Impact of the COVID-19 Italian Lockdown on the Physiological and Psychological Well-Being of Children with Fragile X Syndrome and Their Families
Abstract
:1. Introduction
2. Materials and Methods
Participants
3. Procedure
4. Measures
4.1. Sleep Quality, Daily Routines and External Support Perception Information
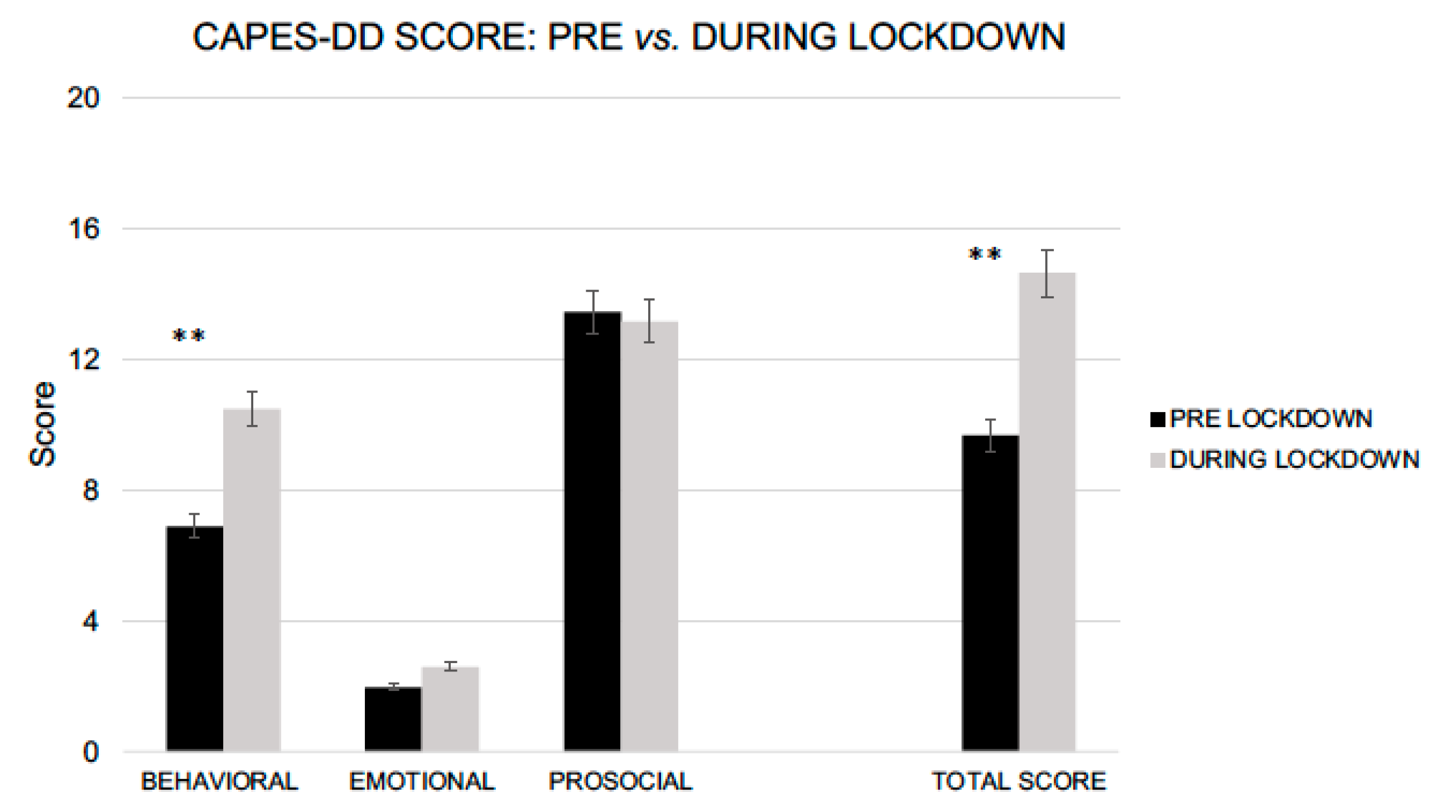
4.2. Child Adjustment and Parent Efficacy Scale-Developmental Disability (CAPES-DD)
5. Results
5.1. Sleep Quality, Daily Routines and External Support Perception Information
5.2. CAPES-DD
6. Discussion
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV); WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelov, S.; Riemann, D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052. [Google Scholar] [CrossRef] [PubMed]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef]
- Cellini, N.; Di Giorgio, E.; Mioni, G.; Di Riso, D. Sleep and psychological difficulties in italian school-age children during COVID-19 lockdown. J. Pediatr. Psychol. 2021, 46, 153–167. [Google Scholar] [CrossRef] [PubMed]
- Cusinato, M.; Iannattone, S.; Spoto, A.; Poli, M.; Moretti, C.; Gatta, M.; Miscioscia, M. Stress, Resilience, and Well-Being in Italian Children and Their Parents during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8297. [Google Scholar] [CrossRef] [PubMed]
- Di Giorgio, E.; Di Riso, D.; Mioni, G.; Cellini, N. The interplay between mothers’ and children behavioral and psychological factors during COVID-19: An Italian study. Eur. Child. Adolesc. Psychiatry 2020. [Google Scholar] [CrossRef]
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020, 221, 264–266. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Zhang, Y.; Zhao, J.; Zhang, J.; Jiang, F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020, 395, 945–947. [Google Scholar] [CrossRef]
- Bentenuto, A.; Mazzoni, N.; Giannotti, M.; Venuti, P.; de Falco, S. Psychological impact of Covid-19 pandemic in Italian families of children with neurodevelopmental disorders. Res. Dev. Disabil. 2021, 109, 103840. [Google Scholar] [CrossRef] [PubMed]
- Narzisi, A. Handle the autism spectrum condition during coronavirus (COVID-19) Stay At home period: Ten tips for helping parents and caregivers of young children. Brain Sci. 2020, 10, 207. [Google Scholar] [CrossRef] [Green Version]
- Nonweiler, J.; Rattray, F.; Baulcomb, J.; Happe, F.; Absoud, M. Prevalence and associated factors of emotional and behavioural difficulties during COVID-19 pandemic in children with neurodevelopmental disorders. Children 2020, 7, 128. [Google Scholar] [CrossRef]
- Belmonte, M.K.; Bourgeron, T. Fragile X syndrome and autism at the intersection of genetic and neural networks. Nat. Neurosci. 2006, 9, 1221–1225. [Google Scholar] [CrossRef]
- Farzin, F.; Perry, H.; Hessl, D.; Loesch, D.; Cohen, J.; Bacalman, S.; Gane, L.; Tassone, F.; Hagerman, P.; Hagerman, R. Autism spectrum disorders and attention deficit/hyperactivity disorder in boys with the fragile X premutation. J. Dev. Behav. Pediatr. 2006, 27, S137–S144. [Google Scholar] [CrossRef]
- Tsiouris, J.A.; Brown, W.T. Neuropsychiatric symptoms of fragile X syndrome. CNS Drugs 2004, 18, 687–703. [Google Scholar] [CrossRef] [PubMed]
- Rodger, S.; Umaibalan, V. The Routines and Rituals of Families of Typically Developing Children Compared with Families of Children with Autism Spectrum Disorder: An Exploratory Study. Br. J. Occup. Ther. 2011, 74, 20–26. [Google Scholar] [CrossRef]
- Jones, T.L.; Prinz, R.J. Potential roles of parental self-efficacy in parent and child adjustment: A review. Clin. Psychol. Rev. 2005, 25, 341–363. [Google Scholar] [CrossRef] [PubMed]
- Wanamaker, C.E.; Glenwick, D.S. Stress, coping, and perceptions of child behaviour in parents of preschooloers with cerebral palsy. Rehabil. Psychol. 1998, 43, 292–312. [Google Scholar] [CrossRef]
- Barlow, J.H.; Wright, C.C.; Shaw, K.L.; Luqmani, R.; Wyness, I.J. Maternal stressors, maternal wellbeing and children’s wellbeing in the context of juvenile idiopathic arthritis. Early Child Dev. Care 2002, 172, 89–98. [Google Scholar] [CrossRef]
- Roberts, C.; Mazzucchelli, T.; Taylor, K.; Reid, R. Early intervention for behaviour problems in young children with developmental disabilities. Int. J. Disabil. Dev. Educ. 2003, 50, 275–292. [Google Scholar] [CrossRef]
- Mazzucchelli, T.G.; Sanders, M.R.; Morawska, A. Child Adjustment and Parent Efficacy Scale-Developmental Disability (CAPES-DD); Parenting and Family Support Centre, University of Queensland: Brisbane, Australia, 2011. [Google Scholar]
- Emser, T.S.; Mazzucchelli, T.G.; Christiansen, H.; Sanders, M.R. Child Adjustment and Parent Efficacy Scale-Developmental Disability (CAPES-DD): First psychometric evaluation of a new child and parenting assessment tool for children with a developmental disability. Res. Dev. Disabil. 2016, 53, 158–177. [Google Scholar] [CrossRef]
- Kronk, R.; Bishop, E.E.; Raspa, M.; Bickel, J.O.; Mandel, D.A.; Bailey, D.B., Jr. Prevalence, nature, and correlates of sleep problems among children with fragile X syndrome based on a large scale parent survey. Sleep 2010, 33, 679–687. [Google Scholar] [CrossRef] [Green Version]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Pate, R.R.; Turner-McGrievy, G.M.; Kaczynski, A.T.; von Hippel, P.T. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int. J. Behav. Nutr. Phys. Act 2017, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Schaaf, R.C.; Toth-Cohen, S.; Johnson, S.L.; Outten, G.; Benevides, T.W. The everyday routines of families of children with autism: Examining the impact of sensory processing difficulties on the family. Autism 2011, 15, 373–389. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.A.; Tint, A.; Paquette-Smith, M.; Lunsky, Y. Perceived self-efficacy in parents of adolescents and adults with autism spectrum disorder. Autism 2016, 20, 425–434. [Google Scholar] [CrossRef]
- Sofronoff, K.; Farbotko, M. The effectiveness of parent management training to increase self-efficacy in parents of children with Asperger syndrome. Autism 2002, 6, 271–286. [Google Scholar] [CrossRef] [PubMed]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The effect of COVID-19 on youth mental health. Psychiatr. Q. 2020, 91, 841–852. [Google Scholar] [CrossRef]
- Hipp, L.; Bünning, M.; Munnes, S.; Sauermann, A. Problems and pitfalls of retrospective survey questions in COVID-19 studies. Surv. Res. Methods 2020, 14, 109–114. [Google Scholar]
| MOTHERS | N (%) | |
|---|---|---|
| Diagnosis | Full Mutation | 8 (17) |
| Premutation | 30 (62) | |
| Mosaicism | 10 (21) | |
| Work condition | Smart working | 18 (38) |
| Stopped | 8 (16) | |
| No work | 13 (27) | |
| Regular | 9 (19) | |
| COVID-19 information (How often…?) | Never | 2 (4) |
| Sometimes | 31 (65) | |
| Often | 13 (27) | |
| Frequently | 2 (4) | |
| COVID-19 information (Where…?) | TV | 45 (94) |
| Daily Newspapers | 31 (65) | |
| Internet | 24 (50) | |
| Social Media | 19 (40) | |
| CHILDREN | N (%) | |
| Diagnosis | Full Mutation | 42 (79) |
| Premutation | 2 (4) | |
| Mosaicism | 9 (17) | |
| Covid-19 information (How…?) | Fairy Tails | 15 (28) |
| Video | 20 (38) | |
| Scientific Information | 13 (25) | |
| Family | 45 (85) | |
| CHILDREN SLEEP QUALITY | ||
| BEFORE LOCKDOWN N (%) | DURING LOCKDOWN N (%) | |
| Difficulty falling asleep | Never 31 (58) | 24 (45) |
| Sometimes 19 (36) | 21 (40) | |
| Often 3 (6) | 8 (15) | |
| Time to fall asleep | >60 min 1 (2) | 4 (7) |
| 45–60 min 4 (7) | 7 (13) | |
| 30–45 min 7 (13) | 10 (19) | |
| 15–30 min 21 (40) | 18 (34) | |
| <15 min 20 (38) | 14 (27) | |
| Hours sleeping per night | 8–11 h 39 (73) | 39 (73) |
| 5–8 h 13 (25) | 13 (25) | |
| <5 h 1 (2) | 1 (2) | |
| Number of times of night awakenings | Never 27 (51) | 24 (45) |
| <2 times 21 (40) | 21 (40) | |
| 2–4 times 5 (9) | 6 (11) | |
| >4 times 0 (0) | 2 (4) | |
| Difficulty waking up in the morning | Yes 10 (19) | 8 (15) |
| No 43 (81) | 45 (85) | |
| CHILDREN DAILY ROUTINES | ||
| BEFORE LOCKDOWN N (%) | DURING LOCKDOWN N (%) | |
| Speech Therapy | 21 (40) | 7 (13) |
| Psychomotor Therapy | 27 (51) | 10 (19) |
| Occupational Therapy | 11 (21) | 3 (6) |
| Sport Activities | 35 (66) | 6 (11) |
| Educational and peer Activities | 20 (38) | 9 (17) |
| χ2 | p | |
|---|---|---|
| Family (grandparents) | 40.82 | <0.001 |
| Friends | 18.02 | 0.001 |
| X-Fragile Associations | 49.25 | <0.001 |
| Educators | 35.76 | <0.001 |
| Teachers | 30.15 | <0.001 |
| Other (Doctors) | 31.32 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Giorgio, E.; Polli, R.; Lunghi, M.; Murgia, A. Impact of the COVID-19 Italian Lockdown on the Physiological and Psychological Well-Being of Children with Fragile X Syndrome and Their Families. Int. J. Environ. Res. Public Health 2021, 18, 5752. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18115752
Di Giorgio E, Polli R, Lunghi M, Murgia A. Impact of the COVID-19 Italian Lockdown on the Physiological and Psychological Well-Being of Children with Fragile X Syndrome and Their Families. International Journal of Environmental Research and Public Health. 2021; 18(11):5752. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18115752
Chicago/Turabian StyleDi Giorgio, Elisa, Roberta Polli, Marco Lunghi, and Alessandra Murgia. 2021. "Impact of the COVID-19 Italian Lockdown on the Physiological and Psychological Well-Being of Children with Fragile X Syndrome and Their Families" International Journal of Environmental Research and Public Health 18, no. 11: 5752. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18115752






