A One-Year, Multicenter, Retrospective Evaluation of Narrow and Low-Profile Abutments Used to Rehabilitate Complete Edentulous Lower Arches: The OT Bridge Concept
Abstract
:1. Introduction
2. Materials and Methods
- Implant failure was defined as mobility, infection, fracture, and/or any other mechanical or biological issue that determined its removal.
- A prosthesis was considered a failure any time it had to be replaced.
- Any biological (e.g., drug-resistant pain, swelling, excessive marginal bone loss, suppuration, etc.) and/or technical (e.g., fracture of the veneering material and or framework, screw loosening, etc.) complications were recorded during follow-up.
- Marginal bone levels were measured as the distance between the implant platform to the first bone to implant contact. Mean values of mesial and distal measurements were calculated for each implant. Marginal bone level was measured on digital periapical radiographic images obtained by parallel technique with Rinn’s film holder (Rinn XCP, Dentsply, Elgin, IL, USA) taken at definitive implant loading (baseline) and then one year after. All radiographs were analyzed through a dedicate software (DFW2.8 for Windows, Soredex, Tuuka, Finland), calibrated for each image using the known distance between two consecutive threads. The difference between baseline and last follow-up was taken as marginal bone loss. One dentist at each center, not previously involved in this study, performed every radiographic measurement.
- Bleeding index and plaque index were evaluated in six sites around each implant–abutment interface at the one-year examination with a periodontal probe (PCPUNC156, Hu-Friedy, Milan, Italy). One dental hygienist at each center, not previously involved in this study, performed the periodontal measurements
- Oral Health Impact Profile (OHIP-21) was calculated with a questionnaire of 21 questions, divided in seven subscales (functional limitations, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap), consisting of two to four questions each, filled out by patients. Patients were instructed to choose between five possible responses ranging from 1 (never) to 5 (very often). The questionnaire was administered by an independent dentist before treatment and one year after definitive prosthesis delivery.
3. Statistical Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Scrascia, R.; Fiorillo, L.; Gaita, V.; Secondo, L.; Nicita, F.; Cervino, G. Implant-Supported Prosthesis for Edentulous Patient Rehabilitation. From Temporary Prosthesis to Definitive with a New Protocol: A Single Case Report. Prosthesis 2020, 2, 10–24. [Google Scholar] [CrossRef] [Green Version]
- Pozzi, A.; Tallarico, M.; Moy, P. Four-implant overdenture fully supported by a CAD-CAM titanium bar: A single-cohort prospective 1-year preliminary study. J. Prosthet. Dent. 2016, 116, 516–523. [Google Scholar] [CrossRef] [Green Version]
- Tallarico, M.; Meloni, S.; Canullo, L.; Caneva, M.; Polizzi, G. Five-Year Results of a Randomized Controlled Trial Comparing Patients Rehabilitated with Immediately Loaded Maxillary Cross-Arch Fixed Dental Prosthesis Supported by Four or Six Implants Placed Using Guided Surgery. Clin. Implant Dent. Relat. Res. 2016, 18, 965–972. [Google Scholar] [CrossRef]
- Tallarico, M.; Caneva, M.; Meloni, S.; Xhanari, E.; Covani, U.; Canullo, L. Definitive Abutments Placed at Implant Insertion and Never Removed: Is It an Effective Approach? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Oral Maxillofac. Surg. 2018, 76, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Caneva, M.; Baldini, N.; Gatti, F.; Duvina, M.; Billi, M.; Iannello, G.; Piacentini, G.; Meloni, S.M.; Cicciù, M. Patient-centered rehabilitation of single, partial, and complete edentulism with cemented- or screw-retained fixed dental prosthesis: The First Osstem Advanced Dental Implant Research and Education Center Consensus Conference 2017. Eur. J. Dent. 2018, 12, 617. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Esposito, M.; Xhanari, E.; Caneva, M.; Meloni, S.M. Computer-guided vs free-hand placement of immediately loaded dental implants: 5-year postloading results of a randomised controlled trial. Eur. J. Oral Implant. 2018, 11, 203–213. [Google Scholar]
- Tallarico, M.; Meloni, S. Retrospective Analysis on Survival Rate, Template-Related Complications, and Prevalence of Peri-implantitis of 694 Anodized Implants Placed Using Computer-Guided Surgery: Results Between 1 and 10 Years of Follow-Up. Int. J. Oral Maxillofac. Implant. 2017, 32, 1162–1171. [Google Scholar] [CrossRef]
- Tallarico, M.; Meloni, S.M.; Canullo, L.; Xhanari, E.; Polizzi, G. Guided surgery for single-implant placement: A critical review. J. Oral Sci. Rehabil. 2016, 2, 8–14. [Google Scholar]
- Tallarico, M.; Martinolli, M.; Kim, Y.-J.; Cocchi, F.; Meloni, S.M.; Alushi, A.; Xhanari, E. Accuracy of Computer-Assisted Template-Based Implant Placement Using Two Different Surgical Templates Designed with or without Metallic Sleeves: A Randomized Controlled Trial. Dent. J. 2019, 7, 41. [Google Scholar] [CrossRef] [Green Version]
- Tallarico, M.; Kim, Y.-J.; Cocchi, F.; Martinolli, M.; Meloni, S.M. Accuracy of newly developed sleeve-designed templates for insertion of dental implants: A prospective multicenters clinical trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 108–113. [Google Scholar] [CrossRef] [Green Version]
- Tallarico, M.; Ceruso, F.; Xhanari, E.; Gargari, M.; Canullo, L.; Meloni, S. Immediately loaded tilted implants combined with angulated screw channel zirconia abutments in atrophic maxillary patients: A three-year after loading prospective case series study. ORAL Implantol. 2018, 11, 106–114. [Google Scholar]
- Tallarico, M.; Fiorellini, J.; Nakajima, Y.; Omori, Y.; Takeshi, I.; Canullo, L. Mechanical Outcomes, Microleakage, and Marginal Accuracy at the Implant-Abutment Interface of Original versus Nonoriginal Implant Abutments: A Systematic Review of In Vitro Studies. BioMed Res. Int. 2018, 2018, 2958982. [Google Scholar] [CrossRef] [Green Version]
- Pozzi, A.; Tallarico, M.; Moy, P.K. Three-year post-loading results of a randomised, controlled, split-mouth trial comparing implants with different prosthetic interfaces and design in partially posterior edentulous mandibles. Eur. J. Oral Implant. 2014, 7, 47–61. [Google Scholar]
- Pozzi, A.; Agliardi, E.; Tallarico, M.; Barlattani, A. Clinical and Radiological Outcomes of Two Implants with Different Prosthetic Interfaces and Neck Configurations: Randomized, Controlled, Split-Mouth Clinical Trial. Clin. Implant. Dent. Relat. Res. 2014, 16, 96–106. [Google Scholar] [CrossRef]
- Meloni, S.M.; Lumbau, A.; Baldoni, E.; Pisano, M.; Spano, G.; Massarelli, O.; Tallarico, M. Platform switching versus regular platform single implants: 5-year post-loading results from a randomised controlled trial. Int. J. Oral Implantol. 2020, 13, 43–52. [Google Scholar]
- Meloni, S.M.; Tallarico, M.; Pisano, M.; Xhanari, E.; Canullo, L. Immediate Loading of Fixed Complete Denture Prosthesis Supported by 4–8 Implants Placed Using Guided Surgery: A 5-Year Prospective Study on 66 Patients with 356 Implants. Clin. Implant. Dent. Relat. Res. 2017, 19, 195–206. [Google Scholar] [CrossRef]
- Tallarico, M.; Scrascia, R.; Annucci, M.; Meloni, S.M.; Lumbau, A.I.; Koshovari, A.; Xhanari, E.; Martinolli, M. Errors in Implant Positioning Due to Lack of Planning: A Clinical Case Report of New Prosthetic Materials and Solutions. Materials 2020, 13, 1883. [Google Scholar] [CrossRef] [Green Version]
- Xhanari, E.; Scrascia, R.; Kadiu, B.; Tallarico, M. Two implants sup- porting a mandibular over-denture to rehabilitate Cawood and Howell Class V and VI patients: A proof-of-concept study. J. Oral Sci. Rehabil. 2017, 3, 52–59. [Google Scholar]
- Tallarico, M.; Ortensi, L.; Martinolli, M.; Casucci, A.; Ferrari, E.; Malaguti, G.; Montanari, M.; Scrascia, R.; Vaccaro, G.; Venezia, P.; et al. Multicenter Retrospective Analysis of Implant Overdentures Delivered with Different Design and Attachment Systems: Results Between One and 17 Years of Follow-Up. Dent. J. 2018, 6, 71. [Google Scholar] [CrossRef] [Green Version]
- Pozzi, A.; Tallarico, M.; Mangani, F.; Barlattani, A. Different implant impression techniques for edentulous patients treated with CAD/CAM complete-arch prostheses: A randomised controlled trial reporting data at 3 year post-loading. Eur. J. Oral Implant. 2013, 6, 325–340. [Google Scholar]
- Abduo, J.; Bennani, V.; Waddell, N.; Lyons, K.; Swain, M. Assessing the fit of implant fixed prostheses: A critical review. Int. J. Oral Maxillofac. Implant. 2010, 25, 506–515. [Google Scholar]
- Galindo-Moreno, P.; Leon-Cano, A.; Monje, A.; Ortega-Oller, I.; O’Valle, F.; Catena, A. Abutment height influences the effect of platform switching on peri-implant marginal bone loss. Clin. Oral Implant. Res. 2016, 27, 167–173. [Google Scholar] [CrossRef]
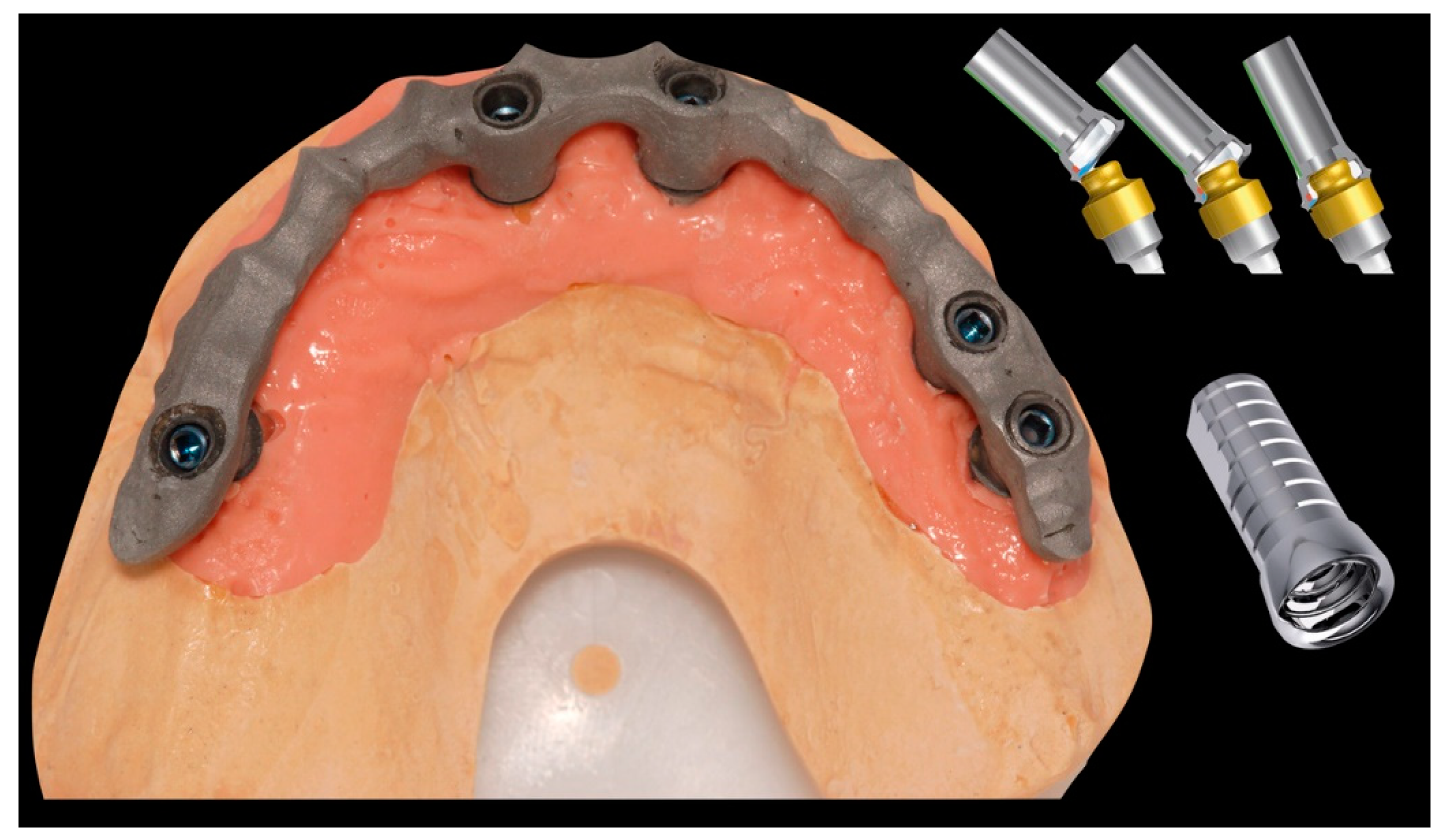
- Acampora, R.; Montanari, M.; Scrascia, R.; Ferrari, E.; Pasi, M.; Cervino, G.; Meloni, S.; Lum-bau, A.; Erta, X.; Koshovari, A.; et al. 1-Year Evaluation of OT Bridge Abutments for Immediately Loaded Maxillary Fixed Restorations: A Multicenter Study. Eur. J. Dent. 2020. Ahead of Print. [Google Scholar] [CrossRef]
- Montanari, M.; Bonato, G.; Ortensi, L. Oral Rehabilitation with Implant-Supported Overden-ture and a New Protocol for Bar Passivation. Global J. Oral Sci. 2016, 2, 10–19. [Google Scholar]
- Cervino, G.; Cicciù, M.; Fedi, S.; Milone, D.; Fiorillo, L. FEM Analysis Applied to OT Bridge Abutment with Seeger Retention System. Eur. J. Dent. 2020. Epub Ahead of Print, PMID: 32869222. [Google Scholar] [CrossRef]
- Ceruti, P.; Mobilio, N.; Bellia, E.; Borracchini, A.; Catapano, S.; Gassino, G. Simplified edentulous treatment: A multicenter randomized controlled trial to evaluate the timing and clinical outcomes of the technique. J. Prosthet. Dent. 2017, 118, 462–467. [Google Scholar] [CrossRef]
- Mobilio, N.; Catapano, S. The use of monolithic lithium disilicate for posterior screw-retained implant crowns. J. Prosthet. Dent. 2017, 118, 703–705. [Google Scholar] [CrossRef]
- Mobilio, N.; Fasiol, A.; Catapano, S. Survival Rates of Lithium Disilicate Single Restorations: A Retrospective Study. Int. J. Prosthodont. 2018, 31, 283–286. [Google Scholar] [CrossRef]




| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Aged 18 years or older | General contraindications for oral surgery |
| Signed informed consent | Heavy smokers (≥11 cigarettes per day) |
| OT Bridge in the mandible arch | Poor oral hygiene (Bleeding on Probing > 25%) |
| Screw-retained prosthetic retention | Local acute or chronic infections |
| One-year after loading follow-up (FU) | Substance abuse (drugs or alcohol) |
| Available radiographs (implant loading and 1-year FU) | Psychiatric problems |
| Pregnancy or breastfeeding | |
| Treatment with intravenous bisphosphonates | |
| Irradiation of the neck or head area in the past 5 years | |
| Absence of teeth in the opposite arch | |
| Severe bruxism or jaw clenching |
| Implant Placement (mm) | 1-Year After Loading (mm) | Difference (mm) | |
|---|---|---|---|
| Marginal bone | 0.05 ± 0.07 | 0.32 ± 0.2 | 0.27 ± 0.14 |
| Bleeding on probing | 8.9% | ||
| 5.8% | |||
| 87.7 ± 6.00 | 23.6 ± 1.2 | 64.1 ± 7.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montanari, M.; Scrascia, R.; Cervino, G.; Pasi, M.; Ferrari, E.; Xhanari, E.; Koshovari, A.; Tallarico, M. A One-Year, Multicenter, Retrospective Evaluation of Narrow and Low-Profile Abutments Used to Rehabilitate Complete Edentulous Lower Arches: The OT Bridge Concept. Prosthesis 2020, 2, 352-361. https://0-doi-org.brum.beds.ac.uk/10.3390/prosthesis2040033
Montanari M, Scrascia R, Cervino G, Pasi M, Ferrari E, Xhanari E, Koshovari A, Tallarico M. A One-Year, Multicenter, Retrospective Evaluation of Narrow and Low-Profile Abutments Used to Rehabilitate Complete Edentulous Lower Arches: The OT Bridge Concept. Prosthesis. 2020; 2(4):352-361. https://0-doi-org.brum.beds.ac.uk/10.3390/prosthesis2040033
Chicago/Turabian StyleMontanari, Marco, Roberto Scrascia, Gabriele Cervino, Massimo Pasi, Emiliano Ferrari, Erta Xhanari, Alba Koshovari, and Marco Tallarico. 2020. "A One-Year, Multicenter, Retrospective Evaluation of Narrow and Low-Profile Abutments Used to Rehabilitate Complete Edentulous Lower Arches: The OT Bridge Concept" Prosthesis 2, no. 4: 352-361. https://0-doi-org.brum.beds.ac.uk/10.3390/prosthesis2040033







