3. Discussion
With regard to our first research question of whether there were within individual changes in 3-T1AM and 3,5-T2 across the time points of the two studies, we did not identify such changes. This was true for both the healthy volunteers given a single dose of LT3 and the patients treated with daily LT3. The lack of trends over time in 3,5-T2 and 3-T1AM during the successive weeks, as LT4 therapy was replaced with LT3 therapy in the hypothyroid patients, suggests that 3,5-T2 and 3-T1AM, regardless of the source of T3 (direct or from LT4) and the varied amount of residual thyroid function as a source of T4 in the participants, is protected and maintained relatively constant. This was true not only for the weekly trough levels, which might be expected to be more constant, but even acutely during hourly sampling after LT3 administration. These data do not provide support for the suggestion that 3,5-T2 is produced from exogenous T3. However, these data suggest that 3,5-T2 and 3-T1AM levels are defended within particular limits.
Our second research question probed relationships between 3,5-T2 and 3-T1AM and queried whether there were paired, linked or reciprocal changes. No relationship was observed between 3,5-T2 and 3-T1AM levels during the weekly sampling in the hypothyroid patients, suggesting the tight regulation of metabolites. However, during the dynamic sampling after the administration of the last LT3 dose, there was a positive correlation between 3,5-T2 and 3-T1AM which could suggest that 3-T1AM production is via 3,5-T2. Acutely after the T3 rise, it could be hypothesized that 3,5-T2 levels rose and resulted in higher 3-T1AM concentrations. However, such a hypothesis does not explain why higher T3 levels were associated with lower 3-T1AM levels unless T3 negatively regulated 3-T1AM production from 3,5-T2.
We also queried whether there were changes in 3,5-T2 or 3-T1AM that were related to or linked to the corresponding T4, T3, FT4, FT3 and TSH values. The fact that no acute changes in 3,5-T2 or 3-T1AM were observed after exogenous LT3 administration in individuals with intact thyroid function, despite the fact that their mean T3 concentrations rose from 120 ng/dL to 346 ng/dL, either suggests that these metabolites are not produced via exogenous T3 or that metabolite concentrations are tightly and rapidly regulated. The lack of relationships between TH concentrations and TH metabolites concentrations in these same individuals with native thyroid function also suggests rapid autoregulation in individuals with normal endogenous thyroid function. Some possible hypotheses for the stability of 3,5-T2 or 3-T1AM might include tight binding to ApoB100. The possibility that 3-T1AM might be tightly bound to ApoB100 has been suggested previously [
11], but there are no comparable data on 3,5-T2. Both 3,5-T2 and 3-T1AM might be preferably intracellularly generated and localized in specific tissues (such as the liver), with these metabolites then slowly “leaking” from such sites into the circulation.
During the weekly steady state sampling in the hypothyroid patients, a positive correlation between both T4 and free T4 levels and 3,5-T2 concentrations was observed, which could suggest that 3,5-T2 is produced from T4. Other studies have suggested extra-thyroidal production of TH metabolites from exogenous LT4 in athyreotic individuals [
6,
7,
8]. However, the hypothyroid patients in our second study retained at least some degree of residual endogenous thyroid function and were exclusively receiving LT3. They would have had some remaining T4 from exogenous LT4 at the beginning of the study, which then declined, so that by the end of the study any T4 would be from endogenous sources. This could raise the possibility that 3,5-T2 can also be made from endogenous T4, but does not support the concept of 3,5-T2 production from exogenous T3.
Our final research question was whether 3,5-T2 or 3-T1AM values, or changes in 3,5-T2 and 3-T1AM values, were related to age, sex, or other characteristics such as BMI. We did not find any relationships between these characteristics and TH metabolites, with one exception. Our finding of a sex difference in 3-T1AM concentrations in those with endogenous normal thyroid function is a novel finding that has yet to be confirmed. Given the small number of individuals studied, this may not be a true finding. If it is confirmed in future adequately powered studies that TIAM levels are indeed higher in women, this could potentially be due to higher thyroxine-binding globulin levels in women, direct stimulation from sex-specific steroid hormones or other unknown factors. However, no sex difference in 3-T1AM levels was observed in the treated hypothyroid patients in the study, and, admittedly, this theory does not explain why these findings were not also seen in women being treated for hypothyroidism.
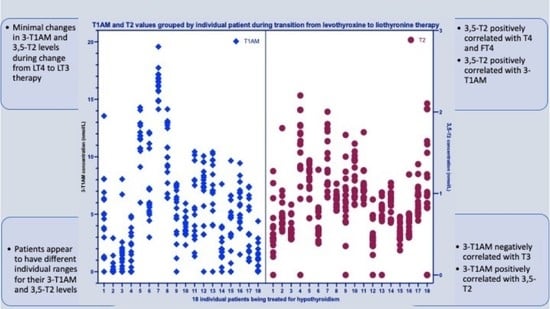
However, interestingly, we did find that both healthy volunteers and hypothyroid patients seemed to have personal ranges for 3,5-T2 and 3-T1AM. The distribution of the data points for 3,5-T2 and 3-T1AM from individuals with intact thyroid function suggests that there is a distinct setpoint for these metabolites for each individual participant that is composed of closely grouped values and is not subject to perturbations caused by exogenous LT3. Similar individual setpoints have been observed for TSH, T4 and T3 [
12,
13]. These setpoints also seem to extend to LT4-treated patients [
14,
15,
16]. As was the case in the euthyroid individuals, the data from the individuals with treated hypothyroidism also suggested characteristic individual setpoints for TH metabolites.
There is a rich literature describing patient dissatisfaction with LT4 therapy [
17,
18] and patient preferences for synthetic combination therapy and desiccated thyroid extract [
1,
19,
20]. There has been speculation that the levels of TH metabolites achieved during LT4 monotherapy may provide some underpinning for this dissatisfaction [
2,
8]. Our data do not support this theory as TH metabolites did not appear to change during the transition from LT4 to LT3. In addition, our study was uncontrolled and so could not assess satisfaction with therapy during the transition. A prior study of TH metabolites has also reported that there was no association between 3,5-T2 concentrations and quality of life in patients with thyroid cancer who were receiving LT4 replacement [
21].
The strengths of our studies are that we are able to provide some data from volunteers and patients with normal and partial endogenous thyroid function, respectively, receiving LT3, thus potentially complementing data regarding athyreotic LT4-treated patients already reported in the literature [
6,
7,
8]. We were also able to measure not only 3,5-T2 concentrations, but 3-T1AM concentrations too, which have not been included in recent studies utilizing tandem mass spectrometry [
8]. The limitations of our study are numerous. Foremost, we did not utilize the very specific tandem mass spectrometry methodology for measuring TH metabolites. Our samples had been stored for several years prior to their use for this secondary analysis. However, the samples were appropriately stored in a −80° centigrade freezer with continuous monitoring, thus ensuring sample quality. There were no intervening episodes of thawing prior to use. Additionally, our participant numbers were very small and this was a secondary analysis of two prior studies with different designs performed for other purposes. Due to the multiple comparisons in the studies, the authors cannot exclude the possibility of multiple testing bias. The sex and age composition of the participants in the two studies differed. In addition, the inclusion of individuals with varying degrees of endogenous thyroid function (full endogenous function in study one and variable degrees of residual function in study two) added complexity to separating the influences of endogenous versus exogeneous sources of T4. An additional layer of complexity was that the hypothyroid participants in study two were being transitioned off LT4 therapy to LT3 therapy. Although the limitations of this secondary analysis make hypothesis testing challenging, these data may be useful for generating hypotheses to test in future studies.
There are currently challenges and controversies in the field of clinical chemistry regarding the measurement of the serum concentrations of 3,5-T2 and 3-T1AM [
22,
23]. There are differences within the groups who have developed mass spectrometry assays [
22] and immunoassay-based data do not correlate with mass spectrometry data. For example, 3,5-T2 is below the limit of detection using mass spectrometry assays [
8,
24], compared with levels of 0.253 ± 0.029 nmol/L detected in healthy individuals using immunoassay [
6]. Another mass spectrometry method found average 3,5-T2 concentration of 78 ± 9 pmol/L in euthyroid individuals [
25]. Such differences are presumably due to various methodologic and technologic considerations, including those pertaining to internal standards. Some mass spectrometry assays have not detected 3-T1AM [
8,
22]. In one case due to sample preparation being selective for negatively charged ions, as opposed to positively charged ones as would be present in 3-T1AM [
8]. Comparing studies reporting the measurement of 3-T1AM in human samples, these studies reported average concentrations varying between 0.219 nmol/L measured by mass spectrometry [
26] and 14–66 nmol/L measured by immunoassay [
7,
27]. Determination of TH metabolites from human samples simultaneously measured by immunoassay and tandem mass spectrometry would be helpful.
To summarize our findings, the positive correlations between weekly trough levels of 3,5-T2 and both T4 and FT4 during T3 therapy and their significance with respect to 3,5-T2 production is unclear. However, this finding may possibly suggest some production of 3,5-T2 from endogenous T4, but not from exogenous T3. In the acute hourly sampling immediately after T3 administration the negative correlation between T3 levels and 3-T1AM, but positive correlation between 3,5-T2 and 3-T1AM could lead to speculation that 3-T1AM production is from 3,5-T2 with negative regulation by T3. However, more studies are needed both to elaborate the pathways for TH metabolite production in the native euthyroid versus the hypothyroid LT3-replaced state versus the hypothyroid LT4-replaced state, and to clarify the pathways for 3-T1AM production. During LT3 treatment, both endogenous euthyroid volunteers and hypothyroid patients seem to maintain individual setpoints for their TH metabolite concentration.
4. Materials and Methods
This report involves a secondary analysis of additional laboratory testing performed on stored samples from two prior studies [
9,
10]. Participants in both studies provided written informed consent, which included permission for future testing of stored samples. TH metabolite measurement was not pre-planned at the time of the initial studies and a formal power analysis was not performed. The research questions considered in these analyses were: (a) are there within individual changes in 3-T1AM and 3,5-T2 across the time points of the 2 studies, (b) are there relationships between any 3,5-T2 and 3-T1AM changes (paired, linked or reciprocal changes, etc.), (c) are there changes in 3,5-T2 or 3-T1AM that are related to or linked to the corresponding T4, T3, FT4, FT3 and TSH values and (d) are the 3,5-T2 or 3-T1AM values, or changes in 3,5-T2 and 3-T1AM values, related to individual age, sex or other characteristics?
The first study involved healthy volunteers with normal thyroid function who were given a single dose of 50 mcg LT3. The trial was approved by the Institutional Review Board and registered at
ClinicalTrials.gov as clinical trial NCT01581463 (Detailed description provided in [
9]). Volunteers aged 18–55 years without thyroid disease were recruited and screened by telephone for any conditions or medications known to affect thyroid hormone (TH) metabolism, absorption or binding. Potentially eligible participants were scheduled for an in-person visit to the Georgetown University Clinical Research Unit (GCRU) and signed a written consent form for the study. A medical history, physical examination, electrocardiogram and screening TSH were then obtained. Participants in good health and with a TSH value within the reference range (0.4–4.5 mIU/L) were then scheduled for pharmacokinetic testing. Testing commenced at 7:30 am after an overnight fast. The 50 mcg LT3 dose was administered at 8:00 am. Blood samples were collected at 15 min interval for 4 samples, then at 30 min intervals for 6 samples, hourly for 2 samples and then at 6, 8, 12, 24, 48, 72 and 96 h after LT3 administration. Samples were initially assayed for TSH, T4, FT4, T3 and FT3 at the Georgetown University Laboratory in one batch for each participant using a Siemens Dimension Vista Analyzer [
9]. Later, all samples for all participants were measured for 3,5-T2 and 3-T1AM in 2017 at Charité–Universitätsmedizin Berlin [
2].
The second group was composed of patients with hypothyroidism in whom their usual LT4 treatment was replaced with daily LT3 for 6 weeks. This study was approved by the Institutional Review Board and registered at
ClinicalTrials.gov as clinical trial NCT01800617 (Detailed description provided in [
10]). Briefly, participants aged 18–65 years with hypothyroidism of any etiology and taking at least 75 mcg LT4 daily were recruited and screened by telephone to exclude individuals with any significant medical conditions and any conditions or medications known to affect TH metabolism, absorption or binding. Potentially eligible participants were seen on the GCRU where they signed a written informed consent form and underwent a medical history, physical examination, electrocardiogram and screening TSH measurement. Participants with hypothyroidism and otherwise in good health and with a TSH within the reference range (0.4–4.5 mIU/L) while taking LT4 were then studied for 6 weeks. At the initial visit the participant was asked to present after discontinuing their LT4 therapy (last dose of LT4 taken the day prior), baseline pre-LT3 dose (trough) measurements of TSH, T4, FT4, T3 and FT3 were obtained, and the patient was started on 15 mcg LT3 once daily. A week later, a second set of trough (pre-LT3 dose) thyroid function tests was obtained and the participant continued on 15 mcg LT3 daily. The following week after the trough thyroid function tests were obtained the participants were switched to either 30 mcg or 45 mcg LT3 based on their pre-study dose of LT4. There were then 4 subsequent visits at which trough levels of TSH, T4, FT4, T3 and FT3 were obtained. At the time of the seventh and final study visit, following the baseline thyroid function tests, the participants took their final LT3 dose of the study and thyroid function tests were repeated at 30 min and then hourly for eight hours in an abbreviated pharmacokinetic study. All samples were assayed at the Georgetown University Laboratory using a Siemens Dimension Vista Analyzer on the day they were obtained for LT3 dose adjustment and safety monitoring [
10].
Samples from both studies were later analyzed for TH metabolites (3,5-T2 and 3-T1AM) in 2017 at Charité–Universitätsmedizin Berlin. The samples from both studies were pooled together and placed in a randomized order prior to analysis to avoid between-run bias. The detailed assay methodology using a monoclonal antibody-based chemiluminescence immunoassay has been previously described [
2,
6,
7] and preliminary analysis of the 3,5-T2 and 3-T1AM concentrations from these cohorts has also been described [
2].
Statistical Methods
Continuous variables were time in hours or time in weeks. A linear regression model was fit to the data to measure the change in 3-T1AM and 3,5-T2 concentrations over time by calculating the slope of a line. Considering the repeated measures within individuals, linear regression was fit using a repeated measures model with autoregressive covariance structure. During the first study, measurements were collected at shorter intervals during the first 5 h and at larger intervals during later hours, hence analysis was conducted over all 96 h as well as for the subset of measurements during the first 5 h.
Correlation between 3-T1AM and 3,5-T2 concentrations was tested using a linear regression model with repeated measures and autoregressive covariance structures. 3-T1AM was considered as a dependent variable and 3,5-T2 as an independent variable. The model also adjusted for time as a continuous variable. An additional model was constructed to include interaction between time and 3,5-T2 to test the change in correlation between 3-T1AM and 3,5-T2 over time. Similarly, the relationship between 3-T1AM or 3,5-T2 with T4, T3, FT3, FT4, TSH and individual characteristics such as age and sex was tested using a linear regression model with repeated measures and autoregressive covariance structure controlling for time as a continuous variable. Analysis was conducted using SAS 9.4. Statistical analysis did not utilize listwise deletion. Missing data were addressed using the “Proc Mixed” procedure in SAS. This analyzes all of the data that are present with the assumption that the data are missing at random.