Complementary and Integrative Management of Pediatric Lower Urinary Tract Dysfunction Implemented within an Interprofessional Clinic
Abstract
:1. Background
2. Complementary and Integrative Interventions for Children with LUTD
2.1. Urology Interventions
2.2. The Importance of the Pelvic Floor
2.3. Gastroenterology Interventions
2.4. Behavioral Interventions
3. An Interprofessional Integrative Clinic Model
4. Patient Examples
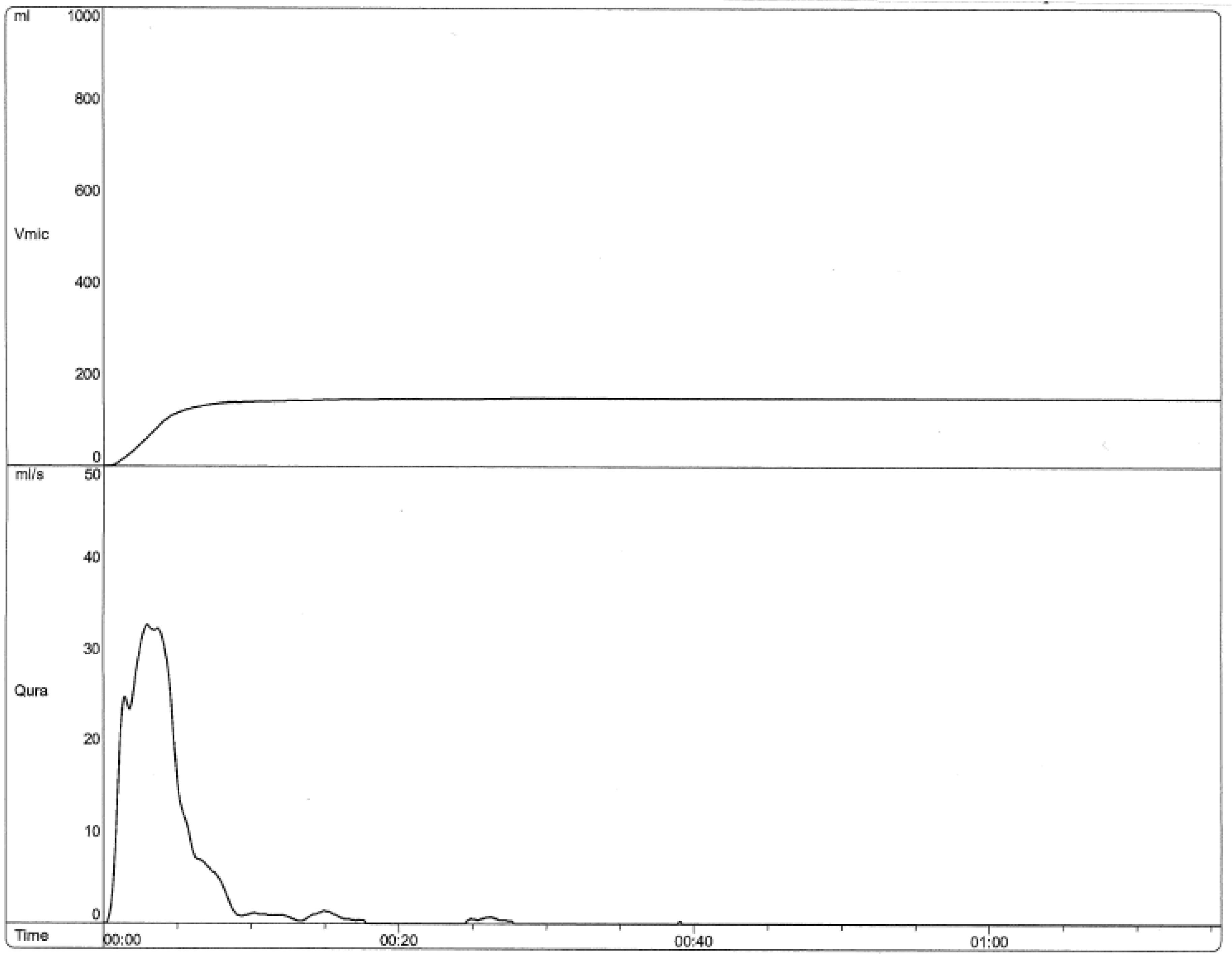
4.1. Example 1—Pelvic Floor Physical Therapy
4.2. Example 2—Pelvic Floor Physical Therapy
4.3. Example 3—Behavioral Interventions
4.4. Example 4—Behavioral Interventions
5. Conclusions
Future Directions
Author Contributions
Conflicts of Interest
References
- National Center for Complementary and Integrative Health. Complementary, Alternative, or Integrative Health: What’s in a Name? Available online: https://nccih.nih.gov/health/integrative-health (accessed on 25 May 2019).
- Austin, F.P.; Bauer, S.B.; Bower, W.; Chase, J.; Franco, I.; Hoebeke, P.; Rittig, S.; Walle, J.V.; von Gontard, A.; Wright, A.; et al. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the Standardization Committee of the International Children’s Continence Society. J. Urol. 2014, 191, 1863–1865. [Google Scholar] [CrossRef] [PubMed]
- Nordenström, J.; Sillen, U.; Holmdahl, G.; Linnér, T.; Stokland, E.; Sjöström, S. The Swedish Infant High-grade Reflux Trial–Bladder function. J. Pediatr. Urol. 2017, 13, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Bergers, E.R.; Mugie, S.M.; Chase, J.; Cooper, C.S.; von Gontard, A.; Rittig, C.S.; Homsy, Y.; Bauer, S.B.; Benninga, M.A. Management of functional constipation in children with lower urinary tract symptoms: Report from the Standardization Committee of the International Children’s Continence Society. J. Urol. 2013, 190, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Collis, D.; Kennedy-Behr, A.; Kearney, L. The impact of bowel and bladder problems on children’s quality of life and their parents: A scoping review. Child Care Health Dev. 2019, 45, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Marciano, R.C.; Cardoso, M.G.F.; Vasconcelos, J.J.; Paula, N.C.; Pinho, A.C.; Oliveira, E.A.; Lima, E.M. Behavioral disorders and impairment of quality of life in children and adolescents with lower urinary tract dysfunction. J. Pediatr. Urol. 2018, 14, 568-e1–568-e7. [Google Scholar] [CrossRef]
- Anderson, E.G.; Jimerson, S.R.; Whipple, D.A. Student ratings of stressful experiences at home and school: Loss of a parent and grade retention as superlative stressors. J. Appl. Sch. Psychol. 2005, 21, 1–20. [Google Scholar] [CrossRef]
- Ollendick, H.T.; King, N.J.; Frary, R.B. Fears in children and adolescents: Reliability and generalizability across gender, age and nationality. Behav. Res. Ther. 1989, 27, 19–26. [Google Scholar] [CrossRef]
- Youssef, N.N.; Langseder, L.A.; Verga, J.B.; Mones, L.R.; Rosh, R.J. Chronic childhood constipation is associated with impaired quality of life: A case-controlled study. J. Pediatr. Gastroenterol. Nutr. 2005, 41, 56–60. [Google Scholar] [CrossRef]
- von Gontard, A.; Baeyens, D.; van Hoecke, E.; Warzak, W.J.; Bachmann, C. Psychological and psychiatric issues in urinary and fecal incontinence. J. Urol. 2011, 185, 1432–1437. [Google Scholar] [CrossRef] [PubMed]
- Campbell, L.K.; Cox, D.J.; Borowitz, S.M. Elimination disorders: Enuresis and encopresis. In Handbook of Pediatric Psychology; Roberts, M., Ed.; The Guilford Press: New York, NY, USA, 2009; pp. 481–490. [Google Scholar]
- Shepard, J.A.; Cox, D.J. Elimination Disorders. In Handbook of Pediatric Psychology; Roberts, M., Ed.; The Guilford Press: New York, NY, USA, 2017; pp. 442–451. [Google Scholar]
- McKeown, C.; Hisle-Gorman, E.; Eide, M.; Gorman, G.H.; Nylund, C.M. Association of constipation and fecal incontinence with attention-deficit/hyperactivity disorder. Pediatric 2013, 132, e1210–e1215. [Google Scholar] [CrossRef]
- von Gontard, A.; Niemczyk, J.; Weber, M.; Equit, M. Specific behavioral comorbidity in a large sample of children with functional incontinence: Report of 1001 cases. Neurourol. Urodyn. 2015, 34, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Van Herzeele, C.V.; DeBruyne, P.; DeBruyne, E.; Vande Walle, J. Challenging factors for enuresis treatment: Psychological problems and non-adherence. J. Pediatr. Urol. 2015, 11, 308–313. [Google Scholar] [CrossRef]
- Shepard, J.A.; Poler, J.E.; Grabman, J. Evidence-based psychosocial treatments for pediatric elimination disorders. J. Clin. Child Adolesc. Psychol. 2017, 46, 767–797. [Google Scholar] [CrossRef] [PubMed]
- Kakizaki, H.; Masafumi, K.; Masaki, W.; Naoki, W. Pathophysiological and Therapeutic Considerations for Non-Neurogenic Lower Urinary Tract Dysfunction in Children. LUTS Low. Urin. Tract Symptoms 2016, 8, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Farhat, W.; Bagli, D.J.; Capolicchio, G.; O’Reilly, S.; Merguerian, P.A.; Antoine, K.; Gordon, A.M. The dysfunctional voiding scoring system: Quantitative standardization of dysfunctional voiding symptoms in children. J. Urol. 2000, 164, 1011–1015. [Google Scholar] [CrossRef]
- Jansson, B.U.; Hanson, M.; Sillen, U.; Hellström, A.L. Voiding pattern and acquisition of bladder control from birth to age 6 years—A longitudinal study. J. Urol. 2005, 174, 289–293. [Google Scholar] [CrossRef]
- Hodges, S.J. Overactive bladder in children. Curr. Bladder Dysfunct. Rep. 2012, 7, 27–32. [Google Scholar] [CrossRef]
- Chase, J.; Paul, A.; Piet, H.; Patrick, M. The management of dysfunctional voiding in children: A report from the Standardization Committee of the International Children’s Continence Society. J. Urol. 2010, 183, 1296–1302. [Google Scholar] [CrossRef]
- Hagstroem, S.; Søren, R.; Konstantinos, K.; Jens, C.D. Timer watch assisted urotherapy in children: A randomized controlled trial. J. Urol. 2010, 184, 1482–1488. [Google Scholar] [CrossRef]
- Thom, M.; Campigotto, M.; Vemulakonda, V.; Coplen, D.; Austin, P.F. Management of lower urinary tract dysfunction: A stepwise approach. J. Pediatr. Urol. 2012, 8, 20–24. [Google Scholar] [CrossRef]
- Bernasconi, M.; Borsari, A.; Garzoni, L.; Siegenthaler, G.; Bianchetti, M.G.; Rizzi, M. Vaginal voiding: A common cause of daytime urinary leakage in girls. J. Pediatr. Adolesc. Gynecol. 2009, 22, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.; Thimmesch, I.; Aardsma, N.; Terrell, M.; Carstater, S.; Schober, J. The prevalence of abnormal genital findings, vulvovaginitis, enuresis and encopresis in children who present with allegations of sexual abuse. J. Pediatr. Urol. 2014, 10, 1216–1221. [Google Scholar] [CrossRef] [PubMed]
- Wennergren, M.H.; Öberg, B.E.; Sandstedt, P. The Importance of Leg Support for Relaxation of the Pelvic Floor Muscles A Surface Electromyograph Study in Healthy Girls. Scand. J. Urol. Nephrol. 1991, 25, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Tremback-Ball, A.; Gherghel, E.; Hegge, A.; Kindig, K.; Marsico, H.; Scanlon, R. The effectiveness of biofeedback therapy in managing Bladder Bowel Dysfunction in children: A systematic review. J. Pediatr. Rehabil. Med. 2018, 11, 161–173. [Google Scholar] [CrossRef] [PubMed]
- Brooks, C.R.; Copen, R.M.; Cox, D.J.; Morris, J.; Borowitz, S.; Sutphen, J. Review of the treatment literature for encopresis, functional constipation, and stool-toileting refusal. Ann. Behav. Med. 2000, 22, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Mugie, M.S.; di Lorenzo, C.; Benninga, M.A. Constipation in childhood. Nat. Rev. Gastroenterol. Hepatol. 2011, 8, 502. [Google Scholar] [CrossRef]
- McGrath, M.L.; Mellon, M.W.; Murphy, L. Empirically supported treatments in pediatric psychology: Constipation and encopresis. J. Pediatr. Psychol. 2000, 25, 225–254. [Google Scholar] [CrossRef] [PubMed]
- Culbert, P.T.; Banez, G.A. Integrative approaches to childhood constipation and encopresis. Pediatr. Clin. N. Am. 2007, 54, 927–947. [Google Scholar] [CrossRef]
- Newman, D.K.; Wein, A.J. Office-based behavioral therapy for management of incontinence and other pelvic disorders. Urol. Clin. N. Am. 2013, 40, 613–635. [Google Scholar] [CrossRef]
- Cox, J.D.; Sutphen, J.; Ling, W.; Quillian, W.; Borowitz, S. Additive benefits of laxative, toilet training, and biofeedback therapies in the treatment of pediatric encopresis. J. Pediatr. Psychol. 1996, 21, 659–667. [Google Scholar] [CrossRef]


| ICCS Lower Urinary Tract Symptoms |
|---|
| Increased or decreased frequency |
| Incontinence |
| Urinary urgency |
| Nocturia |
| Hesitancy |
| Straining |
| Dysuria |
| Weak stream |
| Intermittent stream |
| Holding maneuvers |
| Feelings of incomplete emptying |
| Urinary retention |
| Post micturition dribbling |
| Spraying or splitting of the urinary stream |
| Pain of the LUT—genital, urethral or bladder |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morgan, K.E.; Leroy, S.V.; Corbett, S.T.; Shepard, J.A. Complementary and Integrative Management of Pediatric Lower Urinary Tract Dysfunction Implemented within an Interprofessional Clinic. Children 2019, 6, 88. https://0-doi-org.brum.beds.ac.uk/10.3390/children6080088
Morgan KE, Leroy SV, Corbett ST, Shepard JA. Complementary and Integrative Management of Pediatric Lower Urinary Tract Dysfunction Implemented within an Interprofessional Clinic. Children. 2019; 6(8):88. https://0-doi-org.brum.beds.ac.uk/10.3390/children6080088
Chicago/Turabian StyleMorgan, Kathryn E., Susan V. Leroy, Sean T. Corbett, and Jaclyn A. Shepard. 2019. "Complementary and Integrative Management of Pediatric Lower Urinary Tract Dysfunction Implemented within an Interprofessional Clinic" Children 6, no. 8: 88. https://0-doi-org.brum.beds.ac.uk/10.3390/children6080088




