T.G.; Horan, T.C.; Hughes, J.M. CDC definitions for nosocomial infections, 1988. Am. J. Infect. Control. 1988, 16, 128–140. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef] [PubMed]
- Chotiprasitsakul, D.; Han, J.H.; Cosgrove, S.E.; Harris, A.D.; Lautenbach, E.; Conley, A.T.; Tolomeo, P.; Wise, J.; Tamma, P.D.; Antibacterial Resistance Leadership, G. Comparing the Outcomes of Adults With Enterobacteriaceae Bacteremia Receiving Short-Course Versus Prolonged-Course Antibiotic Therapy in a Multicenter, Propensity Score-Matched Cohort. Clin. Infect. Dis. 2018, 66, 172–177. [Google Scholar] [CrossRef]
- Sawyer, R.G.; Claridge, J.A.; Nathens, A.B.; Rotstein, O.D.; Duane, T.M.; Evans, H.L.; Cook, C.H.; O’Neill, P.J.; Mazuski, J.E.; Askari, R.; et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N. Engl. J. Med. 2015, 372, 1996–2005. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, N.I.; Wolfe, R.E.; Moore, R.B.; Smith, E.; Burdick, E.; Bates, D.W. Mortality in Emergency Department Sepsis (MEDS) score: A prospectively derived and validated clinical prediction rule. Crit. Care Med. 2003, 31, 670–675. [Google Scholar] [CrossRef]
- Schellevis, F.G.; van der Velden, J.; van de Lisdonk, E.; van Eijk, J.T.; van Weel, C. Comorbidity of chronic diseases in general practice. J. Clin. Epidemiol. 1993, 46, 469–473. [Google Scholar] [CrossRef] [Green Version]
- McCabe, W.R. Gram-negative bacteremia. Adv. Intern. Med. 1974, 19, 135–158. [Google Scholar] [PubMed]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amodio-Groton, M.; Madu, A.; Madu, C.N.; Briceland, L.L.; Seligman, M.; McMaster, P.; Miller, M.H. Sequential parenteral and oral ciprofloxacin regimen versus parenteral therapy for bacteremia: A pharmacoeconomic analysis. Ann. Pharmacother. 1996, 30, 596–602. [Google Scholar] [CrossRef] [PubMed]
- MacGregor, R.R.; Graziani, A.L. Oral administration of antibiotics: A rational alternative to the parenteral route. Clin. Infect. Dis. 1997, 24, 457–467. [Google Scholar] [CrossRef] [Green Version]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonca, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Le Gall, J.R.; Lemeshow, S.; Saulnier, F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993, 270, 2957–2963. [Google Scholar] [CrossRef]
- Knaus, W.A.; Wagner, D.P.; Draper, E.A.; Zimmerman, J.E.; Bergner, M.; Bastos, P.G.; Sirio, C.A.; Murphy, D.J.; Lotring, T.; Damiano, A.; et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991, 100, 1619–1636. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.C.; Lin, W.L.; Lin, C.C.; Hsieh, W.H.; Hsieh, C.H.; Wu, M.H.; Wu, J.Y.; Lee, C.C. Outcome of inadequate empirical antibiotic therapy in emergency department patients with community-onset bloodstream infections. J. Antimicrob. Chemother. 2013, 68, 947–953. [Google Scholar] [CrossRef] [Green Version]
| Clinical Variables | Patients Number (%) | |||||
|---|---|---|---|---|---|---|
| Overall Cohort | Matched Cohort | |||||
| Early Switch N = 482 | Late/No Switch N = 6664 | p Value | Early Switch N = 482 | Late/No Switch N = 2410 | p Value | |
| Gender, male | 236 (49.0) | 3434 (51.5) | 0.28 | 236 (49.0) | 1174 (48.7) | 0.92 |
| Elderly, ≥65 years | 229 (47.5) | 4086 (61.3) | <0.001 | 229 (47.5) | 1198 (49.7) | 0.38 |
| Nursing-home residents | 8 (1.7) | 405 (6.1) | <0.001 | 8 (1.7) | 63 (2.6) | 0.22 |
| Inadequate source control during IV antimicrobial administration | 14 (2.9) | 226 (3.4) | 0.57 | 14 (2.9) | 49 (2.0) | 0.23 |
| Inappropriate empirical antimicrobial therapy | 82 (17.0) | 1290 (19.4) | 0.21 | 82 (17.0) | 414 (17.2) | 0.93 |
| Periods of antimicrobial administration, days, median (IQR) | ||||||
| IV (before IV-to-PO switch) | 0.9 (0.3–2.0) | 6 (6–16) | <0.001 | 0.9 (0.3–2.0) | 9 (6–14) | <0.001 |
| Total | 13.0 (10.5–14.3) | 10 (13–18) | <0.001 | 13.0 (10.5–14.3) | 13 (10–16) | 0.12 |
| Lengths of stay, median (IQR) | ||||||
| Emergency department, hours | 24.0 (7.3–52.8) | 16.0 (5.9–27.0) | <0.001 | 24.0 (7.3–52.8) | 15.7 (6.0–16.2) | <0.001 |
| Total hospitalisation, days | 1.0 (0.3–2.2) | 11 (7–19) | <0.001 | 1.0 (0.3–2.2) | 7 (10–16) | <0.001 |
| Polymicrobial bacteraemia | 36 (7.5) | 646 (9.7) | 0.11 | 36 (7.5) | 170 (7.1) | 0.75 |
| Complicated bacteraemia | 36 (7.5) | 1469 (22.0) | <0.001 | 36 (7.5) | 490 (20.3) | <0.001 |
| MEDS scores at bacteraemia onset | <0.001 | |||||
| High risk (≥13) | 30 (6.2) | 1596 (23.9) | 30 (6.2) | 155 (6.2) | 0.87 | |
| Low risk (<8) * | 358 (74.3) | 3062 (45.9) | 358 (74.3) | 1718 (71.3) | 0.18 | |
| Comorbidity severity (McCabe classification) | <0.001 | 0.06 | ||||
| Ultimately and rapidly fatal | 88 (18.3) | 1766 (26.5) | 88 (18.3) | 357 (14.8) | ||
| Nonfatal | 394 (81.7) | 4898 (73.5) | 394 (81.7) | |||
| Major comorbidities | ||||||
| Hypertension | 201 (41.7) | 3290 (49.4) | 0.001 | 201 (41.7) | 1121 (46.5) | 0.05 |
| Diabetes mellitus | 129 (26.8) | 2632 (39.5) | <0.001 | 129 (26.8) | 751 (31.2) | 0.07 |
| Malignancies | 108 (22.4) | 2107 (31.6) | <0.001 | 108 (22.4) | 553 (22.9) | 0.80 |
| Neurological diseases | 78 (16.2) | 1607 (24.1) | <0.001 | 78 (16.2) | 440 (18.3) | 0.28 |
| Chronic kidney diseases | 92 (19.1) | 1282 (19.2) | 0.94 | 92 (19.1) | 413 (17.1) | 0.30 |
| Liver cirrhosis | 48 (10.0) | 854 (12.8) | 0.07 | 48 (10.0) | 201 (8.3) | 0.25 |
| Coronary artery diseases | 43 (8.9) | 662 (9.9) | 0.47 | 43 (9.1) | 211 (8.8) | 0.91 |
| Urological disorders | 30 (6.2) | 520 (9.3) | 0.02 | 30 (6.2) | 210 (8.7) | 0.07 |
| Major sources of bacteraemia | ||||||
| Urinary tract | 192 (39.8) | 2267 (34.0) | 0.009 | 190 (39.4) | 921 (38.2) | 0.62 |
| Skin and soft-tissue infections | 72 (14.9) | 784 (11.8) | 0.04 | 72 (14.9) | 341 (14.1) | 0.65 |
| Intraabdominal | 58 (12.0) | 810 (12.2) | 0.94 | 58 (12.0) | 285 (11.8) | 0.90 |
| Pneumonia | 54 (11.2) | 985 (14.8) | 0.03 | 54 (11.2) | 233 (9.7) | 0.30 |
| Biliary tract | 25 (5.2) | 614 (9.2) | 0.003 | 25 (5.2) | 185 (7.7) | 0.06 |
| Liver abscess | 4 (0.8) | 270 (4.1) | <0.001 | 4 (0.8) | 32 (1.3) | 0.37 |
| Crude mortality rates after bacteraemia onset | ||||||
| 15-day | 12 (2.5) | 564 (8.5) | <0.001 | 12 (2.5) | 60 (2.5) | 1.00 |
| 30-day | 16 (3.3) | 830 (12.5) | <0.001 | 16 (3.3) | 111 (4.6) | 0.21 |
| Variables | Patient Number (%) | Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|---|---|
| Death, N = 846 | Survival, N = 6300 | OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Gender, male | 514 (60.8) | 3156 (50.1) | 1.54 (1.33–1.79) | <0.001 | NS | NS |
| Elderly | 551 (65.1) | 3764 (59.7) | 1.25 (1.08–1.46) | 0.003 | 1.31 (1.09–1.57) | 0.004 |
| Nursing-home residents | 108 (12.8) | 306 (4.9) | 2.87 (2.27–3.62) | <0.001 | 1.42 (1.07–1.89) | 0.02 |
| High risk patients (MEDS score ≥ 13) at bacteraemia onset | 610 (72.1) | 1016 (16.1) | 13.44 (10.40–15.85) | <0.001 | 9.60 (7.93–11.63) | <0.001 |
| Inadequate source control during IV antimicrobial administration | 56 (6.6) | 184 (2.9) | 2.36 (1.73–3.21) | <0.001 | 3.72 (2.54–5.44) | <0.001 |
| Inappropriate empirical antibiotic therapy | 212 (25.1) | 1160 (18.4) | 1.48 (1.25–1.75) | <0.001 | 1.97 (1.60–2.41 | <0.001 |
| Polymicrobial bacteraemia | 142 (16.8) | 540 (8.6) | 2.15 (1.76–2.63) | <0.001 | 1.62 (1.27–2.07) | <0.001 |
| Bacteraemia sources | ||||||
| Pneumonia | 341 (40.3) | 698 (11.1) | 5.42 (4.63–6.35) | <0.001 | 2.09 (1.67–2.63) | <0.001 |
| Intraabdominal | 134 (15.8) | 734 (11.7) | 1.43 (1.17–1.74) | <0.001 | 1.46 (1.11–1.91) | 0.006 |
| Urinary tract | 122 (14.4) | 2337 (37.1) | 0.29 (0.23–0.35) | <0.001 | 0.50 (0.39–0.64) | <0.001 |
| Biliary tract | 46 (5.4) | 593 (9.4) | 0.55 (0.41–0.75) | <0.001 | 0.66 (0.46 -1.01) | 0.06 |
| Liver abscess | 14 (1.7) | 260 (4.1) | 0.39 (0.23–0.67) | <0.001 | 0.40 (0.22–0.71) | 0.002 |
| Comorbidities | ||||||
| Malignancies | 441 (52.1) | 1774 (28.2) | 2.78 (2.40–3.21) | <0.001 | 2.02 (1.70–2.39) | <0.001 |
| Hypertension | 350 (41.4) | 3141 (49.9) | 0.71 (0.61–0.82) | <0.001 | NS | NS |
| Diabetes mellitus | 294 (34.8) | 2467 (39.2) | 0.83 (0.71–0.96) | 0.01 | NS | NS |
| Liver cirrhosis | 188 (22.2) | 714 (11.3) | 2.24 (1.87–2.68) | <0.001 | 1.32 (1.06–1.65) | 0.01 |
| Neurological diseases | 238 (28.1) | 1447 (23.0) | 1.31 (1.12–1.54) | 0.001 | NS | NS |
| Chronic kidney diseases | 184 (21.7) | 1190 (18.9) | 1.19 (1.00–1.42) | 0.047 | NS | NS |
| Variables | Patient Numbers (%) | p Values | |
|---|---|---|---|
| Early Switch N = 482 | Late/No Switch N = 2410 | ||
| Antimicrobial costs (US $), median (IQR) | |||
| IV | 6.1 (3.2–7.5) | 146.7 (44.2–300.0) | <0.001 |
| Oral | 12.6 (10.2–19.0) | 3.4 (2.1–4.8) | <0.001 |
| Total | 11.2 (8.6–36.8) | 153.8 (48.6–302.9) | <0.001 |
| Daily antimicrobial costs (US $), median (IQR) | 0.9 (0.6–2.9) | 11.8 (3.8–23.3) | <0.001 |
| Intolerability of antimicrobial therapy | |||
| Phlebitis | 4 (0.8) | 55 (2.3) | 0.04 |
| Gastrointestinal intolerance | 12 (2.5) | 26 (1.1) | 0.01 |
| Clinical failure rate within 30 days of IV-to-PO switch | |||
| Post-switch crude mortality | 16 (3.3) | 55 (2.3) | 0.18 |
| ED revisit | 14 (2.9) | 65 (2.7) | 0.80 |
| Re-hospitalisation | 10 (2.1) | 55 (2.3) | 0.78 |
| Re-initiation of IV antimicrobials | 12 (2.5) | 39 (1.6) | 0.19 |
| Variables | Patient Numbers (%) | Univariate Analyses | Multivariate Analyses | |||
|---|---|---|---|---|---|---|
| Death N = 16 | Survival N = 466 | OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Polymicrobial bacteraemia | 4 (25.0) | 32 (6.9) | 4.52 (1.38–14.82) | 0.03 | NS | NS |
| Inappropriate empirical antibiotic therapy | 8 (50.0) | 74 (15.9) | 5.30 (1.93–14.56) | 0.002 | 15.24 (3.45–67.32) | <0.001 |
| Inadequate source control during IV antimicrobial administration | 4 (25.0) | 10 (2.1) | 15.20 (4.17–55.41) | <0.001 | 73.15 (9.21–581.34) | <0.001 |
| Moderate- and high-risk patients (MEDS score ≥ 8) | 16 (100) | 108 (23.2) | – | <0.001 | NS | NS |
| Comorbidities | ||||||
| Neurological diseases | 8 (50.0) | 70 (14.0) | 5.66 (2.06–15.57) | 0.001 | 3.68 (0.90–17.62) | 0.07 |
| Chronic kidney diseases | 8 (50.0) | 84 (18.0) | 4.55 (1.66–12.45) | 0.004 | NS | NS |
| Bacteraemia sources | ||||||
| Pneumonia | 6 (37.5) | 48 (10.3) | 5.02 (1.82–15.01) | 0.005 | NS | NS |
| Urinary tract | 2 (12.5) | 190 (40.8) | 0.21 (0.05–0.92) | 0.02 | NS | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, C.-C.; Chen, P.-L.; Hsieh, C.-C.; Yang, C.-Y.; Lin, C.-H.; Ko, W.-C. Is Early Oral Antimicrobial Switch Useful for Less Critically Ill Adults with Community-Onset Bacteraemia in Emergency Departments? Antibiotics 2020, 9, 807. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9110807
Lee C-C, Chen P-L, Hsieh C-C, Yang C-Y, Lin C-H, Ko W-C. Is Early Oral Antimicrobial Switch Useful for Less Critically Ill Adults with Community-Onset Bacteraemia in Emergency Departments? Antibiotics. 2020; 9(11):807. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9110807
Chicago/Turabian StyleLee, Ching-Chi, Po-Lin Chen, Chih-Chia Hsieh, Chao-Yung Yang, Chih-Hao Lin, and Wen-Chien Ko. 2020. "Is Early Oral Antimicrobial Switch Useful for Less Critically Ill Adults with Community-Onset Bacteraemia in Emergency Departments?" Antibiotics 9, no. 11: 807. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9110807





