Influence of a Child’s Cancer on the Functioning of Their Family
Abstract
:1. Introduction
2. Objective of this Research
3. Material and Method
3.1. Study Design
3.2. Participants
3.3. Research Procedures
3.4. Method
3.4.1. Questionnaire
3.4.2. Scales
Zung’s Self-Assessment Scale
Dysfunction Assessment Scale
3.5. Data Analysis
4. Results
4.1. Demographic Data
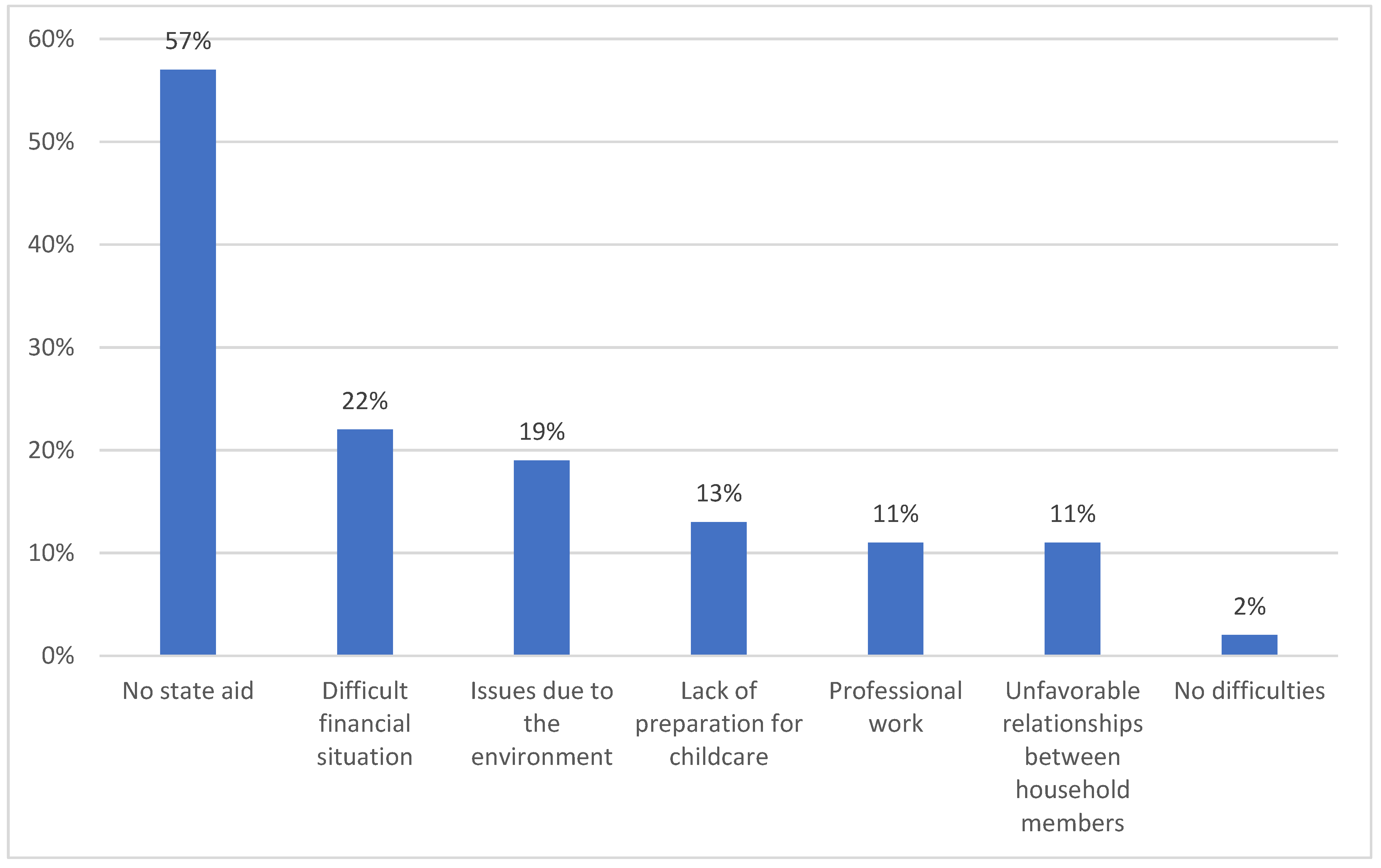
4.2. Financial Problems
4.3. Caring Problems
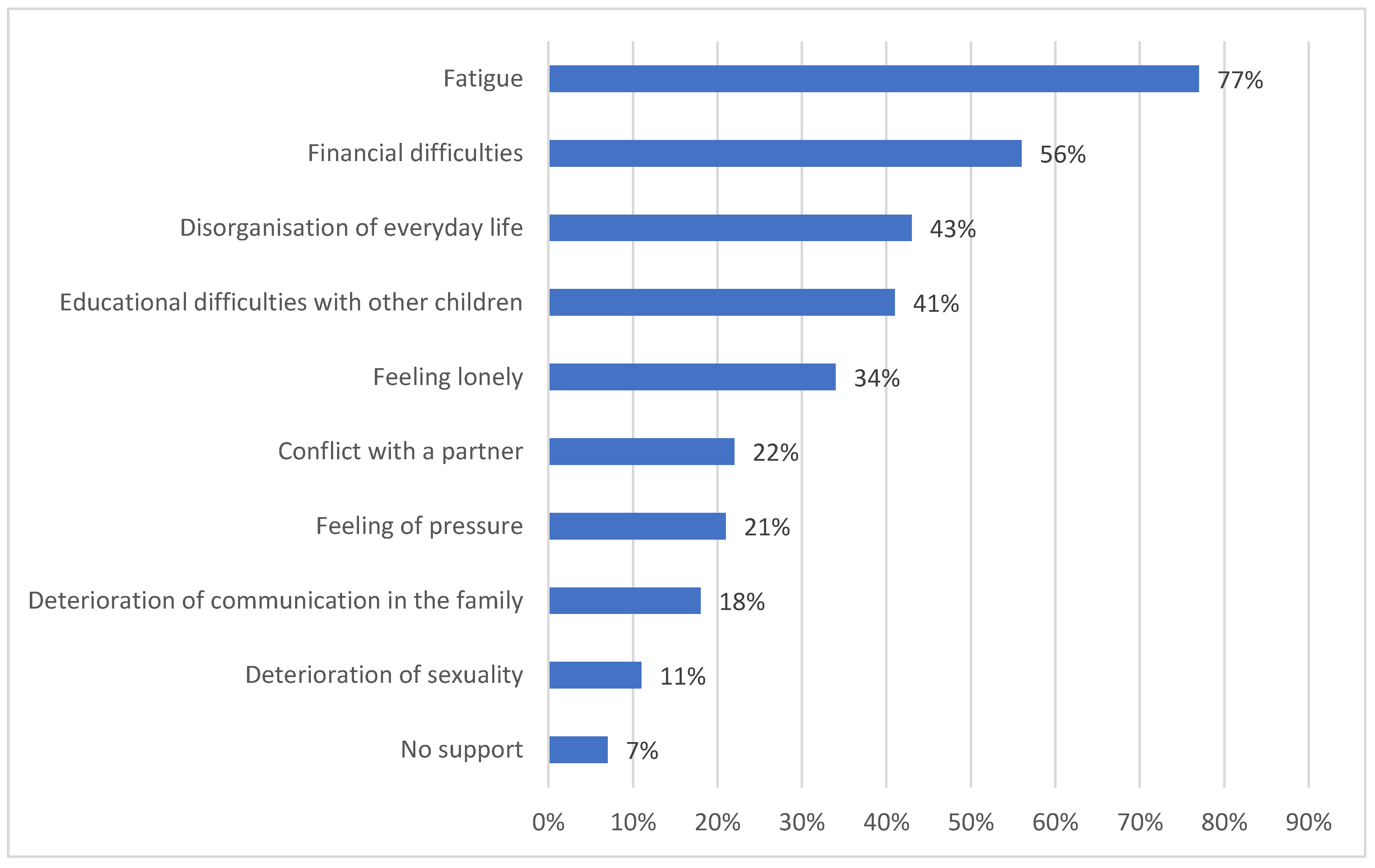
4.4. Psychological Problems
4.5. Somatic Problems
4.6. Communication Problems
4.7. Family Problems
4.8. Occurrence of Dysfunction
5. Discussion
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grudzińska, M.; Samardakiewicz, M. PAT.2.0 as a method identifying the psychosocial needs of families of children with cancer in Polish conditions. Psychoonkologia 2012, 16, 55–58. [Google Scholar]
- Öhman, M.; Woodford, J.; von Essen, L. Socioeconomic consequences of parenting a child with cancer for fathers and mothers in Sweden: A population-based difference-in-difference study. Int. J. Cancer 2021, 148, 2535–2541. [Google Scholar] [CrossRef]
- Patterson, J.M.; Holm, K.E.; Gurney, J.G. The impact of childhood cancer on the family: A qualitative analysis of strains, resources, and coping behaviors. PsychoOncology 2004, 13, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Budziszewska, B.K.; Piusińska-Macoch, R.; Sułek, K.; Stępień, A. Psychological problems of the family of cancer patients in the systemic concept. Acta Haematol. Pol. 2005, 36, 317–325. [Google Scholar]
- Tremolada, M.; Bonichini, S.; Schiavo, S.; Pillon, M. Post-traumatic stress symptoms in mothers of children with leukaemia undergoing the first 12 months of therapy: Predictive models. Psychol. Health 2012, 27, 1448–1462. [Google Scholar] [CrossRef]
- Norberg, A.L.; Pöder, U.; von Essen, L. Early avoidance of disease- and treatment-related distress predicts post-traumatic stress in parents of children with cancer. Eur. J. Oncol. Nurs. 2011, 15, 80–84. [Google Scholar] [CrossRef]
- Graj, E.; Muscara, F.; Anderson, V.; Hearps, S.; McCarthy, M. Quality of life in parents of seriously Ill/injured children: A prospective longitudinal study. Qual. Life Res. 2021, 30, 193–202. [Google Scholar] [CrossRef]
- van Warmerdam, J.; Zabih, V.; Kurdyak, P.; Sutradhar, R.; Nathan, P.C.; Gupta, S. Prevalence of anxiety, depression, and posttraumatic stress disorder in parents of children with cancer: A meta-analysis. Pediatric Blood Cancer 2019, 66, e27677. [Google Scholar] [CrossRef]
- Koumarianou, A.; Symeonidi, A.E.; Kattamis, A.; Linardatou, K.; Chrousos, G.P.; Darviri, C. A review of psychosocial interventions targeting families of children with cancer. Palliat. Supportive Care 2021, 19, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Boye, K. Can you stay home today? Parents’ occupations, relative resources and division of care leave for sick children. Acta Sociol. 2015, 58, 357–370. [Google Scholar] [CrossRef]
- Hiyoshi, A.; Montgomery, S.; Bottai, M.; Hovén, E. Trajectories of income and social benefits for mothers and fathers of children with cancer: A national cohort study in Sweden. Cancer 2018, 124, 1492–1500. [Google Scholar] [CrossRef]
- Lau, S.; Lu, X.; Balsamo, L.; Devidas, M.; Winick, N.; Hunger, S.P.; Carroll, W.; Stork, L.; Maloney, K.; Kadan-Lottick, N. Family life events in the first year of acute lymphoblastic leukemia therapy: A children’s oncology group report. Pediatric Blood Cancer 2014, 61, 2277–2284. [Google Scholar] [CrossRef] [Green Version]
- Lindahl Norberg, A.; Montgomery, S.M.; Bottai, M.; Heyman, M.; Hovén, E.I. Short-term and long-term effects of childhood cancer on income from employment and employment status: A national cohort study in Sweden. Cancer 2017, 123, 1238–1248. [Google Scholar] [CrossRef] [Green Version]
- Reisi-Dehkordi, N.; Baratian, H.; Zargham-Boroujeni, A. Challenges of children with cancer and their mothers: A qualitative research. Iran. J. Nurs. Midwifery Res. 2014, 19, 334–339. [Google Scholar]
- Markward, M.J.; Benner, K.; Freese, R. Perspectives of parents on making decisions about the care and treatment of a child with cancer: A review of literature. Fam. Syst. Health 2013, 31, 406–413. [Google Scholar] [CrossRef]
- Ljungman, L.; Cernvall, M.; Ghaderi, A.; Ljungman, G.; von Essen, L.; Ljótsson, B. An open trial of individualized face-to-face cognitive behavior therapy for psychological distress in parents of children after end of treatment for childhood cancer including a cognitive behavioral conceptualization. PeerJ 2018, 6, e4570. [Google Scholar] [CrossRef] [PubMed]
- Klassen, A.F.; Klaassen, R.; Dix, D.; Pritchard, S.; Yanofsky, R.; O’Donnell, M.; Scott, A.; Sung, L. Impact of caring for a child with cancer on parents’ health-related quality of life. J. Clin. Oncol. 2008, 26, 5884–5889. [Google Scholar] [CrossRef] [PubMed]
- Beheshtipour, N.; Nasirpour, P.; Yektatalab, S.; Karimi, M.; Zare, N. The Effect of Educational-Spiritual Intervention on The Burnout of The Parents of School Age Children with Cancer: A Randomized Controlled Clinical Trial. Int. J. Community Based Nurs. Midwifery 2016, 4, 90–97. [Google Scholar] [PubMed]
- Kazak, A.E.; Barakat, L.P.; Ditaranto, S.; Biros, D.; Hwang, W.T.; Beele, D. Screening for psychosocial risk at pediatric cancer diagnosis: The psychosocial assessment tool. J. Pediatric Hematol. Oncol. 2011, 33, 289–294. [Google Scholar] [CrossRef] [Green Version]
- Kazak, A.E.; Brier, M.; Alderfer, M.A.; Reilly, A.; Parker, S.F.; Rogerwick, S. Screening for psychosocial risk in pediatric cancer. Pediatric Blood Cancer 2012, 59, 822–827. [Google Scholar] [CrossRef] [Green Version]
- Kazak, A.E.; Abrams, A.N.; Banks, J.; Christofferson, J.; DiDonato, S.; Grootenhuis, M.A.; Kupst, M.J. Psychosocial assessment as a standard of care in pediatric cancer. Pediatric Blood Cancer 2015, 62, S426–S459. [Google Scholar] [CrossRef] [Green Version]
- Kazak, A.; Schneider, S.; DiDonato, S.; Pai, A. Family psychosocial risk screening guided by the Pediatric Preventative Psychosocial Health Model (PPPHM) using the Psychosocial Assessment Tool (PAT). Acta Oncol. 2015, 54, 574–580. [Google Scholar] [CrossRef]
- Gilleland, J.; Reed-Knight, B.; Brand, S.; Griffin, A.; Wasilewski-Masker, K.; Meacham, L.; Mertens, A. Assessment of family psychosocial functioning in survivors of pediatric cancer using the PAT2.0. Psychooncology 2013, 22, 2133–2139. [Google Scholar] [CrossRef]
- Alderfer, M.A.; Long, K.A.; Lown, A.; Marsland, A.L.; Ostrowski, N.L.; Hock, J.M.; Ewing, L.J. Psychosocial adjustment of siblings of children with cancer: A systematic review. Psychooncology 2010, 19, 789–805. [Google Scholar] [CrossRef] [PubMed]
- Gerhardt, C.A.; Lehmann, V.K.; Long, A.; Alderfer, M.A. Supporting Siblings as a Standard of Care in Pediatric Oncology. Pediatric Blood Cancer 2015, 62, S750–S804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kearney, J.A.; Salley, C.G.; Muriel, A.C. Standards of Psychosocial Care for Parents of Children With Cancer. Pediatric Blood Cancer 2015, 62, S632–S683. [Google Scholar] [CrossRef] [Green Version]
- Wiener, L.; Kazak, A.E.; Noll, R.B.; Patenaude, A.F.; Kupst, M.J. Interdisciplinary Collaboration in Standards of Psychosocial Care. Pediatric Blood Cancer 2015, 62, S425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajajee, S.; Ezhilarasi, S.; Indumathi, D. Psychosocial problems in families of children with cancer. Indian J. Pediatrics 2007, 74, 837–839. [Google Scholar] [CrossRef]
- Brody, A.C.; Simmons, L.A. Family resiliency during childhood cancer: The father’s perspective. J. Pediatric Oncol. Nurs. 2007, 24, 152–165. [Google Scholar] [CrossRef]
- Lavee, Y.; May-Dan, M. Patterns of change in marital relationships among parents of children with cancer. Health Soc. Work 2003, 28, 255–263. [Google Scholar] [CrossRef]
- da Silva, F.M.; Jacob, E.; Nascimento, L.C. Impact of Childhood Cancer on Parents’ Relationships: An Integrative Review. J. Nurs. Scholarsh. 2010, 42, 250–261. [Google Scholar] [CrossRef]
- Shapiro, J.; Perez, M.; Warden, M.J. The importance of family functioning to caregiver adaptation in mothers of child cancer patients: Testing a social ecological model. J. Pediatric Oncol. Nurs. 1998, 15, 47–54. [Google Scholar] [CrossRef]
- Pai, A.L.; Greenley, R.N.; Lewandowski, A.; Drotar, D.; Youngstrom, E.; Peterson, C.C. A meta-analytic review of the influence of pediatric cancer on parent and family functioning. J. Fam. Psychol. 2007, 21, 407–415. [Google Scholar] [CrossRef]
- Colletti, C.J.; Wolfe-Christensen, C.; Carpentier, M.Y.; Page, M.C.; McNall-Knapp, R.Y.; Meyer, W.H.; Chaney, J.M.; Mullins, L.L. The relationship of parental overprotection, perceived vulnerability, and parenting stress to behavioral, emotional, and social adjustment in children with cancer. Pediatric Blood Cancer 2008, 51, 269–274. [Google Scholar] [CrossRef]


| Demographic Information | Total N = 800 | p |
|---|---|---|
| Characteristics % (N) | ||
| Sex | ||
| Women | 85% (680) | 0.01 |
| Men | 15% (120) | |
| The age of the study group | ||
| SD | 44.1 (7.76) | 0.12 |
| 95% CI | <26; 57> | |
| The age of women | ||
| Age ± standard deviation | 38.2 ± 7.25 | 0.21 |
| Range | [26; 57] | |
| Median | 38 | |
| 95% CI | [39.8; 41.8] | |
| The age of men | ||
| Age ± standard deviation | 41,1 ± 7,03 | 0.19 |
| Range | [26; 57] | |
| Median | 41 | |
| 95% CI | [39.8; 41.8] | |
| Place of residence | ||
| City | 68% (544) | 0.21 |
| Village | 32% (256) | |
| Financial situation | ||
| Very good | 1% (8) | 0.01 |
| Good | 8% (64) | |
| Average | 68% (544) | |
| Bad | 10% (80) | |
| Very bad | 13% (104) | |
| Age groups | ||
| 20–29 | 3% (24) | 0.01 |
| 30–40 | 35% (280) | |
| 41–50 | 37% (296) | |
| 51–60 | 25% (200) | |
| Education of the study group | ||
| Higher education | 47% (378) | 0.01 |
| Secondary education | 35% (276) | |
| Vocational education | 18% (146) | |
| Primary education | 0% (0) | |
| Marital status | ||
| Married | 74% (592) | 0.62 |
| Widowed | 3% (24) | |
| Unmarried | 23% (184) | |
| Source of income | ||
| Professionally active | 76% (608) | 0.59 |
| Annuity | 15% (120) | |
| Benefit | 9% (72) | |
| Type of the child’s cancer | ||
| Leukemia | 54% (432) | 0.07 |
| Brain tumors | 19% (152) | |
| Solid tumors | 27% (216) | |
| Age of children with cancer | ||
| Up to 5 years | 22% (176) | 0.19 |
| 5–10 years | 51% (408) | |
| 11–18 years | 27% (216) | |
| Number of children in each family | ||
| One child | 45% (360) | 0.71 |
| Two children | 41% (328) | |
| Three children | 10% (80) | |
| Four children | 4% (32) | |
| Duration of illness | ||
| 3–12 months | 43% (344) | 0.01 |
| 1–2 years | 37% (296) | |
| 3–4 years | 20% (160) | |
| Area | Duration of the Disease | p | Place of Residence | p | Employment Status | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 3–12 Months | 1–2 Years | 3–4 Years | City | Village | Working | Not Working | ||||
| Characteristics % (N) | ||||||||||
| Somatic | ||||||||||
| Limited independence | 18% (68) | 7% (26) | 11% (41) | 0.41 | 15% (56) | 21% (79) | 0.91 | 27% (101) | 9% (68) | 0.01 |
| Disability | 3% (11) | 10% (38) | 10% (38) | 0.55 | 9% (34) | 14% (53) | 0.41 | 17% (64) | 6% (68) | 0.41 |
| Skin problems | 56% (210) | 30% (113) | 14% (53) | 0.01 | 52% (195) | 48% (180) | 0.81 | 55% (207) | 45% (68) | 0.19 |
| Gastric problems | 46% (173) | 26% (98) | 7% (26) | 0.01 | 38% (143) | 41% (154) | 0.77 | 39% (147) | 40% (150) | 0.88 |
| Psychological | ||||||||||
| Attention and memory deficits | 14% (62) | 25% (110) | 18% (79) | 0.41 | 24% (106) | 33% (145) | 0.91 | 21% (92) | 36% (158) | 0.64 |
| Learning difficulties | 11% (48) | 23% (101) | 20% (88) | 0.71 | 28% (123) | 26% (114) | 0.55 | 30% (132) | 24% (106) | 0.88 |
| Anxiety, restlessness | 34% (150) | 29% (128) | 17% (75) | 0.88 | 44% (194) | 36% (158) | 0.44 | 41% (180) | 39% (172) | 0.55 |
| Depression | 4% (18) | 15% (66) | 18% (79) | 0.55 | 17% (75) | 20% (88) | 0.55 | 15% (66) | 22% (97) | 0.71 |
| Mood swings | 34% (150) | 15% (66) | 18% (79) | 0.01 | 34% (150) | 33% (145) | 0.91 | 44% (194) | 23% (101) | 0.01 |
| Social | ||||||||||
| Difficulties in peer relationships | 12% (58) | 19% (93) | 24% (117) | 0.88 | 14% (68) | 41% (200) | 0.01 | 31% (151) | 24% (117) | 0.55 |
| Sibling relationship problems | 12% (58) | 10% (49) | 24% (117) | 0.41 | 21% (102) | 25% (122) | 0.62 | 40% (195) | 4% (19) | 0.01 |
| Reluctance to attend school | 10% (49) | 25% (122) | 21% (102) | 0.55 | 14% (68) | 42% (205) | 0.01 | 30% (146) | 26% (127) | 0.17 |
| Insulation | 13% (63) | 18% (89) | 27% (132) | 0.59 | 16% (78) | 42% (205) | 0.01 | 32% (156) | 26% (127) | 0.19 |
| Symptoms | Duration of Illness | p | Sex | p | |||
|---|---|---|---|---|---|---|---|
| 3–12 Months | 1–2 Years | 3–4 Years | Women | Men | |||
| Characteristics % (N) | |||||||
| Fatigue | 19% (65) | 10% (30) | 39% (62) | 0.01 | 39% (265) | 29% (35) | 0.02 |
| Weight loss | 7% (24) | 4% (12) | 13% (21) | 0.54 | 20% (136) | 4% (5) | 0.01 |
| Loss of appetite | 14% (48) | 18% (53) | 7% (11) | 0.03 | 19% (129) | 20% (24) | 0.88 |
| Gastric disorders | 24% (82) | 14% (41) | 9% (14) | 0.03 | 37% (252) | 10% (12) | 0.01 |
| Headaches | 22% (76) | 11% (32) | 9% (14) | 0.88 | 20% (136) | 22% (26) | 0.91 |
| Difficulty sleeping | 19% (65) | 4% (12) | 28% (45) | 0.01 | 29% (197) | 22% (26) | 0.71 |
| Difficulty concentrating | 9% (31) | 11% (32) | 19% (30) | 0.09 | 19% (129) | 20% (24) | 0.74 |
| Fear for the future | 29% (100) | 10% (30) | 10% (16) | 0.55 | 30% (204) | 19% (23) | 0.01 |
| Problems | Range | p | ||
|---|---|---|---|---|
| 0–10 | 11–20 | 21–30 | ||
| Characteristics % (N) | ||||
| Financial difficulties | 8% (64) | 10% (80) | 5% (40) | 0.71 |
| Lack of social support | 3% (24) | 3% (24) | 0% (0) | 0.54 |
| Lack of family support | 2% (16) | 2% (16) | 0% (0) | 0.03 |
| Psychological problems | 4% (32) | 4% (32) | 2% (16) | 0.03 |
| Problems in the relationship between partners | 5% (40) | 5% (40) | 2% (16) | 0.88 |
| Problems with stimulants | 4% (32) | 4% (32) | 1% (8) | 0.19 |
| Health problems | 4% (32) | 7% (56) | 5% (40) | 0.09 |
| Problems with caring for a sick child | 2% (16) | 7% (56) | 3% (24) | 0.55 |
| Problems with caring for siblings | 2% (16) | 4% (32) | 2% (16) | 0.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewandowska, A. Influence of a Child’s Cancer on the Functioning of Their Family. Children 2021, 8, 592. https://0-doi-org.brum.beds.ac.uk/10.3390/children8070592
Lewandowska A. Influence of a Child’s Cancer on the Functioning of Their Family. Children. 2021; 8(7):592. https://0-doi-org.brum.beds.ac.uk/10.3390/children8070592
Chicago/Turabian StyleLewandowska, Anna. 2021. "Influence of a Child’s Cancer on the Functioning of Their Family" Children 8, no. 7: 592. https://0-doi-org.brum.beds.ac.uk/10.3390/children8070592






