Real World Use of Antidiabetic Drugs in the Years 2011–2017: A Population-Based Study from Southern Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Study Design
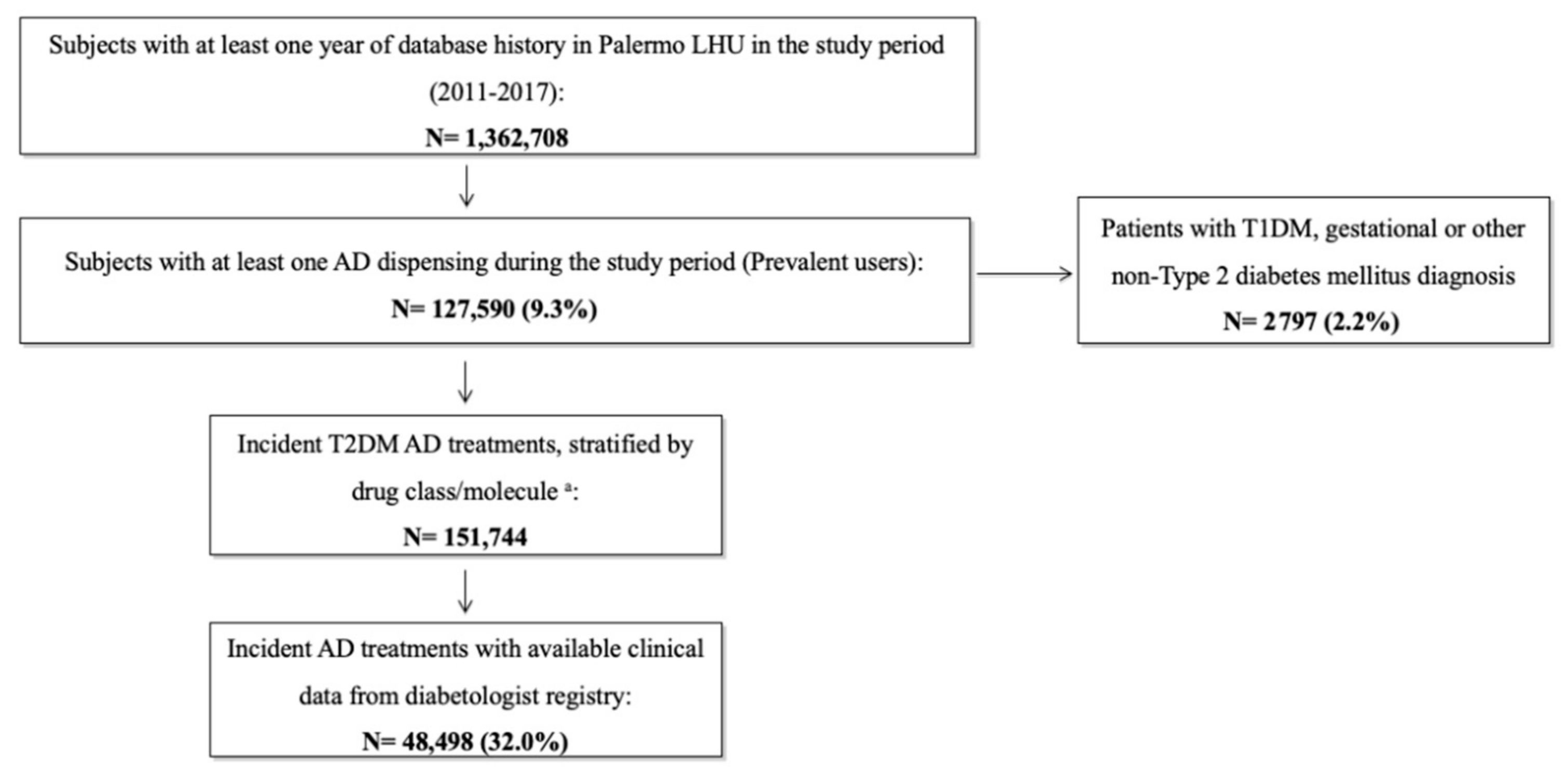
2.2. Study Population
2.3. Study Drugs
2.4. Data Analysis
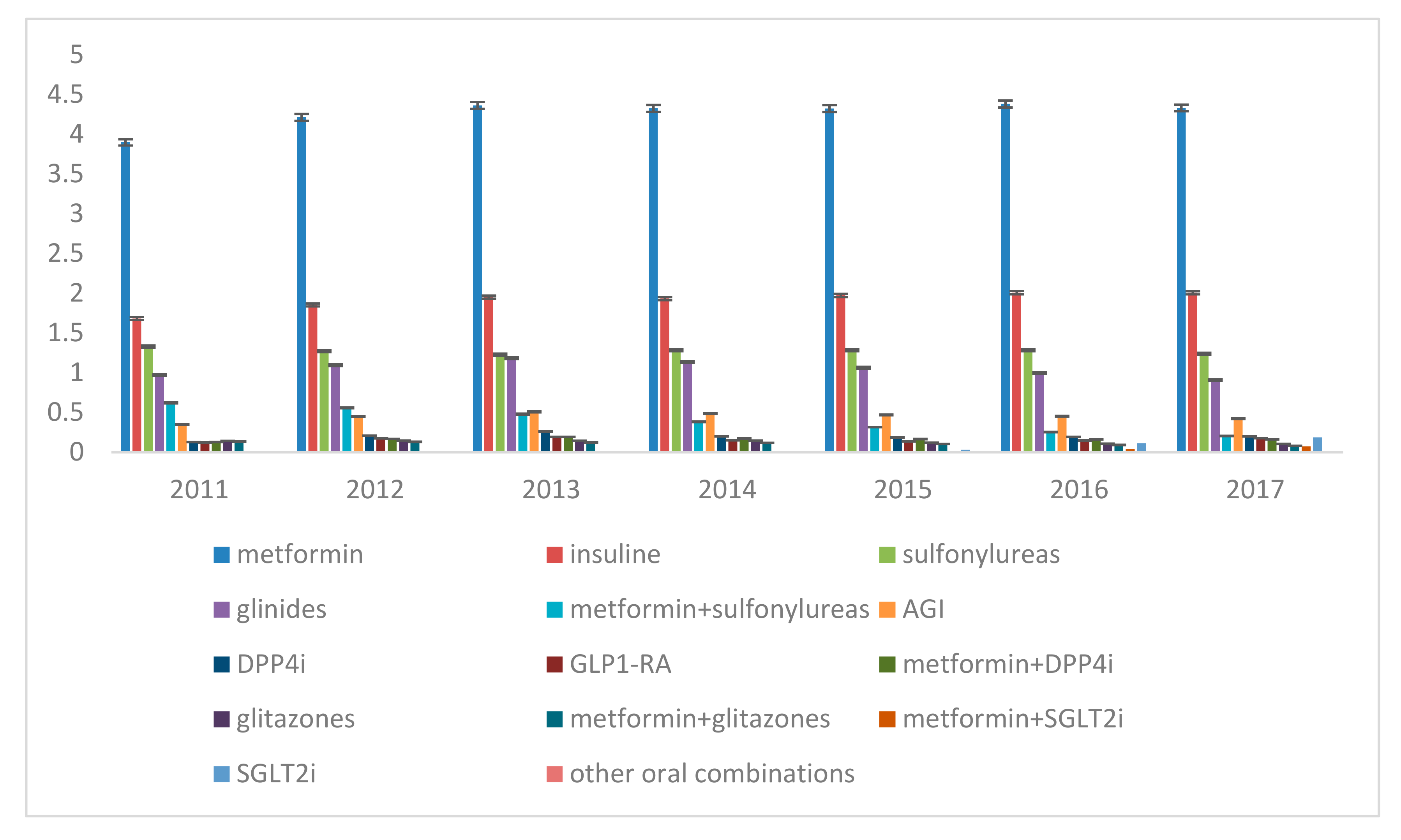
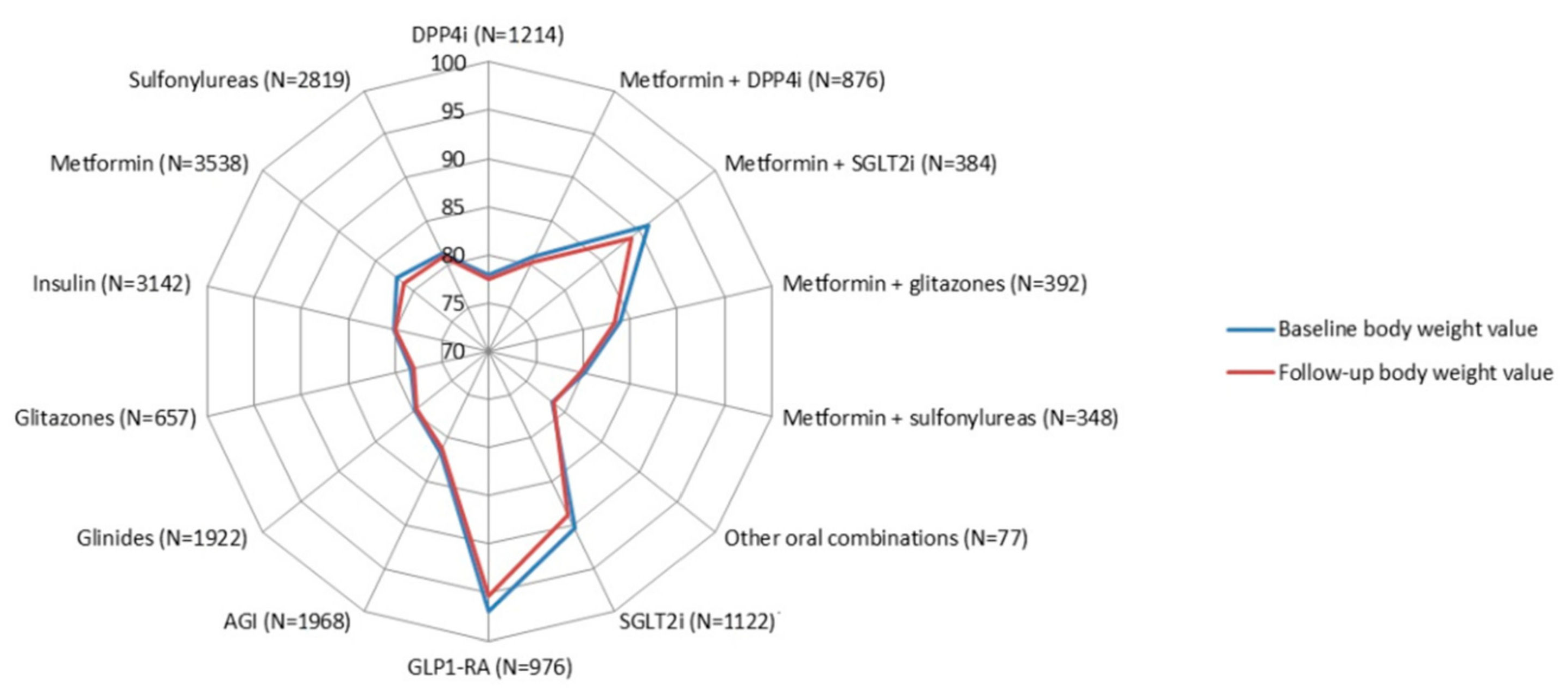
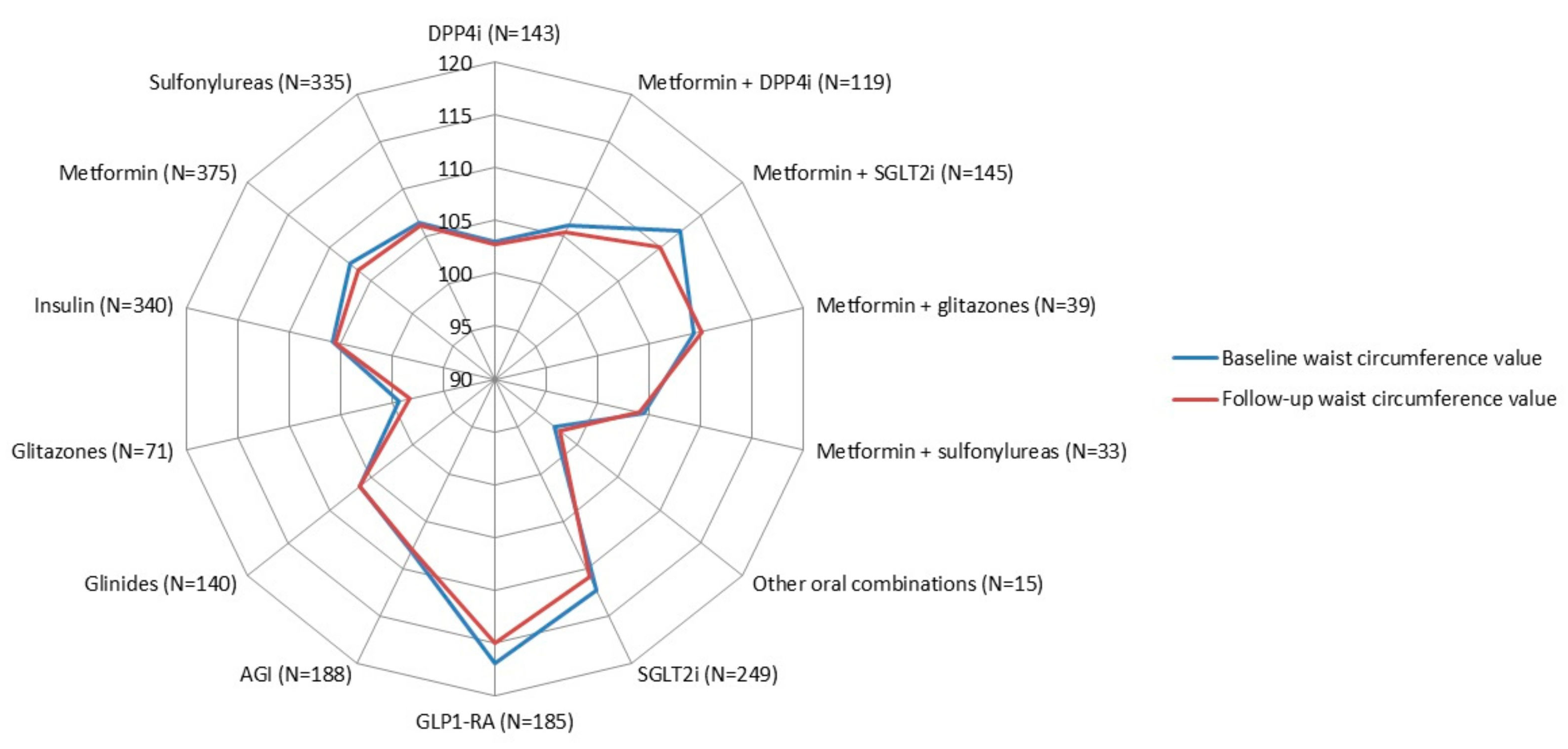
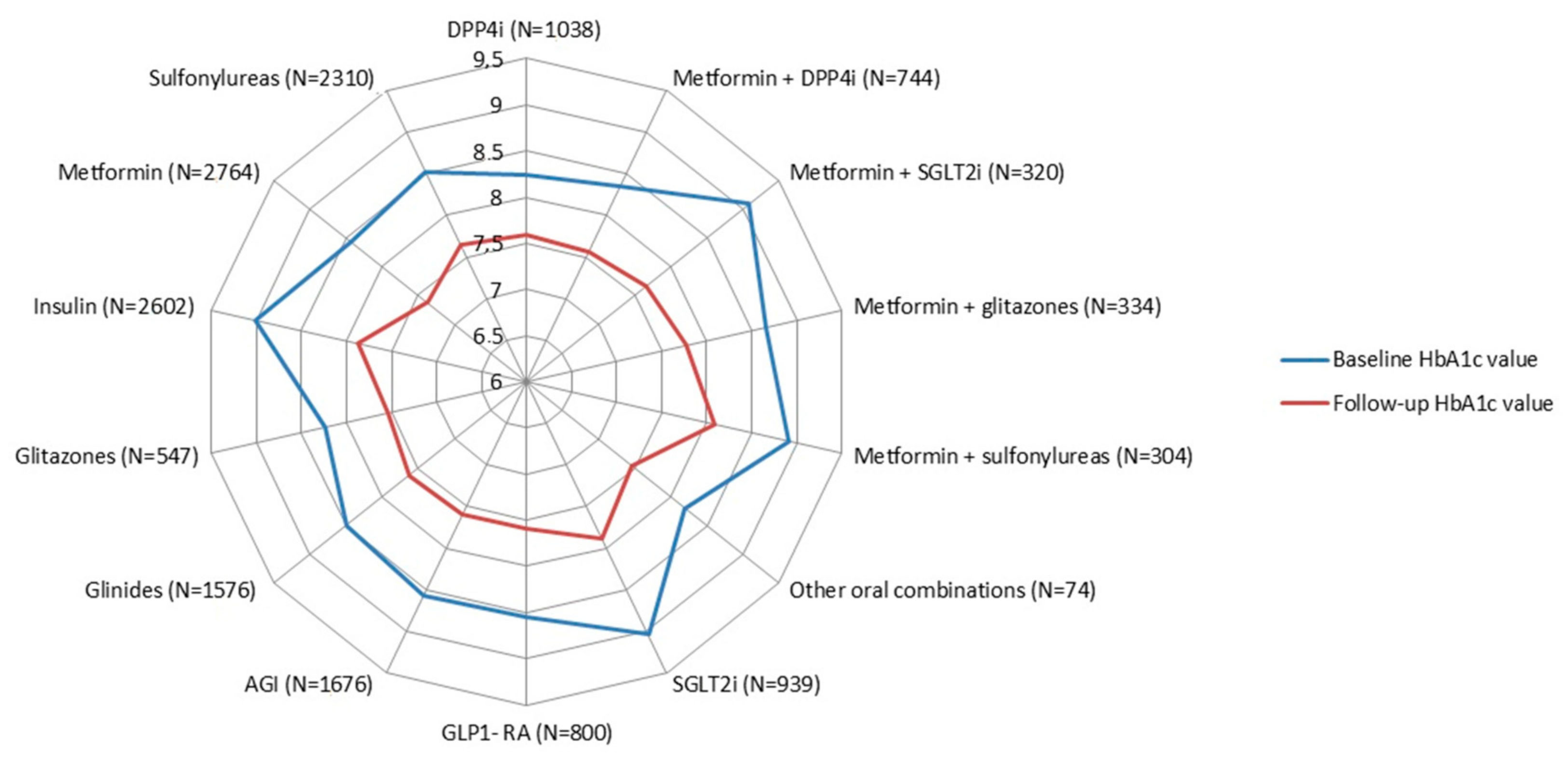
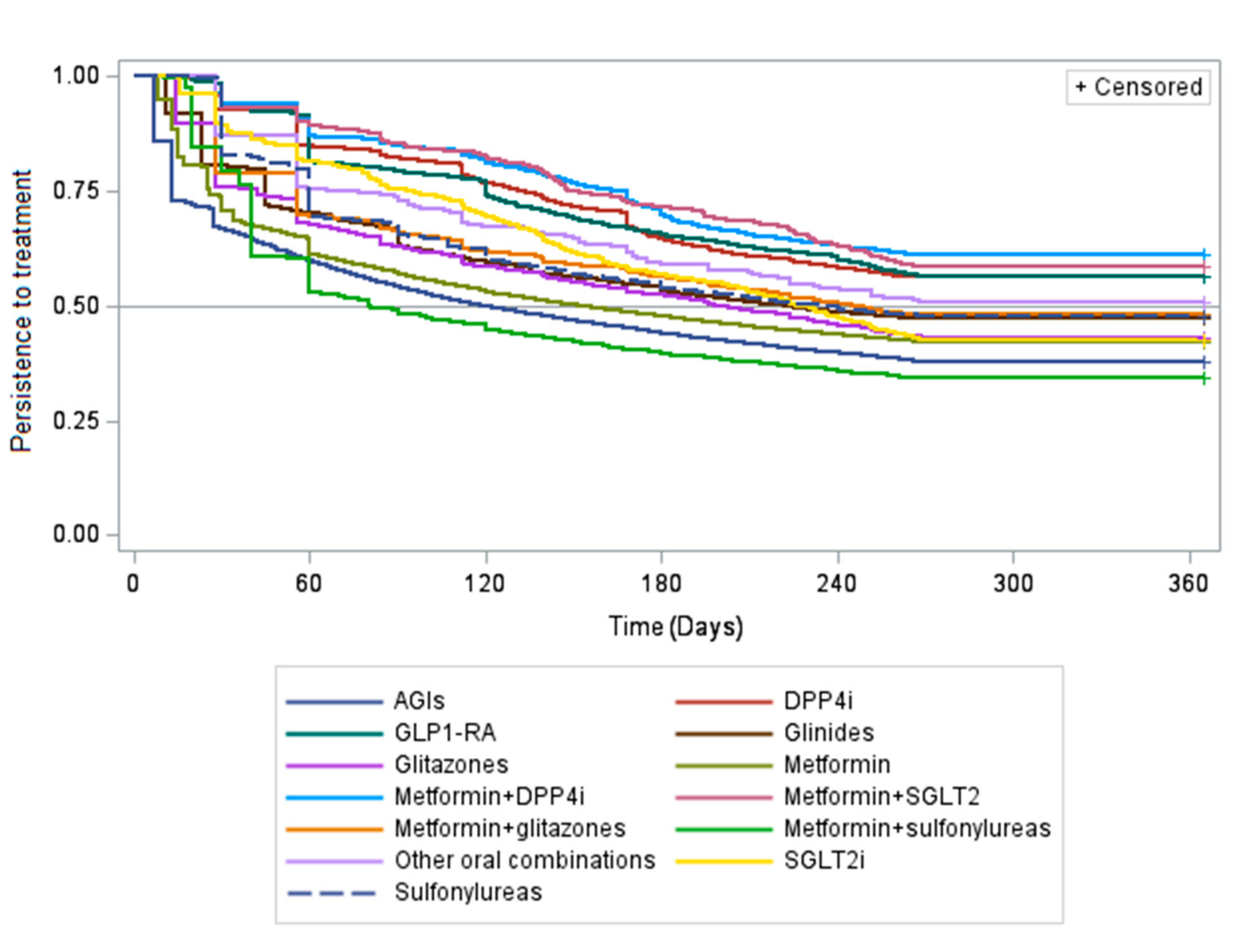
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Molecule/Class | ATC Codes |
|---|---|
| Metformin | A10BA02 |
| DPP4i | A10BH01, A10BH02, A10BH03, A10BH04, A10BH05 |
| SGLT2i | A10BK01, A10BK02, A10BK03, A10BX09, A10BX11, A10BX12 |
| GLP1-RA | A10BJ01, A10BJ02, A10BJ03, A10BJ04, A10BJ05, A10BX04, A10BX07, A10BX10, A10BX13, A10BX14 |
| AGI | A10BF01 |
| Glinides | A10BX02 |
| Glitazones | A10BG02, A10BG03 |
| Insulin | A10AB.xx, A10AC.xx, A10AD.xx, A10AE01, A10AE04, A10AE05, A10AE06 |
| Sulfonylureas | A10BB.xx |
| Fixed-dose combinations | |
| Metformin + DPP4i | A10BD07, A10BD08, A10BD10, A10BD11, A10BD13 |
| Metformin + SGLT2i | A10BD15, A10BD16, A10BD20 |
| Metformin + glitazones | A10BD03, A10BD05 |
| Metformin + sulfonylureas | A10BD01, A10BD02 |
| Other oral combinations | A10BD09, A10BD04, A10BD06 |
| Covariates | Identification Criteria |
|---|---|
| Patient demographics | |
| Sex | Evaluated at index date |
| Age | |
| Comorbidities | |
| Heart failure | ICD-9 codes from discharge diagnosis database or codes from exemptions from healthcare service co-payment database any time prior to index date |
| Atrial fibrillation | |
| COPD | |
| Liver disease | |
| Anemia | |
| Hypertension | ICD9-CM codes from discharge diagnosis database, or codes from exemptions from healthcare service co-payment database or the specific ATC codes from outpatient drug dispensing database any time prior to index date |
| Lipid metabolism disorders | |
| Dementia | |
| Hyperuricemia/Gout | |
| Complications | |
| Nephropathy | ICD-9 codes from discharge diagnosis database or diabetologist registry or codes from exemptions from healthcare service co-payment database any time prior to index date |
| Retinopathy | |
| Neuropathy | |
| Cardiovascular diseases a | |
| Cerebrovascular diseases b | |
| Diabetic foot | |
| Concomitant drugs | |
| Proton pump inhibitors | ATC codes from outpatient drug dispensing within three months prior to index date |
| Anticoagulants c | |
| Antiplatelet agents d | |
| Systemic glucocorticoids | |
| Antidepressants | |
| Drugs for neuropathic pain e | |
| Anti-osteoporotic drugs | |
| Clinical parameters | |
| Glycated hemoglobin (HbA1c) | Available only for a subgroup of patients with data recorded in the diabetologist registry, measured within three months prior to index date |
| Cholesterol | |
| Transaminases | |
| Albumin extraction rate | |
| Creatinine clearance | |
| BMI | |
| Waist circumference | |
| Body weight | |

References
- International Diabetes Federation. IDF Diabetes Atlas Eighth Edition 2017; International Diabetes Federation: Brussel, Belgium, 2017. [Google Scholar]
- Associazione Medici Diabetologi (AMD)-Società Italiana di Diabetologia (SID). Standard Italiani per la Cura del Diabete Mellito 2018; Associazione Medici Diabetologi (AMD)-Società Italiana di Diabetologia (SID): Rome, Italy, 2018. [Google Scholar]
- Istat. Il Diabete in Italia Anni 2000–2016; WwwIstatIt: Genova GE, Italy, 2017. [Google Scholar]
- Cucinotta, D.; Alleva, G.; Buratta, V.; Burgio, A.; Caputo, S.; Cianfarani, S.; Comaschi, M.; Crialesi, R.; Cricelli, C.; Dotta, F.; et al. 11th Italian Diabetes & Obesity Barometer Report; ITALIAN DIABETES MONITOR: Rome, Italy, 2018. [Google Scholar]
- Agenzia Italiana del Farmaco (AIFA). Osservatorio Nazionale sull’impiego dei Medicinali. L’uso dei farmaci in Italia. Rapporto Nazionale Anno 2018; AIFA: Rome, Italy, 2019. [Google Scholar]
- Giorda, C.B.; Manicardi, V.; Cabezudo, J.D. The Impact of Diabetes Mellitus on Healthcare Costs in Italy. Expert Rev. Pharmacoecon. Outcomes Res. 2011, 11, 709–719. [Google Scholar] [CrossRef] [PubMed]
- The Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [CrossRef] [Green Version]
- Davies, M.J.; D’Alessio, D.A.; Fradkin, J.; Kernan, W.N.; Mathieu, C.; Mingrone, G.; Rossing, P.; Tsapas, A.; Wexler, D.J.; Buse, J.B. Correction to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2019, 62, 873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahelić, D.; Javor, E.; Lucijanić, T.; Skelin, M. Effects of antidiabetic drugs on the incidence of macrovascular complications and mortality in type 2 diabetes mellitus: A new perspective on sodium–glucose co-transporter 2 inhibitors. Ann. Med. 2017, 49, 51–62. [Google Scholar] [CrossRef]
- Skelin, M.; Javor, E.; Lucijanić, M.; Lucijanić, T.; Jakupović, L.; Rahelić, D. The role of glucagon in the possible mechanism of cardiovascular mortality reduction in type 2 diabetes patients. Int. J. Clin. Pract. 2018, 72, e13274. [Google Scholar] [CrossRef]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [Green Version]
- Inzucchi, S.E.; Bergenstal, R.M.; Buse, J.B.; Diamant, M.; Ferrannini, E.; Nauck, M.; Peters, A.L.; Tsapas, A.; Wender, R.; Matthews, D.R. Management of Hyperglycemia in Type 2 Diabetes, 2015: A Patient-Centered Approach: Update to a Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015, 38, 140–149. [Google Scholar] [CrossRef] [Green Version]
- Inzucchi, S.E.; Bergenstal, R.M.; Buse, J.B.; Diamant, M.; Ferrannini, E.; Nauck, M.; Peters, A.L.; Tsapas, A.; Wender, R.; Matthews, D.R. Management of Hyperglycemia in Type 2 Diabetes: A Patient-Centered Approach: Position Statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012, 35, 1364–1379. [Google Scholar] [CrossRef] [Green Version]
- Agenzia Italiana del Farmaco (AIFA), Ministero della Salute. Circolare AIFA del 3 agosto 2007. In Linee Guida per la Classificazione e Conduzione Degli Studi Osservazionali sui Farmaci; Azienda Regionale di: Rome, Italy, 2007. [Google Scholar]
- Methodology W-CC for DS. In International Language for Drug Utilization Research; WHO Collaborating Centre: Oslo, Norway, 2012.
- ADVANCE collaborative group; Patel, A.; MacMahon, S.; Chalmers, J.; Neal, B.; Billot, L.; Woodward, M.; Marre, M.; Cooper, M.; Glasziou, P.; et al. Intensive Blood Glucose Control and Vascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2008, 358, 2560–2572. [Google Scholar]
- Libardi, F.; Sirolli, V.; Cappelli, P.; Bonomini, M. Use of oral hypoglycemic agents in patients with chronic kidney failure. G. Ital. Nefrol. 2009, 26, 679–685. [Google Scholar]
- Hernandez, A.V.; Usmani, A.; Rajamanickam, A.; Moheet, A. Thiazolidinediones and Risk of Heart Failure in Patients with or at High Risk of Type 2 Diabetes Mellitus. Am. J. Cardiovasc. Drugs 2011, 11, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Lehrke, M.; Marx, N. Diabetes Mellitus and Heart Failure. Am. J. Med. 2017, 130, S40–S50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grimes, R.T.; Bennett, K.; Tilson, L.; Usher, C.; Smith, S.M.; Henman, M.C. Initial therapy, persistence and regimen change in a cohort of newly treated type 2 diabetes patients. Br. J. Clin. Pharmacol. 2015, 79, 1000–1009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noh, Y.; Lee, S.; Shin, S. Durability of initial antidiabetic monotherapy and subsequent treatment adjustment patterns among newly treated type 2 diabetes patients. Ther. Clin. Risk Manag. 2018, 14, 1563–1571. [Google Scholar] [CrossRef] [Green Version]
- Mata-Cases, M.; Franch-Nadal, J.; Real, J.; Mauricio, D. Glycaemic control and antidiabetic treatment trends in primary care centres in patients with type 2 diabetes mellitus during 2007–2013 in Catalonia: A population-based study. BMJ Open 2016, 6, e012463. [Google Scholar] [CrossRef] [Green Version]
- Baviera, M.; Monesi, L.; Marzona, I.; Avanzini, F.; Monesi, G.; Nobili, A.; Tettamanti, M.; Riva, E.; Cortesi, L.; Bortolotti, A.; et al. Trends in drug prescriptions to diabetic patients from 2000 to 2008 in Italy’s Lombardy Region: A large population-based study. Diabetes Res. Clin. Pract. 2011, 93, 123–130. [Google Scholar] [CrossRef]
- Chang, C.-H.; Jiang, Y.-D.; Chung, C.-H.; Ho, L.-T.; Chuang, L.-M. National trends in anti-diabetic treatment in Taiwan, 2000–2009. J. Formos. Med. Assoc. 2012, 111, 617–624. [Google Scholar] [CrossRef] [Green Version]
- Leal, I.; Romio, S.A.; Schuemie, M.; Oteri, A.; Sturkenboom, M.; Trifirò, G. Prescribing pattern of glucose lowering drugs in the United Kingdom in the last decade: A focus on the effects of safety warnings about rosiglitazone. Br. J. Clin. Pharmacol. 2013, 75, 861–868. [Google Scholar] [CrossRef] [Green Version]
- Turner, L.W.; Nartey, D.; Stafford, R.S.; Singh, S.; Alexander, G.C. Ambulatory Treatment of Type 2 Diabetes in the U.S., 1997–2012. Diabetes Care 2014, 37, 985–992. [Google Scholar] [CrossRef] [Green Version]
- Storgaard, H.; Gluud, L.L.; Bennett, C.; Grøndahl, M.F.; Christensen, M.B.; Knop, F.K.; Vilsbøll, T. Benefits and Harms of Sodium-Glucose Co-Transporter 2 Inhibitors in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0166125. [Google Scholar] [CrossRef]
- Milder, T.Y.; Stocker, S.L.; Abdel Shaheed, C.; McGrath-Cadell, L.; Samocha-Bonet, D.; Greenfield, J.R.; Day, R.O. Combination Therapy with an SGLT2 Inhibitor as Initial Treatment for Type 2 Diabetes: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nathan, D.M.; Buse, J.B.; Davidson, M.B.; Ferrannini, E.; Holman, R.R.; Sherwin, R.; Zinman, B.; American Diabetes Association; European Association for Study of Diabetes. Medical Management of Hyperglycemia in Type 2 Diabetes: A Consensus Algorithm for the Initiation and Adjustment of Therapy: A consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009, 32, 193–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Onder, G.; Bonassi, S.; Abbatecola, A.M.; Folino-Gallo, P.; Lapi, F.; Marchionni, N.; Pani, L.; Pecorelli, S.; Sancarlo, D.; Scuteri, A.; et al. High prevalence of poor quality drug prescribing in older individuals: A nationwide report from the Italian Medicines Agency (AIFA). J. Gerontol-Ser. A Biol. Sci. Med. Sci. 2014, 69, 430–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curkendall, S.M.; Thomas, N.; Bell, K.F.; Juneau, P.L.; Weiss, A.J. Predictors of medication adherence in patients with type 2 diabetes mellitus. Curr. Med. Res. Opin. 2013, 29, 1275–1286. [Google Scholar] [CrossRef] [PubMed]
- Yakaryilmaz, F.D.; Öztürk, Z.A. Treatment of type 2 diabetes mellitus in the elderly. World J. Diabetes 2017, 8, 278–285. [Google Scholar] [CrossRef]
- Neuser, D.; Benson, A.; Brükner, A.; Goldberg, R.B.; Hoogwerf, B.J.; Petzinna, D. Safety and Tolerability of Acarbose in the Treatment of Type 1 and Type 2 Diabetes Mellitus. Clin. Drug Investig. 2005, 25, 579–587. [Google Scholar] [CrossRef]
- Laires, P.; Kurtyka, K.; Witt, E.A.; Qiu, Y.; Yu, S.; Iglay, K. Factors Associated with Physicians’ Decision to Discontinue or Down-Titrate Sulfonylureas for Type 2 Diabetes Patients. Expert Rev. Pharmacoecon. Outcomes Res. 2019, 19, 71–79. [Google Scholar] [CrossRef]
- Stratton, I.M.; Adler, A.I.; Neil, H.A.; Matthews, D.R.; Manley, S.E.; Cull, C.A.; Hadden, D.; Turner, R.C.; Holman, R.R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ 2000, 321, 405–412. [Google Scholar] [CrossRef] [Green Version]
- Apovian, C.M.; Okemah, J.; O’Neil, P.M. Body Weight Considerations in the Management of Type 2 Diabetes. Adv. Ther. 2019, 36, 44–58. [Google Scholar] [CrossRef] [Green Version]
- Comaschi, M.; Di Lenarda, A.; Medea, G.; Aglialoro, A.; Cucinotta, D.; Gulizia, M.; Vespasiani, G.; Zuin, G.; Nicolucci, A.; Spandonaro, F.; et al. INtegration of care for reaching targetS In Diabetic patiEnts: Design of the INSIDE Study. Diabetes Ther. 2019, 11, 359–367. [Google Scholar] [CrossRef] [Green Version]


| Metformin N = 50,544 (%) | Insulin N = 24,270 (%) | SU N = 19,296 (%) | Glinides N = 18,590 (%) | AGI N = 12,170 (%) | DPP4i N = 5869 (%) | GLP-1 RA N = 4273 (%) | Glitazones N = 2977 (%) | SGLT2i N = 2900 (%) | Metformin + DPP4i N = 3987 (%) | Metformin + SGLT2i N = 971 (%) | Metformin + Glitazones N = 1828 (%) | Metformin + SU N = 3701 (%) | Other Oral Combinations N = 368 (%) | Total N = 151,744 (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | 24,852 (49.2) | 12,643 (52.1) | 9716 (50.4) | 9314 (50.1) | 5835 (47.9) | 3079 (52.5) | 2308 (54.0) | 1589 (53.4) | 1547 (53.3) | 2224 (55.8) | 569 (58.6) | 1067 (58.4) | 1848 (49.9) | 213 (57.9) | 76,804 (50.6) |
| Median Age (Q1–Q3) | 64 (55–72) | 69 (58–77) | 68 (60–76) | 70 (61–77) | 66 (58–74) | 65 (58–73) | 57 (50–64) | 64 (56–71) | 57 (50–63) | 62 (55–69) | 56 (49–61) | 63 (55–70) | 71 (63–79) | 63 (56–70) | 66 (57–75) |
| Age ranges—N (%) | |||||||||||||||
| <45 | 6820 (13.5) | 2192 (9.0) | 1045 (5.4) | 731 (3.9) | 715 (5.9) | 260 (4.4) | 594 (13.9) | 218 (7.3) | 310 (10.7) | 233 (5.8) | 140 (14.4) | 126 (6.9) | 195 (5.3) | 21 (5.7) | 13,600 (9.0) |
| 45–64 | 21,864 (43.3) | 7866 (32.4) | 8015 (41.5) | 5994 (32.3) | 4814 (39.6) | 2437 (41.5) | 2790 (65.3) | 1491 (50.2) | 2061 (71.1) | 2231 (56.0) | 686 (70.6) | 1006 (55.0) | 1389 (37.5) | 186 (50.5) | 62,830 (41.4) |
| 65–84 | 20,076 (39.7) | 12,372 (51.0) | 9396 (48.7) | 10,650 (57.3) | 6170 (50.7) | 3056 (52.1) | 880 (20.6) | 1216 (40.8) | 527 (18.1) | 1503 (37.7) | 145 (14.9) | 665 (36.4) | 1896 (51.2) | 157 (42.7) | 68,709 (45.3) |
| ≥85 | 1784 (3.5) | 1840 (7.6) | 840 (4.4) | 1215 (6.5) | 471 (3.9) | 116 (2.0) | 9 (0.2) | 52 (1.7) | 2 (0.1) | 20 (0.5) | – | 31 (1.7) | 221 (6.0) | 4 (1.1) | 6605 (4.3) |
| Comorbidities a —N (%) | |||||||||||||||
| Heart failure | 2129 (4.2) | 2813 (11.6) | 1159 (6.0) | 1888 (10.2) | 834 (6.9) | 501 (8.5) | 254 (5.9) | 129 (4.3) | 149 (5.1) | 156 (3.9) | 26 (2.7) | 75 (4.1) | 216 (5.8) | 14 (3.8) | 10,343 (6.8) |
| Atrial fibrillation | 2001 (4.0) | 2164 (8.9) | 1024 (5.3) | 1519 (8.2) | 667 (5.5) | 339 (5.8) | 184 (4.3) | 99 (3.3) | 110 (3.8) | 129 (3.2) | 18 (1.9) | 53 (2.9) | 194 (5.2) | 7 (1.9) | 8508 (5.6) |
| Hypertensionb | 34,762 (68.8) | 19,040 (78.5) | 15,412 (79.9) | 15,711 (84.5) | 9940 (81.7) | 4918 (83.8) | 3469 (81.2) | 2264 (76.0) | 2304 (79.4) | 3181 (79.8) | 754 (77.7) | 1373 (75.1) | 2858 (77.2) | 280 (76.1) | 116,266 (76.6) |
| Lipid metabolism disordersb | 20,356 (40.3) | 11,960 (49.3) | 10,361 (53.7) | 10,303 (55.4) | 7165 (58.9) | 3964 (67.5) | 2706 (63.3) | 1792 (60.2) | 1950 (67.2) | 2,715 (68.1) | 616(63.4) | 1,102 (60.3) | 1754 (47.4) | 243 (66.0) | 76,987 (50.7) |
| COPD | 2008 (4.0) | 2014 (8.3) | 928 (4.8) | 1331 (7.2) | 596 (4.9) | 281 (4.8) | 196 (4.6) | 101 (3.4) | 94 (3.2) | 126 (3.2) | 23 (2.4) | 46 (2.5) | 209 (5.6) | 8 (2.2) | 7961 (5.2) |
| Dementiab | 583 (1.2) | 659 (2.7) | 274 (1.4) | 366 (2.0) | 197 (1.6) | 95 (1.6) | 17 (0.4) | 35 (1.2) | 7 (0.2) | 32 (0.8) | 5 (0.5) | 4 (0.2) | 67 (1.8) | 5 (1.4) | 2346 (1.5) |
| Liver disease | 1769 (3.5) | 1598 (6.6) | 737 (3.8) | 811 (4.4) | 530 (4.4) | 294 (5.0) | 241 (5.6) | 121 (4.1) | 167 (5.8) | 177 (4.4) | 47 (4.8) | 59 (3.2) | 159 (4.3) | 13 (3.5) | 6723 (4.4) |
| Anemia | 1737 (3.4) | 2300 (9.5) | 945 (4.9) | 1380 (7.4) | 671 (5.5) | 364 (6.2) | 177 (4.1) | 139 (4.7) | 109 (3.8) | 154 (3.9) | 32 (3.3) | 64 (3.5) | 216 (5.8) | 18 (4.9) | 8306 (5.5) |
| Hyperuricemia/Goutb | 7965 (15.8) | 5752 (23.7) | 4128 (21.4) | 5161 (27.8) | 2970 (24.4) | 1452 (24.7) | 870 (20.4) | 591 (19.9) | 516 (17.8) | 633 (15.9) | 143 (14.7) | 307 (16.8) | 727 (19.6) | 74 (20.1) | 31,289 (20.6) |
| Complications e—N (%) | |||||||||||||||
| Nephropathy | 1737 (3.4) | 3007 (12.4) | 1168 (6.1) | 2087 (11.2) | 1016 (8.3) | 688 (11.7) | 315 (7.4) | 236 (7.9) | 223 (7.7) | 195 (4.9) | 41 (4.2) | 89 (4.9) | 217 (5.9) | 22 (6.0) | 11,041 (7.3) |
| Retinopathy | 1252 (2.5) | 1308 (5.4) | 993 (5.1) | 906 (4.9) | 907 (7.5) | 486 (8.3) | 355 (8.3) | 194 (6.5) | 395 (13.6) | 337 (8.5) | 106 (10.9) | 112 (6.1) | 159 (4.3) | 28 (7.6) | 7538 (5.0) |
| Neuropathy | 770 (1.5) | 491 (2.0) | 362 (1.9) | 380 (2.0) | 251 (2.1) | 157 (2.7) | 126 (2.9) | 55 (1.8) | 89 (3.1) | 105 (2.6) | 26 (2.7) | 31 (1.7) | 62 (1.7) | 11 (3.0) | 2916 (1.9) |
| Cardiovascular diseasesc | 5676 (11.2) | 5206 (21.5) | 2993 (15.5) | 3561 (19.2) | 2036 (16.7) | 1283 (21.9) | 737 (17.2) | 384 (12.9) | 689 (23.8) | 710 (17.8) | 161 (16.6) | 212 (11.6) | 546 (14.8) | 41 (11.1) | 24,235 (16.0) |
| Cerebrovascular diseasesd | 5059 (10.0) | 4796 (19.8) | 2550 (13.2) | 3204 (17.2) | 1638 (13.5) | 967 (16.5) | 474 (11.1) | 313 (10.5) | 421 (14.5) | 525 (13.2) | 113 (11.6) | 154 (8.4) | 522 (14.1) | 42 (11.4) | 20,778 (13.7) |
| Diabetic foot | 188 (0.4) | 249 (1.0) | 128 (0.7) | 140 (0.8) | 151 (1.2) | 70 (1.2) | 57 (1.3) | 29 (1.0) | 50 (1.7) | 43 (1.1) | 19 (2.0) | 21 (1.1) | 42 (1.1) | 4 (1.1) | 1191 (0.8) |
| Concomitant drugs f —N (%) | |||||||||||||||
| Proton pump inhibitors | 23,168 (45.8) | 15,376 (63.4) | 11,071 (57.4) | 11,850 (63.7) | 7335 (60.3) | 3770 (64.2) | 2351 (55.0) | 1638 (55.0) | 1601 (55.2) | 2,232 (56.0) | 477 (49.1) | 924 (50.5) | 2156 (58.3) | 208 (56.5) | 84,157 (55.5) |
| Anticoagulantsg | 4572 (9.1) | 4828 (19.9) | 2287 (11.9) | 2991 (16.1) | 1541 (12.7) | 728 (12.4) | 445 (10.4) | 293 (9.8) | 249 (8.6) | 378 (9.5) | 70 (7.2) | 165 (9.0) | 506 (13.7) | 31 (8.4) | 9084 (12.6) |
| Antiplatelet agentsh | 14,577 (28.8) | 10,797 (44.5) | 7956 (41.2) | 8801 (47.3) | 5626 (46.2) | 2838 (48.4) | 1577 (36.9) | 1158 (38.9) | 1183 (40.8) | 1,676 (42.0) | 347 (35.7) | 681 (37.3) | 1537 (41.5) | 154 (41.9) | 58,908 (38.8) |
| Systemic glucocorticoids | 6556 (13.0) | 4914 (20.2) | 2905 (15.1) | 3132 (16.8) | 1688 (13.9) | 667 (11.4) | 405 (9.5) | 354 (11.9) | 262 (9.0) | 374 (9.4) | 72 (7.4) | 195 (10.7) | 613 (16.6) | 40 (10.9) | 22,177 (14.6) |
| Antidepressants | 4593 (9.1) | 2557 (10.5) | 2061 (10.7) | 2112 (11.4) | 1383 (11.4) | 617 (10.5) | 436 (10.2) | 326 (11.0) | 260 (9.0) | 375 (9.4) | 95 (9.8) | 170 (9.3) | 442 (11.9) | 46 (12.5) | 15,473 (10.2) |
| Drugs for neuropathic pain i | 2128 (4.2) | 1648 (6.8) | 1286 (6.7) | 1326 (7.1) | 963 (7.9) | 497 (8.5) | 388 (9.1) | 219 (7.4) | 236 (8.1) | 315 (7.9) | 87 (9.0) | 124 (6.8) | 263 (7.1) | 33 (9.0) | 9513 (6.3) |
| Anti-osteoporotic drugs | 1815 (3.6) | 1085 (4.5) | 1010 (5.2) | 1026 (5.5) | 747 (6.1) | 340 (5.8) | 112 (2.6) | 150 (5.0) | 82 (2.8) | 186 (4.7) | 29 (3.0) | 72 (3.9) | 181 (4.9) | 12 (3.3) | 6847 (4.5) |
| Metformin N = 12,230 | Insulin N = 8081 | SU N = 6587 | Glinides N = 5532 | AGI N = 4759 | DPP4i N = 2411 | GLP-1 RA N = 1909 | Glitazones N = 1299 | SGLT2i N = 1533 | Metformin + DPP4i N = 1713 | Metformin + SGLT2i N = 551 | Metformin + Glitazones N = 778 | Metformin + SU N = 961 | Other Oral Combinations N = 154 | Total N = 48,498 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical parameter: median [IQR] (Proportion (%) of incident AD treatments with ≥ 1 measurement within 3 months prior to ID) | |||||||||||||||
| Glycated hemoglobin (target range: 7–8%) * | 8.0 [7.0–9.2] (38.0) | 8.8 [7.7–10.2] (47.6) | 8.2 [7.4–9.3] (52.8) | 8.2 [7.2–9.3] (44.7) | 8.2 [7.4–9.4] (52.7) | 8.0 [7.5–8.7] (59.3) | 8.3 [7.7–9.2] (58.3) | 8.0 [7.1–9.1] (60.7) | 8.9 [7.9–9.9] (79.6) | 8.2 [7.6–8.8] (59.7) | 8.3 [8.0–9.9] (79.3) | 8.5 [7.6–9.7] (63.5) | 8.7 [7.6–10.0] (48.2) | 8.0 [7.6–8.9] (68.8) | 8.3 [7.4–9.4] (49.5) |
| Cholesterol (target range: 120–220 mg/dl) | 184.0 [155.0–216.0] (34.1) | 172.0 [145.0–202.0] (41.0) | 173.0 [147.0–204.0] (46.8) | 173.0 [146.0–202.0] (40.0) | 170.0 [144.0–200.0] (46.8) | 171.0 [144.0–199.0] (51.5) | 170.0 [142.0–199.0] (51.8) | 175.0 [149.0–203.0] (53.3) | 168.0 [142.0–197.0] (68.0) | 164.0 [141.0–193.0] (52.4) | 171.0 [147.0–195.0] (68.2) | 176.0 [149.0–202.0] (59.4) | 176.0 [148.5–210.5] (42.9) | 177.5 [159.0–213.0] (63.6) | 174.0 [147.0–204.0] (43.7) |
| SGOT (target range: 1–35 UI/l) | 20.0 [15.0–27.0] (22.6) | 18.0 [14.0–25.0] (28.1) | 19.0 [15.0–26.0] (33.5) | 18.0 [14.0–25.0] (25.5) | 19.0 [15.0–25.0] (33.3) | 19.0 [15.0–25.0] (38.0) | 21.0 [16.0–28.0] (37.8) | 19.0 [15.0–25.0] (39.1) | 20.0 [15.0–28.0] (49.4) | 18.0 [15.0–25.0] (38.2) | 20.0 [15.0–28.0] (48.8) | 19.0 [15.0–28.0] (32.0) | 18.0 [15.0–25.0] (24.3) | 18.0 [14.0–22.5] (44.2) | 19.0 [15.0–26.0] (30.1) |
| SGPT (target range: 1–43 UI/l) | 23.0 [16.0–36.0] (23.9) | 21.0 [14.0–32.0] (29.8) | 22.0 [16.0–33.0] (35.2) | 21.0 [15.0–30.0] (27.8) | 21.0 [15.0–31.0] (36.0) | 21.0 [15.0–31.0] (39.6) | 26.0 [18.0–39.0] (39.4) | 21.0 [15.0–31.0] (41.3) | 24.0 [17.0–36.0] (50.0) | 22.0 [16.0–32.0] (39.4) | 25.0 [17.0–36.0] (51.0) | 25.0 [17.0–37.0] 39.5) | 22.0 [15.0–30.0] (30.7) | 20.0 [15.0–28.0] (53.2) | 22.0 [16.0–34.0] (32.1) |
| Albumin extraction rate (target range: 1, 5–20 µg/min) | 10.9 [5.0–27.0] (11.8) | 13.60 [6.0–40.30] (16.5) | 12.0 [5.0–33.0] (19.0) | 14.0 [5.6–49.0] (14.8) | 13.0 [5.3–37.0] (18.2) | 13.0 [5.0–37.5] (21.3) | 14.0 [6.0–47.5] (22.7) | 11.0 [5.0–26.0] (25.1) | 12.3 [5.20–41.0] (32.2) | 12.8 [5.3–31.0] (23.0) | 12.0 [5.5–30.0] (32.3) | 12.0 [5.0–34.0] (25.2) | 11.8 [5.0–35.0] (17.7) | 12.0 [7.0–57.8] (29.9) | 12.15 [5.0–36.0] (17.5) |
| Creatinine clearance (target range: 70–120 mL/min) | 87.0 [66.0–115.0] (17.2) | 78.0 [53.0–108.0] (25.7) | 84.0 [60.0–111.0] (27.0) | 67.0 [48.0–96.0] (25.1) | 79.0 [56.0–107.0] (27.1) | 72.0 [51.0–99.0] (33.5) | 113.0 [89.0–145.0] (30.4) | 78.0 [57.0–108.0] (32.7) | 102.5 [81.0–133.5] (45.9) | 88.0 [68.0–107.0] (30.9) | 111.0 [89.0–139.0] (52.1) | 95.0 [73.0–119.0] (32.5) | 80.0 [58.0–110.0] (21.3) | 81.0 [62.0–108.0] (27.9) | 84.0 [60.0–114.0] (25.7) |
| BMI (target range: 18.5–24.9 Kg/m2) | 29.9 [26.7–34.0] (37.5) | 29.3 [25.8–33.1] (45.7) | 30.0 [26.6–33.7] (51.1) | 29.4 [26.2–33.3] (42.8) | 30.1 [26.8–34.0] (48.7) | 28.9 [25.8–32.4] (57.3) | 34.5 [31.0–39.1] (57.5) | 28.4 [25.2–32.5] (58.1) | 32.4 [28.9–36.7] (79.3) | 29.4 [26.6–32.9] (57.5) | 32.5 [29.0–36.7] (78.9) | 30.5 [27.5–34.0] (59.6) | 30.1 [26.5–33.6] (43.4) | 28.8 [24.6–32.5] (61.0) | 30.1 [26.6–34.0] (47.8) |
| Waist circumference (target values: women: < 80cm;men: <94cm) | 108.0 [100.0–116.0](14.8) | 106.0 [98.0–115.0] (17.2) | 107.0 [99.0–116.0] (19.9) | 107.0 [100.0–116.0] (14.6) | 109.0 [100.0–118.0] (16.6) | 103.0 [97.0–112.0] (24.8) | 116.0 [108.0–123.0] (29.8) | 102.0 [94.0–112.0] (23.2) | 112.0 [104.0–120.0] (43.6) | 105.0 [99.0–113.0] (29.0) | 115.0 [106.0–120.0] (53.5) | 107.0 [100.0–115.0] (26.6) | 104.0 [98.0–114.0] (15.1) | 100.0 [92.0–109.0] (25.3) | 108.0 [100.0–117.0] (19.4) |
| Body weight (kg) | 80.0 [70.0–93.0] (38.7) | 78.0 [67.5–90.0] (47.3) | 79.0 [69.0–91.0] (52.6) | 77.0 [68.0–89.0] (44.3) | 80.0 [70.0–91.7] (50.3) | 77.0 [66.8–87.0] (58.4) | 95.0 [84.0–107.5] (59.0) | 75.7 [66.0–88.0] (59.7) | 87.7 [77.5–100.4] (80.3) | 80.0 [71.0–90.0] (58.7) | 89.0 [79.0–102.0] (79.5) | 82.6 [72.0–93.0] (60.9) | 79.0 [69.0–91.0] (44.8) | 77.2 [66.5–86.3] (62.3) | 80.0 [70.0–92.5] (49.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ingrasciotta, Y.; Bertuccio, M.P.; Crisafulli, S.; Ientile, V.; Muscianisi, M.; L’Abbate, L.; Pastorello, M.; Provenzano, V.; Scorsone, A.; Scondotto, S.; et al. Real World Use of Antidiabetic Drugs in the Years 2011–2017: A Population-Based Study from Southern Italy. Int. J. Environ. Res. Public Health 2020, 17, 9514. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249514
Ingrasciotta Y, Bertuccio MP, Crisafulli S, Ientile V, Muscianisi M, L’Abbate L, Pastorello M, Provenzano V, Scorsone A, Scondotto S, et al. Real World Use of Antidiabetic Drugs in the Years 2011–2017: A Population-Based Study from Southern Italy. International Journal of Environmental Research and Public Health. 2020; 17(24):9514. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249514
Chicago/Turabian StyleIngrasciotta, Ylenia, Maria Paola Bertuccio, Salvatore Crisafulli, Valentina Ientile, Marco Muscianisi, Luca L’Abbate, Maurizio Pastorello, Vincenzo Provenzano, Alessandro Scorsone, Salvatore Scondotto, and et al. 2020. "Real World Use of Antidiabetic Drugs in the Years 2011–2017: A Population-Based Study from Southern Italy" International Journal of Environmental Research and Public Health 17, no. 24: 9514. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249514





