A Systematic Review of the Efficacy of Repetitive Transcranial Magnetic Stimulation Treatment for Women with Postpartum Depression
Abstract
:1. Introduction
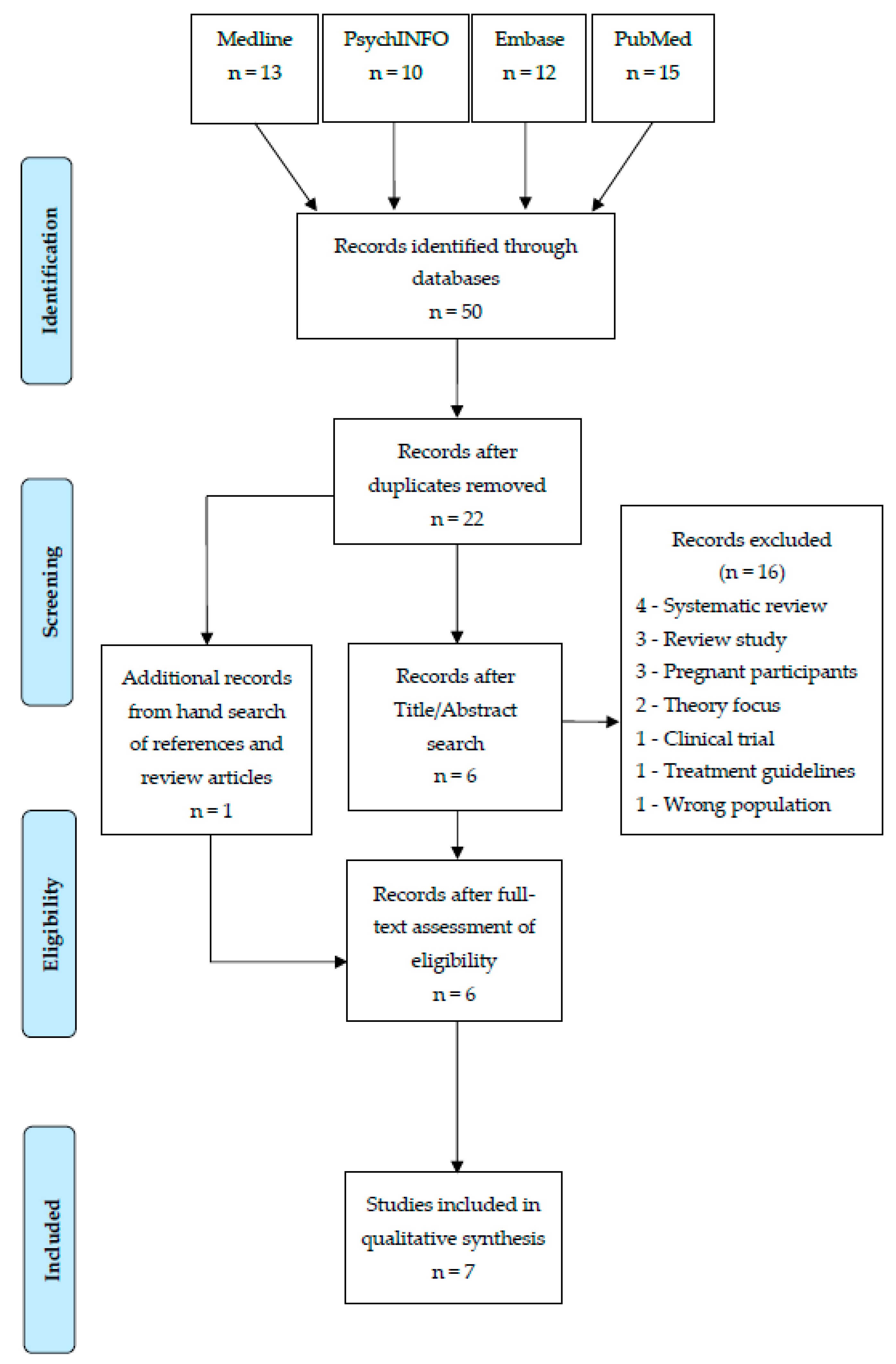
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Quality Assessment
2.4. Data Analysis
3. Results
3.1. Description of Studies
3.2. Clinical Psychiatric Outcomes
3.3. Social-Relational Outcomes
3.4. Neuropsychological Testing
3.5. Side Effects
4. Discussions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gavin, N.; Gaynes, B.; Lohr, K.; Meltzer-Brody, S.; Gartlehner, G.; Swinson, T. Perinatal Depression. Obstet. Gynecol. 2005, 106, 1071–1083. [Google Scholar] [CrossRef]
- Almond, P. Postnatal depression: A global public health perspective. Perspect. Public Health 2009, 129, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Kirmayer, L.; Gómez-Carrillo, A. Agency, embodiment and enactment in psychosomatic theory and practice. Med. Humanit. 2019, 45, 169–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia, K.; Flynn, P.; Pierce, K.; Caudle, M. Repetitive transcranial magnetic stimulation treats postpartum depression. Brain Stimul. 2010, 3, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Ganho-Ávila, A.; Poleszczyk, A.; Mohamed, M.; Osório, A. Efficacy of Rtms in Decreasing Postnatal Depression Symptoms: A Systematic Review. Psychiatry Res. 2019, 279, 315–322. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Wisner, K.; Sit, D.; McShea, M.; Rizzo, D.; Zoretich, R.; Hughes, C.; Eng, H.; Luther, J.; Wisniewski, S.; Costantino, M.; et al. Onset Timing, Thoughts of Self-Harm, and Diagnoses in Postpartum Women with Screen-Positive Depression Findings. JAMA Psychiatry 2013, 70, 490. [Google Scholar] [CrossRef]
- Woody, C.; Ferrari, A.; Siskind, D.; Whiteford, H.; Harris, M. A Systematic Review and Meta-Regression of The Prevalence and Incidence of Perinatal Depression. J. Affect. Disord. 2017, 219, 86–92. [Google Scholar] [CrossRef] [Green Version]
- Semkovska, M.; McLoughlin, D. Objective Cognitive Performance Associated with Electroconvulsive Therapy for Depression: A Systematic Review and Meta-Analysis. Biol. Psychiatry 2010, 68, 568–577. [Google Scholar] [CrossRef]
- Semkovska, M.; Noone, M.; Carton, M.; McLoughlin, D. Measuring Consistency of Autobiographical Memory Recall in Depression. Psychiatry Res. 2012, 197, 41–48. [Google Scholar] [CrossRef]
- Guille, C.; Newman, R.; Fryml, L.; Lifton, C.; Epperson, C. Management of Postpartum Depression. J. Midwifery Womens Health 2013, 58, 643–653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parsons, C.; Young, K.; Rochat, T.; Kringelbach, M.; Stein, A. Postnatal Depression and Its Effects on Child Development: A Review of Evidence from Low- and Middle-Income Countries. Br. Med. Bull. 2011, 101, 57–79. [Google Scholar] [CrossRef] [PubMed]
- Sockol, L.; Epperson, C.; Barber, J. A Meta-Analysis of Treatments for Perinatal Depression. Clin. Psychol. Rev. 2011, 31, 839–849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Ravesteyn, L.; Lambregtse-van den Berg, M.; Hoogendijk, W.; Kamperman, A. Interventions to Treat Mental Disorders During Pregnancy: A Systematic Review and Multiple Treatment Meta-Analysis. PLoS ONE 2017, 12, e0173397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacQueen, G.; Frey, B.; Ismail, Z.; Jaworska, N.; Steiner, M.; Lieshout, R.; Kennedy, S.; Lam, R.; Milev, R.; Parikh, S.; et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults With Major Depressive Disorder. Can. J. Psychiatry 2016, 61, 588–603. [Google Scholar] [CrossRef] [Green Version]
- De Crescenzo, F.; Perelli, F.; Armando, M.; Vicari, S. Selective Serotonin Reuptake Inhibitors (Ssris) for Post-Partum Depression (PPD): A Systematic Review of Randomized Clinical Trials. J. Affect. Disord. 2014, 152–154, 39–44. [Google Scholar] [CrossRef]
- Sharma, V.; Sommerdyk, C.; Xie, B.; Campbell, K. Pharmacotherapy of bipolar II disorder during and after pregnancy. Curr. Drug Saf. 2013, 8, 246–252. [Google Scholar] [CrossRef]
- Kim, D.; Epperson, C.; Weiss, A.; Wisner, K. Pharmacotherapy of Postpartum Depression: An Update. Expert Opin. Pharmacother. 2014, 15, 1223–1234. [Google Scholar] [CrossRef] [Green Version]
- Thomson, M.; Sharma, V. Therapeutics of Postpartum Depression. Expert Rev. Neurother. 2016, 17, 495–507. [Google Scholar] [CrossRef]
- Munk-Olsen, T.; Gasse, C.; Laursen, T. Prevalence of Antidepressant Use and Contacts with Psychiatrists and Psychologists in Pregnant and Postpartum Women. Acta Psychiatr. Scand. 2011, 125, 318–324. [Google Scholar] [CrossRef]
- Pearlstein, T.; Zlotnick, C.; Battle, C.; Stuart, S.; O’Hara, M.; Price, A.; Grause, M.; Howard, M. Patient Choice of Treatment for Postpartum Depression: A Pilot Study. Arch. Womens Ment. Health 2006, 9, 303–308. [Google Scholar] [CrossRef]
- Cassano, P.; Fava, M. Tolerability Issues During Long-Term Treatment with Antidepressants. Ann. Clin. Psychiatry 2004, 16, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Turner, K.; Sharp, D.; Folkes, L.; Chew-Graham, C. Women’s views and experiences of antidepressants as a treatment for postnatal depression: A qualitative study. Fam. Pract. 2008, 25, 450–455. [Google Scholar] [CrossRef] [Green Version]
- Kendall-Tackett, K.; Hale, T. Review: The Use of Antidepressants in Pregnant and Breastfeeding Women: A Review of Recent Studies. J. Hum. Lact. 2010, 26, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Kornstein, S.; Sloan, D.; Thase, M. Gender-specific differences in depression and treatment response. Psychopharmacol. Bull. 2002, 36, 99–112. [Google Scholar] [PubMed]
- Sloan, D.; Kornstein, S. Gender differences in depression and response to antidepressant treatment. Psychiatr. Clin. N. Am. 2003, 26, 581–594. [Google Scholar] [CrossRef]
- Brummelte, S.; Galea, L. Depression during pregnancy and postpartum: Contribution of stress and ovarian hormones. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2010, 34, 766–776. [Google Scholar] [CrossRef]
- Gutiérrez-Lobos, K.; Scherer, M.; Anderer, P.; Katschnig, H. The influence of age on the female/male ratio of treated incidence rates in depression. BMC Psychiatry 2002, 2, 3. [Google Scholar] [CrossRef] [Green Version]
- Hammarström, A.; Lehti, A.; Danielsson, U.; Bengs, C.; Johansson, E. Gender-related explanatory models of depression: A critical evaluation of medical articles. Public Health 2009, 123, 689–693. [Google Scholar] [CrossRef]
- Polanía, R.; Nitsche, M.; Ruff, C. Studying and Modifying Brain Function with Non-Invasive Brain Stimulation. Nat. Neurosci. 2018, 21, 174–187. [Google Scholar] [CrossRef]
- Karsen, E.; Watts, B.; Holtzheimer, P. Review of the Effectiveness of Transcranial Magnetic Stimulation for Post-Traumatic Stress Disorder. Brain Stimul. 2014, 7, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Borgomaneri, S.; Battaglia, S.; Garofalo, S.; Tortora, F.; Avenanti, A.; di Pellegrino, G. State-Dependent TMS over Prefrontal Cortex Disrupts Fear-Memory Reconsolidation and Prevents the Return of Fear. Curr. Biol. 2020, 30, 3672–3679.e4. [Google Scholar] [CrossRef]
- Borgomaneri, S.; Battaglia, S.; Avenanti, A.; Pellegrino, G. Don’t Hurt Me No More: State-Dependent Transcranial Magnetic Stimulation for the Treatment of Specific Phobia. J. Affect. Disord. 2021, 286, 78–79. [Google Scholar] [CrossRef]
- Herrmann, M.; Katzorke, A.; Busch, Y.; Gromer, D.; Polak, T.; Pauli, P.; Deckert, J. Medial Prefrontal Cortex Stimulation Accelerates Therapy Response of Exposure Therapy in Acrophobia. Brain Stimul. 2017, 10, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Trevizol, A.; Shiozawa, P.; Cook, I.; Sato, I.; Kaku, C.; Guimarães, F.; Sachdev, P.; Sarkhel, S.; Cordeiro, Q. Transcranial Magnetic Stimulation for Obsessive-Compulsive Disorder. J. ECT 2016, 32, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Carmi, L.; Alyagon, U.; Barnea-Ygael, N.; Zohar, J.; Dar, R.; Zangen, A. Clinical and Electrophysiological Outcomes of Deep TMS over the Medial Prefrontal and Anterior Cingulate Cortices in OCD Patients. Brain Stimul. 2018, 11, 158–165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tran, B.; Ha, G.; Vu, G.; Nguyen, L.; Latkin, C.; Nathan, K.; McIntyre, R.; Ho, C.; Tam, W.; Ho, R. Indices of Change, Expectations, and Popularity of Biological Treatments for Major Depressive Disorder between 1988 and 2017: A Scientometric Analysis. Int. J. Environ. Res. Public Health 2019, 16, 2255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carpenter, L.; Janicak, P.; Aaronson, S.; Boyadjis, T.; Brock, D.; Cook, I.; Dunner, D.L.; Lanocha, K.; Solvason, H.B.; Demitrack, M.A. Transcranial magnetic stimulation (TMS) for major depression: A multisite, naturalistic, observational study of acute treatment outcomes in clinical practice. Depress. Anxiety 2012, 29, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Taïb, S.; Arbus, C.; Sauvaget, A.; Sporer, M.; Schmitt, L.; Yrondi, A. How Does Repetitive Transcranial Magnetic Stimulation Influence the Brain in Depressive Disorders? J. ECT 2018, 34, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Benadhira, R.; Thomas, F.; Bouaziz, N.; Braha, S.; Andrianisaina, P.; Isaac, C.; Moulier, V.; Januel, D. A Randomized, Sham-Controlled Study of Maintenance Rtms for Treatment-Resistant Depression (TRD). Psychiatry Res. 2017, 258, 226–233. [Google Scholar] [CrossRef]
- Bulteau, S.; Sébille, V.; Fayet, G.; Thomas-Ollivier, V.; Deschamps, T.; Bonnin-Rivalland, A.; Laforgue, E.; Pichot, A.; Valrivière, P.; Auffray-Calvier, E.; et al. Efficacy of Intermittent Theta Burst Stimulation (Itbs) and 10-Hz High-Frequency Repetitive Transcranial Magnetic Stimulation (Rtms) in Treatment-Resistant Unipolar Depression: Study Protocol for a Randomised Controlled Trial. Trials 2017, 18, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Lefaucheur, J.; Aleman, A.; Baeken, C.; Benninger, D.; Brunelin, J.; Di Lazzaro, V.; Filipović, S.; Grefkes, C.; Hasan, A.; Hummel, F.; et al. Evidence-Based Guidelines on the Therapeutic Use of Repetitive Transcranial Magnetic Stimulation (Rtms): An Update (2014–2018). Clin. Neurophysiol. 2020, 131, 474–528. [Google Scholar] [CrossRef] [PubMed]
- Miron, J.; Voetterl, H.; Mansouri, F.; Blumberger, D.; Daskalakis, Z.; Downar, J. A Case Series of a Novel 1 Hz Right-Sided Dorsolateral Prefrontal Cortex Rtms Protocol in Major Depression. Brain Stimul. 2020, 13, 372–374. [Google Scholar] [CrossRef] [Green Version]
- Sehatzadeh, S.; Daskalakis, Z.; Yap, B.; Tu, H.; Palimaka, S.; Bowen, J.; O’Reilly, D. Unilateral and Bilateral Repetitive Transcranial Magnetic Stimulation for Treatment-Resistant Depression: A Meta-Analysis of Randomized Controlled Trials over 2 Decades. J. Psychiatry Neurosci. 2019, 44, 151–163. [Google Scholar] [CrossRef] [Green Version]
- Berlim, M.; Van den Eynde, F.; Daskalakis, Z. A Systematic Review and Meta-Analysis on the Efficacy and Acceptability of Bilateral Repetitive Transcranial Magnetic Stimulation (Rtms) for Treating Major Depression. Psychol. Med. 2012, 43, 2245–2254. [Google Scholar] [CrossRef]
- Perera, T.; George, M.; Grammer, G.; Janicak, P.; Pascual-Leone, A.; Wirecki, T. The Clinical TMS Society Consensus Review and Treatment Recommendations for TMS Therapy for Major Depressive Disorder. Brain Stimul. 2016, 9, 336–346. [Google Scholar] [CrossRef] [Green Version]
- Aarre, T.; Dahl, A.; Johansen, J.; Kjønniksen, I.; Neckelmann, D. Efficacy of repetitive transcranial magnetic stimulation in depression: A review of the evidence. Nord. J. Psychiatry 2003, 57, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Slotema, C.; Blom, J.; Hoek, H.; Sommer, I. Should We Expand the Toolbox of Psychiatric Treatment Methods to Include Repetitive Transcranial Magnetic Stimulation (rTMS)? J. Clin. Psychiatry 2010, 71, 873–884. [Google Scholar] [CrossRef]
- Peng, L.; Fu, C.; Xiong, F.; Zhang, Q.; Liang, Z.; Chen, L.; He, C.; Wei, Q. Effects of repetitive transcranial magnetic stimulation on depression symptoms and cognitive function in treating patients with postpartum depression: A systematic review and meta-analysis of randomized controlled trials. Psychiatry Res. 2020, 290, 113124. [Google Scholar] [CrossRef]
- Myczkowski, M.; Dias, A.; Luvisotto, T.; Arnaut, D.; Bellini, B.; Marcolin, M.; Mansur, C.G.; Rennó, J.; de Souza, G.T.; Ribeiro, P.L. Effects of repetitive transcranial magnetic stimulation on clinical, social, and cognitive performance in postpartum depression. Neuropsychiatr. Dis. Treat. 2012, 8, 491–500. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Crowe, M.; Sheppard, L. A general critical appraisal tool: An evaluation of construct validity. Int. J. Nurs. 2011, 48, 1505–1516. [Google Scholar] [CrossRef]
- Crowe, M. Crowe Critical Appraisal Tool (CCAT) User Guide; Conchra House: Scotland, UK, 2013. [Google Scholar]
- Crowe, M.; Sheppard, L. A review of critical appraisal tools show they lack rigor: Alternative tool structure is proposed. J. Clin. Epidemiol. 2011, 64, 79–89. [Google Scholar] [CrossRef]
- Crowe, M.; Sheppard, L.; Campbell, A. Comparison of the effects of using the Crowe Critical Appraisal Tool versus informal appraisal in assessing health research: A randomised trial. Int. J. Evid. Based Healthc. 2011, 9, 444–449. [Google Scholar] [CrossRef]
- Cox, E.; Killenberg, S.; Frische, R.; McClure, R.; Hill, M.; Jenson, J.; Pearson, B.; Meltzer-Brody, S. Repetitive transcranial magnetic stimulation for the treatment of postpartum depression. J. Affect. Disord. 2020, 264, 193–200. [Google Scholar] [CrossRef]
- Brock, D.; Demitrack, M.; Groom, P.; Holbert, R.; Rado, J.; Gross, P.; Goethe, J.W.; Schrodt, G.R.; Weeks, H.R. Effectiveness of NeuroStar transcranial magnetic stimulation (TMS) in patients with major depressive disorder with postpartum onset. Brain Stimul. 2016, 9, e7. [Google Scholar] [CrossRef]
- Ozmut, O.; Balibey, H.; Yilan, Y.; Algul, A.; Ebrinc, S.; Cetin, M.; Tutuncu, R.; Ates, A. Repetitive transcranial magnetic stimulation for the treatment of depression during pregnancy and postpartum period. Bull. Clin. Psychopharmacol. 2015, 25, S203. [Google Scholar]
- Cohen, R.; Ferreira, M.; Ferreira, M.; Fregni, F. Use of repetitive transcranial magnetic stimulation for the management of bipolar disorder during the postpartum period. Brain Stimul. 2008, 1, 224–226. [Google Scholar] [CrossRef]
- Ogden, M.; Lyndon, W.; Pridmore, S. Repetitive transcranial magnetic stimulation (rTMS) in major depressive episode with postpartum onset—A case study. German J. Psychiatry 1999. Available online: http://ecite.utas.edu.au/17760 (accessed on 1 May 2021).
- Lisanby, S.; Gutman, D.; Luber, B.; Schroeder, C.; Sackeim, H. Sham TMS: Intracerebral measurement of the induced electrical field and the induction of motor-evoked potentials. Biol. Psychiatry 2001, 49, 460–463. [Google Scholar] [CrossRef] [Green Version]
- Beck, A. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [Green Version]
- Cox, J.; Holden, J.; Sagovsky, R. Detection of Postnatal Depression. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Spielberger, C. Manual for the State-Trait Anxiety Inventory: STAI (Form Y); Consult. Psychol Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Hamilton, M. Development of a Rating Scale for Primary Depressive Illness. Br. J. Soc. Clin. Psychol. 1967, 6, 278–296. [Google Scholar] [CrossRef]
- Guy, W. ECDEU Assessment Manual for Psychopharmacology; National Institute of Mental Health, US Department of Health, Education, and Welfare: Rockville, MD, USA, 1976.
- Blacker, D. Psychiatric rating scales. In Compr Textbook Psychiatry, 7th ed.; Sadock, B., Sadock, V., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2000. [Google Scholar]
- Mansur, C.; Myczkowki, M.; de Barros Cabral, S.; Sartorelli, M.; Bellini, B.; Dias, Á.; Bernik, M.A.; Marcolin, M.A. Placebo effect after prefrontal magnetic stimulation in the treatment of resistant obsessive-compulsive disorder: A randomized controlled trial. Int. J. Neuropsychopharmacol. 2011, 14, 1389–1397. [Google Scholar] [CrossRef]
- Hamilton, M. The Assessment of Anxiety States by Rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef]
- Campolina, A.; Ciconelli, R. SF-36 and the development of new quality of life assessment measures [SF-36 and the development of new assessment tools for quality of life]. Acta Reum. Port. 2008, 33, 127–133. [Google Scholar]
- Cline, M.; Herman, J.; Shaw, E.; Morton, R. Standardization of the Visual Analogue Scale. Nurs. Res. 1992, 41, 378–379. [Google Scholar] [CrossRef]
- Young, R.; Biggs, J.; Ziegler, V.; Meyer, D. A Rating Scale for Mania: Reliability, Validity and Sensitivity. Br. J. Psychiatry 1978, 133, 429–435. [Google Scholar] [CrossRef]
- Brockington, I.; Oates, J.; George, S.; Turner, D.; Vostanis, P.; Sullivan, M.; Loh, C.; Murdoch, C. A Screening Questionnaire for mother-infant bonding disorders. Arch. Womens Ment. Health 2001, 3, 133–140. [Google Scholar] [CrossRef]
- Brockington, I.; Fraser, C.; Wilson, D. The Postpartum Bonding Questionnaire: A validation. Arch. Womens Ment. Health 2006, 9, 233–242. [Google Scholar] [CrossRef]
- Gorenstein, C.; Moreno, R.; Bernik, M.; Carvalho, S.; Nicastri, S.; Cordás, T.; Camargo, A.P.P.; Artes, R.; Andrade, L. Validation of the Portuguese version of the Social Adjustment Scale on Brazilian samples. J. Affect. Disord. 2002, 69, 167–175. [Google Scholar] [CrossRef]
- Folstein, M.; McHugh, S. ‘Mini-Mental State’ a practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Lezak, M. Neuropsychological Assessment, 3rd ed.; Oxford University Press: New York, NY, USA, 1995. [Google Scholar]
- Rao, S. Cognitive Function Study Group of the National Multiple Sclerosis Society. A Manual for the Brief Repeatable Battery of Neuropsychological Tests in Multiple Sclerosis; National Multiple Sclerosis Society: New York, NY, USA, 1990. [Google Scholar]
- Spreen, S.; Strauss, E. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary, 3rd ed.; Oxford University Press: Oxford, UK, 1991. [Google Scholar]
| Study | Quality Rating | Participants | Study Design | Stimulation Site | Frequency (Hz) | No. of Pulses | No. of Trains ITI | Intensity (%RMT) | No. of Sessions | Outcome Measures | Time-Points | Outcomes | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Age * | ||||||||||||
| Brock et al. (2016) | 20% | 19 | - | Conference paper | Left DLPFC | - | - | - | - | - | EPDS | Baseline, week 8 | Reduction in depressive symptoms. Follow up scores remained below baseline scores. 73.7% of patients achieved remission of their depressive symptoms with acute treatment. |
| Cox et al. (2020). | 67.5% | 6 | 33.5 (30–41 years) | Open-label | Left DLPFC | 10 | 3000 | 75 26 s | 120 | 20 | BDI EPDS STAI | Baseline, weekly, and 3 and 6 months follow up | A general reduction in symptoms however variable across outcome measures. Follow up scores remained below baseline scores. |
| Cohen et al. (2008). | 50% | 1 | 36 years | Case study | Right DLPFC | 20 | 1600 | - | 100 | 1 | HDRS YMRS | Baseline, weekly, and 1 month follow up | Reduction of mania symptoms after right DLPFC Tx; however; returned symptoms of depression: sadness, depressed mood, feelings of guilt, and difficulty concentrating with no psychotic symptoms. Post bilateral Tx, reduction of both depression and manic symptoms. |
| Bilateral DLPFC | 20 | 800 right, 800 left | - | 100 | 9 | ||||||||
| Garcia et al. (2010). | 65% | 9 | 34.11 ± 6.05 | Open-label | Left DLPFC | 10 | 3000 | 75 26 s | 120 | 20 | HRDS-24 EPDS IDS-SR CGI-S | Baseline, end of week 2, end of week 4, and 180-day follow-up | General reduction in depressive symptoms. 88.9% of participants achieved remission of symptoms. Results also indicated a significant improvement in bonding. |
| Myczkowski et al. (2012). | 72.5% | 14 | 28.5 (18–36 years) | RCT | Left DLPFC Sham | 5 | 1250 | 25 20 s | 120 | 20 | HDRS-17 EPDS HARS-14 CGI−1, −2, −3 GA SF-36 SAS NAB | Baseline, 4 weeks of treatment, week 6 follow up | General reduction in symptoms however variable across outcome measures. Follow up scores remained below baseline scores. |
| Ogden et al. (1999). | 40% | 1 | 40 years | Case study | Left DLPFC | 20 | 1200 | 30 28 s | 100 | 13 | HDRS BDI VAS | Baseline, end of treatment | General reduction in symptoms however Pt complained of low energy and motivation, lack of enjoyment and poor sleep a week after discharge. Citalopram dose was increased to 40 mg daily. Follow up revealed no symptoms of depression and improved family relationships. |
| Ozmut et al. (2015) | 17.5% | 15 | - | Conference paper | - | 20 | 1000 | 50 s | 80 | 15 | HDRS-17 HARS-14 EDS-10 | Sessions 1, 7, 15 | Less than half of participants achieved a general reduction in symptoms, however variable across outcome measures. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huddle, M.M.; Costello, S.C.; Barton, D.A. A Systematic Review of the Efficacy of Repetitive Transcranial Magnetic Stimulation Treatment for Women with Postpartum Depression. Psychiatry Int. 2021, 2, 265-276. https://0-doi-org.brum.beds.ac.uk/10.3390/psychiatryint2030020
Huddle MM, Costello SC, Barton DA. A Systematic Review of the Efficacy of Repetitive Transcranial Magnetic Stimulation Treatment for Women with Postpartum Depression. Psychiatry International. 2021; 2(3):265-276. https://0-doi-org.brum.beds.ac.uk/10.3390/psychiatryint2030020
Chicago/Turabian StyleHuddle, Maddison M., Shane C. Costello, and David A. Barton. 2021. "A Systematic Review of the Efficacy of Repetitive Transcranial Magnetic Stimulation Treatment for Women with Postpartum Depression" Psychiatry International 2, no. 3: 265-276. https://0-doi-org.brum.beds.ac.uk/10.3390/psychiatryint2030020






