Global Mapping of Research Trends on Interventions to Improve Health-Related Quality of Life in Asthma Patients
Abstract
:1. Introduction
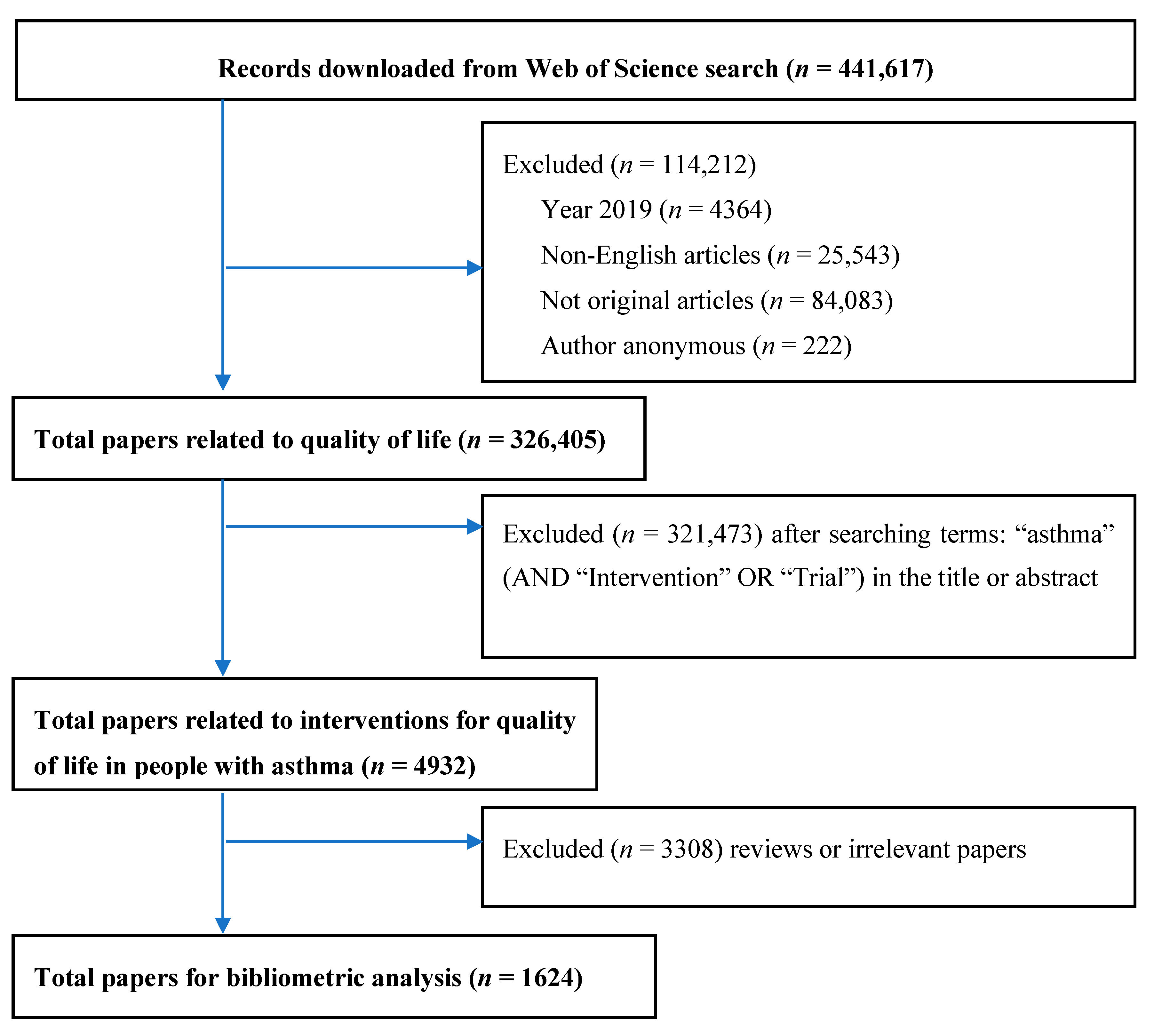
2. Materials and Methods
2.1. Search Strategy
- Step 1: With the use of Boolean operators “OR”, the search query was developed to identify the number of published items included “quality of life” OR “QoL” OR “HRQoL” OR “well-being”. We downloaded papers in text format (txt.) and imported to STATA for further extraction.
- Step 2: Among papers found in Step 1, we used STATA syntax to filter the papers with the following terms in titles or abstracts: (“asthma” OR “asthmatic*”) AND (“intervention*” OR “trial*”). Papers that did not mention “asthma” in their titles and abstracts were removed at this step.
- Step 3: We screened the abstracts of the papers from Step 2 to figure out the papers with asthmatics as study participants and which mentioned quality of life as an outcome. The process was performed by two independent researchers. Any arisen disagreement was solved by discussing with the research team and senior researchers.
2.2. Data Download and Extraction
- Total number of publications
- Authors’ names, their affiliations and the number of total papers, and total citations for each author
- Most prolific countries and collaborations
- Institutional affiliations and frequency of citation
- The top cited articles with titles, authors, journal details, year of publication, total citations and citation per year.
- Titles, abstracts and keywords
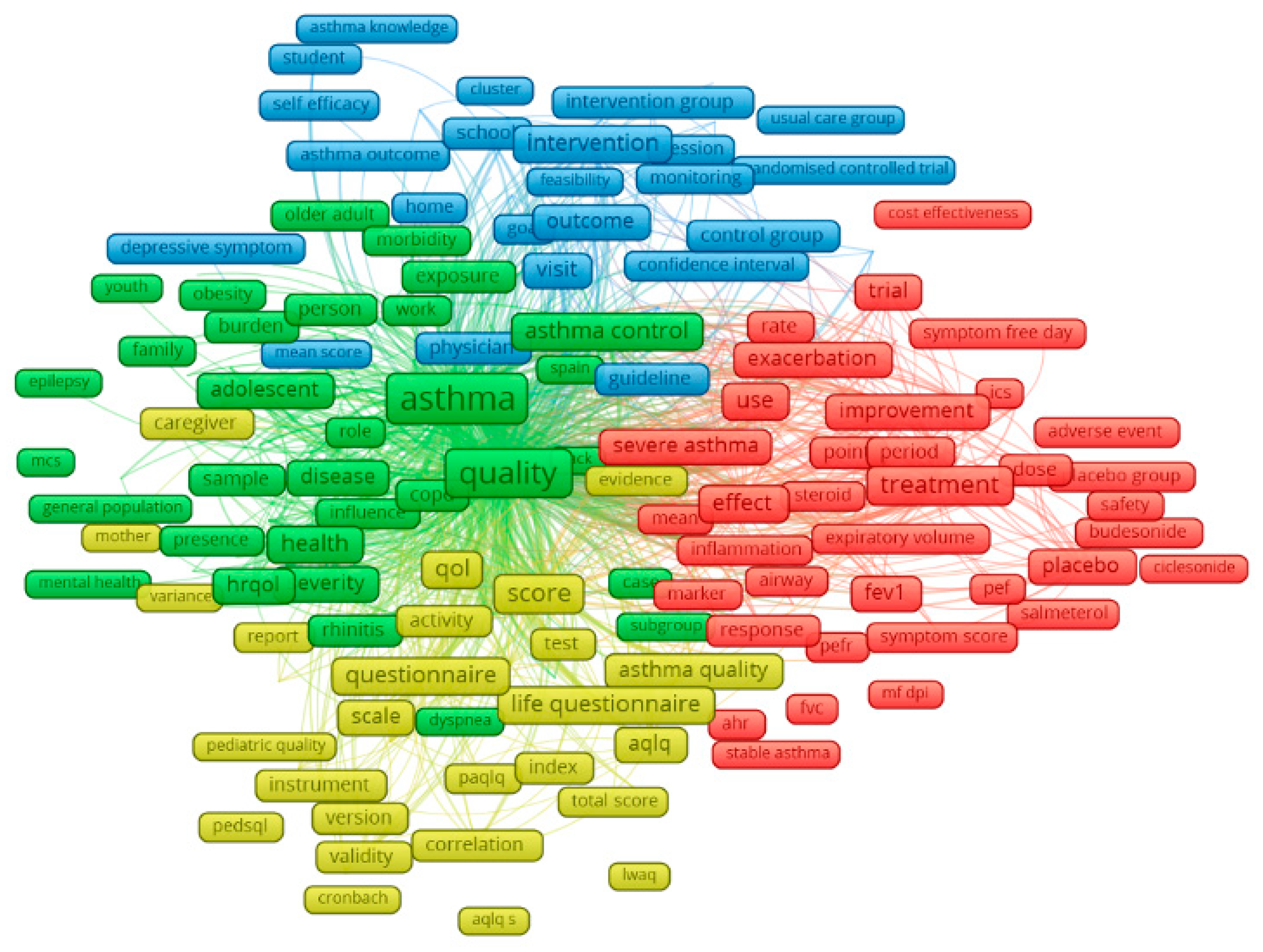
2.3. Data Analysis
3. Results
3.1. Number of Published Items and Publication Trend
3.2. Number of Study Settings by Countries
3.3. Thematic Analysis of Literature and Research Interests Over Time
4. Discussion
4.1. Summary of Findings
4.2. Current Research on Asthma in Different Countries
4.3. Emerging Research Interests
4.4. Identified Research Gaps
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2017. Available online: www.ginasthma.org (accessed on 20 June 2019).
- Poddighe, D.; Brambilla, I.; Licari, A.; Marseglia, G.L. Omalizumab in the Therapy of Pediatric Asthma. Recent Pat. Inflamm. Allergy Drug Discov. 2018, 12, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Busse, W.W. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma; National Institutes of Health: Bethesda, MD, USA, 2007.
- The Global Asthma Report 2018; Global Asthma Network: Auckland, New Zealand, 2018.
- World Health Organization (WHO). Asthma. Available online: https://www.who.int/news-room/fact-sheets/detail/asthma (accessed on 30 September 2019).
- The Global Asthma Report; Global Asthma Network: Auckland, New Zealand, 2014.
- Dharmage, S.C.; Perret, J.L.; Custovic, A. Epidemiology of Asthma in Children and Adults. Front. Pediatr. 2019, 7, 246. [Google Scholar] [CrossRef]
- Poddighe, D.; Brambilla, I.; Licari, A.; Marseglia, G.L. Pediatric rhinosinusitis and asthma. Respir Med. 2018, 141, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Kercsmar, C.M.; Shipp, C. Management/Comorbidities of School-Aged Children with Asthma. Immunol. Allergy Clin. N. Am. 2019, 39, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Weatherburn, C.J.; Guthrie, B.; Mercer, S.W.; Morales, D.R. Comorbidities in adults with asthma: Population-based cross-sectional analysis of 1.4 million adults in Scotland. Clin. Exp. Allergy 2017, 47, 1246–1252. [Google Scholar] [CrossRef] [PubMed]
- Juniper, E.F.; Guyatt, G.H.; Ferrie, P.J.; Griffith, L.E. Measuring quality of life in asthma. Am. Rev. Respir Dis. 1993, 147, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, J.A.; Lemanske, R.F., Jr.; Canino, G.J.; Elward, K.S.; Kattan, M.; Matsui, E.C.; Mitchell, H.; Sutherland, E.R.; Minnicozzi, M. Asthma outcomes: Symptoms. J. Allergy Clin. Immunol. 2012, 129, S124–S135. [Google Scholar] [CrossRef] [Green Version]
- Tepper, R.S.; Wise, R.S.; Covar, R.; Irvin, C.G.; Kercsmar, C.M.; Kraft, M.; Liu, M.C.; O’Connor, G.T.; Peters, S.P.; Sorkness, R.; et al. Asthma outcomes: Pulmonary physiology. J. Allergy Clin. Immunol. 2012, 129, S65–S87. [Google Scholar] [CrossRef] [Green Version]
- Kalyva, E.; Eiser, C.; Papathanasiou, A. Health-Related Quality of Life of Children with Asthma: Self and Parental Perceptions. Int. J. Behav. Med. 2016, 23, 730–737. [Google Scholar] [CrossRef]
- Stern, J.; Pier, J.; Litonjua, A.A. Asthma epidemiology and risk factors. Semin. Immunopathol. 2020, 42, 5–15. [Google Scholar] [CrossRef]
- Melani, A.S.; Bonavia, M.; Cilenti, V.; Cinti, C.; Lodi, M.; Martucci, P.; Serra, M.; Scichilone, N.; Sestini, P.; Aliani, M.; et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir. Med. 2011, 105, 930–938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyd, M.; Lasserson, T.J.; McKean, M.C.; Gibson, P.G.; Ducharme, F.M.; Haby, M. Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst. Rev. 2009, CD001290. [Google Scholar] [CrossRef] [PubMed]
- Pinnock, H.; Parke, H.L.; Panagioti, M.; Daines, L.; Pearce, G.; Epiphaniou, E.; Bower, P.; Sheikh, A.; Griffiths, C.J.; Taylor, S.J.; et al. Systematic meta-review of supported self-management for asthma: A healthcare perspective. BMC Med. 2017, 15, 64. [Google Scholar] [CrossRef] [Green Version]
- Aghaei chadegani, A.; Salehi, H.; Yunus, M.; Farhadi, H.; Fooladi, M.; Farhadi, M.; Ale Ebrahim, N. A Comparison between Two Main Academic Literature Collections: Web of Science and Scopus Databases. Asian Soc. Sci. 2013, 9, 18–26. [Google Scholar] [CrossRef] [Green Version]
- Ding, Y.; Rousseau, R.; Wolfram, D. Measuring Scholarly Impact: Methods and Practice; Springer: Berlin, Germany, 2014. [Google Scholar]
- Li, Y.; Rapkin, B.; Atkinson, T.M.; Schofield, E.; Bochner, B.H. Leveraging Latent Dirichlet Allocation in processing free-text personal goals among patients undergoing bladder cancer surgery. Qual. Life Res. 2019, 28, 1441–1455. [Google Scholar] [CrossRef] [PubMed]
- Valle, D.; Albuquerque, P.; Zhao, Q.; Barberan, A.; Fletcher, R.J., Jr. Extending the Latent Dirichlet Allocation model to presence/absence data: A case study on North American breeding birds and biogeographical shifts expected from climate change. Glob. Chang. Biol. 2018, 24, 5560–5572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Zare, A.; Trinh, H.N.; Omotara, G.O.; Cobb, J.T.; Lagaunne, T.A. Partial Membership Latent Dirichlet Allocation for Soft Image Segmentation. IEEE Trans. Image Process. Publ. IEEE Signal. Process. Soc. 2017, 26, 5590–5602. [Google Scholar] [CrossRef]
- Lu, H.M.; Wei, C.P.; Hsiao, F.Y. Modeling healthcare data using multiple-channel latent Dirichlet allocation. J. Biomed. Inform. 2016, 60, 210–223. [Google Scholar] [CrossRef]
- Gross, A.; Murthy, D. Modeling virtual organizations with Latent Dirichlet Allocation: A case for natural language processing. Neural Netw. Off. J. Int. Neural Netw. Soc. 2014, 58, 38–49. [Google Scholar] [CrossRef]
- Tong, Z.; Zhang, H. A document exploring system on LDA topic model for Wikipedia articles. Int. J. Multimed. Its Appl. 2016, 8. [Google Scholar] [CrossRef]
- Moffat, D.; Ronan, D.; Reiss, J.D. Unsupervised taxonomy of sound effects. Context 2017, 6, 7. [Google Scholar]
- Bank, T.W. High Income. Available online: https://data.worldbank.org/income-level/high-income (accessed on 1 February 2020).
- Asher, M.I.; Montefort, S.; Bjorksten, B.; Lai, C.K.; Strachan, D.P.; Weiland, S.K.; Williams, H.; Group, I.P.T.S. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 2006, 368, 733–743. [Google Scholar] [CrossRef]
- Mallol, J.; Crane, J.; von Mutius, E.; Odhiambo, J.; Keil, U.; Stewart, A.; Group, I.P.T.S. The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three: A global synthesis. Allergol. Immunopathol. (Madr.) 2013, 41, 73–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pumphrey, R.S.; Gowland, M.H. Further fatal allergic reactions to food in the United Kingdom, 1999–2006. J. Allergy Clin. Immunol. 2007, 119, 1018–1019. [Google Scholar] [CrossRef] [PubMed]
- Black, P.N.; Udy, A.A.; Brodie, S.M. Sensitivity to fungal allergens is a risk factor for life-threatening asthma. Allergy 2000, 55, 501–504. [Google Scholar] [CrossRef]
- Kodadhala, V.; Obi, J.; Wessly, P.; Mehari, A.; Gillum, R.F. Asthma-related mortality in the United States, 1999 to 2015: A multiple causes of death analysis. Ann. Allergy Asthma Immunol. 2018, 120, 614–619. [Google Scholar] [CrossRef]
- Levy, M.L. The national review of asthma deaths: What did we learn and what needs to change? Breathe (Sheff) 2015, 11, 14–24. [Google Scholar] [CrossRef] [Green Version]
- Fu, L.S.; Tsai, M.C. Asthma exacerbation in children: A practical review. Pediatr. Neonatol. 2014, 55, 83–91. [Google Scholar] [CrossRef] [Green Version]
- Castillo, J.R.; Peters, S.P.; Busse, W.W. Asthma Exacerbations: Pathogenesis, Prevention, and Treatment. J. Allergy Clin. Immunol. 2017, 5, 918–927. [Google Scholar] [CrossRef]
- Bloom, C.I.; Nissen, F.; Douglas, I.J.; Smeeth, L.; Cullinan, P.; Quint, J.K. Exacerbation risk and characterisation of the UK’s asthma population from infants to old age. Thorax 2018, 73, 313–320. [Google Scholar] [CrossRef] [Green Version]
- Royal College of Physicians. Why Asthma Still Kills: The National Review of Asthma Deaths (NRAD) Confidential Enquiry Report; Royal College of Physicians: London, UK, 2014. [Google Scholar]
- Fy, O.K.R. Why Asthma Still Kills. Ulst. Med. J. 2017, 86, 44. [Google Scholar]
- Lenney, W.; Bush, A.; Fitzgerald, D.A.; Fletcher, M.; Ostrem, A.; Pedersen, S.; Szefler, S.J.; Zar, H.J. Improving the global diagnosis and management of asthma in children. Thorax 2018, 73, 662–669. [Google Scholar] [CrossRef] [Green Version]
- Tan, W.C. Asthma management in the developing world: Achievements and challenges. Expert Rev. Respir Med. 2008, 2, 323–328. [Google Scholar] [CrossRef] [PubMed]
- McDonald, V.M.; Gibson, P.G. Asthma self-management education. Chron. Respir. Dis. 2006, 3, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Heikkinen, S.A.M.; Makikyro, E.M.S.; Hugg, T.T.; Jaakkola, M.S.; Jaakkola, J.J.K. Effects of regular exercise on asthma control in young adults. J. Asthma 2018, 55, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Hakami, R.; Gillis, D.E.; Poureslami, I.; FitzGerald, J.M. Patient and Professional Perspectives on Nutrition in Chronic Respiratory Disease Self-Management: Reflections on Nutrition and Food Literacies. Health Lit. Res. Pract. 2018, 2, e166–e174. [Google Scholar] [CrossRef] [PubMed]
- Kouba, J.; Velsor-Friedrich, B.; Militello, L.; Harrison, P.R.; Becklenberg, A.; White, B.; Surya, S.; Ahmed, A. Efficacy of the I Can Control Asthma and Nutrition Now (ICAN) pilot program on health outcomes in high school students with asthma. J. Sch. Nurs. 2013, 29, 235–247. [Google Scholar] [CrossRef]
- Julia, V.; Macia, L.; Dombrowicz, D. The impact of diet on asthma and allergic diseases. Nat. Rev. Immunol. 2015, 15, 308–322. [Google Scholar] [CrossRef]
- Guo, C.H.; Liu, P.J.; Lin, K.P.; Chen, P.C. Nutritional supplement therapy improves oxidative stress, immune response, pulmonary function, and quality of life in allergic asthma patients: An open-label pilot study. Altern Med. Rev. 2012, 17, 42–56. [Google Scholar]
- Roberts, G.; Patel, N.; Levi-Schaffer, F.; Habibi, P.; Lack, G. Food allergy as a risk factor for life-threatening asthma in childhood: A case-controlled study. J. Allergy Clin. Immunol. 2003, 112, 168–174. [Google Scholar] [CrossRef]
- Wanrooij, V.H.; Willeboordse, M.; Dompeling, E.; van de Kant, K.D. Exercise training in children with asthma: A systematic review. Br. J. Sports Med. 2014, 48, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Orru, H.; Ebi, K.L.; Forsberg, B. The Interplay of Climate Change and Air Pollution on Health. Curr. Environ. Health Rep. 2017, 4, 504–513. [Google Scholar] [CrossRef]
- Khreis, H.; Kelly, C.; Tate, J.; Parslow, R.; Lucas, K.; Nieuwenhuijsen, M. Exposure to traffic-related air pollution and risk of development of childhood asthma: A systematic review and meta-analysis. Environ. Int. 2017, 100, 1–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vardoulakis, S.; Osborne, N. Air pollution and asthma. Arch. Dis. Child. 2018, 103, 813–814. [Google Scholar] [CrossRef]
- Cai, Y.; Zijlema, W.L.; Doiron, D.; Blangiardo, M.; Burton, P.R.; Fortier, I.; Gaye, A.; Gulliver, J.; de Hoogh, K.; Hveem, K.; et al. Ambient air pollution, traffic noise and adult asthma prevalence: A BioSHaRE approach. Eur. Respir. J. 2017, 49. [Google Scholar] [CrossRef] [Green Version]
- Guan, W.J.; Zheng, X.Y.; Chung, K.F.; Zhong, N.S. Impact of air pollution on the burden of chronic respiratory diseases in China: Time for urgent action. Lancet 2016, 388, 1939–1951. [Google Scholar] [CrossRef]
- Orellano, P.; Quaranta, N.; Reynoso, J.; Balbi, B.; Vasquez, J. Effect of outdoor air pollution on asthma exacerbations in children and adults: Systematic review and multilevel meta-analysis. PLoS ONE 2017, 12, e0174050. [Google Scholar] [CrossRef]
- Romeo, E.; De Sario, M.; Forastiere, F.; Compagnucci, P.; Stafoggia, M.; Bergamaschi, A.; Perucci, C.A. PM 10 exposure and asthma exacerbations in pediatric age: A meta-analysis of panel and time-series studies. Epidemiol. Prev. 2006, 30, 245–254. [Google Scholar]
- Weinmayr, G.; Romeo, E.; De Sario, M.; Weiland, S.K.; Forastiere, F. Short-term effects of PM10 and NO2 on respiratory health among children with asthma or asthma-like symptoms: A systematic review and meta-analysis. Environ. Health Perspect 2010, 118, 449–457. [Google Scholar] [CrossRef] [Green Version]
- Barbosa, J.P.; Ferreira-Magalhaes, M.; Sa-Sousa, A.; Azevedo, L.F.; Fonseca, J.A. Cost of asthma in Portuguese adults: A population-based, cost-of-illness study. Rev. Port. Pneumol. 2017, 23, 323–330. [Google Scholar] [CrossRef]
- Ehteshami-Afshar, S.; FitzGerald, J.M.; Doyle-Waters, M.M.; Sadatsafavi, M. The global economic burden of asthma and chronic obstructive pulmonary disease. Int. J. Tuberc. Lung Dis. 2016, 20, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, L.; Dashti, R.; Pourpak, Z.; Fazlollahi, M.R.; Movahedi, M.; Chavoshzadeh, Z.; Soheili, H.; Bokaie, S.; Kazemnejad, A.; Moin, M. Economic Burden of Pediatric Asthma: Annual Cost of Disease in Iran. Iran. J. Public Health 2018, 47, 256–263. [Google Scholar] [PubMed]
- Ait-Khaled, N.; Enarson, D.A.; Bissell, K.; Billo, N.E. Access to inhaled corticosteroids is key to improving quality of care for asthma in developing countries. Allergy 2007, 62, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Martinez, C.E.; Nino, G.; Castro-Rodriguez, J.A. Cost-utility analysis of daily versus intermittent inhaled corticosteroids in mild-persistent asthma. Pediatr. Pulmonol. 2015, 50, 735–746. [Google Scholar] [CrossRef] [Green Version]


| Type of Data | Unit of Analysis | Analytical Methods | Presentations of Results |
|---|---|---|---|
| Keywords, Countries | Words | Frequency of co-occurrence | Map of keywords clusters |
| Abstracts | Papers | Latent Dirichlet Allocation | 10 classifications of research topics |
| WoS classification of research areas | WoS research areas | Frequency of co-occurrence | Dendrogram of research disciplines (WoS classification) |
| Year Published | Total Number of Papers | Total Citations | Mean Cite Rate Per Year 1 | Total Usage 2 Last 6 Months | Total Usage 2 Last 5 Years | Mean Use rate Last 6 Months 3 | Mean Use Rate Last 5 Years 4 |
|---|---|---|---|---|---|---|---|
| 2018 | 129 | 229 | 1.78 | 228.00 | 364.00 | 1.77 | 0.56 |
| 2017 | 143 | 640 | 2.24 | 171.00 | 725.00 | 1.20 | 1.01 |
| 2016 | 109 | 888 | 2.72 | 70.00 | 718.00 | 0.64 | 1.32 |
| 2015 | 95 | 1056 | 2.78 | 49.00 | 677.00 | 0.52 | 1.43 |
| 2014 | 93 | 1185 | 2.55 | 37.00 | 785.00 | 0.40 | 1.69 |
| 2013 | 85 | 1710 | 3.35 | 43.00 | 996.00 | 0.51 | 2.34 |
| 2012 | 73 | 1467 | 2.87 | 24.00 | 664.00 | 0.33 | 1.82 |
| 2011 | 72 | 1880 | 3.26 | 23.00 | 475.00 | 0.32 | 1.32 |
| 2010 | 82 | 2259 | 3.06 | 44.00 | 509.00 | 0.54 | 1.24 |
| 2009 | 76 | 3302 | 4.34 | 33.00 | 464.00 | 0.43 | 1.22 |
| 2008 | 67 | 1833 | 2.49 | 11.00 | 280.00 | 0.16 | 0.84 |
| 2007 | 74 | 3357 | 3.78 | 29.00 | 359.00 | 0.39 | 0.97 |
| 2006 | 60 | 2601 | 3.33 | 22.00 | 271.00 | 0.37 | 0.90 |
| 2005 | 69 | 3399 | 3.52 | 18.00 | 274.00 | 0.26 | 0.79 |
| 2004 | 65 | 2539 | 2.60 | 13.00 | 203.00 | 0.20 | 0.62 |
| 2003 | 47 | 2009 | 2.67 | 12.00 | 161.00 | 0.26 | 0.69 |
| 2002 | 48 | 2528 | 3.10 | 11.00 | 191.00 | 0.23 | 0.80 |
| 2001 | 47 | 2559 | 3.02 | 6.00 | 160.00 | 0.13 | 0.68 |
| 2000 | 49 | 2366 | 2.54 | 8.00 | 187.00 | 0.16 | 0.76 |
| 1999 | 32 | 3088 | 4.83 | 9.00 | 96.00 | 0.28 | 0.60 |
| 1998 | 32 | 1764 | 2.63 | 1.00 | 53.00 | 0.03 | 0.33 |
| 1997 | 26 | 2001 | 3.50 | 4.00 | 84.00 | 0.15 | 0.65 |
| 1996 | 16 | 2268 | 6.16 | 5.00 | 57.00 | 0.31 | 0.71 |
| 1995 | 12 | 865 | 3.00 | 1.00 | 41.00 | 0.08 | 0.68 |
| 1994 | 10 | 1908 | 7.63 | 2.00 | 36.00 | 0.20 | 0.72 |
| 1993 | 8 | 1132 | 5.44 | 4.00 | 27.00 | 0.50 | 0.68 |
| 1992 | 2 | 1094 | 20.26 | 0.00 | 22.00 | 0.00 | 2.20 |
| 1991 | 3 | 469 | 5.58 | 0.00 | 7.00 | 0.00 | 0.47 |
| Country Settings | Frequency | % | Country Settings | Frequency | % | ||
|---|---|---|---|---|---|---|---|
| 1 | United States | 58 | 14.3% | 36 | Cuba | 2 | 0.5% |
| 2 | Australia | 37 | 9.1% | 37 | Finland | 2 | 0.5% |
| 3 | United Kingdom | 32 | 7.9% | 38 | Georgia | 2 | 0.5% |
| 4 | Sweden | 18 | 4.4% | 39 | Greece | 2 | 0.5% |
| 5 | Spain | 17 | 4.2% | 40 | Hungary | 2 | 0.5% |
| 6 | Netherlands | 15 | 3.7% | 41 | Kuwait | 2 | 0.5% |
| 7 | Canada | 13 | 3.2% | 42 | Norway | 2 | 0.5% |
| 8 | Japan | 13 | 3.2% | 43 | South Africa | 2 | 0.5% |
| 9 | Taiwan | 12 | 2.9% | 44 | Sri Lanka | 2 | 0.5% |
| 10 | Brazil | 11 | 2.7% | 45 | Tunisia | 2 | 0.5% |
| 11 | India | 11 | 2.7% | 46 | United Arab Emirates | 2 | 0.5% |
| 12 | Italy | 11 | 2.7% | 47 | Wallis and Futuna | 2 | 0.5% |
| 13 | China | 10 | 2.5% | 48 | Argentina | 1 | 0.2% |
| 14 | Germany | 10 | 2.5% | 49 | Barbados | 1 | 0.2% |
| 15 | France | 9 | 2.2% | 50 | Benin | 1 | 0.2% |
| 16 | Ireland | 9 | 2.2% | 51 | Chile | 1 | 0.2% |
| 17 | Saudi Arabia | 7 | 1.7% | 52 | Czech | 1 | 0.2% |
| 18 | Switzerland | 7 | 1.7% | 53 | Dominica | 1 | 0.2% |
| 19 | Egypt | 6 | 1.5% | 54 | Dominican Republic | 1 | 0.2% |
| 20 | Jordan | 5 | 1.2% | 55 | Iceland | 1 | 0.2% |
| 21 | Singapore | 5 | 1.2% | 56 | Indonesia | 1 | 0.2% |
| 22 | Belgium | 4 | 1.0% | 57 | Iran | 1 | 0.2% |
| 23 | Hong Kong | 4 | 1.0% | 58 | Israel | 1 | 0.2% |
| 24 | Mexico | 4 | 1.0% | 59 | Jamaica | 1 | 0.2% |
| 25 | Turkey | 4 | 1.0% | 60 | Jersey | 1 | 0.2% |
| 26 | Denmark | 3 | 0.7% | 61 | Lebanon | 1 | 0.2% |
| 27 | Malaysia | 3 | 0.7% | 62 | Lithuania | 1 | 0.2% |
| 28 | New Zealand | 3 | 0.7% | 63 | Malta | 1 | 0.2% |
| 29 | Niger | 3 | 0.7% | 64 | Oman | 1 | 0.2% |
| 30 | Nigeria | 3 | 0.7% | 65 | Peru | 1 | 0.2% |
| 31 | Pakistan | 3 | 0.7% | 66 | Puerto Rico | 1 | 0.2% |
| 32 | Poland | 3 | 0.7% | 67 | Qatar | 1 | 0.2% |
| 33 | Portugal | 3 | 0.7% | 68 | Serbia | 1 | 0.2% |
| 34 | Thailand | 3 | 0.7% | 69 | Uruguay | 1 | 0.2% |
| 35 | Austria | 2 | 0.5% |
| Topic (Ranked by the Highest Volume in the Last 5 Years) | Research Topics | n (%) |
|---|---|---|
| middleic 1 | Asthma control and education interventions for asthmatics | 355 (21.8) |
| middleic 2 | Development of medication for persistent asthma and allergic asthma | 238 (14.6) |
| middleic 3 | Association between diet and exercises and quality of life of people with asthma | 167 (10.3) |
| middleic 4 | Validation of questionnaires and evaluation of instruments | 308 (18.9) |
| middleic 5 | Impact of psychological and environmental factors on asthma-related quality of life | 232 (14.3) |
| middleic 6 | Asthma care and intervention for children and adolescents | 160 (9.8) |
| middleic 7 | Drugs for refractory asthma, eosinophilic asthma and non-eosinophilic asthma | 71 (4.4) |
| middleic 8 | Quality of life of asthmatics’ caregiversAsthma-related quality of life among the elderly | 36 (2.2) |
| middleic 9 | Relationship between allergens, allergic rhinitis and asthma status | 52 (3.2) |
| middleic 10 | Impact of non-medical treatment on health outcomes | 7 (0.5) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Phan, H.T.; Vu, G.V.; Vu, G.T.; Ha, G.H.; Pham, H.Q.; Latkin, C.A.; Tran, B.X.; Ho, C.S.H.; Ho, R.C.M. Global Mapping of Research Trends on Interventions to Improve Health-Related Quality of Life in Asthma Patients. Int. J. Environ. Res. Public Health 2020, 17, 3540. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103540
Phan HT, Vu GV, Vu GT, Ha GH, Pham HQ, Latkin CA, Tran BX, Ho CSH, Ho RCM. Global Mapping of Research Trends on Interventions to Improve Health-Related Quality of Life in Asthma Patients. International Journal of Environmental Research and Public Health. 2020; 17(10):3540. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103540
Chicago/Turabian StylePhan, Hai Thanh, Giap Van Vu, Giang Thu Vu, Giang Hai Ha, Hai Quang Pham, Carl A. Latkin, Bach Xuan Tran, Cyrus S.H. Ho, and Roger C.M. Ho. 2020. "Global Mapping of Research Trends on Interventions to Improve Health-Related Quality of Life in Asthma Patients" International Journal of Environmental Research and Public Health 17, no. 10: 3540. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103540






