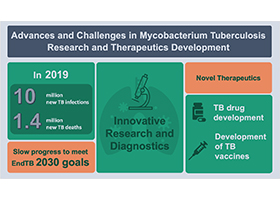
Advances and Challenges in Mycobacterium tuberculosis Research and Therapeutics Development
A special issue of Microorganisms (ISSN 2076-2607). This special issue belongs to the section "Medical Microbiology".
Deadline for manuscript submissions: closed (31 December 2021) | Viewed by 3590
Special Issue Editors
Interests: tuberculosis; global health; tropical infections; bone and joint infections; meningitis; neonatal infections; viral infections
Interests: tuberculosis (TB); neglected tropical diseases; point-of-care testing; TB therapeutics.
Interests: infectious diseases; tuberculosis; microbiology; anti-microbial resistance.
Special Issue Information
Dear Colleagues,
Tuberculosis (TB) is the leading cause of death worldwide from a single infectious agent and is one of the top ten causes of death overall, causing an estimated 10 million infections and 1.4 million deaths in 2019. In 2014, the WHO committed to large reductions in TB incidence and death through the “End TB” strategy, and although incidence is falling globally, it is not falling fast enough to meet these goals.
In recent years, molecular techniques such as GeneXpert and Whole Genome Sequencing have led to improvements in diagnostic efficiency, contact tracing, and resistance testing and contributed to our understanding of key aspects of the organism, such as transmission and virulence.
Furthermore, novel therapeutic agents provide more options for treatment of Multi-Drug Resistant Tuberculosis (MDR-TB), and injectable free regimens may in future improve compliance and cure rates.
At a time when progress in the fight against TB is being threatened by the global COVID-19 pandemic, it is important to focus on bold technological improvements such as improved vaccines, point-of-care diagnostic testing, treatment for latent TB, and shorter treatment regimens for active TB. For this Special Issue, we invite contributions on all aspects of the development of tuberculosis diagnostics and therapeutics.
Dr. Louis Grandjean
Dr. Marc Woodman
Dr. Shruthi Chandran
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Microorganisms is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- tuberculosis (TB)
- TB diagnostics
- whole genome sequencing (WGS)
- resistance
- TB therapeutics
- infectious diseases.






