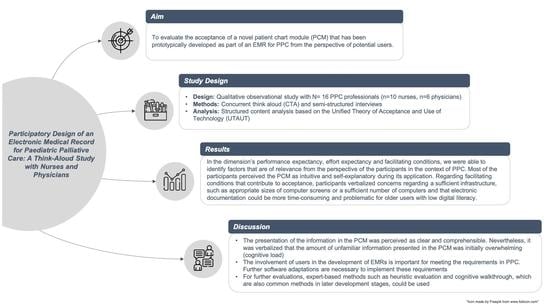
Participatory Design of an Electronic Medical Record for Paediatric Palliative Care: A Think-Aloud Study with Nurses and Physicians
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Participants and Recruitment
2.3. Patient Chart Module (PCM)
2.4. Study Procedure
2.5. Data Analysis
3. Results
3.1. General Observations
“Well, of course it’s a bit strange at first to do everything online on a PC, because you’re just used to writing. And I also thought at first that it would be totally difficult because I don’t really get along with computers, but I found it relatively simple and easy to understand. So, I often didn’t have to think long about where to find it and so on. It was already clear. I thought that was good in any case. I would have imagined it to be more difficult.”(Nurse_08_#00: 35:48#)
“I find them very clear. So, because with the PCM everything can be seen relatively quickly. I don’t have to go through umpteen sheets. I think that’s totally good. Yes. Otherwise. Yes, that you can jump back and forth very quickly. […] You have a quick overview of what you want to search for. I find the buttons so, so the individual sub-items listed quite well, so that you can also find it well and quickly. Exactly.”(Nurse_04_#00:44:15#)
“First of all, a lot of information for the beginning, a lot in the overview. Where you first have to get used to it, just get a bit of an overview. After a little bit of use, it was quite clear, I must say. I think it’s good that […], that not all menus appear here immediately. Because I think otherwise it’s going to overwhelm you. If now in and out with a patient is actually no problem at all, we also have patients who have no [Catheter] or anything similar. Then it’s not in there either. I think it’s good that you don’t have to worry about it and that it only appears when I really actively enter something in it. I also like the fact that you can do all this via this menu [Plus Button] item here and then really select the individual things. I think that’s really good. Here with the curve, with the fever curve, I think you have to get used to it a little bit first.”(Nurse_05_#00:49:49#)
3.2. General View and Plus-Button
“[…] Yeah, okay I’ll get on the tasks here and look at one day, three days, seven days. That’s probably up here. And click on-. Oh, three days I have to apply. No. Oh, I have to select the days. Now I would have thought, for example, that it would automatically select the [...] the last three are.”(Physician_15_#00:01:28#)
“Exactly, when many things are next to each other. Can you then scale, well there are scaling options at the moment, days, three days, seven days. And the question is, of course, whether the nursing staff might be happier, or the doctors, if you also have the option of eight hours, for example. So that one sees his shift there. Then it’s all bigger, easier to meet. […]. That will be at the latest when the medication process and so on is to be included. And they have a lot of medications.”(Physician_13_#00:43:17#)
“Mhm, so I wanted seven days now, right? And of course, I choose the last seven days now first, that’s the most common, isn’t it? So, I would have expected that I now somehow have the 3rd of July here. Now I can’t get to June. So, I already have to set the-, the date up here. Like this, isn’t it? And I have already said, I want seven days, then of course it would make sense he would shaded back from three, give me the last seven days, so that I then-. Now I would have to count, one, two, three, four, five, six, seven, is the 25th, isn’t it?”(Physician_13_#00:09:53#)
“I would have expected now, when I document on the 18th, that the 18th page also opens up [after saving]. And not the 17th […].”(Nurse_02_#00:29:19)
3.3. Vital Signs
“So, it has the advantage, if it is in the header, that it is immediately visible. The question is always: Is it then the current weight? Because the date of recording and the reason for recording are written here. So here you have the impression that there are, so to speak, the fixed quantities at time X. That this is now on the day weight and size, I would not expect now, if I consider the above as master data, first of all. Because that looks as if that’s something fixed that accompanies the patient over the whole time.”(Physician_10_#00: 13:26#)
“With the weight, you could still maybe somehow-, that you have another line like that [the vital signs chart]. There is only the current weight. So, if I have now weighed today, that one has there somehow again what. Or a button that you can click on, so that you can see the weights. That you can see such a progression. Especially for children, where it is important. They come because they are really too skinny. Or they have to be weighed every day or something. I think that would be cool.”(Nurse_02_#00: 45:32)
“And now here with the vital signs is-, there are no labels now, right? So, the red one is just red and down here it says minutes or something, whatever that’s supposed to be. Because I don’t know what that is. It doesn’t say that anywhere, does it.”(Physician_10_#00: 14:46#)
3.4. Sleep Patterns
“Exactly, the time span is the problem. That’s something, that’s unfortunate because that requires double steps. […] Document 12 to 12:30 bedside—will be the same. That means I have to do basically the same thing and I have to enter something twice. And then have to change the position again, so to speak. It’s doable, but it’s time consuming.”(Physician_10_#00:28:55#)
“But exactly, I would find that cool too, if you can click on it and then just change it to sleep [from awake] if you did it wrong.”(Physician_15_#00:20:10#)
“[…] So that, I think, would be quite good if you could perhaps add that to the sleep/wake rhythm, that you could somehow mark a time of restlessness once again. […] Because we currently also do this with red lines and red bars when the child has a restlessness phase.”(Nurse_05_#00:18:29#)
“But you don’t have a view of how the day and night rhythm changed during the week. That gets lost in the representation here. No. It’s just that I have a-, the same as our (paper-based) 24-h (sleep) protocol. But there you have it just among each other. And you see how a day and night rhythm shifts or forms. Evolves. And the info gets lost in here. That’s kind of difficult in the view, of course. We have this seven-day view now. But if I were to click on it now, make a double click, then maybe I would like to have the individual days one below the other.”(Physician_09_#00: 45:12#)
3.5. Symptom Observation
“There I go again on the plus and on symptoms. For example, I would write nausea-. For example, I could now enter severe nausea. Now I could write here, the current value is, I think, a degree of severity. That’s how I would interpret it now. I would still be missing, I don’t know, from zero to ten, zero to four, that you just-. Because everyone evaluates it a little bit differently and if I now enter a five, because for me it’s from zero to ten, I don’t know how it is with my successor, how they would then enter it or evaluate it.”(Nurse_11_#00:22:24#)
“I first thought that red was for pain and shortness of breath was yellow, for example. That both are clicked.”(Nurse_01_#00:06:34#)
3.6. Catheter Management
“Yes, exactly, the end times are a bit confusing, with the catheters. That everything, even if they continue, also has a start and an end point, so to speak. […] And if the others still continue, the line would actually just have to continue, and not also have, for me somehow, the same end point.”(Nurse_01_#00:34:01#)
3.7. Positioning
“Yes, the thing with the times. […] So, I would rather enter a time span, really, from 10:00 to 10:30, instead of always clicking on sleep from ten and then again on awake, from, I don’t know, eleven. So I find that kind of, yeah, so-. I would find it easier if I could just type that in, really. Sleep, like I do with my marker, I draw the line and that’s it, yeah. But that would be so the only thing.”(Nurse_01_#00:33:02#)
3.8. Intake and Output
“So I would have said now, red means that the urine somehow, that there was blood in it. Here is the colour brown, ah okay. In and out stool. That’s what’s confusing me right now. It says urine, but when I go to it [via mouse over], it says bowel movement. […] Okay, that’s maybe a little bit confusing because you get a little bit mixed up. Exactly. I would maybe somehow separate urine and stool, so there’s another extra line like we have in the curves now. I think that would make it a bit clearer.”(Nurse_08_#00:04:04#)
“Especially now with the balance sheet, for example, that I don’t have to calculate it myself later, that the PC spits it out for me when I can then close the balance sheet or something. That the PC then tells me, “Okay. We have now calculated this. The patient has drunk so and so many millilitres in total or litres and has excreted so and so much.” And it is still important that especially with our children who are diapered-. If, for example, there is stool in the Pampers and I weigh them, then I would document the number of grams of the Pampers as I have weighed them, plus loss or plus stool. Because that doesn’t actually count in the balance sheet, but I can’t separate it.”(Nurse_05_#00:41:45#)
3.9. Events
“If the patient now has an acute crisis, so to speak, so let’s say here would be because of me the saturation on nothing and then you would always have to scroll down to see [documented events]. Whether it can then be useful if the events slide upwards. So because if, so events are probably rather crises. […]. Because then I would rather want to know in the morning, I come somehow and think oh God, what was there. Then I don’t want to know whether he [the patient] was asleep or not, but what was there. But otherwise, I find it first of all somehow totally clear and easy to use and helpful. And I think that makes a lot of things easier, because you can see how long things have been there and need to be changed and so on.”(Physician_15_#00:49:10#)
3.10. Facilitating Conditions
“So, in the end, you have the values practically on a piece of paper and then you just enter them, right? So that’s how I imagine it now. Or I have directly, have such a laptop at the bed, where I can carry it then directly in. Yes. Somehow. Otherwise, one writes oneself also again doubly, if I write it first on a scratch note I say times and then into the curve. If I were with the PC at the bed or such a laptop, then one could enter it directly. So, then I think it’s not so time-consuming now.”(Nurse_04_#00: 14:17#)
“I still see the problem that actually everyone must have such a thing [e.g., computer, tablet], that you have to have space to sit down, I need a display which is good and clear. Where I also see difficulties is when I have such a small display and such a curve that it becomes confusing. […] You always like to look at statistics, whether the statistics are also such a small picture afterwards, but I don’t need that at all. If I always have such a small display afterwards, that doesn’t help me either. So, I think the hardware is actually important. And also the supply in the hardware.”(Nurse_03_#01:10:33#)
“Well, I think the younger ones can cope with it better than the older ones. I count myself as one of the younger ones. We more or less grew up with this kind of thing. We do a lot more with [computers] than our older colleagues. I think they’ll really have to get to grips with it. I think it will be more of a burden than a relief for them. I could imagine that.”(Nurse_07_#00:50:49#)
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Elements of the Plus-Button Menu |
 |
| General view |
 |
Appendix B
| General View and Plus-Button |
|
| Vital signs |
|
| Sleep patterns |
|
| Symptom observation |
|
| Catheter management |
|
| Positioning |
|
| Intake and output |
|
| Events |
|
Appendix C
| Interview Guide |
|
References
- Côté, A.-J.; Payot, A.; Gaucher, N. Paediatric Palliative Care in Practice: Perspectives between Acute and Long-Term Healthcare Teams. Acta Paediatr. 2020, 109, 613–619. [Google Scholar] [CrossRef]
- Bösch, A.; Wager, J.; Zernikow, B.; Thalemann, R.; Frenzel, H.; Krude, H.; Reindl, T. Life-Limiting Conditions at a University Pediatric Tertiary Care Center: A Cross-Sectional Study. J. Palliat. Med. 2018, 21, 169–176. [Google Scholar] [CrossRef]
- Taylor, J.; Booth, A.; Beresford, B.; Phillips, B.; Wright, K.; Fraser, L. Specialist Paediatric Palliative Care for Children and Young People with Cancer: A Mixed-Methods Systematic Review. Palliat. Med. 2020, 34, 731–775. [Google Scholar] [CrossRef]
- Thrane, S.E.; Maurer, S.H.; Cohen, S.M.; May, C.; Sereika, S.M. Pediatric Palliative Care: A Five-Year Retrospective Chart Review Study. J. Palliat. Med. 2017, 20, 1104–1111. [Google Scholar] [CrossRef]
- Siden, H. Pediatric Palliative Care for Children with Progressive Non-Malignant Diseases. Children 2018, 5, 28. [Google Scholar] [CrossRef] [Green Version]
- Lin, S.-C.; Huang, M.-C.; Yasmara, D.; Wuu, H.-L. Impact of Palliative Care on End-of-Life Care and Place of Death in Children, Adolescents, and Young Adults with Life-Limiting Conditions: A Systematic Review. Palliat. Supportive Care 2021, 19, 488–500. [Google Scholar] [CrossRef]
- Feudtner, C.; Kang, T.I.; Hexem, K.R.; Friedrichsdorf, S.J.; Osenga, K.; Siden, H.; Friebert, S.E.; Hays, R.M.; Dussel, V.; Wolfe, J. Pediatric Palliative Care Patients: A Prospective Multicenter Cohort Study. Pediatrics 2011, 127, 1094–1101. [Google Scholar] [CrossRef] [Green Version]
- Hoell, J.I.; Weber, H.; Warfsmann, J.; Trocan, L.; Gagnon, G.; Danneberg, M.; Balzer, S.; Keller, T.; Janßen, G.; Kuhlen, M. Facing the Large Variety of Life-Limiting Conditions in Children. Eur. J. Pediatr. 2019, 178, 1893–1902. [Google Scholar] [CrossRef] [PubMed]
- Radbruch, L.; Lima, L.D.; Knaul, F.; Wenk, R.; Ali, Z.; Bhatnaghar, S.; Blanchard, C.; Bruera, E.; Buitrago, R.; Burla, C.; et al. Redefining Palliative Care—A New Consensus-Based Definition. J. Pain Symptom Manag. 2020, 60, 754–764. [Google Scholar] [CrossRef] [PubMed]
- van der Zanden, T.M.; de Hoog, M.; Windster, J.D.; van Rosmalen, J.; van der Sijs, I.H.; de Wildt, S.N. Does a Dose Calculator as an Add-On to a Web-Based Paediatric Formulary Reduce Calculation Errors in Paediatric Dosing? A Non-Randomized Controlled Study. Pediatr. Drugs 2020, 22, 229–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García-López, I.; Vendrell, M.C.-M.; Romero, I.M.; de Noriega, I.; González, J.B.; Martino-Alba, R. Off-Label and Unlicensed Drugs in Pediatric Palliative Care: A Prospective Observational Study. J. Pain Symptom Manag. 2020, 60, 923–932. [Google Scholar] [CrossRef]
- Whalen, K.; Lynch, E.; Moawad, I.; John, T.; Lozowski, D.; Cummings, B.M. Transition to a New Electronic Health Record and Pediatric Medication Safety: Lessons Learned in Pediatrics within a Large Academic Health System. J. Am. Med. Inform. Assn. 2018, 25, 848–854. [Google Scholar] [CrossRef] [Green Version]
- Meyer, D.; Kernebeck, S.; Busse, T.S.; Ehlers, J.; Wager, J.; Zernikow, B.; Dreier, L.A. Electronic Health Records in Specialized Pediatric Palliative Care: A Qualitative Needs Assessment among Professionals Experienced and Inexperienced in Electronic Documentation. Children 2021, 8, 249. [Google Scholar] [CrossRef]
- Atasoy, H.; Greenwood, B.N.; McCullough, J.S. The Digitization of Patient Care: A Review of the Effects of Electronic Health Records on Health Care Quality and Utilization. Annu. Rev. Publ. Health 2018, 40, 487–500. [Google Scholar] [CrossRef] [Green Version]
- Rouleau, G.; Gagnon, M.-P.; Côté, J.; Payne-Gagnon, J.; Hudson, E.; Dubois, C.-A. Impact of Information and Communication Technologies on Nursing Care: Results of an Overview of Systematic Reviews. J. Med. Internet Res. 2017, 19, e122. [Google Scholar] [CrossRef]
- Campanella, P.; Lovato, E.; Marone, C.; Fallacara, L.; Mancuso, A.; Ricciardi, W.; Specchia, M.L. The Impact of Electronic Health Records on Healthcare Quality: A Systematic Review and Meta-Analysis. Eur. J. Public Health 2015, 26, 60–64. [Google Scholar] [CrossRef] [Green Version]
- Tsai, C.H.; Eghdam, A.; Davoody, N.; Wright, G.; Flowerday, S.; Koch, S. Effects of Electronic Health Record Implementation and Barriers to Adoption and Use: A Scoping Review and Qualitative Analysis of the Content. Life 2020, 10, 327. [Google Scholar] [CrossRef] [PubMed]
- Schneider, E.C.; Ridgely, M.S.; Meeker, D.; Hunter, L.E.; Khodyakov, D.; Rudin, R.S. Promoting Patient Safety Through Effective Health Information Technology Risk Management. Rand Health Q. 2014, 4, 7. [Google Scholar]
- Jones, S.S.; Rudin, R.S.; Perry, T.; Shekelle, P.G. Health Information Technology: An Updated Systematic Review With a Focus on Meaningful Use. Ann. Intern. Med. 2014, 160, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An Overview of Clinical Decision Support Systems: Benefits, Risks, and Strategies for Success. NPJ Digit. Med. 2020, 3, 17. [Google Scholar] [CrossRef] [Green Version]
- Vanderhook, S.; Abraham, J. Unintended Consequences of EHR Systems: A Narrative Review. Proc. Int. Symp. Hum. Factors Ergon. Healthc. 2017, 6, 218–225. [Google Scholar] [CrossRef]
- Kim, M.O.; Coiera, E.; Magrabi, F. Problems with Health Information Technology and Their Effects on Care Delivery and Patient Outcomes: A Systematic Review. J. Am. Med. Inform. Assn. 2017, 24, 246–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wisner, K.; Lyndon, A.; Chesla, C.A. The Electronic Health Record’s Impact on Nurses’ Cognitive Work: An Integrative Review. Int. J. Nurs. Stud. 2019, 94, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Melnick, E.R.; Dyrbye, L.N.; Sinsky, C.A.; Trockel, M.; West, C.P.; Nedelec, L.; Tutty, M.A.; Shanafelt, T. The Association Between Perceived Electronic Health Record Usability and Professional Burnout among US Physicians. Mayo Clin. Proc. 2020, 95, 476–487. [Google Scholar] [CrossRef] [Green Version]
- Senathirajah, Y.; Kaufman, D.R.; Cato, K.D.; Borycki, E.M.; Fawcett, J.A.; Kushniruk, A.W. Characterizing and Visualizing Display and Task Fragmentation in the Electronic Health Record: Methodological Approaches (Preprint). JMIR Hum. Factors 2020, 7, e18484. [Google Scholar] [CrossRef]
- Rothenberger, D.A. Physician Burnout and Well-Being: A Systematic Review and Framework for Action. Dis. Colon Rectum 2017, 60, 567–576. [Google Scholar] [CrossRef]
- Khairat, S.; Xi, L.; Liu, S.; Shrestha, S.; Austin, C. Understanding the Association between Electronic Health Record Satisfaction and the Well-Being of Nurses: Survey Study. JMIR Nurs. 2020, 3, e13996. [Google Scholar] [CrossRef]
- Vehko, T.; Hyppönen, H.; Puttonen, S.; Kujala, S.; Ketola, E.; Tuukkanen, J.; Aalto, A.-M.; Heponiemi, T. Experienced Time Pressure and Stress: Electronic Health Records Usability and Information Technology Competence Play a Role. BMC Med. Inform. Decis. 2019, 19, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Howe, J.L.; Adams, K.T.; Hettinger, A.Z.; Ratwani, R.M. Electronic Health Record Usability Issues and Potential Contribution to Patient Harm. JAMA 2018, 319, 1276–1278. [Google Scholar] [CrossRef]
- Tajirian, T.; Stergiopoulos, V.; Strudwick, G.; Sequeira, L.; Sanches, M.; Kemp, J.; Ramamoorthi, K.; Zhang, T.; Jankowicz, D. The Influence of Electronic Health Record Use on Physician Burnout: Cross-Sectional Survey. J. Med. Internet Res. 2020, 22, e19274. [Google Scholar] [CrossRef]
- Vandekerckhove, P.; de Mul, M.; Bramer, W.M.; de Bont, A.A. Generative Participatory Design Methodology to Develop Electronic Health Interventions: Systematic Literature Review. J. Med. Internet Res. 2020, 22, e13780. [Google Scholar] [CrossRef]
- Merkel, S.; Kucharski, A. Participatory Design in Gerontechnology: A Systematic Literature Review. Gerontologist 2019, 59, e16–e25. [Google Scholar] [CrossRef] [PubMed]
- Sadoughi, F.; Khodaveisi, T.; Ahmadi, H. The Used Theories for the Adoption of Electronic Health Record: A Systematic Literature Review. Health Technol. 2019, 9, 383–400. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.; Davis, G.; Davis, F. User Acceptance of Information Technology: Toward a Unified View. MIS Quart. 2003, 27, 425–478. [Google Scholar] [CrossRef] [Green Version]
- Ebnehoseini, Z.; Tabesh, H.; Jangi, M.J.; Deldar, K.; Mostafavi, S.M.; Tara, M. Investigating Evaluation Frameworks for Electronic Health Record: A Literature Review. Open Access Maced. J. Med. Sci. 2021, 9, 8–25. [Google Scholar] [CrossRef]
- Fan, M.; Lin, J.; Chung, C.; Truong, K.N. Concurrent Think-Aloud Verbalizations and Usability Problems. ACM Trans. Comput.-Hum. Int. 2019, 26, 1–35. [Google Scholar] [CrossRef]
- Denzin, N.K.; Ericsson, K.A.; Simon, H.A. Protocol Analysis: Verbal Reports as Data. Contemp. Sociol. 1985, 14, 125–126. [Google Scholar] [CrossRef]
- Bolle, S.; Romijn, G.; Smets, E.M.A.; Loos, E.F.; Kunneman, M.; van Weert, J.C.M. Older Cancer Patients’ User Experiences With Web-Based Health Information Tools: A Think-Aloud Study. J. Med. Internet Res. 2016, 18, e208. [Google Scholar] [CrossRef] [PubMed]
- Breuning, M.; Schäfer-Fauth, L.; Lucius-Hoene, G.; Holmberg, C. Connecting One’s Own Illness Story to the Illness Experiences of Others on a Website—An Evaluation Study Using the Think Aloud Method. Patient Educ. Couns. 2019, 103, 199–207. [Google Scholar] [CrossRef]
- Georgsson, M.; Staggers, N.; Årsand, E.; Kushniruk, A. Employing a User-Centered Cognitive Walkthrough to Evaluate a MHealth Diabetes Self-Management Application: A Case Study and Beginning Method Validation. J. Biomed. Inform. 2019, 91, 103110. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.G.S.; Robinson, I.; AlShawi, S. Developing Medical Device Technologies from Users’ Perspectives: A Theoretical Framework for Involving Users in the Development Process. Int. J. Technol. Assess. 2009, 25, 514–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ellsworth, M.A.; Dziadzko, M.; O’Horo, J.C.; Farrell, A.M.; Zhang, J.; Herasevich, V. An Appraisal of Published Usability Evaluations of Electronic Health Records via Systematic Review. J. Am. Med Inform. Assoc. JAMIA 2016, 24, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Russ, A.L.; Saleem, J.J. Ten Factors to Consider When Developing Usability Scenarios and Tasks for Health Information Technology. J. Biomed. Inform. 2018, 78, 123–133. [Google Scholar] [CrossRef]
- Alhadreti, O.; Mayhew, P. Are Two Pairs of Eyes Better Than One? A Comparison of Concurrent Think-Aloud and Co-Participation Methods in Usability Testing. J. Usability Stud. 2020, 13, 177–195. [Google Scholar]
- Moore, G.; Wilding, H.; Gray, K.; Castle, D. Participatory Methods to Engage Health Service Users in the Development of Electronic Health Resources: Systematic Review. J. Particip. Med. 2019, 11, e11474. [Google Scholar] [CrossRef] [Green Version]
- Kuckartz, U. Qualitative Text Analysis: A Guide to Methods, Practice & Using Software; Sage: London, UK, 2014. [Google Scholar] [CrossRef]
- Habibi, M.R.M.; Khajouei, R.; Eslami, S.; Jangi, M.; Ghalibaf, A.K.; Zangouei, S. Usability Testing of Bed Information Management System: A Think-Aloud Method. J. Adv. Pharm. Technol. Res. 2018, 9, 153–157. [Google Scholar] [CrossRef]
- den Haak, M.J.V.; de Jong, M.D.T.; Schellens, P.J. Employing Think-Aloud Protocols and Constructive Interaction to Test the Usability of Online Library Catalogues: A Methodological Comparison. Interact. Comput. 2004, 16, 1153–1170. [Google Scholar] [CrossRef] [Green Version]
- Khawaja, M.A.; Chen, F.; Marcus, N. Measuring Cognitive Load Using Linguistic Features: Implications for Usability Evaluation and Adaptive Interaction Design. Int J. Hum. Comput. Int 2014, 30, 343–368. [Google Scholar] [CrossRef]
- Melnick, E.R.; Harry, E.; Sinsky, C.A.; Dyrbye, L.N.; Wang, H.; Trockel, M.T.; West, C.P.; Shanafelt, T. Perceived Electronic Health Record Usability as a Predictor of Task Load and Burnout Among US Physicians: Mediation Analysis. J. Med. Internet Res. 2020, 22, e23382. [Google Scholar] [CrossRef]
- Roman, L.C.; Ancker, J.S.; Johnson, S.B.; Senathirajah, Y. Navigation in the Electronic Health Record: A Review of the Safety and Usability Literature. J. Biomed. Inform. 2017, 67, 69–79. [Google Scholar] [CrossRef]
- O’Donnell, H.C.; Suresh, S.; Technology, C.O.C.I. Electronic Documentation in Pediatrics: The Rationale and Functionality Requirements. Pediatrics 2020, 146, e20201682. [Google Scholar] [CrossRef] [PubMed]
- Subbe, C.P.; Tellier, G.; Barach, P. Impact of electronic health records on predefined safety outcomes in patients admitted to hospital: A scoping review. BMJ Open 2021, 11, e047446. [Google Scholar] [CrossRef]
- Horwood, L.; Mok, E.; Li, P.; Oskoui, M.; Shevell, M.; Constantin, E. Prevalence of Sleep Problems and Sleep-Related Characteristics in Preschool-and School-Aged Children with Cerebral Palsy. Sleep Med. 2018, 50, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Dreier, L.A.; Zernikow, B.; Stening, K.; Wager, J. Insights into the Frequency and Distinguishing Features of Sleep Disorders in Pediatric Palliative Care Incorporating a Systematic Sleep Protocol. Children 2021, 8, 54. [Google Scholar] [CrossRef]
- Zernikow, B.; Szybalski, K.; Hübner-Möhler, B.; Wager, J.; Paulussen, M.; Lassay, L.; Jorch, N.; Weber, C.; Schneider, D.T.; Janßen, G.; et al. Specialized Pediatric Palliative Care Services for Children Dying from Cancer: A Repeated Cohort Study on the Developments of Symptom Management and Quality of Care over a 10-Year Period. Palliat. Med. 2019, 33, 381–391. [Google Scholar] [CrossRef]
- Oostendorp, L.J.; Rajapakse, D.; Kelly, P.; Crocker, J.; Dinsdale, A.; Fraser, L.; Bluebond-Langner, M. Documentation of Breakthrough Pain in Narrative Clinical Records of Children with Life-Limiting Conditions: Feasibility of a Retrospective Review. J. Child. Health Care 2019, 23, 564–578. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.; Phillips, M.; Hamilton, R.J. Pain Management in the Pediatric Palliative Care Population. J. Nurs. Scholarsh. 2018, 50, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Van Beukering, M.; Velu, A.; van den Berg, L.; Kok, M.; Mol, B.W.; Frings-Dresen, M.; de Leeuw, R.; van der Post, J.; Peute, L. Usability and Usefulness of a Mobile Health App for Pregnancy-Related Work Advice: Mixed-Methods Approach. JMIR Mhealth Uhealth 2019, 7, e11442. [Google Scholar] [CrossRef] [Green Version]
- Martikainen, S.; Kaipio, J.; Lääveri, T. End-User Participation in Health Information Systems (HIS) Development: Physicians’ and Nurses’ Experiences. Int J. Med. Inform. 2020, 137, 104117. [Google Scholar] [CrossRef] [PubMed]
- Lagha, R.R.; Burningham, Z.; Sauer, B.; Leng, J.; Peters, C.; Huynh, T.; Patel, S.; Halwani, A.; Kramer, B. Usability Testing a Potentially Inappropriate Medication Dashboard: A Core Component of the Dashboard Development Process. Appl. Clin. Inform. 2020, 11, 528–534. [Google Scholar] [CrossRef]
- Kaipio, J.; Kuusisto, A.; Hyppönen, H.; Heponiemi, T.; Lääveri, T. Physicians’ and Nurses’ Experiences on EHR Usability: Comparison between the Professional Groups by Employment Sector and System Brand. Int J. Med. Inform. 2020, 134, 104018. [Google Scholar] [CrossRef] [PubMed]
- Dabliz, R.; Poon, S.K.; Ritchie, A.; Burke, R.; Penm, J. Usability Evaluation of an Integrated Electronic Medication Management System Implemented in an Oncology Setting Using the Unified Theory of the Acceptance and Use of Technology. BMC Med. Inform. Decis. 2021, 21, 1–11. [Google Scholar] [CrossRef]
- Kruse, C.S.; Kristof, C.; Jones, B.; Mitchell, E.; Martinez, A. Barriers to Electronic Health Record Adoption: A Systematic Literature Review. J. Med. Syst. 2016, 40, 252. [Google Scholar] [CrossRef] [Green Version]
- Schaaf, J.; Sedlmayr, M.; Sedlmayr, B.; Prokosch, H.-U.; Storf, H. Evaluation of a Clinical Decision Support System for Rare Diseases: A Qualitative Study. BMC Med. Inform. Decis. 2021, 21, 65. [Google Scholar] [CrossRef] [PubMed]
- Richardson, S.; Mishuris, R.; O’Connell, A.; Feldstein, D.; Hess, R.; Smith, P.; McCullagh, L.; McGinn, T.; Mann, D. “Think Aloud” and “Near Live” Usability Testing of Two Complex Clinical Decision Support Tools. Int. J. Med. Inform. 2017, 106, 1–8. [Google Scholar] [CrossRef]
- McDonald, S.; Edwards, H.M.; Zhao, T. Exploring Think-Alouds in Usability Testing: An International Survey. IEEE Trans. Prof. Commun. 2012, 55, 2–19. [Google Scholar] [CrossRef]
- Mazur, L.M.; Mosaly, P.R.; Moore, C.; Marks, L. Association of the Usability of Electronic Health Records with Cognitive Workload and Performance Levels among Physicians. JAMA Netw. Open 2019, 2, e191709. [Google Scholar] [CrossRef] [PubMed]
- Wiebe, N.; Varela, L.O.; Niven, D.J.; Ronksley, P.E.; Iragorri, N.; Quan, H. Evaluation of Interventions to Improve Inpatient Hospital Documentation within Electronic Health Records: A Systematic Review. J. Am. Med. Inform. Assoc. 2019, 26, 1389–1400. [Google Scholar] [CrossRef]



| Sex | n (%) |
|---|---|
| Female | 11 (68.75) |
| Male | 5 (31.25) |
| Age in years (SD) | 42 (12) |
| Profession | |
| Physician | 6 (56.25) |
| Nurse | 10 (43.75) |
| Years of PPC experience | |
| 0–9 | 6 (37.5) |
| 10–20 | 5 (31.25) |
| >20 | 5 (31.25) |
| Years of experience in current position | |
| 0–9 | 13 (81.25) |
| 10–20 | 2 (12.5) |
| >20 | 1 (6.25) |
| Experience in professional use of EMR | 6 (37.5) |
| Experience in professional use of EMR in years | |
| 0–4 | 4 (66.67) |
| 5–8 | 1 (16.76) |
| ≥9 | 1 (16.67) |
| |
|---|---|
| |
|
|
| General view and plus-button | |
|
|
| Vital signs | |
|
|
| Sleep patterns | |
|
|
| Symptom observation | |
|
|
| Catheter management | |
|
|
| Positioning | |
|
|
| Intake and output | |
|
|
| Events | |
| |
| |
| |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kernebeck, S.; Busse, T.S.; Jux, C.; Meyer, D.; Dreier, L.A.; Zenz, D.; Zernikow, B.; Ehlers, J.P. Participatory Design of an Electronic Medical Record for Paediatric Palliative Care: A Think-Aloud Study with Nurses and Physicians. Children 2021, 8, 695. https://0-doi-org.brum.beds.ac.uk/10.3390/children8080695
Kernebeck S, Busse TS, Jux C, Meyer D, Dreier LA, Zenz D, Zernikow B, Ehlers JP. Participatory Design of an Electronic Medical Record for Paediatric Palliative Care: A Think-Aloud Study with Nurses and Physicians. Children. 2021; 8(8):695. https://0-doi-org.brum.beds.ac.uk/10.3390/children8080695
Chicago/Turabian StyleKernebeck, Sven, Theresa Sophie Busse, Chantal Jux, Dorothee Meyer, Larissa Alice Dreier, Daniel Zenz, Boris Zernikow, and Jan Peter Ehlers. 2021. "Participatory Design of an Electronic Medical Record for Paediatric Palliative Care: A Think-Aloud Study with Nurses and Physicians" Children 8, no. 8: 695. https://0-doi-org.brum.beds.ac.uk/10.3390/children8080695