Gender-Related Approach to Kidney Cancer Management: Moving Forward
Abstract
:1. Introduction
2. Materials and Methods
3. Epidemiology of RCC and Gender
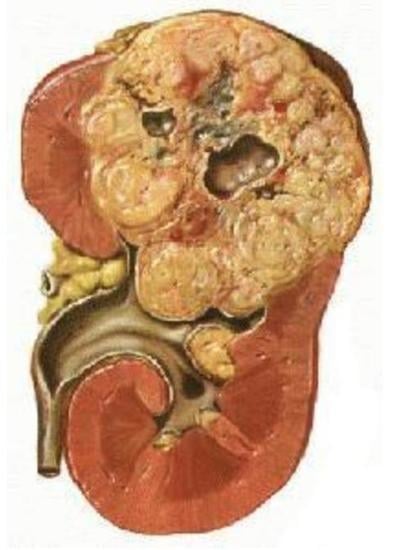
4. Gender-Related Histological Characteristics of Kidney Tumors
5. The Role of Sex Hormones
6. Genetic Factors
7. Impact of Gender on Prognosis
8. Surgery and Surgical Outcomes
9. Other Factors
10. Systemic Therapy
11. Differences in Psychological Distress
12. Conclusive Remarks
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| RCC | renal cell carcinoma |
| BMI | body mass index |
| OS | overall survival |
| CSS | cancer-specific survival |
| OR | odds ratio |
| HR | hazard ratio |
| CI | confidence interval |
| NSS | nephron sparing surgery |
| RN | radical nephrectomy |
| ECOG scale | Eastern Cooperative Oncology Group scale |
| AR | androgen receptor |
| RFS | recurrence-free survival |
| ERβ | oestrogen receptor-β |
| RR | relative risk |
| SNPs | single-nucleotide polymorphisms |
| CSM | cancer-specific mortality |
| VEGF | vascular endothelial growth factor |
| TKI | tyrosine kinase inhibitor |
| mTOR | mammalian target of rapamycin |
| PD-1 | programmed cell death protein-1 |
| CTLA-4 | cytotoxic T-lymphocyte-associated protein 4 |
| PFS | progression-free survival |
References
- Ferlay, J.; Steliarova-Foucher, E.; Lortet-Tieulent, J.; Rosso, S.; Coebergh, J.; Comber, H.; Forman, D.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur. J. Cancer 2013, 49, 1374–1403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capitanio, U.; Bensalah, K.; Bex, A.; Boorjian, S.A.; Bray, F.; Coleman, J.; Gore, J.L.; Sun, M.; Wood, C.; Russo, P. Epidemiology of Renal Cell Carcinoma. Eur. Urol. 2019, 75, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Dy, G.W.; Gore, J.L.; Forouzanfar, M.H.; Naghavi, M.; Fitzmaurice, C. Global Burden of Urologic Cancers, 1990–2013. Eur. Urol. 2017, 71, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Gelfond, J.; Al-Bayati, O.; Kabra, A.; Iffrig, K.; Kaushik, D.; Liss, M.A. Modifiable risk factors to reduce renal cell carcinoma incidence: Insight from the PLCO trial. Urol. Oncol. Semin. Orig. Investig. 2018, 36, 340.e1–340.e6. [Google Scholar] [CrossRef]
- Scelo, G.; Li, P.; Chanudet, E.; Muller, D.C. Variability of Sex Disparities in Cancer Incidence over 30 Years: The Striking Case of Kidney Cancer. Eur. Urol. Focus 2018, 4, 586–590. [Google Scholar] [CrossRef]
- Hew, M.N.; Zonneveld, R.; Kümmerlin, I.P.; Opondo, D.; De La Rosette, J.J.; Laguna, M.P. Age and Gender Related Differences in Renal Cell Carcinoma in a European Cohort. J. Urol. 2012, 188, 33–38. [Google Scholar] [CrossRef] [Green Version]
- Doumas, M.; Papademetriou, V.; Faselis, C.; Kokkinos, P. Gender Differences in Hypertension: Myths and Reality. Curr. Hypertens. Rep. 2013, 15, 321–330. [Google Scholar] [CrossRef]
- Lotan, Y.; Karam, J.; Shariat, S.F.; Gupta, A.; Rouprêt, M.; Bensalah, K.; Margulis, V. Renal-cell carcinoma risk estimates based on participants in the prostate, lung, colorectal, and ovarian cancer screening trial and national lung screening trial. Urol. Oncol. Semin. Orig. Investig. 2016, 34, 167.e9–167.e16. [Google Scholar] [CrossRef]
- Moch, H.; Cubilla, A.L.; Humphrey, P.A.; Reuter, V.E.; Ulbright, T.M. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part A: Renal, Penile, and Testicular Tumours. Eur. Urol. 2016, 70, 93–105. [Google Scholar] [CrossRef]
- Patard, J.-J.; Leray, E.; Rioux-Leclercq, N.; Cindolo, L.; Ficarra, V.; Zisman, A.; De La Taille, A.; Tostain, J.; Artibani, W.; Abbou, C.C.; et al. Prognostic Value of Histologic Subtypes in Renal Cell Carcinoma: A Multicenter Experience. J. Clin. Oncol. 2005, 23, 2763–2771. [Google Scholar] [CrossRef]
- Keegan, K.A.; Schupp, C.W.; Chamie, K.; Hellenthal, N.J.; Evans, C.P.; Koppie, T.M. Histopathology of surgically treated renal cell carcinoma: Survival differences by subtype and stage. J. Urol. 2012, 188, 391–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- May, M.; Aziz, A.; Zigeuner, R.; Chromecki, T.; Cindolo, L.; Schips, L.; De Cobelli, O.; Rocco, B.; De Nunzio, C.; Members of the CORONA project the Young Academic Urologists Renal Cancer Group; et al. Gender differences in clinicopathological features and survival in surgically treated patients with renal cell carcinoma: An analysis of the multicenter CORONA database. World J. Urol. 2013, 31, 1073–1080. [Google Scholar] [CrossRef]
- Lipworth, L.; Morgans, A.K.; Edwards, T.L.; Barocas, D.A.; Chang, S.S.; Herrell, S.D.; Penson, D.; Resnick, M.J.; Smith, J.A.; Clark, P.E. Renal cell cancer histological subtype distribution differs by race and sex. BJU Int. 2015, 117, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Zaitsu, M.; Toyokawa, S.; Takeuchi, T.; Kobayashi, Y.; Kawachi, I. Sex-specific analysis of renal cell carcinoma histology and survival in Japan: A population-based study 2004 to 2016. Heal. Sci. Rep. 2019, 3, e142. [Google Scholar] [CrossRef] [PubMed]
- Bauman, T.M.; Potretzke, A.M.; Wright, A.J.; Knight, B.A.; Vetter, J.M.; Figenshau, R.S. Partial Nephrectomy for Presumed Renal-Cell Carcinoma: Incidence, Predictors, and Perioperative Outcomes of Benign Lesions. J. Endourol. 2017, 31, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Li, S.; Khandwala, Y.; Chung, K.J.; Park, H.K.; Chung, B.I. Association of Prevalence of Benign Pathologic Findings After Partial Nephrectomy With Preoperative Imaging Patterns in the United States From 2007 to 2014. JAMA Surg. 2019, 154, 225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mauermann, J.; De Martino, M.; Waldert, M.; Haitel, A.; Klingler, H.C.; Remzi, M.; Klatte, T. Gender differences in benign renal masses. World J. Urol. 2013, 31, 1051–1057. [Google Scholar] [CrossRef] [PubMed]
- Mancini, M.; Righetto, M.; Baggio, G. Spotlight on gender-specific disparities in bladder cancer. Urol. J. 2019. [Google Scholar] [CrossRef]
- Lucca, I.; Klatte, T.; Fajkovic, H.; De Martino, M.; Shariat, S.F. Gender differences in incidence and outcomes of urothelial and kidney cancer. Nat. Rev. Urol. 2015, 12, 585–592. [Google Scholar] [CrossRef]
- Noh, S.J.; Kang, M.J.; Kim, K.M.; Bae, J.-S.; Park, H.S.; Moon, W.S.; Chung, M.J.; Lee, H.; Lee, D.G.; Jang, K.Y. Acetylation status of P53 and the expression of DBC1, SIRT1, and androgen receptor are associated with survival in clear cell renal cell carcinoma patients. Pathology 2013, 45, 574–580. [Google Scholar] [CrossRef]
- Zhu, G.; Liang, L.; Li, L.; Dang, Q.; Song, W.; Yeh, S.; He, D.; Chang, C. The Expression and Evaluation of Androgen Receptor in Human Renal Cell Carcinoma. Urology 2014, 83, 510.e19–510.e24. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Sun, Y.; Rao, Q.; Xu, H.; Li, L.; Chang, C. Androgen receptor (AR) suppresses miRNA-145 to promote renal cell carcinoma (RCC) progression independent of VHL status. Oncotarget 2015, 6, 31203–31215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, C.-P.; Ho, J.-Y.; Huang, Y.-T.; Cha, T.-L.; Sun, G.-H.; Yu, D.-S.; Chang, F.-W.; Chen, S.-P.; Hsu, R.-J. Estrogen Inhibits Renal Cell Carcinoma Cell Progression through Estrogen Receptor-β Activation. PLOS ONE 2013, 8, e56667. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zucchetto, A.; Talamini, R.; Maso, L.D.; Negri, E.; Polesel, J.; Ramazzotti, V.; Montella, M.; Canzonieri, V.; Serraino, D.; La Vecchia, C.; et al. Reproductive, menstrual, and other hormone-related factors and risk of renal cell cancer. Int. J. Cancer 2008, 123, 2213–2216. [Google Scholar] [CrossRef]
- Setiawan, V.W.; Kolonel, L.N.; Henderson, B.E. Menstrual and reproductive factors and risk of renal cell cancer in the Multiethnic Cohort. Cancer Epidemiol. Biomark. Prev. 2009, 18, 337–340. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Wang, X.-C.; Hu, G.-H.; Huang, T.-B.; Xu, Y.-F. Oral contraceptive use and kidney cancer risk among women: Evidence from a meta-analysis. Int. J. Clin. Exp. Med. 2014, 7, 3954–3963. [Google Scholar]
- Karami, S.; Daugherty, S.E.; Purdue, M.P. Hysterectomy and kidney cancer risk: A meta-analysis. Int. J. Cancer 2013, 134, 405–410. [Google Scholar] [CrossRef] [Green Version]
- Haake, S.M.; Brannon, A.R.; Hacker, K.; Pruthi, R.; Wallen, E.; Nielsen, M.E.; Rathmell, K. Use of meta-analysis of clear cell renal cell carcinoma gene expression to define a variant subgroup and identify gender influences on tumor biology. J. Clin. Oncol. 2012, 30, 412. [Google Scholar] [CrossRef]
- Laskar, R.S.; Muller, D.C.; Li, P.; Machiela, M.J.; Ye, Y.; Gaborieau, V.; Foll, M.; Hofmann, J.N.; Colli, L.; Sampson, J.N.; et al. Sex specific associations in genome wide association analysis of renal cell carcinoma. Eur. J. Hum. Genet. 2019, 27, 1589–1598. [Google Scholar] [CrossRef] [Green Version]
- Ricketts, C.J.; Linehan, W.M. Gender Specific Mutation Incidence and Survival Associations in Clear Cell Renal Cell Carcinoma (CCRCC). PLOS ONE 2015, 10, e0140257. [Google Scholar] [CrossRef] [Green Version]
- Afshar, N.; English, D.R.; Thursfield, V.; Mitchell, P.L.; Marvelde, L.T.; Farrugia, H.; Giles, G.G.; Milne, R.L. Differences in cancer survival by sex: A population-based study using cancer registry data. Cancer Causes Control. 2018, 29, 1059–1069. [Google Scholar] [CrossRef] [PubMed]
- Bhindi, B.; Thompson, R.H.; Lohse, C.M.; Mason, R.J.; Frank, I.; Costello, B.A.; Potretzke, A.M.; Hartman, R.P.; Potretzke, T.A.; Boorjian, S.A.; et al. The Probability of Aggressive Versus Indolent Histology Based on Renal Tumor Size: Implications for Surveillance and Treatment. Eur. Urol. 2018, 74, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Aron, M.; Nguyen, M.M.; Stein, R.J.; Gill, I.S. Impact of Gender in Renal Cell Carcinoma: An Analysis of the SEER Database. Eur. Urol. 2008, 54, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Onishi, T.; Oishi, Y.; Goto, H.; Yanada, S.; Abe, K. Gender as a prognostic factor in patients with renal cell carcinoma. BJU Int. 2002, 90, 32–36. [Google Scholar] [CrossRef] [Green Version]
- Marchioni, M.; Martel, T.; Bandini, M.; Pompe, R.S.; Tian, Z.; Kapoor, A.; Cindolo, L.; Autorino, R.; Briganti, A.; Shariat, S.F.; et al. Marital status and gender affect stage, tumor grade, treatment type and cancer specific mortality in T1–2 N0 M0 renal cell carcinoma. World J. Urol. 2017, 35, 1899–1905. [Google Scholar] [CrossRef]
- Rampersaud, E.N.; Klatte, T.; Bass, G.; Patard, J.-J.; BenSaleh, K.; Böhm, M.; Allhoff, E.P.; Cindolo, L.; De La Taille, A.; Mejean, A.; et al. The effect of gender and age on kidney cancer survival: Younger age is an independent prognostic factor in women with renal cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 2014, 32, 30.e9–30.e13. [Google Scholar] [CrossRef]
- Bertrand, L.A.; Thomas, L.J.; Li, P.; Buchta, C.M.; Boi, S.K.; Orlandella, R.M.; Brown, J.A.; Nepple, K.; Norian, L.A. Obesity as defined by waist circumference but not body mass index is associated with higher renal mass complexity. Urol. Oncol. Semin. Orig. Investig. 2017, 35, 661.e1–661.e6. [Google Scholar] [CrossRef]
- Ito, H.; Makiyama, K.; Kawahara, T.; Osaka, K.; Izumi, K.; Yokomizo, Y.; Nakaigawa, N.; Yao, M. The impact of gender difference on operative time in laparoscopic partial nephrectomy for T1 renal tumor and the utility of retroperitoneal fat thickness as a predictor of operative time. BMC Cancer 2016, 16, 944. [Google Scholar] [CrossRef] [Green Version]
- Tan, H.-J.; Daskivich, T.J.; Shirk, J.; Filson, C.P.; Litwin, M.S.; Hu, J.C. Health status and use of partial nephrectomy in older adults with early-stage kidney cancer. Urol. Oncol. Semin. Orig. Investig. 2017, 35, 153.e7–153.e14. [Google Scholar] [CrossRef]
- O’Malley, R.L.; Underwood, W.; Brewer, K.A.; Hayn, M.H.; Kim, H.L.; Mehedint, D.C.; Safwat, M.W.; Huang, W.C.; Schwaab, T. Gender disparity in kidney cancer treatment: Women are more likely to undergo radical excision of a localized renal mass. Urology 2013, 82, 1065–1070. [Google Scholar] [CrossRef]
- Minnillo, B.J.; Horowitz, A.; Finelli, A.; Alibhai, S.M.; Ponsky, L.E.; Abouassaly, R. Does gender influence morbidity or mortality in the surgical treatment of renal masses? Can. Urol. Assoc. J. 2014, 8, E311–E316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hellou, E.; Bahouth, Z.; Sabo, E.; Abassi, Z.; Nativ, O. The impact of comorbidities, sex and age on the occurrence of acute kidney injury among patients undergoing nephron-sparing surgery. Ther. Adv. Urol. 2018, 10, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Scosyrev, E.; Messing, E.; Sylvester, R.; Van Poppel, H. Exploratory Subgroup Analyses of Renal Function and Overall Survival in European Organization for Research and Treatment of Cancer randomized trial of Nephron-sparing Surgery Versus Radical Nephrectomy. Eur. Urol. Focus 2017, 3, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Lyon, T.D.; Gershman, B.; Shah, P.H.; Thompson, R.H.; Boorjian, S.A.; Lohse, C.M.; Costello, B.A.; Cheville, J.C.; Leibovich, B.C. Risk prediction models for cancer-specific survival following cytoreductive nephrectomy in the contemporary era. Urol. Oncol. Semin. Orig. Investig. 2018, 36, 499.e1–499.e7. [Google Scholar] [CrossRef] [PubMed]
- Rosiello, G.; Knipper, S.; Palumbo, C.; Dzyuba-Negrean, C.; Pecoraro, A.; Mazzone, E.; Mistretta, F.A.; Tian, Z.; Capitanio, U.; Montorsi, F.; et al. Unmarried status is a barrier for access to treatment in patients with metastatic renal cell carcinoma. Int. Urol. Nephrol. 2019, 51, 2181–2188. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef]
- Wallis, C.J.; Butaney, M.; Satkunasivam, R.; Freedland, S.J.; Patel, S.P.; Hamid, O.; Pal, S.K.; Klaassen, Z. Association of Patient Sex With Efficacy of Immune Checkpoint Inhibitors and Overall Survival in Advanced Cancers. JAMA Oncol. 2019, 5, 529. [Google Scholar] [CrossRef]
- Motzer, R.J.; Escudier, B.; McDermott, D.F.; George, S.; Hammers, H.J.; Srinivas, S.; Tykodi, S.S.; Sosman, J.A.; Procopio, G.; Plimack, E.R.; et al. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2015, 373, 1803–1813. [Google Scholar] [CrossRef]
- Motzer, R.J.; Penkov, K.; Haanen, J.; Rini, B.; Albiges, L.; Campbell, M.T.; Venugopal, B.; Kollmannsberger, C.; Negrier, S.; Uemura, M.; et al. Avelumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2019, 380, 1103–1115. [Google Scholar] [CrossRef]
- Conforti, F.; Pala, L.; Bagnardi, V.; De Pas, T.; Martinetti, M.; Viale, G.; Gelber, R.D.; Goldhirsch, A. Cancer immunotherapy efficacy and patients’ sex: A systematic review and meta-analysis. Lancet Oncol. 2018, 19, 737–746. [Google Scholar] [CrossRef]
- Conforti, F.; Pala, L.; Bagnardi, V.; De Pas, T.; Martinetti, M.; Viale, G.; Gelber, R.; Goldhirsch, A. Reply to Jeffrey Graham, Omar Abdel-Rahman, Toni K. Choueiri, and Daniel Y.C. Heng’s Letter to the Editor re: Fabio Conforti, Laura Pala, Vincenzo Bagnardi, et al. Cancer Immunotherapy Efficacy and Patients’ Sex: A Systematic Review and Meta-analysis. Lancet Oncol 2018;19:737-46: Outcomes of Metastatic Renal Cell Carcinoma by Gender: Contrasting Results from the International mRCC Database Consortium. Eur. Urol. 2018, 75, e34–e35. [Google Scholar] [CrossRef] [PubMed]
- Hassler, M.R.; Abufaraj, M.; Kimura, S.; Stangl-Kremser, J.; Gust, K.; Glybochko, P.V.; Schmidinger, M.; Karakiewicz, P.I.; Shariat, S.F. Impact of Patients’ Gender on Efficacy of Immunotherapy in Patients With Metastatic Kidney Cancer: A Systematic Review and Meta-analysis. Clin. Genitourin. Cancer 2020, 18, 88–94.e2. [Google Scholar] [CrossRef] [PubMed]
- Ajaj, R.; Cáceres, J.O.H.; Berlin, A.; Wallis, C.J.D.; Chandrasekar, T.; Klaassen, Z.; Ahmad, A.E.; Leao, R.; Finelli, A.; Fleshner, N.; et al. Gender-based psychological and physical distress differences in patients diagnosed with non-metastatic renal cell carcinoma. World J. Urol. 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bergerot, C.D.; Battle, D.; Staehler, M.D.; Pal, S.K. Distress in patients with renal cell carcinoma: A curious gap in knowledge. BJU Int. 2018, 123, 208–209. [Google Scholar] [CrossRef] [Green Version]
| Factors | Males | Females |
|---|---|---|
| Epidemiology | ||
| Histology | ||
| Sex hormones |
| |
| Genetics |
| |
| Systemic therapy |
| |
| Oncological outcomes | ||
| Surgical outcomes |
|
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mancini, M.; Righetto, M.; Baggio, G. Gender-Related Approach to Kidney Cancer Management: Moving Forward. Int. J. Mol. Sci. 2020, 21, 3378. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21093378
Mancini M, Righetto M, Baggio G. Gender-Related Approach to Kidney Cancer Management: Moving Forward. International Journal of Molecular Sciences. 2020; 21(9):3378. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21093378
Chicago/Turabian StyleMancini, Mariangela, Marialaura Righetto, and Giovannella Baggio. 2020. "Gender-Related Approach to Kidney Cancer Management: Moving Forward" International Journal of Molecular Sciences 21, no. 9: 3378. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21093378