Vertigo and Dizziness in Children: An Update
Abstract
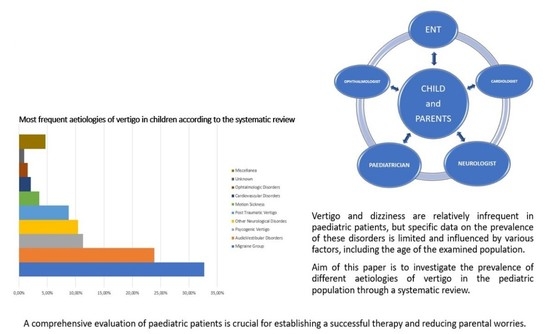
:1. Introduction
2. Materials and Methods
- Original studies on Cohort of patients > 50;
- Studies on paediatric population;
- Studies including audio-vestibular diagnoses.
- Studies containing duplicated data from other published work;
- Cohort of patients < 50;
- Studies published in languages other than English;
- Studies not including audio-vestibular diagnoses;
- Studies published before 2011.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Reilly, R.C.; Morlet, T.; Nicholas, B.D.; Josephson, G.; Horlbeck, D.; Lundy, L.; Mercado, A. Prevalence of Vestibular and Balance Disorders in Children. Otol. Neurotol. 2010, 31, 1441–1444. [Google Scholar] [CrossRef] [PubMed]
- Brodsky, J.R.; Lipson, S.; Bhattacharyya, N. Prevalence of Pediatric Dizziness and Imbalance in the United States. Otolaryngol. Neck Surg. 2020, 162, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Balatsouras, D.G.; Kaberos, A.; Assimakopoulos, D.; Katotomichelakis, M.; Economou, N.C.; Korres, S.G. Etiology of Vertigo in Children. Int. J. Pediatr. Otorhinolaryngol. 2007, 71, 487–494. [Google Scholar] [CrossRef]
- Cumberworth, V.L.; Patel, N.N.; Rogers, W.; Kenyon, G.S. The Maturation of Balance in Children. J. Laryngol. Otol. 2007, 121, 449–454. [Google Scholar] [CrossRef]
- Niemensivu, R.; Kentala, E.; Wiener-Vacher, S.; Pyykkö, I. Evaluation of Vertiginous Children. Eur. Arch. Oto-Rhino-Laryngol. 2007, 264, 1129–1135. [Google Scholar] [CrossRef]
- Shirabe, S. Vestibular Neuronitis in Childhood. Acta Oto-Laryngol. 1988, 105, 120–122. [Google Scholar] [CrossRef]
- Weiss, A.H.; Phillips, J.O. Congenital and Compensated Vestibular Dysfunction in Childhood: An Overlooked Entity. J. Child Neurol. 2006, 21, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Rine, R.M.; Braswell, J.; Fisher, D.; Joyce, K.; Kalar, K.; Shaffer, M. Improvement of Motor Development and Postural Control Following Intervention in Children with Sensorineural Hearing Loss and Vestibular Impairment. Int. J. Pediatr. Otorhinolaryngol. 2004, 68, 1141–1148. [Google Scholar] [CrossRef]
- Braswell, J.; Rine, R.M. Evidence that Vestibular Hypofunction Affects Reading Acuity in Children. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 1957–1965. [Google Scholar] [CrossRef] [PubMed]
- Haripriya, G.; Lepcha, A.; Augustine, A.M.; John, M.; Philip, A.; Mammen, M.D. Prevalence, Clinical Profile, and Diagnosis of Pediatric Dizziness in a Tertiary Care Hospital. Int. J. Pediatr. Otorhinolaryngol. 2021, 146, 110761. [Google Scholar] [CrossRef]
- Gedik-Soyuyuce, O.; Gence-Gumus, Z.; Ozdilek, A.; Ada, M.; Korkut, N. Vestibular Disorders in Children: A Retrospective Analysis of Vestibular Function Test Findings. Int. J. Pediatr. Otorhinolaryngol. 2021, 146, 110751. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, C.; Spataro, D.; de Zinis, L.R. Benign Positional Paroxysmal Vertigo in Children. Audiol. Res. 2021, 11, 47–54. [Google Scholar] [CrossRef]
- Wang, A.; Zhou, G.; Lipson, S.; Kawai, K.; Corcoran, M.; Brodsky, J.R. Multifactorial Characteristics of Pediatric Dizziness and Imbalance. Laryngoscope 2021, 131. [Google Scholar] [CrossRef] [PubMed]
- Duarte, J.A.; Leão, E.M.; Fragano, D.S.; Marquez, G.J.; Pires, A.P.B.D.; Silva, M.L.S.; Ganança, F.F. Vestibular Syndromes in Childhood and Adolescence. Int. Arch. Otorhinolaryngol. 2020, 24, e477–e481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.D.; Kim, C.-H.; Hong, S.M.; Kim, S.H.; Suh, M.-W.; Kim, M.-B.; Shim, D.B.; Chu, H.; Lee, N.H.; Kim, M.; et al. Prevalence of Vestibular and Balance Disorders in Children and Adolescents According to Age: A Multi-Center Study. Int. J. Pediatr. Otorhinolaryngol. 2017, 94, 36–39. [Google Scholar] [CrossRef]
- Sommerfleck, P.A.; Macchi, M.E.G.; Weinschelbaum, R.; De Bagge, M.D.; Bernáldez, P.; Carmona, S. Balance Disorders in Childhood: Main Etiologies According to Age. Usefulness of the Video Head Impulse Test. Int. J. Pediatr. Otorhinolaryngol. 2016, 87, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Wig, R.; Oakley, C.B. Dysautonomia and Headache in the Pediatric Population. Headache J. Head Face Pain 2019, 59, 1582–1588. [Google Scholar] [CrossRef]
- van de Berg, R.; Widdershoven, J.; Bisdorff, A.; Evers, S.; Wiener-Vacher, S.; Cushing, S.L.; Mack, K.J.; Kim, J.S.; Jahn, K.; Strupp, M.; et al. Vestibular Migraine and Recurrent Vertigo of Childhood: Diagnostic Criteria Consensus Document of the Classification Committee of Vestibular Disorders of the Bárány Society and the International Headache Society. J. Vestib. Res. 2021, 31, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef]
- Bachor, E.; Wright, C.G.; Karmody, C.S. The Incidence and Distribution of Cupular Deposits in the Pediatric Vestibular Labyrinth. Laryngoscope 2002, 112, 147–151. [Google Scholar] [CrossRef]
- Giannantonio, S.; Scorpecci, A.; Montemurri, B.; Marsella, P. Case of COVID-19-Induced Vestibular Neuritis in a Child. BMJ Case Rep. 2021, 14, e242978. [Google Scholar] [CrossRef] [PubMed]
- Mat, Q.; Noël, A.; Loiselet, L.; Tainmont, S.; Chiesa-Estomba, C.M.; Lechien, J.R.; Duterme, J.-P. Vestibular Neuritis as Clinical Presentation of COVID-19. Ear Nose Throat J. 2021. [Google Scholar] [CrossRef] [PubMed]
- Park, H.G.; Lee, J.H.; Oh, S.H.; Park, M.K.; Suh, M.-W. Proposal on the Diagnostic Criteria of Definite Isolated Otolith Dysfunction. J. Audiol. Otol. 2019, 23, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Kotait, M.A.; Moaty, A.S.; Gabr, T.A. Vestibular Testing in Children with Severe-To-Profound Hearing loss. Int. J. Pediatr. Otorhinolaryngol. 2019, 125, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Garone, G.; Reale, A.; Vanacore, N.; Parisi, P.; Bondone, C.; Suppiej, A.; Brisca, G.; Calistri, L.; Cordelli, D.M.; Savasta, S.; et al. Acute Ataxia in Paediatric Emergency Departments: A Multicentre Italian Study. Arch. Dis. Child. 2019, 104, 768–774. [Google Scholar] [CrossRef]
- Surmeli, R.; Yalcin, A.D.; Surmeli, M.; Gunay, G. Vertiginous Epilepsy: Documentation of Clinical and Electrophysiological Findings of Nine Patients. Epileptic Disord 2020, 22, 775–781. [Google Scholar] [CrossRef]
- Udaka, Y.T.; Packer, R.J. Pediatric Brain Tumors. Neurol. Clin. 2018, 36, 533–556. [Google Scholar] [CrossRef] [PubMed]
- Flowers, M.; Reneker, J.; Karlson, C. Vestibular Rehabilitation for a Child with Posterior Fossa Syndrome: A Case Report. Pediatr. Phys. Ther. 2020, 32, E1–E5. [Google Scholar] [CrossRef] [PubMed]
- Ketola, S.; Niemensivu, R.; Henttonen, A.; Appelberg, B.; Kentala, E. Somatoform Disorders in Vertiginous Children and Adolescents. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 933–936. [Google Scholar] [CrossRef]
- Mastrangelo, M.; Midulla, F. Minor Head Trauma in the Pediatric Emergency Department: Decision Making Nodes. Curr. Pediatr. Rev. 2017, 13, 92–99. [Google Scholar] [CrossRef]
- Schlick, C.; Schniepp, R.; Loidl, V.; Wuehr, M.; Hesselbarth, K.; Jahn, K. Falls and Fear of Falling in Vertigo and Balance Disorders: A Controlled Cross-Sectional Study. J. Vestib. Res. 2016, 25, 241–251. [Google Scholar] [CrossRef] [Green Version]
- Wang, A.; Zhou, G.; Kawai, K.; O’Brien, M.; Shearer, A.E.; Brodsky, J.R. Benign Paroxysmal Positional Vertigo in Children and Adolescents with Concussion. Sports Health 2021, 13, 380–386. [Google Scholar] [CrossRef]
- Lipson, S.; Wang, A.; Corcoran, M.; Zhou, G.; Brodsky, J.R. Severe motion sickness in infants and children. Eur. J. Paediatr. Neurol. 2020, 28, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Wiener-Vacher, S.R.; Wiener, S.I.; Ajrezo, L.; Obeid, R.; Mohamed, D.; Boizeau, P.; Alberti, C.; Bucci, M.P. Dizziness and Convergence Insufficiency in Children: Screening and Management. Front. Integr. Neurosci. 2019, 13, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Authors | Year | Country | # | Sex | Age |
|---|---|---|---|---|---|
| Haripriya GR et al. [10] | 2021 | India | 89 | ♂ 53, ♀ 36 | 3–18 years |
| Gedik-Soyuyuce O et al. [11] | 2021 | Turkey | 203 | ♂ 82, ♀ 121 | 1–17years |
| Balzanelli C et al. [12] | 2021 | Italy | 423 | ♂ 171, ♀ 252 | Up to 15 years |
| Wang A et al. [13] | 2020 | USA | 1021 | ♂ 397, ♀ 624 | 9 months–21 years |
| Duarte JA et al. [14] | 2020 | Brazil | 117 | ♂ 53, ♀ 64 | 2–17 years |
| Lee JD et al. [15] | 2017 | South Korea | 411 | ♂ 181, ♀ 230 | Up to 18 years |
| Sommerfleck PA et al. [16] | 2016 | Argentina | 206 | ♂ 107, ♀ 99 | 1–18 years |
| Summary | 2016–2021 | 2470 | ♂1044, ♀ 1426 ♂:♀ = 1:1.3 | 9 months to 21 years |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fancello, V.; Palma, S.; Monzani, D.; Pelucchi, S.; Genovese, E.; Ciorba, A. Vertigo and Dizziness in Children: An Update. Children 2021, 8, 1025. https://0-doi-org.brum.beds.ac.uk/10.3390/children8111025
Fancello V, Palma S, Monzani D, Pelucchi S, Genovese E, Ciorba A. Vertigo and Dizziness in Children: An Update. Children. 2021; 8(11):1025. https://0-doi-org.brum.beds.ac.uk/10.3390/children8111025
Chicago/Turabian StyleFancello, Virginia, Silvia Palma, Daniele Monzani, Stefano Pelucchi, Elisabetta Genovese, and Andrea Ciorba. 2021. "Vertigo and Dizziness in Children: An Update" Children 8, no. 11: 1025. https://0-doi-org.brum.beds.ac.uk/10.3390/children8111025