Comparison of Direct Oral Anticoagulant Use for the Treatment of Non-Valvular Atrial Fibrillation in Pivotal Clinical Trials vs. the Real-World Setting: A Population-Based Study from Southern Italy
Abstract
:1. Introduction
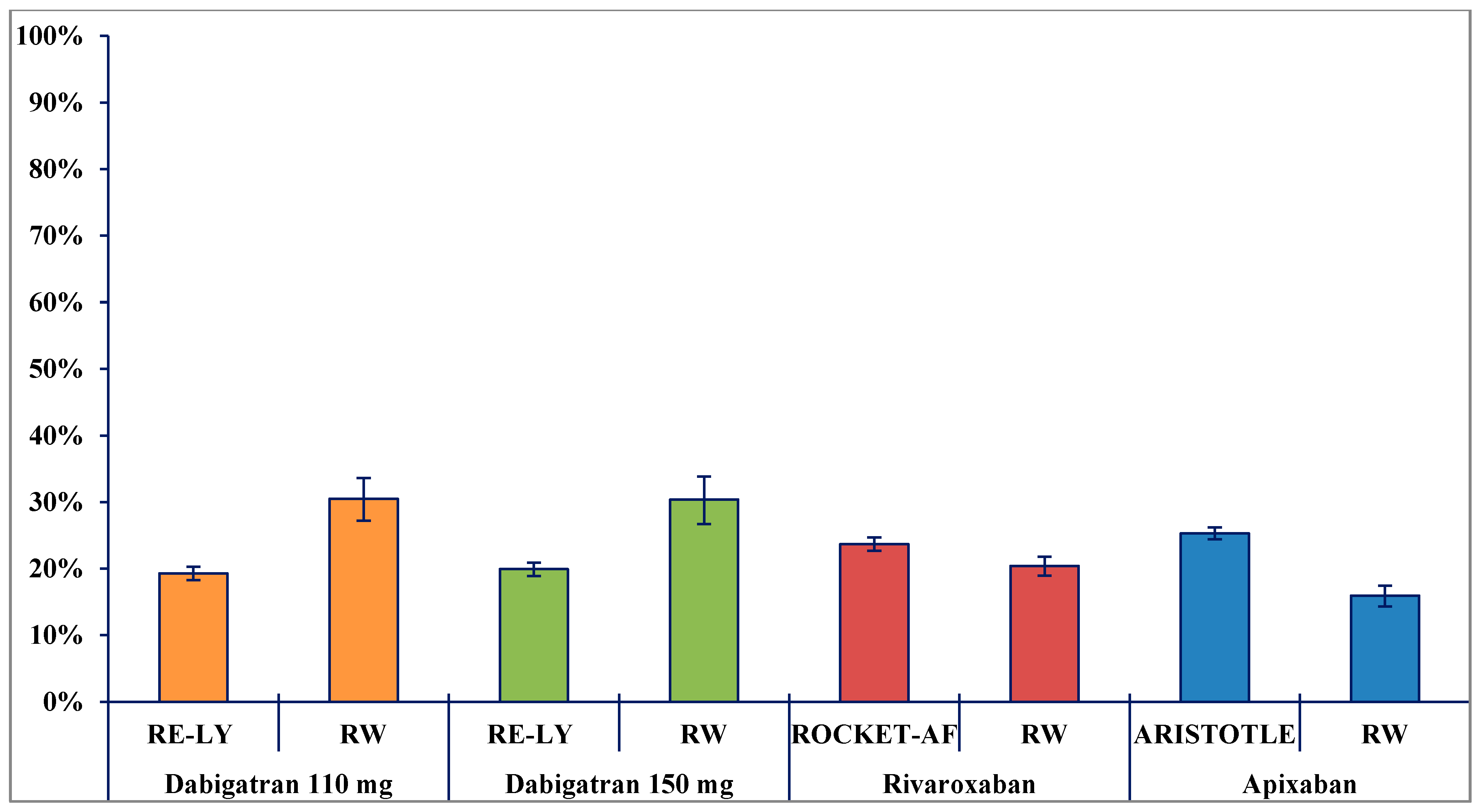
2. Results
3. Discussion
4. Materials and Methods
4.1. Data Source
4.2. Study Population
4.3. Study Drugs
4.4. Data Analysis
4.4.1. Description of Demographic and Clinical Characteristics of DOAC Users
4.4.2. DOAC Treatment Discontinuation
4.4.3. Clinical Outcomes
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deambrosis, P.; Bettiol, A.; Bolcato, J.; Pirolo, R.; Franchin, G.; Themistoclakis, S.; Giusti, P.; Chinellato, A. Thromboprophylaxis in patients with atrial fibrillation: A real practice analysis. Glob. Reg. Health Technol. Assess. 2016, 3, 16–22. [Google Scholar] [CrossRef]
- Zoni-Berisso, M.; Lercari, F.; Carazza, T.; Domenicucci, S. Epidemiology of atrial fibrillation: European perspective. Clin. Epidemiol. 2014, 6, 213–220. [Google Scholar] [CrossRef]
- Italian Drug Agency. Regime di Rimborsabilita’e Prezzo di Vendita del Medicinale per uso Umano «Pradaxa (Dabigatran)», Autorizzata con Procedura Centralizzata Europea Dalla Commissione Europea. (Determina n. 495/2013). 20 May 2013. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2013-06-01&atto.codiceRedazionale=13A04727&elenco30giorni=true (accessed on 16 March 2021).
- Italian Drug Agency. Classificazione del Medicinale per uso Umano «Eliquis (Apixaban)» ai Sensi Dell’Articolo 8, Comma 10, della Legge 24 Dicembre 1993, n. 537. (Determina n. 1109/2013). (13A10345). 2 December 2013. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2013-12-23&atto.codiceRedazionale=13A10345&elenco30giorni=true (accessed on 16 March 2021).
- Italian Drug Agency. Regime di Rimborsabilita’ e Prezzo di Vendita del Medicinale per uso Umano «Xarelto (Rivaroxaban)», autorizzata con Procedura Centralizzata Europea dalla Commissione Europea. (Determina n. 740/2013). (13A07181). 2 August 2013. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2013-08-29&atto.codiceRedazionale=13A07181&elenco30giorni=true (accessed on 16 March 2021).
- Italian Drug Agency. Classificazione, ai sensi dell’articolo 8, comma 10, della legge 24 dicembre 1993, n. 537, del Medicinale per uso Umano «Lixiana». (Determina n. 1105/2016). (16A06311). 4 August 2016. Available online: https://www.gazzettaufficiale.it/eli/id/2016/08/25/16A06311/sg (accessed on 16 March 2021).
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus Warfarin in Nonvalvular Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef]
- Granger, C.B.; Alexander, J.H.; McMurray, J.J.; Lopes, R.D.; Hylek, E.M.; Hanna, M.; Al-Khalidi, H.R.; Ansell, J.; Atar, D.; Avezum, A.; et al. Apixaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, R.P.; Ruff, C.T.; Braunwald, E.; Murphy, S.A.; Wiviott, S.D.; Halperin, J.L.; Waldo, A.L.; Ezekowitz, M.D.; Weitz, J.I.; Špinar, J.; et al. Edoxaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2013, 369, 2093–2104. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, P.M. External validity of randomised controlled trials: “to whom do the results of this trial apply?”. Lancet 2005, 365, 82–93. [Google Scholar] [CrossRef]
- Desmaele, S.; Steurbaut, S.; Cornu, P.; Brouns, R.; Dupont, A.G. Clinical trials with direct oral anticoagulants for stroke prevention in atrial fibrillation: How representative are they for real life patients? Eur. J. Clin. Pharmacol. 2016, 72, 1125–1134. [Google Scholar] [CrossRef] [PubMed]
- Camm, A.J.; Fox, K.A.; Virdone, S.; Bassand, J.P.; Fitzmaurice, D.A.; Berchuck, S.I.; Gersh, B.J.; Goldhaber, S.Z.; Goto, S.; Haas, S.; et al. Comparative effectiveness of oral anticoagulants in everyday practice. Heart 2021. [Google Scholar] [CrossRef]
- Menichelli, D.; Del Sole, F.; Di Rocco, A.; Farcomeni, A.; Vestri, A.; Violi, F.; Pignatelli, P.; Lip, G.Y.; Pastori, D. Real-world safety and efficacy of direct oral anticoagulants in atrial fibrillation: A systematic review and meta-analysis of 605 771 patients. Eur. Heart J. Cardiovasc. Pharmacother. 2021. [Google Scholar] [CrossRef]
- Beyer-Westendorf, J.; Ehlken, B.; Evers, T. Real-world persistence and adherence to oral anticoagulation for stroke risk reduction in patients with atrial fibrillation. Europace 2016, 18, 1150–1157. [Google Scholar] [CrossRef]
- Salmasi, S.; Loewen, P.S.; Tandun, R.; Andrade, J.G.; De Vera, M.A. Adherence to oral anticoagulants among patients with atrial fibrillation: A systematic review and meta-analysis of observational studies. BMJ Open 2020, 10, e034778. [Google Scholar] [CrossRef]
- Lee, S.; Monz, B.U.; Clemens, A.; Brueckmann, M.; Lip, G.Y.H. Representativeness of the dabigatran, apixaban and rivaroxaban clinical trial populations to real-world atrial fibrillation patients in the United Kingdom: A cross-sectional analysis using the General Practice Research Database. BMJ Open 2012, 2. [Google Scholar] [CrossRef]
- Fanning, L.; Ilomäki, J.; Bell, J.S.; Dārziņš, P. The representativeness of direct oral anticoagulant clinical trials to hospitalized patients with atrial fibrillation. Eur. J. Clin. Pharmacol. 2017, 73, 1427–1436. [Google Scholar] [CrossRef]
- Olimpieri, P.P.; Di Lenarda, A.; Mammarella, F.; Gozzo, L.; Cirilli, A.; Cuomo, M.; Gulizia, M.M.; Colivicchi, F.; Murri, G.; Gabrielli, D.; et al. Non-vitamin K antagonist oral anticoagulation agents in patients with atrial fibrillation: Insights from Italian monitoring registries. IJC Hear Vasc. 2020, 26, 100465. [Google Scholar] [CrossRef]
- Amin, A.; Stokes, M.; Wu, N.; Gatt, E.; Makenbaeva, D.; Wiederkehr, D.; Boulanger, L. Application of randomized clinical trial data to actual practice: Apixaban therapy for reduction of stroke risk in non-valvular atrial fibrillation patients. Curr. Med. Res. Opin. 2013, 29, 1253–1261. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2020, 42, 373–498. [Google Scholar] [CrossRef]
- Chen, N.; Brooks, M.M.; Hernandez, I. Latent Classes of Adherence to Oral Anticoagulation Therapy Among Patients With a New Diagnosis of Atrial Fibrillation. JAMA Netw. Open 2020, 3, e1921357. [Google Scholar] [CrossRef]
- European Medicines Agency. Dabigatran Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/pradaxa-epar-product-information_en.pdf (accessed on 16 March 2021).
- Yao, X.; Shah, N.D.; Sangaralingham, L.R.; Gersh, B.J.; Noseworthy, P.A. Non–Vitamin K Antagonist Oral Anticoagulant Dosing in Patients with Atrial Fibrillation and Renal Dysfunction. J. Am. Coll. Cardiol. 2017, 69, 2779–2790. [Google Scholar] [CrossRef]
- Italian Drug Agency. National Report on Medicines use in Italy. 2018. Available online: https://www.aifa.gov.it/documents/20142/241052/OsMed_2018_Eng.pdf/29ebc13d-a9ba-3365-efef-8e2adfa61252 (accessed on 16 March 2021).
- Al-Khalili, F.; Lindström, C.; Benson, L. The safety and persistence of non-vitamin-K-antagonist oral anticoagulants in atrial fibrillation patients treated in a well structured atrial fibrillation clinic. Curr. Med. Res. Opin. 2016, 32, 779–785. [Google Scholar] [CrossRef]
- Ruigómez, A.; Vora, P.; Balabanova, Y.; Brobert, G.; Roberts, L.; Fatoba, S.; Fernandez, O.; Rodríguez, L.A.G. Discontinuation of non-Vitamin K antagonist oral anticoagulants in patients with non-valvular atrial fibrillation: A population-based cohort study using primary care data from the Health Improvement Network in the UK. BMJ Open 2019, 9, e031342. [Google Scholar] [CrossRef]
- Hellfritzsch, M.; Grove, E.L.; Husted, S.E.; Rasmussen, L.; Poulsen, B.K.; Johnsen, S.P.; Hallas, J.; Pottegård, A. Clinical events preceding switching and discontinuation of oral anticoagulant treatment in patients with atrial fibrillation. Ep Eur. 2017, 19, 1091–1095. [Google Scholar] [CrossRef]
- Ingrasciotta, Y.; Crisafulli, S.; Pizzimenti, V.; Marciano, I.; Mancuso, A.; Ando, G.; Corrao, S.; Capranzano, P.; Trifiro, G. Pharmacokinetics of new oral anticoagulants: Implications for use in routine care. Expert Opin. Drug Metab. Toxicol. 2018, 14, 1057–1069. [Google Scholar] [CrossRef]
- Ozaki, A.F.; Choi, A.S.; Le, Q.T.; Ko, D.T.; Han, J.K.; Park, S.S.; Jackevicius, C.A. Real-World Adherence and Persistence to Direct Oral Anticoagulants in Patients with Atrial Fibrillation: A Systematic Review and Meta-Analysis. Circ Cardiovasc. Qual. Outcomes 2020, 13, e005969. [Google Scholar] [CrossRef]
- Martinez, B.K.; Sood, N.A.; Bunz, T.J.; Coleman, C.I. Effectiveness and Safety of Apixaban, Dabigatran, and Rivaroxaban Versus Warfarin in Frail Patients With Nonvalvular Atrial Fibrillation. J. Am. Heart Assoc. 2018, 7, e008643. [Google Scholar] [CrossRef]
- Jansson, M.; Själander, S.; Sjögren, V.; Renlund, H.; Norrving, B.; Själander, A. Direct comparisons of effectiveness and safety of treatment with Apixaban, Dabigatran and Rivaroxaban in atrial fibrillation. Thromb. Res. 2020, 185, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, P.B.; Skjøth, F.; Søgaard, M.; Kjældgaard, J.N.; Lip, G.Y.H.; Larsen, T.B. Effectiveness and safety of reduced dose non-Vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: Propensity weighted nationwide cohort study. BMJ 2017, 356, j510. [Google Scholar] [CrossRef] [PubMed]
- Gorst-Rasmussen, A.; Lip, G.Y.H.; Bjerregaard Larsen, T. Rivaroxaban versus warfarin and dabigatran in atrial fibrillation: Comparative effectiveness and safety in Danish routine care. Pharmacoepidemiol. Drug Saf. 2016, 25, 1236–1244. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov (accessed on 16 March 2021).
- Parsons, L.S. Reducing bias in a propensity score Matched-pair Sample using greedy matching techniques. In Proceedings of the Twenty-Sixth Annual SAS Users Group International Conference 2001, Long Beach, CA, USA, 22–25 April 2001; pp. 214–226. [Google Scholar]
- Stuart, E.A.; Cole, S.R.; Bradshaw, C.P.; Leaf, P.J. The use of propensity scores to assess the generalizability of results from randomized trials. J. R. Stat. Soc. Ser. A Stat. Soc. 2011, 174, 369–386. [Google Scholar] [CrossRef] [PubMed]
| DABIGATRAN 110 mg | DABIGATRAN 150 mg | RIVAROXABAN | APIXABAN | EDOXABAN 30 mg | EDOXABAN 60 mg | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RE-LY n = 6015 | RW n = 794 | RE-LY n = 6076 | RW n = 635 | ROCKET- AF n = 7111 | RW n = 3028 | ARISTOTLE n = 9120 | RW n = 2113 | ENGAGE AF-TIMI 48 n = 7002 | RW n = 253 | ENGAGE AF-TIMI 48 n = 7012 | RW n = 269 | |
| Sex—n (%) | ||||||||||||
| Males | 3868 (64.3) | 382 (48.1) | 3840 (63.2) | 347 (54.6) | 4292 (60.4) | 1553 (51.3) | 5886 (64.5) | 1031 (48.8) | 4285 (61.2) | 92 (36.4) | 4354 (62.1) | 153 (56.9) |
| Females | 2147 (35.7) | 412 (51.9) | 2236 (36.8) | 288 (45.4) | 2819 (39.6) | 1475 (48.7) | 3234 (35.5) | 1082 (51.2) | 2717 (38.8) | 161 (63.6) | 2658 (37.9) | 116 (43.1) |
| Age, y—mean (±SD) | 71.4 (±8.6) | 79.8 (±7.2) | 71.5 (±8.8) | 69.2 (±8.5) | 71.2 (±9.4) | 75.0 (±9.7) | 69.1 (±9.6) | 76.1 (±9.6) | 70.6 (±9.3) | 83.1 (±7.5) | 70.6 (±9.5) | 72.9 (±9.3) |
| CHADS2 score—mean (±SD) | 2.1 ± 1.1 | 2.5 ± 1.3 | 2.1 ± 1.2 | 1.7 ± 1.3 | 3.5 ± 0.9 | 2.2 ± 1.4 | 2.1 ± 1.1 | 2.4 ± 1.4 | 2.8 ± 1.0 | 2.9 ± 1.4 | 2.8 ± 1.0 | 2.1 ± 1.3 |
| CHA2DS2 VASc score—mean (±SD) | n.a. | 4.0 ± 1.5 | n.a. | 2.9 ± 1.6 | n.a. | 3.6 ± 1.7 | n.a. | 3.8 ± 1.7 | n.a. | 4.5 ± 1.5 | n.a. | 3.4 ± 1.6 |
| Previous vitamin K antagonist use a—n (%) | 3011 (50.1) | 453 (57.1) | 3049 (50.2) | 377 (59.4) | 4430 (62.3) | 1747 (57.7) | 5208 (57.1) | 1035 (49.0) | 4145 (59.2) | 108 (42.7) | 4123 (58.8) | 132 (49.1) |
| Comorbidities a—n (%) | ||||||||||||
| Stroke/TIA | 1195 (19.9) | 138 (17.4) | 1233 (20.3) | 72 (11.3) | 3916 (55.1) | 416 (13.7) | 1748 (19.2) | 491 (23.2) | 2006 (28.6) | 50 (19.8) | 1976 (28.2) | 35 (13.0) |
| Heart failure | 1937 (32.2) | 300 (37.8) | 1934 (31.8) | 180 (28.3) | 4467 (62.8) | 1063 (35.1) | 3235 (35.5) | 828 (39.2) | 3979 (56.8) | 148 (58.5) | 4097 (58.4) | 109 (40.5) |
| Diabetes mellitus | 1409 (23.4) | 266 (33.5) | 1402 (23.1) | 190 (29.9) | 2878 (40.5) | 1020 (33.7) | 2284 (25.0) | 737 (34.9) | 2544 (36.3) | 93 (36.8) | 2559 (36.5) | 87 (32.3) |
| Hypertension | 4738 (78.8) | 513 (64.6) | 4795 (78.9) | 383 (60.3) | 6436 (90.5) | 1917 (63.3) | 7962 (87.3) | 1374 (65.0) | 6575 (93.9) | 165 (65.2) | 6591 (94.0) | 161 (59.8) |
| CKD | n.a. | 76 (9.6) | n.a. | 21 (3.3) | n.a. | 272 (9.0) | 5319 (58.3) | 278 (13.1) | n.a | 82 (32.4) | n.a. | 16 (5.9) |
| DABIGATRAN 110 mg | DABIGATRAN 150 mg | RIVAROXABAN | APIXABAN | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RE-LY n = 6015 | Unmatched RW n = 794 | Matched RW n * = 550 | RE-LY n = 6076 | Unmatched RW n = 635 | Matched RW n * = 457 | ROCKET- AF n = 7061 | Unmatched RW n = 3028 | Matched RW n * = 1405 | ARISTOTLE n = 9120 | Unmatched RW n = 2113 | Matched RW n * = 1082 | |
| Efficacy- n (events per 100 person-years) | ||||||||||||
| Ischemic stroke | 1.34 | 1.55 | 1.35 | 0.93 | 0.40 | 0.11 | 1.34 | 1.42 | 1.10 | 0.97 | 1.33 | 0.96 |
| Safety- n (events per 100 person-years) | ||||||||||||
| Major bleeding | 2.92 | 2.20 | 2.28 | 3.40 | 0.97 | 1.02 | 3.60 | 2.44 | 2.31 | 2.13 | 2.00 | 1.94 |
| Intracranial bleeding | 0.23 | 0.14 | 0.10 | 0.32 | 0.24 | 0.23 | 0.49 | 0.46 | 0.28 | 0.33 | 0.23 | 0.18 |
| Gastrointestinal bleeding | 1.13 | 1.05 | 1.08 | 1.60 | 0.32 | 0.34 | 2.00 | 0.92 | 0.99 | 0.76 | 0.81 | 0.79 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ingrasciotta, Y.; Fontana, A.; Mancuso, A.; Ientile, V.; Sultana, J.; Uomo, I.; Pastorello, M.; Calabrò, P.; Andò, G.; Trifirò, G. Comparison of Direct Oral Anticoagulant Use for the Treatment of Non-Valvular Atrial Fibrillation in Pivotal Clinical Trials vs. the Real-World Setting: A Population-Based Study from Southern Italy. Pharmaceuticals 2021, 14, 290. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14040290
Ingrasciotta Y, Fontana A, Mancuso A, Ientile V, Sultana J, Uomo I, Pastorello M, Calabrò P, Andò G, Trifirò G. Comparison of Direct Oral Anticoagulant Use for the Treatment of Non-Valvular Atrial Fibrillation in Pivotal Clinical Trials vs. the Real-World Setting: A Population-Based Study from Southern Italy. Pharmaceuticals. 2021; 14(4):290. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14040290
Chicago/Turabian StyleIngrasciotta, Ylenia, Andrea Fontana, Anna Mancuso, Valentina Ientile, Janet Sultana, Ilaria Uomo, Maurizio Pastorello, Paolo Calabrò, Giuseppe Andò, and Gianluca Trifirò. 2021. "Comparison of Direct Oral Anticoagulant Use for the Treatment of Non-Valvular Atrial Fibrillation in Pivotal Clinical Trials vs. the Real-World Setting: A Population-Based Study from Southern Italy" Pharmaceuticals 14, no. 4: 290. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14040290







