Dental and Dental Hygiene Students’ Knowledge and Capacity to Discriminate the Developmental Defects of Enamel: A Self-Submitted Questionnaire Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Questionnaire
2.3. Statistical Analysis
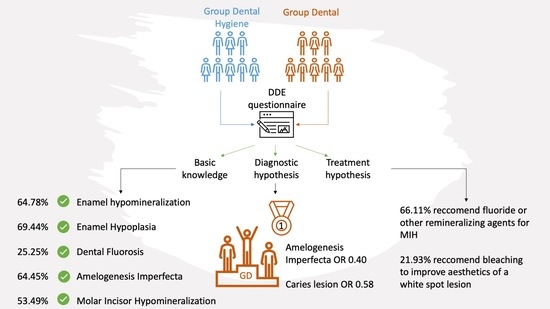
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Seow, W.K. Developmental Defects of Enamel and Dentine: Challenges for Basic Science Research and Clinical Management. Aust. Dent. J. 2014, 59 (Suppl. 1), 143–154. [Google Scholar] [CrossRef] [PubMed]
- Drummond, B.K.; Kilpatrick, N. Planning and Care for Children and Adolescents with Dental Enamel Defects: Etiology, Research and Contemporary Management; Springer: Berlin/Heidelberg, Germany, 2015; ISBN 9783662447994. [Google Scholar]
- Butera, A.; Maiorani, C.; Morandini, A.; Simonini, M.; Morittu, S.; Barbieri, S.; Bruni, A.; Sinesi, A.; Ricci, M.; Trombini, J.; et al. Assessment of Genetical, Pre, Peri and Post Natal Risk Factors of Deciduous Molar Hypomineralization (DMH), Hypomineralized Second Primary Molar (HSPM) and Molar Incisor Hypomineralization (MIH): A Narrative Review. Children 2021, 8, 432. [Google Scholar] [CrossRef]
- Sunderland, E.P.; Smith, C.J.; Sunderland, R. A Histological Study of the Chronology of Initial Mineralization in the Human Deciduous Dentition. Arch. Oral. Biol. 1987, 32, 167–174. [Google Scholar] [CrossRef]
- Salanitri, S.; Seow, W.K. Developmental Enamel Defects in the Primary Dentition: Aetiology and Clinical Management. Aust. Dent. J. 2013, 58, 133–140. [Google Scholar] [CrossRef]
- Caufield, P.W.; Li, Y.; Bromage, T.G. Hypoplasia-Associated Severe Early Childhood Caries-a Proposed Definition. J. Dent. Res. 2012, 91, 544–550. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, J.J.; O’Mullane, D.M. Prevalence of Enamel Defects/Fluorosis in Fluoridated and Non-Fluoridated Areas in Ireland. Commun. Dent. Oral. Epidemiol. 1992, 20, 196–199. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, J.; O’Mullane, D.M. An Epidemiological Index of Developmental Defects of Dental Enamel (DDE Index). Commission on Oral Health, Research and Epidemiology. Int. Dent. J. 1982, 32, 159–167. [Google Scholar]
- Mohamed, A.R.; Thomson, W.M.; MacKay, T.D. An Epidemiological Comparison of Dean’s Index and the Developmental Defects of Enamel (DDE) Index. J. Public Health Dent. 2010, 70, 344–347. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, J.; O’mullane, D. A Modified DDE Index for Use in Epidemiological Studies of Enamel Defects. J. Dent. Res. 1989, 68, 445–450. [Google Scholar] [CrossRef]
- Banks, P.A.; Richmond, S. Enamel Sealants: A Clinical Evaluation of Their Value during Fixed Appliance Therapy. Eur. J. Orthod. 1994, 16, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Dabiri, D.; Eckert, G.J.; Li, Y.; Seow, K.; Schroth, R.J.; Warren, J.; Wright, J.T.; Zhao, S.; Fontana, M. Diagnosing Developmental Defects of Enamel: Pilot Study of Online Training and Accuracy. Pediatr. Dent. 2018, 40, 105–109. [Google Scholar] [PubMed]
- Negre-Barber, A.; Montiel-Company, J.M.; Catalá-Pizarro, M.; Almerich-Silla, J.M. Degree of Severity of Molar Incisor Hypomineralization and Its Relation to Dental Caries. Sci. Rep. 2018, 8, 1248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MIUR Ministerial Acts. Available online: http://attiministeriali.miur.it/media/155598/dmcdl_magistrale.pdf (accessed on 22 May 2022).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [CrossRef] [Green Version]
- MIUR Ministerial Act N236/26062020. Available online: https://www.miur.gov.it/-/decreto-ministeriale-n-236-del-26-06-2020-definizione-dei-posti-disponibili-per-le-immatricolazioni-ai-corsi-di-laurea-magistrale-a-ciclo-unico-in-odo (accessed on 21 April 2022).
- MIUR Ministerial Act 616/08072019. Available online: https://www.miur.gov.it/-/definizione-dei-posti-disponibili-per-le-immatricolazioni-ai-corsi-di-laurea-triennale-delle-professioni-sanitarie-a-a-2019-2020 (accessed on 21 April 2022).
- Rozier, R.G. Epidemiologic Indices for Measuring the Clinical Manifestations of Dental Fluorosis: Overview and Critique. Adv. Dent. Res. 1994, 8, 39–55. [Google Scholar] [CrossRef]
- Ekstrand, K.R.; Gimenez, T.; Ferreira, F.R.; Mendes, F.M.; Braga, M.M. The International Caries Detection and Assessment System—ICDAS: A Systematic Review. Caries Res. 2018, 52, 406–419. [Google Scholar] [CrossRef]
- EasyMedStat—Give Wings to Your Clinical Research. Available online: https://www.easymedstat.com/ (accessed on 24 May 2022).
- Suckling, G.W. Developmental Defects of Enamel—Historical and Present-Day Perspectives of Their Pathogenesis. Adv. Dent. Res. 1989, 3, 87–94. [Google Scholar] [CrossRef]
- Massignan, C.; Ximenes, M.; da Silva Pereira, C.; Dias, L.; Bolan, M.; Cardoso, M. Prevalence of Enamel Defects and Association with Dental Caries in Preschool Children. Eur. Arch. Paediatr. Dent. 2016, 17, 461–466. [Google Scholar] [CrossRef]
- Jälevik, B.; Szigyarto-Matei, A.; Robertson, A. The Prevalence of Developmental Defects of Enamel, a Prospective Cohort Study of Adolescents in Western Sweden: A Barn I TAnadvarden (BITA, Children in Dental Care) Study. Eur. Arch. Paediatr. Dent. 2018, 19, 187–195. [Google Scholar] [CrossRef] [Green Version]
- Rugg-Gunn, A.J.; Al-Mohammadi, S.M.; Butler, T.J. Effects of Fluoride Level in Drinking Water, Nutritional Status, and Socio-Economic Status on the Prevalence of Developmental Defects of Dental Enamel in Permanent Teeth in Saudi 14-Year-Old Boys. Caries Res. 1997, 31, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Angelillo, I.F.; Anfosso, R.; Nobile, C.G.A.; Pavia, M. Prevalence of Dental Caries in Schoolchildren in Italy. Eur. J. Epidemiol. 1998, 14, 351–357. [Google Scholar] [CrossRef]
- Craveia, J.; Rouas, P.; Carat, T.; Manton, D.J.; Boileau, M.J.; Garot, E. Knowledge and Management of First Permanent Molars with Enamel Hypomineralization among Dentists and Orthodontists. J. Clin. Pediatr. Dent. 2020, 44, 20–27. [Google Scholar] [CrossRef]
- Baroni, C.; Marchionni, S. MIH Supplementation Strategies: Prospective Clinical and Laboratory Trial. J. Dent. Res. 2011, 90, 371–376. [Google Scholar] [CrossRef]
- Chay, P.L.; Manton, D.J.; Palamara, J.E.A. The Effect of Resin Infiltration and Oxidative Pre-Treatment on Microshear Bond Strength of Resin Composite to Hypomineralised Enamel. Int. J. Paediatr. Dent. 2014, 24, 252–267. [Google Scholar] [CrossRef]
- Fragelli, C.M.B.; de Souza, J.F.; Jeremias, F.; de Cássia Loiola Cordeiro, R.; Santos-Pinto, L. Molar Incisor Hypomineralization (MIH): Conservative Treatment Management to Restore Affected Teeth. Braz. Oral Res. 2015, 29, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Patel, M.; McDonnell, S.T.; Iram, S.; Chan, M.F.W.Y. Amelogenesis Imperfecta—Lifelong Management. Restorative Management of the Adult Patient. Br. Dent. J. 2013, 215, 449–457. [Google Scholar] [CrossRef]
- Alvarez, J.A.; Rezende, K.M.P.C.; Marocho, S.M.S.; Alves, F.B.T.; Celiberti, P.; Ciamponi, A.L. Dental Fluorosis: Exposure, Prevention and Management. Med. Oral. Patol. Oral. Cir. Bucal. 2009, 1, 14–18. [Google Scholar]
- Lupi, S.M.; Pascadopoli, M.; Maiorani, C.; Preda, C.; Trapani, B.; Chiesa, A.; Esposito, F.; Scribante, A.; Butera, A. Oral Hygiene Practice among Hospitalized Patients: An Assessment by Dental Hygiene Students. Healthcare 2022, 10, 115. [Google Scholar] [CrossRef] [PubMed]
- Bontà, G.; Campus, G.; Cagetti, M.G. COVID-19 Pandemic and Dental Hygienists in Italy: A Questionnaire Survey. BMC Health Serv. Res. 2020, 20, 994. [Google Scholar] [CrossRef]

| Items | GDH N = 157 | GD N = 144 | p-Value |
|---|---|---|---|
| Enamel hypomineralization is a …… defect: | |||
| Qualitative | 92 (58.60%) | 103 (71.53%) | 0.03 |
| Quantitative/Both/I don’t know | 65 (41.4%) | 41 (28.47%) | |
| Enamel hypoplasia is a ……. defect: | |||
| Quantitative | 100 (63.69%) | 109 (75.69%) | 0.03 |
| Qualitative/Both/I don’t know | 57 (36.31%) | 35 (24.31%) | |
| When does Dental Fluorosis develop? | |||
| In the pre-eruptive phase | 53 (33.76%) | 23 (15.97%) | <0.01 |
| In the post-eruptive phase/any age/I don’t know | 104 (66.24%) | 121 (84.03%) | |
| Amelogenesis Imperfecta is a condition caused by: | |||
| Genetic factors | 90 (57.32%) | 104 (72.22%) | 0.01 |
| Systemic factors/Multifactorial/viral or bacterial infection/Don’t know | 67 (42.68%) | 40 (27.78%) | |
| When does Amelogenesis Imperfecta develop? | |||
| In the pre-eruptive phase | 117 (74.52%) | 116 (80.56%) | 0.26 |
| In the post-eruptive phase/any age/I don’t know | 40 (25.48%) | 28 (19.44%) | |
| Molar Incisor Hypomineralization is a …… defect: | |||
| Qualitative | 76 (48.41%) | 85 (59.03%) | 0.08 |
| Quantitative/Both/Don’t know | 81 (51.59%) | 59 (40.97%) | |
| When does Molar Incisor Hypomineralization develop? | |||
| In the pre-eruptive phase | 88 (56.05%) | 70 (48.61%) | 0.24 |
| In the post-eruptive phase/any age/I don’t know | 69 (43.95%) | 74 (51.39%) |
| Items | GDH | GD | p-Value |
|---|---|---|---|
| Picture 1: Molar Incisor Hypomineralization | N = 137 | N = 121 | |
| Possible choices | |||
| Molar Incisor Hypomineralization | 83 (60.58%) | 91 (75.21%) | 0.04 |
| Amelogenesis Imperfecta | 24 (17.52%) | 9 (7.44%) | |
| Plaque demineralization | 17 (12.41%) | 13 (10.74%) | |
| Dental Fluorosis | 13 (9.49%) | 8 (6.61%) | |
| I don’t know | 20/157 (12.74%) | 23/144 (15.97%) | |
| The caries risk in this situation is generally: | |||
| High | 98 (71.53%) | 48 (39.67%) | <0.01 |
| Medium | 38 (27.74%) | 68 (56.20%) | |
| Low | 1 (0.73%) | 5 (4.13%) | |
| Which of the following treatments would you recommend? | |||
| Remineralizing products and/or fluoride-based varnish or gel | 119 (86.86%) | 84 (69.42%) | 0.01 |
| Glass-ionomer sealants | 63(45.99%) | 52 (42.98%) | 0.72 |
| Resin-based sealants | 51 (37.23%) | 49 (40.50%) | 0.68 |
| Professional bleaching | 28 (20.44%) | 15 (12.40%) | 0.12 |
| Picture 2: Amelogenesis Imperfecta | N = 131 | N = 135 | |
| Possible choices | |||
| Amelogenesis Imperfecta | 89 (67.94%) | 112 (82.96%) | 0.02 |
| Plaque demineralization | 25 (19.08%) | 10 (7.41%) | |
| Molar Incisor Hypomineralization | 12 (9.16%) | 10 (67.41%) | |
| Dental Fluorosis | 5 (3.82%) | 3 (2.22%) | |
| I don’t know | 26/157 (16.56%) | 9/144(6.25%) | |
| The caries risk in this situation is generally: | |||
| High | 125 (95.42%) | 117(86.67%) | 0.02 |
| Medium | 6 (4.58%) | 16 (11.85%) | |
| Low | 0 (0.00%) | 2 (1.48%) | |
| Which of the following treatments would you recommend? | |||
| Remineralizing products and/or fluoride-based varnish or gel | 100 (76.34%) | 86 (63.7%) | 0.03 |
| Glass-ionomer sealants | 66 (50.38%) | 55 (40.74%) | 0.16 |
| Resin-based sealants | 53 (40.46%) | 41(30.37%) | 0.11 |
| Professional bleaching | 14 (10.69%) | 15 (11.11%) | >0.99 |
| Picture 3: Dental Fluorosis | N = 146 | N = 133 | |
| Possible choices | |||
| Dental Fluorosis | 61 (41.78%) | 46 (34.59%) | 0.01 |
| Plaque demineralization | 46 (31.51%) | 66 (49.62%) | |
| Molar Incisor Hypomineralization | 33 (22.60%) | 18 (13.53%) | |
| Amelogenesis Imperfecta | 6 (4.11%) | 3 (2.26%) | |
| I don’t know | 11/157 (7.01%) | 11/144 (7.64%) | |
| The caries risk in this situation is generally: | |||
| High | 53 (36.30%) | 25 (18.80%) | <0.01 |
| Medium | 71 (48.63%) | 83 (62.41%) | |
| Low | 22 (15.07%) | 25 (18.80%) | |
| Which of the following treatments would you recommend? | |||
| Remineralizing products and/or fluoride-based varnish or gel | 104 (71.23%) | 78 (58.65%) | 0.04 |
| Glass-ionomer sealants | 74 (50.68%) | 70 (52.63%) | 0.84 |
| Resin-based sealants | 88 (60.27%) | 72 (54.14%) | 0.36 |
| Professional bleaching | 31 (21.23%) | 24 (18.05%) | 0.60 |
| Picture 4: White spot lesion | N = 133 | N = 112 | |
| Possible choices | |||
| Plaque demineralization | 54 (40.60%) | 45 (40.18%) | 0.22 |
| Dental Fluorosis | 61 (45.86%) | 60 (53.57%) | |
| Amelogenesis Imperfecta | 11 (8.27%) | 3 (2.68%) | |
| Molar Incisor Hypomineralization | 7 (5.26%) | 4 (3.57%) | |
| I don’t know | 24/157 (15.29%) | 32/144 (22.22%) | |
| The caries risk in this situation is generally: | |||
| High | 62 (46.62%) | 17 (15.18%) | <0.01 |
| Medium | 53 (39.85%) | 62 (55.36%) | |
| Low | 18 (13.53%) | 33 (29.46%) | |
| Which of the following treatment would you recommend? | |||
| Remineralizing products and/or fluoride-based varnish or gel | 91 (68.42%) | 73 (65.18%) | 0.69 |
| Glass-ionomer sealants | 57 (42.86%) | 56 (50.00%) | 0.32 |
| Resin-based sealants | 58 (43.61%) | 68 (60.71%) | 0.01 |
| Professional bleaching | 35 (26.32%) | 21 (18.75%) | 0.21 |
| Picture 5: Caries lesion | N = 121 | N = 104 | |
| Possible choices | |||
| Plaque demineralization | 48 (39.67%) | 65 (62.50%) | <0.01 |
| Molar Incisor Hypomineralization | 67 (55.37%) | 37 (35.58%) | |
| Dental Fluorosis | 4 (3.31%) | 1 (0.96%) | |
| Amelogenesis Imperfecta | 2 (1.65%) | 1 (0.96%) | |
| I don’t know | 36/157 (22.93%) | 40/104 (27.78%) | |
| Which of the following treatments would you recommend? | |||
| Remineralizing products and/or fluoride-based varnish or gel | 91 (75.21%) | 76 (73.08%) | 0.83 |
| Glass-ionomer sealants | 86 (71.07%) | 66 (63.46%) | 0.28 |
| Resin-based sealants | 71 (58.68%) | 71 (68.27%) | 0.18 |
| Professional bleaching | 9 (7.44%) | 15 (14.42%) | 0.14 |
| For each clinical pictures’ comparison analysis, the answer “I don’t know” was excluded | |||
| Ref: Group of students in Dentistry (GD) | ||
|---|---|---|
| Clinical Pictures | Odds Ratio | p-Value |
| 0.93 [0.56;1.54] | 0.77 |
| 0.40 [0.23;0.69] | <0.01 |
| 1.38 [0.81;2.35] | 0.23 |
| 1.30 [0.75;2.24] | 0.35 |
| 0.58 [0.34;0.94] | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cagetti, M.G.; Salerno, C.; Bontà, G.; Bisanti, A.; Maspero, C.; Tartaglia, G.M.; Campus, G. Dental and Dental Hygiene Students’ Knowledge and Capacity to Discriminate the Developmental Defects of Enamel: A Self-Submitted Questionnaire Survey. Children 2022, 9, 1759. https://0-doi-org.brum.beds.ac.uk/10.3390/children9111759
Cagetti MG, Salerno C, Bontà G, Bisanti A, Maspero C, Tartaglia GM, Campus G. Dental and Dental Hygiene Students’ Knowledge and Capacity to Discriminate the Developmental Defects of Enamel: A Self-Submitted Questionnaire Survey. Children. 2022; 9(11):1759. https://0-doi-org.brum.beds.ac.uk/10.3390/children9111759
Chicago/Turabian StyleCagetti, Maria Grazia, Claudia Salerno, Giuliana Bontà, Anna Bisanti, Cinzia Maspero, Gianluca Martino Tartaglia, and Guglielmo Campus. 2022. "Dental and Dental Hygiene Students’ Knowledge and Capacity to Discriminate the Developmental Defects of Enamel: A Self-Submitted Questionnaire Survey" Children 9, no. 11: 1759. https://0-doi-org.brum.beds.ac.uk/10.3390/children9111759