SettleIN: Using a Manualised Intervention to Facilitate the Adjustment of Older Adults with Dementia Following Placement into Residential Care
Abstract
:1. Introduction
2. Method
2.1. Phase One: Developing the Intervention
Consultation
2.2. Phase Two: Feasibility Study of the Enhanced SettleIN Intervention
2.2.1. Design
2.2.2. Ethical approval
2.2.3. Recruitment
Setting
Participants
2.2.4. Procedure
Randomisation
Intervention Training
The SettleIN Programme
2.2.5. Measures
Demographics
Functional Stage of Dementia
Quality of Life
Psychological Wellbeing
Overall Adjustment
Feasibility of SettleIN for staff
Feasibility Measures
2.2.6. Analysis
Missing Data
Qualitative Data
3. Results
3.1. Resident Characteristics
3.2. Staff Participant Characteristics
3.3. Current Adjustment Support
3.4. Missing Data
3.5. Exploratory Analysis of the Efficacy of the SettleIN Intervention
3.5.1. Resident Psychological Wellbeing
3.5.2. Resident Quality of Life
3.5.3. Resident Overall Adjustment
3.6. Feasibility
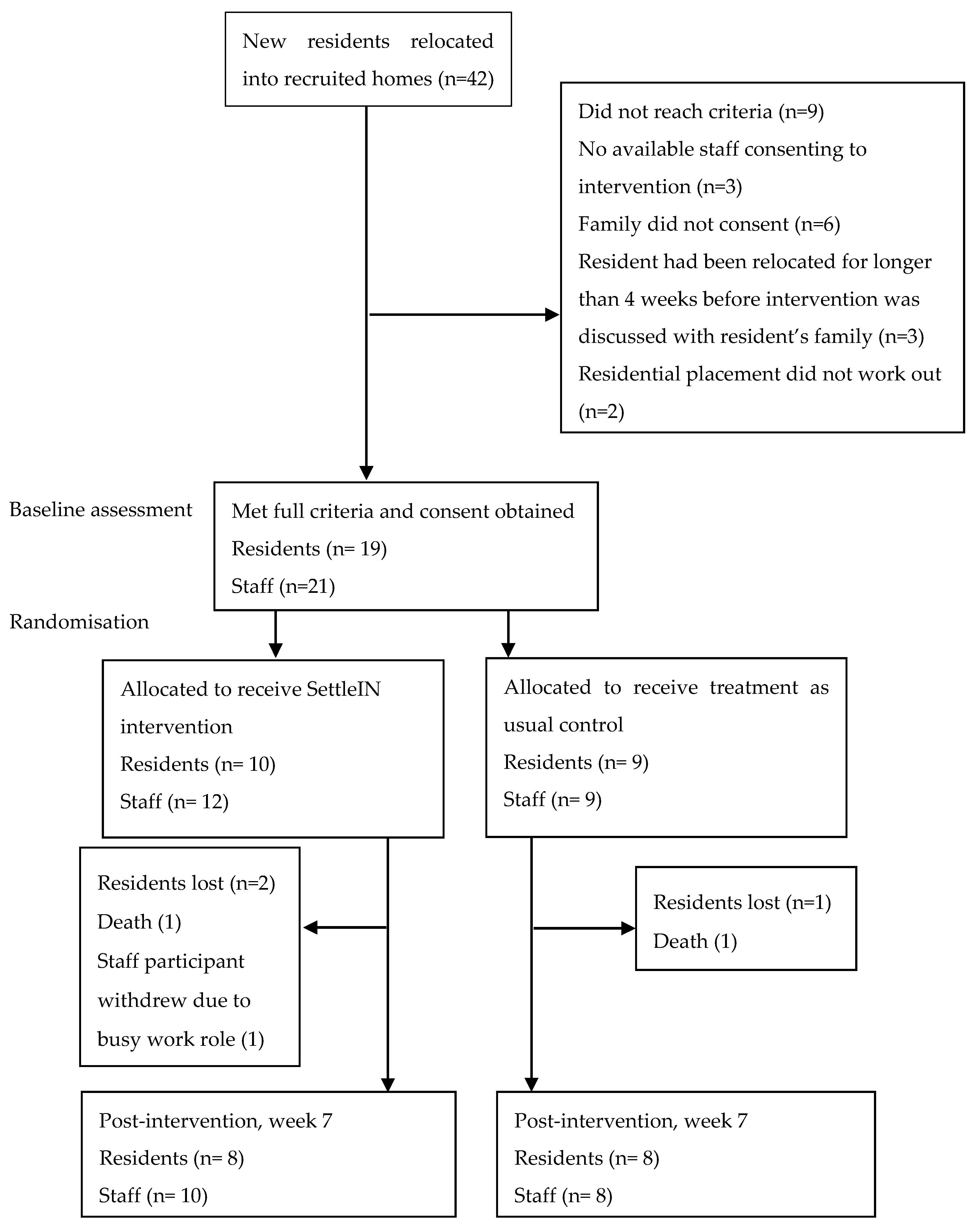
3.6.1. Recruitment and Retention
3.6.2. Implementation
3.6.3. Qualitative Analysis of Staff Interview Data
Organisational Barriers
“care staff are inundated and under, sort of, are under it with their work pressures and their day to day routine”.(P3)
“I can’t sit in one place and only do one thing because it’s the work place”.(P9)
“if there is still someone not up, you can’t just go to do the programme, you have to keep going around”.(P19)
“I had to work overtime, to catch up with work I couldn’t do”.(P17)
“I am nearly always in the last stage of dementia, when (resident) is in the first stage… so it was a lot harder to do any of the work”.(P19)
Programme Factors Acting as Barriers
“the problem is only the writing. It’s very stressful.”.(P2A)
“it took me two weeks to finish week one itself.”(P11)
Individual Resident Factors
“I cannot assume that she does not understand, but she is not responding back, just a smile”.(P8A)
“I think this is focused on the early stages of dementia”.(P11)
“It was challenging for me trying to engage with her … cos she was very ‘no no no, I don’t want to talk’”.(P14)
Acceptability of SettleIN
“I found it quite daunting to get it up and running.”(P3)
“I didn’t feel that comfortable to ask her those kinds of things… the more personal questions.”(P11)
“It is nothing to not enjoy, because its, all the tasks, we are finding they are pleasant to do… And it is just for the benefit of knowing the person more”.(P8A)
“this sort of training will help people acknowledge more about dementia”.(P6)
“Independence. Definitely. She’ll still come and say something, you know ‘where’s my room’ and I’ll go ‘… You show me’. And off she goes … You just stand up here with a silly grin on your face! Yeah! She’s doing this!”(P13)
Overcoming Challenges
“If you have partner, your colleague who you can ask… they give you good ideas”.(P8B)
“I have no time to write it down on the paper. But I have a list … for myself”.(P2B)
4. Discussions
4.1. Summary of Results
4.1.1. Efficacy of SettleIN
4.1.2. Feasibility
4.1.3. Comparison to the First SettleIN Study
4.2. Limitations
4.3. Implications for Future Research
4.4. Clinical Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Prince, M.; Knapp, M.; Guerchet, M.; McCrone, P.; Prina, M.; Comas-Herrera, A.; Wittenberg, R.; Adelaja, B.; Hu, B.; King, D.; et al. Dementia UK: Updated, 2nd ed.; Alzheimer’s Society: London, UK, 2014. [Google Scholar]
- Wilson, S.A. The transition to nursing home life: A comparison of planned and unplanned admissions. J. Adv. Nurs. 1997, 26, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Sury, L.; Burns, K.; Brodaty, H. Moving in: Adjustment of people living with dementia going into a nursing home and their families. Int. Psychogeriatr. 2013, 25, 867–876. [Google Scholar] [CrossRef] [PubMed]
- Achterberg, W.; Pot, A.M.; Kerkstra, A.; Ribbe, M. Depressive symptoms in newly admitted nursing home residents. Int. J. Geriatr. Psychiatry 2006, 21, 1156–1162. [Google Scholar] [CrossRef] [PubMed]
- Scocco, P.; Rapattoni, M.; Fantoni, G. Nursing home institutionalization: A source of eustress or distress for the elderly? Int. J. Geriatr. Psychiatry 2006, 21, 281–287. [Google Scholar] [CrossRef]
- Moon, H.; Dilworth-Anderson, P.; Gräske, J. The effects of placement on dementia care recipients’ and family caregivers’ quality of life: A literature review. Qual. Ageing Older Adults 2017, 18, 44–57. [Google Scholar] [CrossRef]
- Aminzadeh, F.; Molnar, F.J.; Dalziel, W.B.; Garcia, L.J. An exploration of adjustment needs and efforts of persons with dementia after relocation to a residential care facility. J. Hous. Elder. 2013, 27, 221–240. [Google Scholar] [CrossRef]
- Brownie, S.; Horstmanschof, L.; Garbutt, R. Factors that impact residents’ transition and psychological adjustment to long-term aged care: A systematic literature review. Int. J. Nurs. Stud. 2014, 51, 1654–1666. [Google Scholar] [CrossRef]
- Hayward, J.; Nunez, K.; Ballard, C.; Spector, A. Healthy adjustment for new residents with dementia using SettleIN: A feasibility study with staff in UK care homes. Dementia 2018, 24, 471301218806082. [Google Scholar] [CrossRef]
- Craig, P.; Dieppe, P.; Macintrye, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new medical research council guidance. Br. Med. J. 2008, 337, a1655. [Google Scholar] [CrossRef] [Green Version]
- Müller, C.; Lautenschläger, S.; Meyer, G.; Stephan, A. Interventions to support people with dementia and their caregivers during transitions from home care to nursing home care: A systematic review. Int. J. Nurs. Stud. 2017, 71, 139–152. [Google Scholar] [CrossRef]
- Davison, T.E.; Camões-Costa, V.; Clark, A. Adjusting to life in a residential aged care facility: Perspectives of people with dementia, family members and facility care staff. J. Clin. Nurs. 2019, 28, 3901–3913. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Rapaport, P.; Livingston, G.; Murray, J.; Mulla, A.; Cooper, C. Systematic review of the effective components of psychosocial interventions delivered by care home staff to people with dementia. Br. Med. J. Open 2017, 7, e014177. [Google Scholar] [CrossRef] [PubMed]
- Reisberg, B. Functional assessment staging (FAST). Psychopharmacol. Bull. 1987, 24, 653–659. [Google Scholar]
- Sclan, S.G.; Reisberg, B. Functional assessment staging (FAST) in Alzheimer’s disease: Reliability, validity and ordinality. Int. Psychogeriatr. 1992, 4 (Suppl. 1), 55–69. [Google Scholar] [CrossRef]
- Logsdon, R.; Gibbons, L.E.; McCurry, S.M. Quality of life in Alzheimer’s disease: Patient and caregiver reports. J. Ment. Health Aging 1996, 5, 21–32. [Google Scholar]
- Logsdon, R.; Gibbons, L.E.; McCurry, S.M.; Teri, L. Assessing quality of life in older adults with cognitive impairment. Psychosom. Med. 2002, 64, 510–519. [Google Scholar] [CrossRef]
- Alexopoulos, G.S.; Abrams, R.C.; Young, R.C.; Shamoian, C.A. Cornell scale for depression in dementia. Biol. Psychiatry 1988, 23, 271–284. [Google Scholar] [CrossRef]
- Müller-Thomsen, T.; Arlt, S.; Mann, U.; Maß, R.; Ganzer, S. Detecting depression in Alzheimer’s disease: Evaluation of four different scales. Arch. Clin. Neuropsychol. 2005, 20, 271–276. [Google Scholar] [CrossRef] [Green Version]
- Wongpakaran, N.; Wongpakaran, T.; van Reekum, R. Discrepancies in Cornell Scale for Depression in Dementia (CSDD) items between residents and caregivers, and the CSDD’s factor structure. Clin. Interv. Aging 2013, 8, 641–648. [Google Scholar] [CrossRef] [Green Version]
- Prager, E. Components of personal adjustment of long distance elderly movers. Gerontol. 1986, 26, 676–680. [Google Scholar] [CrossRef] [PubMed]
- Bowen, D.; Kreuter, M.; Spring, B.; Coftawoerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Cumming, G. Understanding the New Statistics: Effect Sizes, Confidence Intervals, and Meta-Analysis; Routledge Ltd.: New York, NY, USA, 2013. [Google Scholar]
- Steiner, D.L. The case of the missing data: Methods of dealing with dropouts and other research vagaries. Can. J. Psychiatry 2002, 47, 70–77. [Google Scholar] [CrossRef] [Green Version]
- Hoe, J.; Katona, C.; Roch, B.; Livingston, G. Use of the QOL-AD for measuring quality of life in people with severe dementia—The LASER-AD study. Age Ageing 2005, 34, 130–135. [Google Scholar] [CrossRef] [Green Version]
- Wenborn, J.; Challis, D.; Head, J.; Miranda-Castillo, C.; Popham, C.; Thakur, R.; Illes, J.; Orrell, M. Providing activity for people with dementia in care homes: A cluster randomised controlled trial. Int. J. Geriatr. Psychiatry 2013, 28, 1296–1304. [Google Scholar] [CrossRef]
| Theme | Feedback | Further Changes Made |
|---|---|---|
| Programme intensity |
| Some activity repetitions were reduced further |
| Additions to the programme |
| Kept new module but made it optional Agreed that supervision would be offered weekly |
| Individual resident factors as barriers |
| Inclusion criteria to not include individuals with severe dementia as measured by the Functional Assessment Staging Test To meet this criteria, resident participants had to be able to speak more than 5–7 words a day |
| Criteria | Setting | Residents | Staff |
|---|---|---|---|
| Inclusion |
|
|
|
| Module | Activity | Frequency | Minutes |
|---|---|---|---|
| Orientation | Introduce a buddy or buddies (at least one staff member and possibly another resident who knows their way around) to the new resident | 1 time in week 1 | 15 |
| Lifestyle | Gently ask the resident about how they spent their typical day, week and month prior to moving into the care home. Plan with the resident about how to keep up as many of the routines as possible (examples given) | 1 time in week 2 and week 3 | 20 |
| Family and Friends | Complete a simple family tree (see resources in the management manual for an example) | 2 times in week 1 | 20 |
| Identity | Create a ‘This is Your Life Book’ with the resident (refer to SettleIN Management Manual for guidance) | 2 times in week 3 and week 4 | 20 |
| Struggling to Engage (optional module) | Get to know the resident by talking to them about topics unrelated to their move. Example questions given e.g., what was your favourite holiday? | 2 times in week 1 | 15 |
| Area of Feasibility | Related Research Question | How Assessed |
|---|---|---|
| Acceptability | Is an enhanced version of SettleIN acceptable, attractive and satisfying to stake holders? |
|
| Demand | To what extent was enhanced SettleIN used? |
|
| Implementation | To what extent was enhanced SettleIN successfully delivered? |
|
| Practicality | To what extent was enhanced SettleIN carried out with intended participants without outside intervention? |
|
| Limited efficacy | Is an enhanced version of SettleIN effective in facilitating the adjustment of people with dementia who have recently been placed into residential care? |
|
| Recruitment | How easy was it to recruit? |
|
| Retention | How many participants stayed in the trial? |
|
| Characteristics | Control Condition (N = 9) | Intervention Condition (N = 10) |
|---|---|---|
| Age, mean (SD) | 87.90 (7.20) | 86.33 (6.58) |
| Number of days since relocation, mean (SD) | 17.00 (9.30) | 17.11 (7.83) |
| Gender, N (%) | ||
| Female | 9 (90) | 7 (78) |
| Male | 1 (10) | 2 (22) |
| Ethnicity, N (%) | ||
| White (British) | 10 (100) | 7 (78) |
| White (Other) | 0 (0) | 2 (22) |
| Religion, N (%) | ||
| Church of England | 3 (30) | 5 (56) |
| Catholic | 1 (10) | 2 (22) |
| Jewish | 3 (30) | 0 (0) |
| No religion | 3 (30) | 2 (22) |
| First language, N (%) | ||
| English | 10 (100) | 7 (78) |
| Other | 0 (0) | 2 (22) |
| Marital Status, N (%) | ||
| Single | 0 (0) | 2 (22) |
| Married | 0 (0) | 1 (11) |
| Widowed | 9 (90) | 6 (67) |
| Divorced | 1 (10) | 0 (0) |
| Dementia diagnosis, N (%) | ||
| Alzheimer’s disease | 7 (70) | 7 (78) |
| Vascular | 3 (30) | 1 (11) |
| Other | 0 (0) | 1 (11) |
| FAST score, N (%) | ||
| Mild dementia | 1 (10) | 1 (11) |
| Moderate dementia | 1 (10) | 1 (11) |
| Moderately severe dementia | 8 (80) | 7 (78) |
| Number of long term health conditions, mean (SD) | 4.20(1.99) | 3.00 (1.58) |
| Number of prescribed medications taking, mean (SD) | 7.70(3.68) | 8.00 (5.07) |
| Characteristics | Intervention Condition (N = 12) | Control Condition (N = 9) |
|---|---|---|
| Age (years), mean (SD) | 43.17 (13.72) | 38.78 (12.85) |
| Gender, N (%) | ||
| Female | 11 (92) | 7 (78) |
| Male | 1 (8) | 2 (22) |
| Job title, N (%) | ||
| Care assistant/support | ||
| worker | 8 (67) | 5 (56) |
| Senior care assistant | 1 (8) | 2 (22) |
| Team leader | 1 (8) | 2 (22) |
| Activities co-ordinator | 1 (8) | 0 (0) |
| Care manger | 1 (8) | 0 (0) |
| Years working in dementia, mean (SD) | 9.88 (9.59) | 7.97 (6.77) |
| Characteristic | N | Baseline Mean (SD) | Post-Intervention Mean (SD) | Mean Change from Baseline (SD) | P | Effect Size |
|---|---|---|---|---|---|---|
| CSDD | ||||||
| Intervention | 10 | 10.60 (5.18) | 8.20 (5.07) | +2.40 (5.52) | 0.17 | 0.70 |
| Control | 9 | 13.17 (4.57) | 14.83 (4.30) | −1.67 (6.69) | ||
| QOL-AD | ||||||
| Intervention | 10 | 31.50 (5.21) | 33.60 (6.17) | +2.10 (3.78) | 0.43 | 0.47 |
| Control | 9 | 30.83 (4.37) | 30.78 (5.65) | −0.06 (7.13) | ||
| IRA | ||||||
| Intervention | 5 | 6.40 (2.88) | 11.80 (4.67) | +5.40 (6.23) | 0.24 | 0.91 |
| Control | 5 | 8.00 (3.67) | 8.00 (5.05) | 0.00 (7.07) | ||
| Themes | Subthemes |
|---|---|
| Organisational barriers | Existing heavy workload |
| Existing task-focused approach | |
| Difficult to find the time | |
| Absence of managerial facilitation | |
| Programme factors acting as barriers | Documentation was challenging |
| Inflexibility of programme structure affects programme completion | |
| Individual resident factors | Dementia severity affected implementation |
| Resident preference affected engagement | |
| Acceptability of SettleIN | SettleIN is difficult for staff |
| SettleIN content is acceptable to staff | |
| SettleIN is positive for residents | |
| Overcoming challenges | External support is needed |
| Adopting problem solving |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saint-Bryant, C.A.; Murrill, J.; Hayward, J.K.; Nunez, K.-M.; Spector, A. SettleIN: Using a Manualised Intervention to Facilitate the Adjustment of Older Adults with Dementia Following Placement into Residential Care. Int. J. Environ. Res. Public Health 2020, 17, 2606. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072606
Saint-Bryant CA, Murrill J, Hayward JK, Nunez K-M, Spector A. SettleIN: Using a Manualised Intervention to Facilitate the Adjustment of Older Adults with Dementia Following Placement into Residential Care. International Journal of Environmental Research and Public Health. 2020; 17(7):2606. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072606
Chicago/Turabian StyleSaint-Bryant, Caroline A, Judy Murrill, Janine K Hayward, Kayleigh-Marie Nunez, and Aimee Spector. 2020. "SettleIN: Using a Manualised Intervention to Facilitate the Adjustment of Older Adults with Dementia Following Placement into Residential Care" International Journal of Environmental Research and Public Health 17, no. 7: 2606. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072606





