Neglected Fractures of the Lateral Humeral Condyle in Children; Which Treatment for Which Condition?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Statistical Analysis
3. Results
3.1. Patient Demographics and Baseline Characteristics
3.2. Treatment and Outcomes
4. Discussion
- -
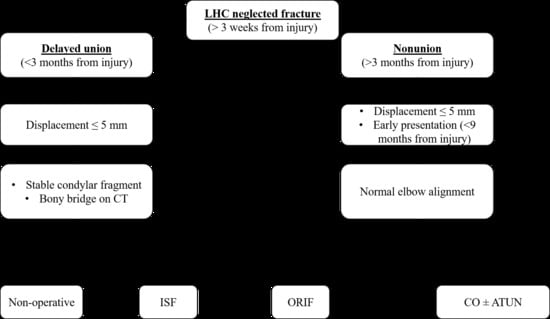
- Neglected LHC fractures presenting within 3 months after injury may be treated conservatively if the lateral displacement is <5 mm and the condylar fragment remains stable in serial radiographs. CT scans could help to identify bony bridges between fragments.
- -
- Neglected LHC fractures presenting within 3 months after injury may be treated by ISF if the lateral displacement is ≤5 mm but the condylar fragment migrates in serial radiographs, or by ORIF if the lateral displacement is >5 mm.
- -
- Neglected LHC fractures presenting at more than 3 months after injury must be treated surgically. ISF should be recommended in the case of minor displacement (≤5 mm) and early presentation (9 months on average in our cohort). ORIF should be preferred in the case of major displacement (>5 mm) and late presentation (24 months on average in our cohort). Corrective osteotomy (possibly combined with ISF and ATUN) should be recommended in case of LHC nonunion associated with severe elbow deformity.
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Tan, S.H.S.; Dartnell, J.; Lim, A.K.S.; Hui, J.H. Paediatric lateral condyle fractures: A systematic review. Arch. Orthop. Trauma Surg. 2018, 138, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Flynn, J.C. Nonunion of slightly displaced fractures of the lateral humeral condyle in children: An update. J. Pediatr. Orthop. 1989, 9, 691–696. [Google Scholar] [CrossRef] [PubMed]
- Song, K.S.; Kang, C.H.; Min, B.W.; Bae, K.C.; Cho, C.-H.; Lee, J.H. Closed Reduction and Internal Fixation of Displaced Unstable Lateral Condylar Fractures of the Humerus in Children. J. Bone Jt. Surg. Am. 2008, 90, 2673–2681. [Google Scholar] [CrossRef] [PubMed]
- Ramo, B.A.; Funk, S.S.; Elliott, M.E.; Jo, C.-H. The Song Classification Is Reliable and Guides Prognosis and Treatment for Pediatric Lateral Condyle Fractures: An Independent Validation Study with Treatment Algorithm. J. Pediatr. Orthop. 2020, 40, e203–e209. [Google Scholar] [CrossRef] [PubMed]
- Flynn, J.C.; Richards, J.F., Jr.; Saltzman, R.I. Prevention and treatment of non-union of slightly displaced fractures of the lateral humeral condyle in children. An end-result study. J. Bone Jt. Surg. Am. 1975, 57, 1087–1092. [Google Scholar] [CrossRef]
- Dhillon, K.S.; Sengupta, S.; Singh, B. Delayed management of fracture of the lateral humeral condyle in children. Acta Orthop. Scand. 1988, 59, 419–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wattenbarger, J.M.; Gerardi, J.; Johnston, C.E. Late Open Reduction Internal Fixation of Lateral Condyle Fractures. J. Pediatr. Orthop. 2002, 22, 394–398. [Google Scholar] [CrossRef]
- Agarwal, A.; Qureshi, N.A.; Gupta, N.; Verma, I.; Pandey, D.K. Management of neglected lateral condyle fractures of humerus in children: A retrospective study. Indian J. Orthop. 2012, 46, 698–704. [Google Scholar] [CrossRef]
- Liu, T.J.; Wang, E.B.; Dai, Q.; Zhang, L.J.; Li, Q.W.; Zhao, Q. Open reduction and internal fixation for the treatment of fractures of the lateral humeral condyle with an early delayed presentation in children: A radiological and clinical prospective study. Bone Jt. J. 2016, 98, 244–248. [Google Scholar] [CrossRef]
- Saraf, S.K.; Khare, G.N. Late presentation of fractures of the lateral condyle of the humerus in children. Indian J. Orthop. 2011, 45, 39–44. [Google Scholar] [CrossRef]
- Salgueiro, L.; Roocroft, J.H.; Bastrom, T.P.; Edmonds, E.W.; Pennock, A.T.; Upasani, V.V.; Yaszay, B. Rate and Risk Factors for Delayed Healing Following Surgical Treatment of Lateral Condyle Humerus Fractures in Children. J. Pediatr. Orthop. 2017, 37, 1–6. [Google Scholar] [CrossRef]
- Eamsobhana, P.; Kaewpornsawan, K. Should we repair nonunion of the lateral humeral condyle in children? Int. Orthop. 2015, 39, 1579–1585. [Google Scholar] [CrossRef]
- Park, H.; Hwang, J.H.; Kwon, Y.U.; Kim, H.W. Osteosynthesis In Situ for Lateral Condyle Nonunion in Children. J. Pediatr. Orthop. 2015, 35, 334–340. [Google Scholar] [CrossRef]
- Jakob, R.; Fowles, J.V.; Rang, M.; Kassab, M.T. Observations concerning fractures of the lateral humeral condyle in children. J. Bone Jt. Surg. Br. Vol. 1975, 57, 430–436. [Google Scholar] [CrossRef]
- Shrestha, S.; Hutchison, R.L. Outcomes for late presenting lateral condyle fractures of the humerus in children: A case series. J. Clin. Orthop. Trauma 2020, 11, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Prakash, J.; Mehtani, A. Open reduction versus in-situ fixation of neglected lateral condyle fractures: A comparative study. J. Pediatr. Orthop. B 2018, 27, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Knight, D.M.; Alves, C.; Alman, B.; Howard, A. Percutaneous Screw Fixation Promotes Healing of Lateral Condyle Nonunion in Children. J. Pediatr. Orthop. 2014, 34, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Masada, K.; Kawai, H.; Kawabata, H.; Masatomi, T.; Tsuyuguchi, Y.; Yamamoto, K. Osteosynthesis for old, established non-union of the lateral condyle of the humerus. J. Bone Jt. Surg. Am. 1990, 72, 32–40. [Google Scholar] [CrossRef]
- Tien, Y.C.; Chen, J.C.; Fu, Y.C.; Chih, T.T.; Hunag, P.J.; Wang, G.J. Supracondylar dome osteotomy for cubitus valgus deformity associ-ated with a lateral condylar nonunion in children. J. Bone Jt. Surg. Am. 2005, 87, 1456–1463. [Google Scholar]
- Abed, Y.; Nour, K.; Kandil, Y.R.; El-Negery, A. Triple management of cubitus valgus deformity complicating neglected nonunion of fractures of lateral humeral condyle in children: A case series. Int. Orthop. 2018, 42, 375–384. [Google Scholar] [CrossRef]
- Weiss, J.M.; Graves, S.; Yang, S.; Mendelsohn, E.; Kay, R.M.; Skaggs, D.L. A New Classification System Predictive of Complications in Surgically Treated Pediatric Humeral Lateral Condyle Fractures. J. Pediatr. Orthop. 2009, 29, 602–605. [Google Scholar] [CrossRef] [PubMed]
- Dodwell, E.; Pathy, R.; Widmann, R.F.; Green, D.W.; Scher, D.M.; Blanco, J.S.; Doyle, S.M.; Daluiski, A.; Sink, E.L. Reliability of the Modified Clavien-Dindo-Sink Complication Classification System in Pediatric Orthopaedic Surgery. JBJS Open Access 2018, 3, e0020. [Google Scholar] [CrossRef] [PubMed]
- Morrey, B.F.; An, K.N.; Chao, E.Y.S. Functional evaluation of the elbow. In The Elbow and Its Disorders, 2nd ed.; Morrey, B.F., Ed.; WB Saunders Co.: Philadelphia, PA, USA, 1993; p. 95. [Google Scholar]




| Baseline Variable | Treatment | ||||
|---|---|---|---|---|---|
| Conservative | ISF | ORIF | CO | Total | |
| Patients (female/male) | 6 (2/4) | 7 (1/6) | 11 (3/8) | 3 (1/2) | 27 (7/20) |
| Age (years) | 4.8 ± 1.4 (4–7) | 5.0 ± 2.2 (2–8) | 5.9 ± 2.2 (3–9) | 14 ± 1.0 (13–15) *** | 6.3 ± 3.3 (2–15) |
| Time interval between injury and treatment (months) | 2 ± 1 (1–3) | 9 ± 16 (2–45) | 24 ± 36 (1–95) | 127 ± 31 (92–152) *** | 27 ± 45 (1–152) |
| Follow-up (years) | 6.8 ± 4.4 (2–13) | 7.6 ± 4.1 (2–15) | 8.6 ± 4.1 (2–16) | 2.3 ± 0.6 (2–3) | 7.3 ± 4.2 (2–16) |
| Weiss classification (II-III) | 4-2 | 4-3 | 2-9 | 1-2 | 11-16 |
| Song classification (III-IV-V) | 5-1-0 | 7-0-0 | 3-6-2 * | 1-2-0 | 10-9-2 |
| Lateral displacement (mm) | 4 ± 2 (3–7) | 4 ± 1 (3–6) | 8 ± 3 (5–12) *** | 13 ± 4 (10–18) | 7 ± 4 (3–18) |
| Medial displacement (mm) | 7 ± 5 (2–16) | 8 ± 3 (4–13) | 10 ± 4 (4–16) | 13 ± 5 (10–19) | 9 ± 4 (2–19) |
| Carrying angle (degrees) | 5 ± 4 (0–7) | −8 ± 22 (−37–10) | 4 ± 17 (−30–25) | 33 ± 12 (21–45) * | 5 ± 20 (−37–45) |
| ROM (degrees) | 86 ± 33 (45–140) | 109 ± 35 (40–145) | 98 ± 50 (20–145) | 135 ± 9 (125–140) | 192 ± 41 (20–145) |
| DhiS overall/functional (points) | 5 ± 2/3 ± 2 | 6 ± 2/3 ± 2 | 5 ± 2/4 ± 2 | 3 ± 0/3 ± 1 | 5 ± 2/3 ± 2 |
| MEPS (points) | 58 ± 25 (30–95) | 66 ± 17 (35–85) | 60 ± 29 (10–100) | 63 ± 3 (60–65) | 62 ± 2 (10–100) |
| Outcome Variable | Treatment | ||||
|---|---|---|---|---|---|
| Conservative | ISF | ORIF | CO | Total | |
| Follow-up (years) | 6.8 ± 4.4 (2–13) | 7.6 ± 4.1 (2–15) | 8.6 ± 4.1 (2–16) | 2.3 ± 0.6 (2–3) | 7.3 ± 4.2 (2–16) |
| Time to union (months) | 6 ± 4 (4–10) | 3 ± 3 (1–13) | 5 ± 7 (1–25) | 6.3 ± 3.3 (1–25) | |
| Overall complications | 4 (67%) | 2 (29%) | 9 (82%) | 1 (33%) | 16 (59%) |
| Major complications (CDS > 2) | 1 (17%) | 1 (14%) | 3 (27%) | 1 (33%) | 6 (22%) |
| Carrying angle (degrees) | 13 ± 18 (0–50) | 3 ± 8 (−10–15) | 5 ± 16 (−20–20) | 18 ± 10 (8–37) | 8 ± 13 (−20–50) |
| ROM (degrees) | 138 ± 4 (130–140) | 139 ± 13 (110–145) | 127 ± 25 (70–145) | 143 ± 3 (140–140) | 134 ± 18 (70–145) |
| DhiS overall/functional (points) | 8 ± 1/6 ± 0.5 | 8 ± 1/6 ± 0.5 | 8 ± 1/5 ± 1 | 7 ± 3/5 ± 2 | 8 ± 2/5 ± 1 |
| MEPS (points) | 98 ± 3 (95–100) | 100 | 98 ± 6 (80–100) | 87 ± 23 (60–100) | 97 ± 8 (60–100) |
| Variables | Spearman’s r | p-Value |
|---|---|---|
| Time interval between injury and treatment/follow-up MEPS | 0.43 | 0.026 |
| CDS/follow-up DhiS (overall) | −0.70 | <0.0005 |
| CDS/follow-up DhiS (function) | −0.42 | 0.029 |
| CDS/follow-up MEPS | −0.55 | 0.003 |
| Weiss/follow-up Dhis (overall) | −0.44 | 0.020 |
| Weiss/follow-up MEPS | −0.40 | 0.042 |
| Song/follow-up DhiS (function) | −0.48 | 0.017 |
| Baseline elbow carrying angle/follow-up elbow carrying angle | 0.69 | 0.001 |
| Baseline ROM/follow-up ROM | 0.43 | 0.026 |
| Baseline DhiS (overall)/follow-up DhiS (function) | 0.48 | 0.012 |
| Baseline DhiS (function)/follow-up ROM | 0.44 | 0.022 |
| Baseline DhiS (function)/follow-up DhiS (function) | 0.44 | 0.023 |
| Baseline MEPS/follow-up ROM | 0.41 | 0.033 |
| Baseline MEPS/follow-up DhiS (function) | 0.46 | 0.017 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trisolino, G.; Antonioli, D.; Gallone, G.; Stallone, S.; Zarantonello, P.; Tanzi, P.; Olivotto, E.; Stilli, L.; Di Gennaro, G.L.; Stilli, S. Neglected Fractures of the Lateral Humeral Condyle in Children; Which Treatment for Which Condition? Children 2021, 8, 56. https://0-doi-org.brum.beds.ac.uk/10.3390/children8010056
Trisolino G, Antonioli D, Gallone G, Stallone S, Zarantonello P, Tanzi P, Olivotto E, Stilli L, Di Gennaro GL, Stilli S. Neglected Fractures of the Lateral Humeral Condyle in Children; Which Treatment for Which Condition? Children. 2021; 8(1):56. https://0-doi-org.brum.beds.ac.uk/10.3390/children8010056
Chicago/Turabian StyleTrisolino, Giovanni, Diego Antonioli, Giovanni Gallone, Stefano Stallone, Paola Zarantonello, Piergiuseppe Tanzi, Eleonora Olivotto, Luca Stilli, Giovanni Luigi Di Gennaro, and Stefano Stilli. 2021. "Neglected Fractures of the Lateral Humeral Condyle in Children; Which Treatment for Which Condition?" Children 8, no. 1: 56. https://0-doi-org.brum.beds.ac.uk/10.3390/children8010056