Pelvic Fixation Technique Using the Ilio-Sacral Screw for 173 Neuromuscular Scoliosis Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Operative Techniques
2.3. Outcomes Assessment
2.4. Statistics
3. Results
3.1. Demographic Data
3.2. Radiological Data
3.3. Complications
3.4. Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thometz, J.G.; Simon, S.R. Progression of scoliosis after skeletal maturity in institutionalized adults who have cerebral palsy. J. Bone Jt. Surg. Am. 1988, 70, 1290–1296. [Google Scholar] [CrossRef]
- Yen, W.; Gartenberg, A.; Cho, W. Pelvic obliquity associated with neuromuscular scoliosis in cerebral palsy: Cause and treatment. Spine Deform. 2021, 9, 1259–1265. [Google Scholar] [CrossRef] [PubMed]
- Hasler, C.; Brunner, R. Spine deformities in patients with cerebral palsy; the role of the pelvis. J. Child. Orthop. 2020, 14, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Saito, N.; Ebara, S.; Ohotsuka, K.; Kumeta, H.; Takaoka, K. Natural history of scoliosis in spastic cerebral palsy. Lancet 1998, 351, 1687–1692. [Google Scholar] [CrossRef]
- Olafsson, Y.; Saraste, H.; Al-Dabbagh, Z. Brace treatment in neuromuscular spine deformity. J. Pediatr. Orthop. 1999, 19, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, C.; Burton, D.C.; Asher, M. Treatment of selected neuromuscular patients with posterior instrumentation and arthrodesis ending with lumbar pedicle screw anchorage. Spine 2000, 25, 2312–2318. [Google Scholar] [CrossRef]
- Lubicky, J.P.; McCarthy, R.E. Sacral pelvic fixation in neuromuscular deformities. Semin. Spine Surg. 2004, 16, 126–133. [Google Scholar] [CrossRef]
- Miladi, L.; Gaume, M.; Khouri, N.; Johnson, M.; Topouchian, V.; Glorion, C. Minimally invasive surgery for neuromuscular scoliosis: Results and complications in a series of one hundred patients. Spine 2018, 43, E968–E975. [Google Scholar] [CrossRef]
- Dimeglio, A.; Canavese, F. The immature spine: Growth and idiopathic scoliosis. Ann. Transl. Med. 2020, 8, 22. [Google Scholar] [CrossRef]
- Gaume, M.; Langlais, T.; Loiselet, K.; Pannier, S.; Skalli, W.; Vergari, C.; Miladi, L. Spontaneous induced bone fusion in minimally invasive fusionless bipolar fixation in neuromuscular scoliosis: A computed tomography analysis. Eur. Spine J. 2023, 32, 2550–2557. [Google Scholar] [CrossRef]
- Modi, H.N.; Suh, S.W.; Song, H.-R.; Yang, J.H.; Jajodia, N. Evaluation of pelvic fixation in neuromuscular scoliosis: A retrospective study in 55 patients. Int. Orthop. 2010, 34, 89–96. [Google Scholar] [CrossRef]
- Moon, E.S.; Nanda, A.; Park, J.O.; Moon, S.H.; Lee, H.M.; Kim, J.Y.; Yoon, S.P.; Kim, H.S. Pelvic Obliquity in Neuromuscular Scoliosis Radiologic Comparative Results of Single-Stage Posterior Versus Two-Stage Anterior and Posterior Approach. Spine 2011, 36, 146–152. [Google Scholar] [CrossRef]
- Shabtai, L.; Andras, L.M.; Portman, M.; Harris, L.R.; Choi, P.D.; Tolo, V.T.; Skaggs, D.L. Sacral alar iliac (sacral alar iliac) screws fail 75% less frequently than iliac screws in neuromuscular scoliosis. J. Pediatr. Orthop. 2017, 37, e470–e475. [Google Scholar] [CrossRef]
- Peelle, M.W.; Lenke, L.G.; Bridwell, K.H.; Sides, B. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine 2006, 31, 2392–2398. [Google Scholar] [CrossRef] [PubMed]
- Anari, J.B.; Spiegel, D.A.; Baldwin, K.D. Neuromuscular scoliosis and pelvic fixation in 2015: Where do we stand? World J. Orthop. 2015, 6, 564–566. [Google Scholar] [CrossRef] [PubMed]
- Cotrel, Y.; Dubousset, J.; Guillaumat, M. New universal instrumentation in spinal surgery. Clin. Orthop. Relat. Res. 1988, 227, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Miladi, L.T.; Ghanem, I.B.; Draoui, M.M.; Zeller, R.D.; Dubousset, J.F. Iliosacral screw fixation for pelvic obliquity in neuromuscular scoliosis. A long-term follow-up study. Spine 1997, 22, 1722–1729. [Google Scholar] [CrossRef] [PubMed]
- Zahi, R.; Vialle, R.; Abelin, K.; Mary, P.; Khouri, N.; Damsin, J.-P. Spinopelvic fixation with iliosacral screws in neuromuscular spinal deformities: Results in a prospective cohort of 62 patients. Childs Nerv. Syst. 2010, 26, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Neustadt, J.B.; Shufflebarger, H.L.; Cammisa, F.P. Spinal fusions to the pelvis augmented by Cotrel-Dubousset instrumentation for neuromuscular scoliosis. J. Pediatr. Orthop. 1992, 12, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.C.; Wijesekera, S.; Sossan, A.D.; Martin, L.; Vogel, L.C.; Boakes, J.L.; Lerman, J.A.; McDonald, C.M.; Betz, R.R. Reliability of radiographic parameters in neuromuscular scoliosis. Spine 2007, 32, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Osebold, W.R.; Mayfield, J.K.; Winter, R.B.; Moe, J.H. Surgical treatment of paralytic scoliosis associated with myelomeningocele. J. Bone Jt. Surg Am. 1982, 64, 841–856. [Google Scholar] [CrossRef]
- Gaume, M.; Vergari, C.; Khouri, N.; Skalli, W.; Glorion, C.; Miladi, L. Minimally Invasive Surgery for Neuromuscular Scoliosis: Results and Complications at a Minimal Follow-up of 5 Years. Spine 2021, 46, 1696–1704. [Google Scholar] [CrossRef]
- Edwards, B.T.; Zura, R.; Bertrand, S.; Leonard, S.; Pellett, J. Treatment of neuromuscular scoliosis with posterior spinal fusion using the Galveston technique: A retrospective review and results of 62 patients. J. Long Term. Eff. Med. Implant. 2003, 13, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Benson, E.R.; Thomson, J.D.; Smith, B.G.; Banta, J.V. Results and morbidity in a consecutive series of patients undergoing spinal fusion for neuromuscular scoliosis. Spine 1988, 23, 2308–2317, discussion 2318. [Google Scholar] [CrossRef] [PubMed]
- Teli, M.; Elsebaie, H.; Biant, L.; Noordeen, H. Neuromuscular scoliosis treated by segmental third-generation instrumented spinal fusion. J. Spinal. Disord. Tech. 2005, 18, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Wolff, S.; Moreau, P.E.; Miladi, L.; Riouallon, G. Is minimally invasive bipolar technique a better alternative to long fusion for adult neuromuscular scoliosis? Global. Spine J. 2023, 21925682231159347. [Google Scholar] [CrossRef]
- Jain, A.; Sullivan, B.T.; Kuwabara, A.; Kebaish, K.M.; Sponseller, P.D. Sacral-alar-iliac fixation in children with neuromuscular scoliosis: Minimum 5-year follow-up. World Neurosurg. 2017, 108, 474–478. [Google Scholar] [CrossRef]
- Sponseller, P.D.; Zimmerman, R.M.; Ko, P.S.; Gunne, A.F.P.T.; Mohamed, A.S.; Chang, T.-L.; Kebaish, K.M. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine 2010, 35, 1887–1889. [Google Scholar] [CrossRef]
- Aleissa, S.; Parsons, D.; Grant, J.; Harder, J.; Howard, J. Deep wound infection following pediatric scoliosis surgery: Incidence and analysis of risk factors. Can. J. Surg. 2011, 54, 263–269. [Google Scholar] [CrossRef]
- Cahill, P.J.; Warnick, D.E.; Lee, M.J.; Gaughan, J.; Vogel, L.E.; Hammerberg, K.W.; Sturm, P.F. Infection afer spinal fusion for pediatric spinal deformity: Tirty years of experience at a single institution. Spine 2010, 35, 1211–1217. [Google Scholar] [CrossRef]
- Bouyer, B.; Bachy, M.; Zahi, R.; Thévenin-Lemoine, C.; Mary, P.; Vialle, R. Correction of pelvic obliquity in neuromuscular spinal deformities using the “T construct”: Results and complications in a prospective series of 60 patients. Eur. Spine J. 2014, 23, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Ramo, B.A.; Roberts, D.W.; Tuason, D.; McClung, A.; Paraison, L.E.; Moore IV, H.G.; Sucato, D.J. Surgical site infections after posterior spinal fusion for neuromuscular scoliosis: A thirty year experience at a single institution. J. Bone Jt. Surg. Am. 2014, 96, 2038–2048. [Google Scholar] [CrossRef] [PubMed]
- Sponseller, P.D.; LaPorte, D.M.; Hungerford, M.W.; Eck, K.; Bridwell, K.H.; Lenke, L.G. Deep wound infections after neuromuscular scoliosis surgery: A multicenter study of risk factors and treatment outcomes. Spine 2000, 25, 2461–2466. [Google Scholar] [CrossRef] [PubMed]
- Weissmann, K.A.; Weissmann, K.A.; Lafage, V.; Lafage, V.; Pitaque, C.B.; Pitaque, C.B.; Lafage, R.; Lafage, R.; Huaiquilaf, C.M.; Huaiquilaf, C.M.; et al. Neuromuscular scoliosis: Comorbidities and complications. Asian Spine J. 2021, 15, 778–790. [Google Scholar] [CrossRef] [PubMed]
- Gaume, M.; Hajj, R.; Khouri, N.; Johnson, M.; Miladi, L. One-Way Self-Expanding Rod in Neuromuscular Scoliosis: Preliminary Results of a Prospective Series of 21 Patients. JBJS Open Access 2021, 6, e21.00089. [Google Scholar] [CrossRef]
- Ilyas, H.; Place, H.; Puryear, A. A comparison of early clinical and radiographic complications of iliac screw fixation versus S2 alar iliac (S2AI) fixation in the adult and pediatric populations. J. Spinal. Disord. Tech. 2015, 28, E199–E205. [Google Scholar] [CrossRef]
- Ravindra, V.M.; Mazur, M.D.; Brockmeyer, D.L.; Kraus, K.L.; Ropper, A.E.; Hanson, D.S.; Dahl, B.T. Clinical Effectiveness of S2-Alar Iliac Screws in Spinopelvic Fixation in Pediatric Neuromuscular Scoliosis: Systematic Literature Review. Global. Spine J. 2020, 10, 1066–1074. [Google Scholar] [CrossRef]
- Shillingford, J.N.; Laratta, J.L.; Tan, L.A.; Sarpong, N.O.; Lin, J.D.; Fischer, C.R.; Lehman, R.A.; Kim, Y.J.; Lenke, L.G. The free-hand technique for s2-alar-iliac screw placement: A safe and effective method for sacropelvic fixation in adult spinal deformity. J. Bone Jt. Surg. Am. 2018, 100, 334–342. [Google Scholar] [CrossRef]
- Hassan, S.K.; Simon, L.; Campana, M.; Julien-Marsollier, F.; Simon, A.-L.; Ilharreborde, B. S2-Alar-iliac screw fixation for paediatric neuromuscular scoliosis: Preliminary results after two years. Orthop. Traumatol. Surg. Res. 2022, 108, 103234. [Google Scholar] [CrossRef]
- Gaume, M.; Triki, M.A.; Glorion, C.; Breton, S.; Miladi, L. Optimal ilio-sacral screw trajectory in paediatric patients: A computed tomography study. Acta Orthop. Belg. 2021, 87, 285–291. [Google Scholar] [CrossRef]
- Azad, T.D.; Warman, A.; Tracz, J.A.; Hughes, L.P.; Judy, B.F.; Witham, T.F. Augmented reality in spine surgery—Past, present, and future. Spine J. 2024, 24, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Asada, T.; Simon, C.Z.; Lu, A.Z.; Adida, S.; Dupont, M.; Parel, P.M.; Zhang, J.; Bhargava, S.; Morse, K.W.; Dowdell, J.E.; et al. Robot-navigated pedicle screw insertion can reduce intraoperative blood loss and length of hospital stay: Analysis of 1633 patients utilizing propensity score matching. Spine J. 2024, 24, 118–124. [Google Scholar] [CrossRef]
- Yamout, T.; Orosz, L.D.; Good, C.R.; Jazini, E.; Allen, B.; Gum, J.L. Technological Advances in Spine Surgery: Navigation, Robotics, and Augmented Reality. Orthop. Clin. N. Am. 2023, 54, 237–246. [Google Scholar] [CrossRef]
- Moreau, M.; Mahood, J.; Moreau, K.; Berg, D.; Hill, D.; Raso, J. Assessing the impact of pelvic obliquity in postoperative neuromuscular scoliosis. Stud. Health Technol. Inf. 2002, 91, 481–485. [Google Scholar]
- Drake, L.; Sukkarieh, H.; McDonald, T.; Bhanat, E.; Quince, E.; Atkins, M.; Wright, P.; Brooks, J. Effect of pelvic fixation on ambulation in children with neuromuscular scoliosis. World J. Orthop. 2022, 13, 753–759. [Google Scholar] [CrossRef] [PubMed]





| PSF | MIFS | PSF and MIFS | p | |
|---|---|---|---|---|
| Patients, n | 62 | 111 | 173 | |
| Mean age, years | 15 (12 to 19) | 12 (6 to 19) | 13.7 (6 to 19) | |
| Etiology | ||||
| Muscular dystrophy, n | 4 (6.5%) | 10 | 14 | 0.0554 |
| Cerebral palsy, n | 42 (67.7%) | 71 | 102 | 0.617 |
| Flaccid Paraplegia, n | 7 (11.3%) | 4 | 11 | 0.057 |
| Spinal muscular atrophy, n | 6 (9.7%) | 13 | 19 | 0.681 |
| Rett syndrom, n | 2 (3.2%) | 5 | 7 | 1 |
| Myelomeningocele | 1 (1.6%) | 8 | 9 | 0.159 |
| Infections, n | 13 (21%) | 16 (14.4%) | 29 (16.7%) | 0.02 * |
| Local debridment and antibiotics, n | 12 | 14 | 26 | |
| Hardware removal, n | 1 | 2 | 3 | |
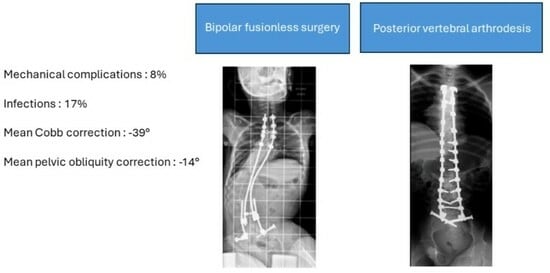
| Mechanical complications, n | 5 (8.1%) | 9 (8.1%) | 14 (8%) | 0.091 |
| Early mobilization of S1 screw, n | 5 | 1 | 6 | |
| S1 root irritation, n | 0 | 6 | 6 | |
| Connector failure, n | 0 | 1 | 1 | |
| Ilio-sacral screw skin prominence, n | 0 | 1 | 1 | |
| Preoperative pelvic obliquity, (°), mean | 23 | 23 | 23 | |
| Last FU pelvic obliquity improvement (°), mean | −10.2 (44%) | −17.8 (77%) | −14 | |
| Preoperative Cobb angle, (°), mean | 50.5 | 77 | 63.8 | |
| Last FU Cobb correction improvement, (°), mean | −31.1 (61%) | −47.8 (62%) | −39.5 | |
| Loss of frontal or sagittal correction | None | None | None | |
| Sitting posture and comfort improvement | All cases | All cases | All cases |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaumé, M.; Saghbiny, E.; Richard, L.; Thouement, C.; Vialle, R.; Miladi, L. Pelvic Fixation Technique Using the Ilio-Sacral Screw for 173 Neuromuscular Scoliosis Patients. Children 2024, 11, 199. https://0-doi-org.brum.beds.ac.uk/10.3390/children11020199
Gaumé M, Saghbiny E, Richard L, Thouement C, Vialle R, Miladi L. Pelvic Fixation Technique Using the Ilio-Sacral Screw for 173 Neuromuscular Scoliosis Patients. Children. 2024; 11(2):199. https://0-doi-org.brum.beds.ac.uk/10.3390/children11020199
Chicago/Turabian StyleGaumé, Mathilde, Elie Saghbiny, Lou Richard, Clélia Thouement, Raphaël Vialle, and Lotfi Miladi. 2024. "Pelvic Fixation Technique Using the Ilio-Sacral Screw for 173 Neuromuscular Scoliosis Patients" Children 11, no. 2: 199. https://0-doi-org.brum.beds.ac.uk/10.3390/children11020199