Impact of COVID-19 Pandemic on Children Visiting Emergency Department for Mental Illness: A Multicenter Database Analysis from Korea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Selection of Participants
2.3. Measurements
2.4. Patient and Public Involvement
2.5. Statistical Analysis
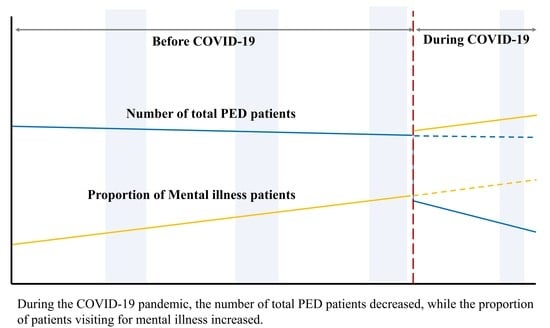
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, P.; Yang, X.L.; Wang, X.G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.R.; Zhu, Y.; Li, B.; Huang, C.L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 2 August 2021).
- Ministry of Health and Welfare. Strong Social Distancing for 15 Days, the Government Will Take the Lead!—Main Contents and Guidelines. Available online: http://ncov.mohw.go.kr/shBoardView.do?brdId=2&brdGubun=27&ncvContSeq=1385 (accessed on 1 December 2021).
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Wang, Y.; Wang, H.; Liu, Z.; Yu, X.; Yan, J.; Yu, Y.; Kou, C.; Xu, X.; Lu, J.; et al. Prevalence of mental disorders in China: A cross-sectional epidemiological study. Lancet Psychiatry 2019, 6, 211–224. [Google Scholar] [CrossRef]
- Lee, S.Y.; Ro, Y.S.; Jeong, J.; Shin, S.D.; Moon, S. Impact of the COVID-19 Pandemic on the Incidence and Characteristics of Patients with Psychiatric Illnesses Visiting Emergency Departments in Korea. J. Clin. Med. 2022, 11, 488. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Otto, C.; Devine, J.; Löffler, C.; Hurrelmann, K.; Bullinger, M.; Barkmann, C.; Siegel, N.A.; et al. Quality of life and mental health in children and adolescents during the first year of the COVID-19 pandemic: Results of a two-wave nationwide population-based study. Eur. Child. Adolesc. Psychiatry 2021, 1–14. [Google Scholar] [CrossRef]
- Tang, S.; Xiang, M.; Cheung, T.; Xiang, Y.-T. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J. Affect. Disord. 2021, 279, 353–360. [Google Scholar] [CrossRef]
- Rogers, A.A.; Ha, T.; Ockey, S. Adolescents’ Perceived Socio-Emotional Impact of COVID-19 and Implications for Mental Health: Results From a U.S.-Based Mixed-Methods Study. J. Adolesc. Health 2021, 68, 43–52. [Google Scholar] [CrossRef]
- Bhatia, G.; Chatterjee, B.; Dhawan, A. Adolescents, Drugs, and COVID-19: Special Challenges during the Pandemic. Indian J. Psychol. Med. 2021, 43, 95–99. [Google Scholar] [CrossRef]
- Lim, T.; Park, J.; Je, S. Pediatric Korean Triage and Acuity Scale. Pediatr. Emerg. Med. J. 2015, 2, 53–58. [Google Scholar] [CrossRef]
- Warren, D.W.; Jarvis, A.; LeBlanc, L.; Gravel, J. Revisions to the Canadian Triage and Acuity Scale paediatric guidelines (PaedCTAS). Can. J. Emerg. Med. 2008, 10, 224–243. [Google Scholar] [CrossRef]
- Statistics Korea. The 7th Korean Standard Disease Classification (KCD-7) Revision and Announcement. Available online: http://www.kostat.go.kr/portal/korea/kor_nw/1/15/index.board?bmode=read&aSeq=346904 (accessed on 1 December 2021).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems (ICD). Available online: https://www.who.int/standards/classifications/classification-of-diseases (accessed on 1 December 2021).
- Choi, D.H.; Jung, J.Y.; Suh, D.; Choi, J.Y.; Lee, S.U.; Choi, Y.J.; Kwak, Y.H.; Kim, D.K. Impact of the COVID-19 Outbreak on Trends in Emergency Department Utilization in Children: A Multicenter Retrospective Observational Study in Seoul Metropolitan Area, Korea. J. Korean Med. Sci. 2021, 36, e44. [Google Scholar] [CrossRef] [PubMed]
- Jang, K.M.; Ahn, J.Y.; Choi, H.J.; Lee, S.; Kim, D.; Lee, D.W.; Choe, J.Y. Pediatric Emergency Department Utilization and Coronavirus Disease in Daegu, Korea. J. Korean Med. Sci. 2021, 36, e11. [Google Scholar] [CrossRef] [PubMed]
- Krass, P.; Dalton, E.; Doupnik, S.K.; Esposito, J. US Pediatric Emergency Department Visits for Mental Health Conditions During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e218533. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Marques de Miranda, D.; da Silva Athanasio, B.; Sena Oliveira, A.C.; Simoes-e-Silva, A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduct. 2020, 51, 101845. [Google Scholar] [CrossRef]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112–118. [Google Scholar] [CrossRef]
- Wan, W.Y.; Thoon, K.C.; Loo, L.H.; Chan, K.S.; Oon, L.L.E.; Ramasamy, A.; Maiwald, M. Trends in Respiratory Virus Infections During the COVID-19 Pandemic in Singapore, 2020. JAMA Netw. Open 2021, 4, e2115973. [Google Scholar] [CrossRef]
- Sheridan, G.A.; Nagle, M.; Russell, S.; Varghese, S.; O’Loughlin, P.F.; Boran, S.; Taylor, C.; Harty, J.A. Pediatric Trauma and the COVID-19 Pandemic: A 12-Year Comparison in a Level-1 Trauma Center. HSS J. 2020, 16 (Suppl. 1), 92–96. [Google Scholar] [CrossRef]
- Kalb, L.G.; Stapp, E.K.; Ballard, E.D.; Holingue, C.; Keefer, A.; Riley, A. Trends in Psychiatric Emergency Department Visits Among Youth and Young Adults in the US. Pediatrics 2019, 143, e20182192. [Google Scholar] [CrossRef]
- Mojtabai, R.; Olfson, M.; Han, B. National Trends in the Prevalence and Treatment of Depression in Adolescents and Young Adults. Pediatrics 2016, 138, e20161878. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M.; Joiner, T.E.; Rogers, M.L.; Martin, G.N. Increases in Depressive Symptoms, Suicide-Related Outcomes, and Suicide Rates Among U.S. Adolescents After 2010 and Links to Increased New Media Screen Time. Clin. Psychol. Sci. 2018, 6, 3–17. [Google Scholar] [CrossRef]
- Lee, R.D.; Chen, J. Adverse childhood experiences, mental health, and excessive alcohol use: Examination of race/ethnicity and sex differences. Child Abus. Negl. 2017, 69, 40–48. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Adolescent Mental Health. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed on 7 December 2021).
- Kessler, R.C.; Angermeyer, M.; Anthony, J.C.; de Graaf, R.; Demyttenaere, K.; Gasquet, I.; de Girolamo, G.; Gluzman, S.; Gureje, O.; Haro, J.M.; et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007, 6, 168–176. [Google Scholar] [PubMed]
- World Health Organization. Growing Up Unequal: Gender and Socioeconomic Differences in Young People’ s Health and Well-Being. Available online: https://apps.who.int/iris/handle/10665/326320 (accessed on 7 December 2021).
- Schwarz, S.W. Adolescent Mental Health in the United States: Facts for Policymakers; National Center for Children in Poverty: New York, NY, USA, 2009. [Google Scholar]
- Yang, L.; Zhao, Y.; Wang, Y.; Liu, L.; Zhang, X.; Li, B.; Cui, R. The Effects of Psychological Stress on Depression. Curr. Neuropharmacol. 2015, 13, 494–504. [Google Scholar] [CrossRef]
- Uchida, S.; Hara, K.; Kobayashi, A.; Otsuki, K.; Yamagata, H.; Hobara, T.; Suzuki, T.; Miyata, N.; Watanabe, Y. Epigenetic status of Gdnf in the ventral striatum determines susceptibility and adaptation to daily stressful events. Neuron 2011, 69, 359–372. [Google Scholar] [CrossRef]
- Washington, T.D. Psychological stress and anxiety in middle to late childhood and early adolescence: Manifestations and management. J. Pediatr. Nurs. 2009, 24, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Mohler-Kuo, M.; Dzemaili, S.; Foster, S.; Werlen, L.; Walitza, S. Stress and Mental Health among Children/Adolescents, Their Parents, and Young Adults during the First COVID-19 Lockdown in Switzerland. Int. J. Environ. Res. Public Health 2021, 18, 4668. [Google Scholar] [CrossRef]
- Mullen, S. Major depressive disorder in children and adolescents. Ment. Health Clin. 2018, 8, 275–283. [Google Scholar] [CrossRef]
- Akampurira, D. Stress, Depression and Substance Abuse among Adolescents. Available online: http://hdl.handle.net/20.500.12281/10230 (accessed on 5 December 2021).
- Charles, N.E.; Mathias, C.W.; Acheson, A.; Bray, B.C.; Ryan, S.R.; Lake, S.L.; Liang, Y.; Dougherty, D.M. Increased Pre- and Early-Adolescent Stress in Youth with a Family History of Substance Use Disorder and Early Substance Use Initiation. J. Youth Adolesc. 2015, 44, 1954–1967. [Google Scholar] [CrossRef]



| Variables | 2017–2019 | 2020 | p |
|---|---|---|---|
| Total PED visits | 84,790 | 14,883 | NA |
| Total mental illness patient visits | 657 (0.77) | 188 (1.26) | <0.001 a |
| Weekly visits, mean ± SD | 4.2 ± 2.4 | 3.6 ± 1.8 | 0.05 b |
| Age | |||
| 5–9 years | 48 (7.31) | 12 (6.83) | 0.55 a |
| 10–14 years | 172 (26.18) | 43 (22.87) | |
| 15–17 years | 437 (66.51) | 133 (70.74) | |
| Sex | |||
| Female | 450 (68.49) | 130 (69.15) | 0.93 a |
| KTAS level | |||
| 1 | 4 (0.61) | 3 (1.60) | 0.08 a |
| 2 | 41 (6.24) | 8 (4.26) | |
| 3 | 262 (39.88) | 93 (49.47) | |
| 4 | 321 (48.86) | 78 (41.49) | |
| 5 | 29 (4.41) | 6 (3.19) | |
| Mode of arrival | |||
| Self-referred | 607 (92.39) | 170 (90.43) | 0.25 a |
| Referred from clinic | 43 (6.54) | 13 (6.91) | |
| Outpatient department | 7 (1.07) | 5 (2.66) | |
| Disposition | |||
| Admission | 122 (18.57) | 33 (17.55) | 0.83 a |
| Variables | 2017–2019 (N = 84,790) | 2020 (N = 14,833) | p |
|---|---|---|---|
| Total mental illness | 657 (0.77) | 188 (1.26) | <0.001 |
| Anxiety disorders | 100 (0.12) | 32 (0.22) | <0.05 |
| Mood disorders | 39 (0.05) | 17 (0.11) | <0.05 |
| Somatoform disorders | 73 (0.09) | 24 (0.16) | <0.05 |
| Developmental disorders | 15 (0.02) | 6 (0.04) | 0.078 |
| Schizophrenia and other psychotic disorders | 14 (0.02) | 3 (0.02) | 0.749 |
| Alcohol-related disorders | 60 (0.07) | 10 (0.07) | 0.887 |
| Substance-related disorders | 265 (0.31) | 78 (0.53) | <0.001 |
| Intentional self-harm | 28 (0.03) | 8 (0.05) | 0.216 |
| Miscellaneous | 63 (0.07) | 10 (0.07) | 0.775 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, W.; Choi, A.; Byun, S.; Kim, K.; Kim, S. Impact of COVID-19 Pandemic on Children Visiting Emergency Department for Mental Illness: A Multicenter Database Analysis from Korea. Children 2022, 9, 1208. https://0-doi-org.brum.beds.ac.uk/10.3390/children9081208
Bae W, Choi A, Byun S, Kim K, Kim S. Impact of COVID-19 Pandemic on Children Visiting Emergency Department for Mental Illness: A Multicenter Database Analysis from Korea. Children. 2022; 9(8):1208. https://0-doi-org.brum.beds.ac.uk/10.3390/children9081208
Chicago/Turabian StyleBae, Woori, Arum Choi, Seonjeong Byun, Kyunghoon Kim, and Sukil Kim. 2022. "Impact of COVID-19 Pandemic on Children Visiting Emergency Department for Mental Illness: A Multicenter Database Analysis from Korea" Children 9, no. 8: 1208. https://0-doi-org.brum.beds.ac.uk/10.3390/children9081208